Abstract
Radiology practice guidelines have been developed to help radiologists achieve quality and safety in their clinical practice. One means to promote the use of practice guidelines in radiology is through wider use of reporting templates, also known as “structured reporting.” This article presents specific examples in which radiology reporting templates can promote adherence to guidelines, gather data for quality improvement efforts, and facilitate compliance with performance incentive programs.
Keywords: Clinical practice guidelines, Reporting, Quality, Education, Evidence-based radiology
Introduction
Radiology practice guidelines, such as those developed by the American College of Radiology (ACR), offer recommendations to help radiologists achieve quality and safety in their clinical practice. One means to promote the use of practice guidelines in radiology is through wider use of reporting templates, also known as “structured reporting.” As the official record of a diagnostic, interventional, or therapeutic procedure, the radiology report contains a wealth of information and serves a wide variety of purposes. The radiology report details the patient demographics, the imaging procedure, the procedure’s date and time stamp, and information provided by the ordering health care provider. The report describes the procedure performed, the technical factors associated with the examination, the imaging observations, and a summary. The report captures important technical and billing information and communicates pertinent clinical findings to the referring providers.
The radiology report also has a role in documenting adherence to external guidelines and mandates developed to measure, standardize, and improve the delivery of health care. The U.S. government has made a significant investment in order to expand the use of Electronic Health Records (EHR) through key components of the American Recovery and Reinvestment Act (ARRA) and the Health Information Technology for Economic and Clinical Health (HITECH) Act of 2009 (1). Hospitals and providers who demonstrate “meaningful use” of EHR will qualify for incentive payments in the short term. For 2015 and later, those that do not successfully demonstrate this meaningful use will have a payment adjustment in their Medicare reimbursement. The Center for Medicare and Medicaid (CMS) states, “‘meaningful use’ means providers need to show they’re using certified EHR technology in ways that can be measured significantly in quality and in quantity”(2).
The current definitions of meaningful use are specified to garner data into EHRs using structured data, including patient demographics, vital signs, problem lists, and specific types of interventions. The activities that document meaningful use include electronic prescribing (e-prescribing), computer physician order entry (CPOE), and implementation of a monitoring system for potential drug-drug and drug-allergy interactions (3). The ARRA specifies that hospitals and providers demonstrate the ability to use EHR in ways that can be measured in order to ensure consistency, improve quality and reduce errors in medical care (4). The adoption of EHR is being advocated with the belief that the information contained in EHR will improve medical decision making with an associated improvement in patient outcomes (3). The radiology report offers a unique medium to facilitate the documentation of structured data elements.
For radiologists, a key benefit and component of these developments will be adoption of evidence-based decision support systems for ordering imaging tests. Although the specific early mandates for CPOE are tied to medication order entry, it is anticipated that utilization of decision support eventually will encompass imaging as well. Such decision support systems require a solid base of evidence (5). There is also an incentive for radiologists (and all physicians) to document compliance with specific imaging metrics via the linked CMS Physicians Quality Reporting System (PQRS) (6). By 2015, like the meaningful use incentive, lack of participation in PQRS will result in a penalty rather than an incentive.
The goal of this article is to present specific examples in which the use of radiology reporting templates – also known as “structured reporting” – can promote adherence to guidelines, provide data for quality improvement efforts, and support “meaningful use” of electronic health records.
Radiology Reporting Templates
The Radiological Society of North America (RSNA) has developed a library of more than 210 reporting templates contributed by radiology societies, institutions, and individuals (7). This effort was undertaken in response to consensus at the 2007 ACR Intersociety Conference that the radiology report is a key area for practice improvement (8). The open, online library (www.radreport.org) offers the templates both in text format resembling dictation systems’ “speech macros” and in Extensible Markup Language (XML) for interoperability with information systems. DICOM Supplement 155, currently under development, seeks to define a standardized structure for radiology reporting templates and how reports based on such templates will be transmitted to an electronic health record system.
Unlike the ACR’s practice guidelines, which have been developed by expert panels, reviewed extensively, and approved by the ACR Council, the RSNA reporting templates are not intended to serve as national standards at this time. Radiologists may adapt and apply these templates to meet the needs of their clinical practice. The templates are designed to provide more standardized language and content, yet offer a flexible way for radiologists to generate reports using existing reporting technologies. The elements of each reporting template are linked to terms in controlled vocabularies such as RadLex® (9, 10) and the Systematized Nomenclature of Medicine Clinical Terms (SNOMED CT®) (11, 12). These vocabularies define the semantics of the terms used in the reporting templates, and allow interoperability across different institutions, between different reporting systems, and even across languages.
