Abstract
This study examines how different information sources relate to Health Belief Model (HBM) constructs, hepatitis B virus (HBV) knowledge, and HBV screening. The Maryland Asian American Liver Cancer Education Program administered a survey of 877 Asian immigrants. The most common sources of information identified by the multiple-answer questions were newspapers (39.8%), physicians (39.3%), friends (33.8%), TV (31.7%), and the Internet (29.5%). Path analyses—controlling for age, sex, educational level, English proficiency, proportion of life in U.S., health insurance coverage, and family history of HBV infection—showed that learning about HBV from physicians had the strongest direct effect; friends had a marginal indirect effect. Perceived risk, benefits, and severity played limited roles in mediation effects. Path analysis results differed by ethnicity. Physician-based HBV screening intervention would be effective, but should be complemented with community health campaigns through popular information sources for the uninsured.
Keywords: Hepatitis B, Asian American, health information, screening, Health Belief Model
Introduction
Over the last decade Asian populations in the U.S. grew by 43%—the fastest rate among other racial groups [1]. The rapid growth of Asian populations is largely driven by immigration to the U.S. [2]. Asian immigrants (AIs)—particularly from hepatitis B endemic countries—have been at greater risk of contracting hepatitis B virus (HBV) infection, and of subsequently developing cirrhosis or liver cancer [3,4]. Those with chronic HBV infection are 200 times more likely to develop liver cancer than those without the infection [5]. Preventive measures such as HBV screening and vaccinations allow us to prevent or manage potential liver disease or liver cancer; however, these preventive measures are not widely practiced among adult AIs[6].
The low levels of HBV knowledge and poor English proficiency are important individual-level barriers to obtaining HBV screening [7,8,9,10]. Lack of health coverage and not having a regular physician are important resource-related barriers for the screening behaviors [11]. An individual’s perceptions and psychosocial factors are also important factors for HBV screening behavior [12,13,14]. Where and how people acquire risk perception and knowledge about preventive health behavior is an important research question [15,16,17,18,19,20]. Very few studies have focused on how different sources of health information influence not only health knowledge, but also important psychosocial factors related to health behavior [21]. Moreover, we have very limited understanding about how these acquired knowledge and perceptions relate to preventive behaviors [20]. To fill in this gap, we examined what the common information sources of HBV are and the associations with HBV screening behavior with a Health Belief Model (HBM) framework. Ma et al. (2007) tested these constructs in relation to HBV screening behavior in a Vietnamese-immigrant sample: perceived risk was positively associated with hepatitis B screening behavior [14]. This finding provided support for the HBM’s premise that higher perceived risk motivates individuals to adopt preventive health behaviors. We further examined the mediating effects of the HBM constructs in associations between information sources and screening behavior.
The purpose of our study is to (1) understand the most common information sources regarding HBV, (2) examine variations of common information sources by ethnicity, educational level, English proficiency, and age, (3) examine how different sources of information relate to psychosocial constructs and HBV knowledge and screening behavior by path analysis with the HBM framework, and (4) assess variations of these associations by ethnicity.
Method
We used baseline survey data collected by the Maryland Asian American Liver Cancer Education Program (hereinafter the Program). The Program was a cluster randomized trial design that tested the effectiveness of a hepatitis B/liver cancer educational program on HBV screening among at-risk Asian immigrants [22]. The study design allowed us to effectively recruit these minority populations in our study and to enhance the ability to control knowledge contaminations across the participants.
The Program recruited 877 participants in Maryland during 2009 and 2010: 294 Korean, 303 Chinese, and 280 Vietnamese immigrants. The Program received approval for Human Subject Research from the Institutional Review Board of XXXXXX.
Recruitment Strategy
Korean, Chinese, and Vietnamese participants were recruited through community organizations, churches, language schools, ethnic grocery stores/restaurants, and nail salons in Maryland [23]. The sampling frame for these organizations was created from ethnic yellow-pages, industry membership directories, and suggestions from community leaders in the Greater Washington, DC Area. Thirty-two organizations agreed to participate in the Program and were randomized to either intervention or control groups. We recruited 877 participants from these organizations on a voluntary basis if they were at least 18 years of age and had never participated in hepatitis B education. Participants filled in a paper form, self-administered baseline questionnaire in their choice of either their native language or English.
Measures
The questionnaires were translated into respective ethnic languages by bilingual research assistants and back-translated into English by different bilingual research assistants. The translated questionnaire were compared and discussed to reach to a consensus of the best wording choices in each ethnic language. The questionnaire was pilot tested in each ethnic group and reviewed by community advisory board members.