Practice guidelines
To explore how template-based reporting might facilitate compliance with radiology practice guidelines, we explored four ACR practice guidelines in detail. We selected guidelines across a variety of scenarios: radiographic and digital imaging examinations, adult and pediatric patient populations, and diagnostic and interventional procedures. The guidelines included esophagography (13), radiographic skeletal survey (for suspected physical child abuse) (14), non-contrast head CT in the setting of stroke (15), and percutaneous nephrostomy (16).
(1) Esophagography
Clinical indications
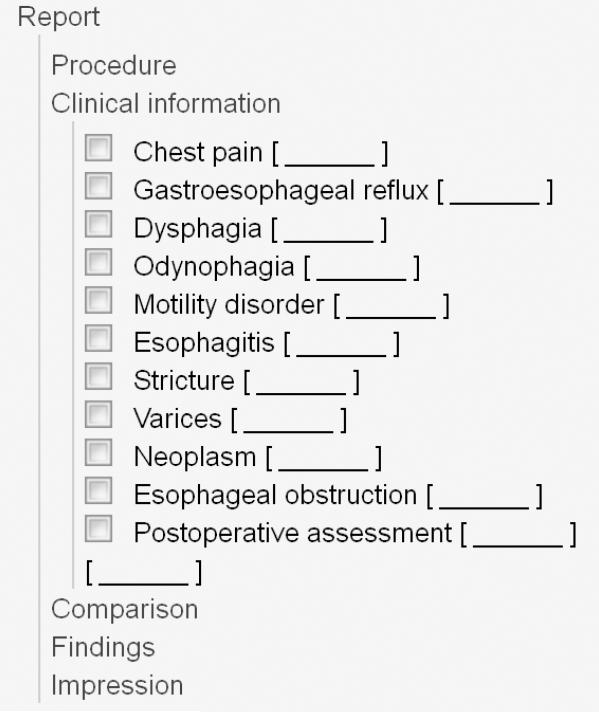
Single-contrast and double-contrast (biphasic) examinations of the esophagus are proven and useful procedures for evaluating the presence, nature, and extent of esophageal disease. The ACR Practice Guideline for the Performance of Esophagrams and Upper Gastrointestinal Examinations in Adults (13) itemizes indications for esophagography (Table 1). The corresponding reporting template provides this list as a set of optional items to be incorporated into the report. By listing potential indications, the radiology report can be used to capture data about the patient, including the symptoms that prompted the examination. If an item is included, one can provide additional details that pertain to that item: for example, one might include the element for “Dysphagia” and provide a comment to indicate “present for 3 months, worse with solids.” The reporting template includes “free text” fields to allow radiologists to incorporate information other than the preselected items (Figure 1).
Table 1. Indications for Esophagography.
|
Figure 1.
Esophagography reporting template, expanded to demonstrate the clinical information section
Fluoroscopy time
The Esophagram reporting template includes a field to indicate fluoroscopy time (in minutes). This field prompts the reporting physician to incorporate this important piece of information, which can be used to meet the goals of PQRS Measure # 145 to compute the percentage of final reports for procedures using fluoroscopy that include documentation of patient radiation exposure or exposure time (6). Further, the fluoroscopy times could be averaged by radiologist and provided as feedback to the division/department for comparison of these times per radiologist to arrive at a reasonable target for the group. Achieving a target fluoroscopy time also may be used for individual focused professional practice evaluation (FPPE) and ongoing professional practice evaluation (OPPE) metrics, which are required by the Joint Commission.
Use of coded information
The schema for reporting templates provides a specification for coded information, such as dose indices, to be extracted from imaging procedure information. The Esophagram report template is coded with a RadLex Playbook identifier, which identifies the procedure so that equivalent procedures can be mapped across institutions (http://rsna.org/RadLex_Playbook.aspx). Indications, such as Dysphagia, are mapped to RadLex and/or SNOMED CT terms. In that way, one can easily extract information from the completed reports to correlate the indications for the examination and whether the test was positive. Ideally, one would wish to correlate the indications and test results more broadly with other health outcomes. The coded value for fluoroscopy time will allow information to be extracted from the report for entry into radiation dose registries. Although not presently collected as part of the ACR Dose Index Registry (DIR) or the General Radiology Improvement Database (GRID), fluoroscopy time is envisioned for incorporation within the next few years (L. Coombs, personal communication, March 2012). By consistently recording the fluoroscopy time, radiologists will be better able to track this information, identify best practices, and potentially reduce radiation dose and thus improve patient safety.
(2) Skeletal survey for the investigation of child abuse
Clinical indications
The ACR-SPR Practice Guideline for Skeletal Surveys in Children (14) identifies three possible indications for skeletal survey examinations, where the condition may be known or suspected: (1) physical abuse in infants and young children; (2) skeletal dysplasias, syndromes, and metabolic disorders; and (3) neoplasia and related disorders. By prompting for these reasons as part of the reporting template, one can capture statistical data about the indications for the examination and the corresponding number of abnormal (positive) examinations.
Procedure performed
The minimum complete skeletal survey examination consists of 21 radiographs, as detailed in Table 1. A radiologist’s reporting template could allow one to check off the views obtained, or to flag those not obtained; such information can be used to monitor examination quality.
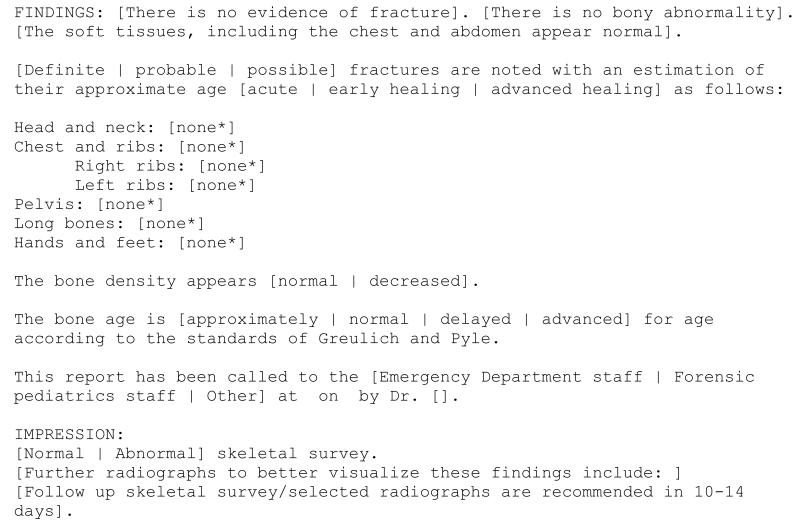
Detection and communication of abnormalities
The official interpretation of the examination should provide a concise description of all sites of definite and suspected abnormality. The practice guideline stipulates that, “When a constellation of radiographic findings is sufficient to raise strong suspicion of abuse, this should be so stated in the radiology report and communicated to the referring physician, and this communication should be documented in the final report.” Because one is often legally required to notify local child protection authorities in cases of suspected child abuse, there are settings where the radiologist may be required to do so if the referring physician does not report the case. The reporting template could be structured to provide a field to capture information about communication of the results to the referring physician and/or child welfare authorities. Placeholders in the report template can help assure that the correct actions take place and that radiologists record those actions appropriately (Figure 2).
Figure 2.
Skeletal survey reporting template for suspected non-accidental trauma
(3) Non-contrast head CT for stroke
The ACR and American Society of Neuroradiology (ASNR) have defined a practice guideline for the performance of computed tomography (CT) of the brain (15). PRQS measure # 10 requires that every non-contrast head CT examination identify whether mass, intracranial hemorrhage, or acute infarction is present (6). Because radiologists’ reimbursement from Medicare eventually will depend on their compliance with this requirement, it is useful to incorporate such information into the reporting template.
The PQRS measure is defined as “For patients aged 18 years and older with either a diagnosis of ischemic stroke or TIA or intracranial hemorrhage OR at least one documented symptom consistent with ischemic stroke or TIA or intracranial hemorrhage that includes documentation of the presence or absence of each of the following: hemorrhage and mass lesion and acute infarction.” Thus, the non-contrast head CT report template might prompt the radiologist to state “There is no evidence of hemorrhage, mass lesion, acute infarction,” or, if the radiologist chooses, to specify the presence or absence of each observation individually.