The primary outcome in our study is a self-reported HBV screening (either yes or no). The main independent variables of the analysis were the top five sources of HBV. We asked respondents about sources of HBV information from 12 potential sources of information, with multiple responses: physicians, other health care providers, local health departments, family, friends, TV, radio, newspapers, books, magazines, the Internet, and community health fairs. These options were adapted from the National Cancer Institute’s Health Information National Trends Survey (HINTS) [24].
Mediators included HBM constructs (perceived benefits, perceived risk, perceived severity, self-efficacy for HBV screening) and knowledge of HBV transmission modes. For perceived benefits, one item assessed how strongly a respondent agreed with the statement “the benefits of getting HBV screening outweigh the costs.” For perceived severity, three items asked about how severely a respondents’ life would be changed if they contracted the virus (α =0.80). Four items on self-efficacy examined the level of self-confidence to undergo the screening in challenging circumstances (α=0.90). We used the 7-point Likert scale to assess these HBM constructs: from “strongly agree” (7) to “strongly disagree” (1). For perceived risk, four items in different time spans asked about the perceived likelihood of contracting HBV in the 10-point Likert scale: from “very likely” (10) to “not at all likely” (0) (α=0.94). The items were used to create a composite index score for each construct by calculating a summative mean: the higher the score, the greater perceived benefit, risk, susceptibility, and self-efficacy. A set of 10 questions to assess knowledge regarding HBV transmission modes was adapted from research studies with Vietnamese and Cambodian Americans in the Pacific Northwest [25]. A sum of respondents’ correct answers was calculated as the knowledge score; the knowledge score could vary from 0 to 10. Reliability of this knowledge scale was above the acceptable level (α=0.88).
Potential confounders included age (continuous variable), sex (0=male; 1=female), educational level (0=<college; 1=college graduate or higher), proportion of life in the U.S. (0=≤25%; 1=>25%), English language proficiency (0=poor/so so; 1=very well/like native), health insurance coverage (0=no; 1=yes), and family history of HBV infection (0=no; 1=yes).
Statistical Analysis
Out of 877 participants, we included 726 people who had heard of HBV from any source. Those who had not heard of HBV were excluded from further analysis (n=151). Subsequent bivariate analyses examined the association between the type of information sources, age, ethnicity, educational attainment, English proficiency, and screening behavior. We conducted a path analysis among the five information sources, HBM constructs, knowledge about HBV transmission mode, and self-reported HBV screening, controlling for the potential confounders. We used Stata version 11.2 and its binary mediation command for data analysis [26]. Stata binary mediation command calculated unstandardized linear regression coefficients between the information sources and HBM constructs and the knowledge of HBV transmission modes, and unstandardized logit regression coefficients between the mediators and the outcome. The logit coefficients were exponentiated to calculate odds ratios for undergoing the screening. Total, direct, and indirect effects were computed by standardizing the coefficients, accounting for differences in scales [26]. The confidence interval for these effects was estimated using bootstrapping with 500 replications [26]. Initial data analysis indicated that within-cluster correlation on HBV screening was minimal (rho=0.01). Therefore, the path analysis did not account for the within-cluster correlation.
Results
The average age of respondents who had heard of HBV was 44.7 years; 42.6% were males; over 50% were college graduates or had more than college education. One third of the respondents reported that their English was poor. Approximately 60% of the respondents had health insurance. On average, respondents reported that they had heard of HBV from 3 different information sources. The basic characteristics of respondents who said they had heard of HBV are presented in Table I.
Table I.
Characteristics of study participants subject to the analysis (n = 726)
| Age (mean ± SD), range | 44.71 ± 13.08, 18 ~ 81 | |
| Sex | ||
| Male | 309 | 42.6% |
| Female | 417 | 57.4% |
| Ethnicity | ||
| Korean | 250 | 34.4% |
| Chinese | 255 | 35.1% |
| Vietnamese | 221 | 30.4% |
| Foreign born | ||
| Yes | 702 | 96.7% |
| No (born in the U.S.) | 24 | 3.3% |
| The proportion of life in U.S. | ||
| >25% | 430 | 59.2% |
| 25% or <25% | 296 | 40.8% |
| Education | ||
| College graduate and plus | 423 | 58.3% |
| No college graduate | 303 | 41.7% |
| English proficiency | ||
| Well | 253 | 34.9% |
| So-so/poor | 472 | 65.1% |
| Employment | ||
| Employed | 449 | 62.0% |
| Unemployed | 275 | 38.0% |
| Health insurance coverage | ||
| Yes | 492 | 67.8% |
| No | 234 | 32.2% |
| Have a regular physician | ||
| Yes | 436 | 60.1% |
| No | 289 | 39.9% |
| Family history of HBV infection | ||
| Yes | 119 | 16.4% |
| No | 607 | 83.6% |
|
Number of information sources on HBV (mean ± SD), range |
3.17 ± 2.90, 0 ~ 12 | |
The percentages of respondents who reported that they had heard of HBV from various information sources are presented in Table II. The most common sources of information—identified by a multiple-answer question—were newspapers (39.8%), physicians (39.3%), friends (33.8%), TV (31.7%), and the Internet (29.5%). Approximately 80% of respondents heard of HBV from at least one of these top five sources. Therefore, we focused our analyses on only these top five information sources as independent variables. For Vietnamese respondents, community health fairs were the third most popular source of HBV information, which was not included in these top five sources.
Table II.
Self-reported sources of HBV information, by a multiple-answer question
| Self-reported sources of HBV information |
All respondents (n=726) |
Korean (n=250) |
Chinese (n=255) |
Vietnamese (n=221) |
|---|---|---|---|---|
| 1 Newspapers | 39.8% | 30.4% | 47.8% | 41.2% |
| 2 Physicians | 39.3% | 34.4% | 36.8% | 47.5% |
| 3 Friends | 33.8% | 28.4% | 39.2% | 33.5% |
| 4 TV | 31.7% | 27.6% | 34.5% | 33.0% |
| 5 Internet | 29.5% | 19.6% | 38.4% | 30.3% |
| 6 Books | 24.1% | 12.0% | 34.9% | 25.3% |
| 7 Other health care providers | 22.6% | 14.0% | 23.9% | 30.8% |
| 8 Family | 22.3% | 14.4% | 29.8% | 22.6% |
| 9 Magazines | 20.4% | 12.4% | 27.8% | 20.8% |
| 10 Community health fairs | 20.4% | 4.4% | 22.3% | 36.2% |
Note: Percentages do not add to 100% because respondents were allowed to choose multiple answers.
Bivariate analyses of HBV screening, information sources, and psychosocial measures
Ethnicity, educational level, English proficiency, and age were associated with where respondents heard of HBV. There are significant differences in common sources of HBV information among Asian subgroups. A higher percentage of Vietnamese respondents (47.5%) than other subgroups (p < 0.001) had heard about HBV from physicians. A higher percentage of Chinese had learned about HBV from newspapers (47.8%), the Internet (38.4%), and friends (39.2%) than other subgroups (p < 0.001 for newspapers and the Internet, p < 0.05 for friends).
There were significant associations between identification of the Internet and newspapers as the information source and their educational level. Respondents with college degrees (35.5%) identified the Internet as their source, compared to 21.1% among those without college degree (p < 0.001). Respondents without college degree (45.4%) were more likely to report newspapers as their source than respondents with college degree (35.7%) (p < 0.01). There were no significant associations between educational levels and learning about HBV from physicians, TV, or friends.
TV and newspapers were more common sources of learning about HBV among those who were not proficient in English. Respondents with less English proficiency said that TV (35.6%) and newspapers (46.0%) were their main sources, whereas those with good English proficiency reported less use of those as information sources (24.5% and 28.1%, respectively; p < 0.001).
Age was another determinant for where respondents heard of HBV. Among age groups 18–39, 40–59, and ≥ 60 years, there were no differences in learning from physicians or friends. On the other hand, older respondents were more likely to report that they learned about HBV from traditional media such as newspapers or TV (p < 0.001). And a larger proportion of young respondents reported that they learned from the Internet (p < 0.01).
Bivariate analyses between the information sources and screening behavior showed that only learning HBV from physicians was significantly associated with screening behavior (OR: 2.98, 95% CI: 2.17, 4.08). Ethnic-specific bivariate analysis also showed that only having a physician as the source was significantly associated with the screening behavior (Table not shown).