(4) Percutaneous nephrostomy
The ACR and Society of Interventional Radiology (SIR) have defined a practice guideline that sets out proper indications, materials, and reporting standards for the performance of percutaneous nephrostomy (16) as well as a guideline on reporting and archiving of interventional radiology procedures (17). Proper documentation of interventional procedures requires a record of informed consent, pre-procedure time-out, description of the procedure performed, materials used, patient complications, and fluoroscopy time. By prompting the radiologist to incorporate these elements in the report, the reporting template promotes compliance with the corresponding practice guideline and assures complete documentation for billing, compliance initiatives such as PQRS measure #145 for fluoroscopy time, and quality review.
Clinical Indications
The practice guideline lists the most common indications for nephrostomy. By listing potential indications, the radiology report can systematically and uniformly capture patient- and procedure-specific data, including the symptoms that prompted the examination. The guideline also suggests a trigger for a quality-assurance review if, in more than 5% of cases, the procedure is performed for non-standard indications.
Complication rates and thresholds
The Society of Interventional Radiology (SIR) has developed a standardized terminology for reporting complications of interventional radiology procedures (18, 19). Such an approach could allow radiologists to aggregate information about complications from individual radiology practices into a regional or national data registry. Registries allow benchmarking (comparing one’s own practice to national norms) and trend analysis (tracking national and/or local complication rates over time). Each interventional radiology report should contain structured fields for documentation of the most frequent complications so that they may be tracked. For example, nephrostomy procedures have risks of septic shock, hemorrhage, and pleural complications. The literature suggests that the success rate for relieving obstruction is 85% to 98% and the complication rate is 0.1% to14% (20). By incorporating specific elements into the template, it is possible to evaluate performance relative to evidence-based expectations.
Discussion
This article draws upon practice guidelines and reporting templates for four specific radiology procedures to illustrate how structured reporting can improve consistency, capture mandated quality metrics, and promote guideline-based care. The primary goals of structured reporting initiatives to date have been to facilitate the creation of imaging reports and to make them easier for referring physicians to read and understand (21). However, template-based reports clearly have additional advantages. By prompting the reporting physician to include specific pieces of information, the templates can make reports more uniform and complete. Detailed information within the report can help assure that performance-related data are described systematically. Standardized text can assist the radiologist in disseminating professional society guidelines. Structured reports can provide a framework from which coded values may be extracted routinely into a database to allow data mining. Finally, structured reporting can facilitate the capture and encoding of information that is necessary for decision support.
The CMS Physician Quality Reporting System (PQRS) provides an incentive payment to physicians who voluntarily and satisfactorily report data on quality measures for covered professional services. The PQRS is mandated by federal legislation, and implemented through a series of published regulations. In 2012, successful reporting of measures will qualify an individual provider for a payment equal to 0.5% of their total estimated Medicare Part B physician fee schedule allowed charges. However, after 2014, this incentive will become a penalty (6). Two of five PQRS measures relevant to radiologists are described in detail in the examples provided above. With a field for fluoroscopy time in the esophagram report, it becomes a simple process to compute the percentage of fluoroscopy procedures that document radiation exposure time (to meet the 50% minimum target). By requiring the systematic documentation of hemorrhage, mass lesion and acute infarction in the non-contrast head CT template, the radiologist can provide appropriate patient care and avoid penalties for omitting required information.
Standardized report text could help the radiologist capture information to develop benchmarks for practice and to disseminate professional society guidelines. The percutaneous nephrostomy template shows how a template provides the information for which consistently defined data could be collected across enterprises and aggregated to build national registries of clinical outcomes, radiation dose, and complication rates. As more data are collected from benchmarking, the quality thresholds might be tailored to represent more accurately the acuity mix at a given institution.
Reporting templates can serve as an educational tool to help radiologists achieve best practices. Direct evidence of this benefit of structured reporting does not yet exist. However, studies have highlighted gaps in compliance with PQRS measures and variability in practice recommendations (22, 23). In one study, only 58% of CT and MRI examinations for suspected stroke specifically documented the presence or absence of hemorrhage, mass, and acute infarction to comply with PQRS measure #10 (23). A 2008 survey (24) demonstrated a gap between the knowledge of the Fleischner Society guidelines for the management of small, incidentally detected lung nodules (25) and their use in practice. In one series, only 34% of radiology reports included recommendations consistent with the guidelines (22). Unlike practice guidelines, which may not be available at the point of care, reporting templates provide a ready-made reminder script that radiologists can choose to apply. The Breast Imaging Reporting and Data System (BI-RADS) is the best known example of the use of controlled terminology and structured reporting to promote adherence to guidelines (26, 27).
By creating standardized text that is easily inserted into a report at the time of dictation, one can improve the dissemination of guidelines, compliance with guidelines, and study of their impact. Many radiology residents train at institutions with speech-recognition systems for dictating reports that typically include “macros” of pre-specified text or “fill-in-the-blank” forms. By incorporating reporting templates into their training, residents are prompted to include necessary elements in their reports (28). With the establishment of benchmarks, it will be possible to conduct studies that evaluate which specific tools, including structured reporting, best enable radiologists to adapt to changing practice requirements.
The examples in this document demonstrate potential benefits and opportunities created by template-based reporting. It is important to acknowledge significant limitations in the current state of structured reporting. A study that systematically compared the quality of reports created using a structured reporting system to free-text dictation found that structured reporting reduced both accuracy and completeness; participants indicated that the reporting system was constraining and time-inefficient (29). Based on this experience, it was suggested that structured reporting systems be further optimized to focus on ease of use and on agreement with standardized lexicons. There remains a gap between the current available structured templates, the ease with which they are incorporated into speech recognition and dictation systems, and the measurement of their benefits. However both the template library and systematic review of current practice are creating the tools and opportunities for radiology reporting practices to change and adapt to compliance requirements.
Conclusions
As the ACR Practice Guidelines state in their preamble, “guidelines are an educational tool designed to assist practitioners in providing appropriate radiologic care for patients. They are not inflexible rules or requirements of practice and are not intended, nor should they be used, to establish a legal standard of care.” Radiology reporting templates can promote the use of practice guidelines to improve the quality and safety of clinical practice, and can form a framework to support evidence-based radiology. The authors believe that the ACR should work to refine and improve radiology reporting templates and should recommend their use.
Table 2. Skeletal survey radiographs. for the evaluation of non-accidental trauma.
|
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Blumenthal D, Tavenner M. The “meaningful use” regulation for electronic health records. N Engl J Med. 2010;363(6):501–4. doi: 10.1056/NEJMp1006114. [DOI] [PubMed] [Google Scholar]
- 2.Meaningful Use. Centers for Medicare & Medicaid Services (CMS) 2012 CMS.gov. cited 2012 2 May 2012. Available from: https://www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/Meaningful_Use.html.
- 3.Blumenthal D. Promoting use of health IT: why be a meaningful user? Md Med. 2010;11(3):18–9. [PubMed] [Google Scholar]
- 4.CMS EHR Meaningful Use Overview. Baltimore, MD: Centers for Medicare & Medicaid Services. 2012 CMS.gov. cited 2012 19 April 2012. Available from: https://www.cms.gov/EHRIncentivePrograms/30_Meaningful_Use.asp.
- 5.Khorasani R. Can radiology professional society guidelines be converted to effective decision support? Journal of the American College of Radiology: JACR. 2010;7(8):561–2. doi: 10.1016/j.jacr.2010.05.017. [DOI] [PubMed] [Google Scholar]
- 6.Physician Quality Reporting System: Overview. Centers for Medicare & Medicaid Services. 2011 CMS.gov. updated 10/17/2011; cited 2011 12/19/2011. Available from: http://www.cms.gov/PQRS/
- 7.Kahn CE, Jr., Langlotz CP, Burnside ES, et al. Toward best practices in radiology reporting. Radiology. 2009;252(3):852–6. doi: 10.1148/radiol.2523081992. [DOI] [PubMed] [Google Scholar]
- 8.Dunnick NR, Langlotz CP. The radiology report of the future: a summary of the 2007 Intersociety Conference. Journal of the American College of Radiology: JACR. 2008;5(5):626–9. doi: 10.1016/j.jacr.2007.12.015. [DOI] [PubMed] [Google Scholar]
- 9.Langlotz CP. RadLex: a new method for indexing online educational materials. Radiographics: a review publication of the Radiological Society of North America, Inc. 2006;26(6):1595–7. doi: 10.1148/rg.266065168. [DOI] [PubMed] [Google Scholar]
- 10.Rubin DL. Creating and curating a terminology for radiology: ontology modeling and analysis. J Digit Imaging. 2008;21(4):355–62. doi: 10.1007/s10278-007-9073-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Coté RA, Rothwell DJ, Beckette R, Palotay J. SNOMED International: The Systematized Nomenclature of Human and Veterinary Medicine. 3rd ed. College of American Pathologists; Northfield, IL: 1993. [Google Scholar]
- 12.SNOMED International SNOMED CT. College of American Pathologists. 2005 cited 2005 14 July 2005. Available from: http://www.snomed.org/snomedct/
- 13.ACR Practice Guideline for the Performance of Esophagrams and Upper Gastrointestinal Examinations in Adults. American College of Radiology. 2008 [Google Scholar]
- 14.ACR-SPR Practice Guideline for Skeletal Surveys in Children. American College of Radiology. 2006 [Google Scholar]
- 15.ACR-ASNR Practice Guideline for the Performance of Computed Tomography (CT) of the Brain. American College of Radiology. 2010 [Google Scholar]
- 16.ACR-SIR-SPR Practice Guideline for the Performance of Percutaneous Nephrostomy. American College of Radiology. 2011 [Google Scholar]
- 17.ACR-SIR Practice Guideline for the Reporting and Archiving of Interventional Radiology Procedures. American College of Radiology. 2009 [Google Scholar]
- 18.Omary RA, Bettmann MA, Cardella JF, et al. Quality improvement guidelines for the reporting and archiving of interventional radiology procedures. J Vasc Interv Radiol. 2003;14(9 Pt 2):S293–5. doi: 10.1097/01.rvi.0000094601.83406.e1. [DOI] [PubMed] [Google Scholar]
- 19.Sacks D, McClenny TE, Cardella JF, Lewis CA. Society of Interventional Radiology clinical practice guidelines. J Vasc Interv Radiol. 2003;14(9 Pt 2):S199–202. doi: 10.1097/01.rvi.0000094584.83406.3e. [DOI] [PubMed] [Google Scholar]
- 20.Ramchandani P, Cardella JF, Grassi CJ, et al. Quality improvement guidelines for percutaneous nephrostomy. J Vasc Interv Radiol. 2003;14(9 Pt 2):S277–81. [PubMed] [Google Scholar]
- 21.Schwartz LH, Panicek DM, Berk AR, Li Y, Hricak H. Improving communication of diagnostic radiology findings through structured reporting. Radiology. 2011;260(1):174–81. doi: 10.1148/radiol.11101913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lacson R, Prevedello LM, Andriole KP, et al. Factors associated with radiologists’ adherence to fleischner society guidelines for management of pulmonary nodules. Journal of the American College of Radiology: JACR. 2012;9(7):468–73. doi: 10.1016/j.jacr.2012.03.009. [DOI] [PubMed] [Google Scholar]
- 23.Prevedello LM, Farkas C, Ip IK, et al. Large-scale automated assessment of radiologist adherence to the Physician Quality Reporting System for stroke. Journal of the American College of Radiology: JACR. 2012;9(6):414–20. doi: 10.1016/j.jacr.2012.01.014. [DOI] [PubMed] [Google Scholar]
- 24.Eisenberg RL, Bankier AA, Boiselle PM. Compliance with Fleischner Society guidelines for management of small lung nodules: a survey of 834 radiologists. Radiology. 2010;255(1):218–24. doi: 10.1148/radiol.09091556. [DOI] [PubMed] [Google Scholar]
- 25.MacMahon H, Austin JH, Gamsu G, et al. Guidelines for management of small pulmonary nodules detected on CT scans: a statement from the Fleischner Society. Radiology. 2005;237(2):395–400. doi: 10.1148/radiol.2372041887. [DOI] [PubMed] [Google Scholar]
- 26.Burnside ES, Sickles EA, Bassett LW, et al. The ACR BI-RADS experience: learning from history. J Am Coll Radiol. 2009;6(12):851–60. doi: 10.1016/j.jacr.2009.07.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Langlotz CP. ACR BI-RADS for breast imaging communication: a roadmap for the rest of radiology. J Am Coll Radiol. 2009;6(12):861–3. doi: 10.1016/j.jacr.2009.09.015. [DOI] [PubMed] [Google Scholar]
- 28.Mainiero MB. Incorporating ACR Practice Guidelines, Technical Standards, and Appropriateness Criteria into resident education. J Am Coll Radiol. 2004;1(4):277–9. doi: 10.1016/j.jacr.2004.01.009. [DOI] [PubMed] [Google Scholar]
- 29.Johnson AJ, Chen MY, Swan JS, Applegate KE, Littenberg B. Cohort study of structured reporting compared with conventional dictation. Radiology. 2009;253(1):74–80. doi: 10.1148/radiol.2531090138. [DOI] [PubMed] [Google Scholar]