Path analysis
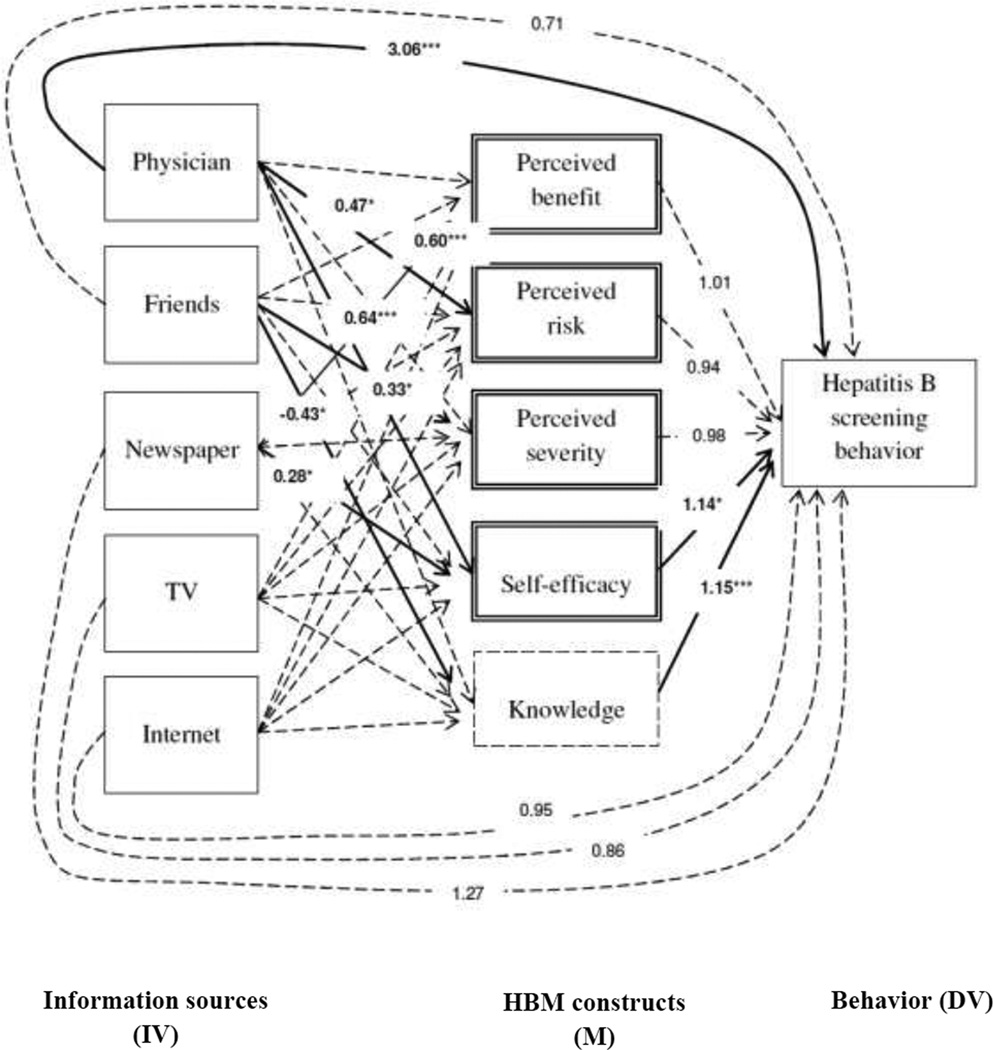
The overall results of the path analysis model that was developed based on the HBM are shown in Figure 1. The model controlled for the potential confounders. The associations between the information sources (IV) and HBM variables and knowledge (M) are shown in regression coefficients. On the other hand, the association between the mediators and HBV screening behavior (DV) and the associations between IV and DV are shown in odds ratio (OR).
Figure 1. Path Analysis Model of HBV Screening with HBM Variables and Information Sources.
Note: The associations between IV and DV, M and DV are shown in odds ratios. On the other hand, the associations between IV and M are shown in linear regression coefficients. Due to the lack of space, only significant linear regression coefficients are shown here. Table 3 has all of the linear regression coefficients between IV and M, regardless of their significance. The significant associations are shown in solid lines; whereas insignificant associations are shown in dotted lines.
The Path analysis model included the following as control variables: age, sex, educational level, English proficiency, proportion of life in the U.S., health insurance coverage, and family history of HBV infection. Among these control variables, having a college education or above and living less than a quarter of life in the U.S. were associated with completing hepatitis B screening.
* p<0.05, ** p<0.01, *** p<0.001
Among the five information sources, only physician, friends, and newspapers had significant associations with some mediators (see Table III). Having a physician as an information source was associated with a higher level of perceived risk (β=0.47, p < 0.05) and higher level of self-efficacy (β=0.64, p < 0.001). Having friends as the information source was associated with a higher level of perceived severity (β= 0.33, p < 0.05), but with a lower level of the knowledge (β= −0.43, p < 0.05). Leaning HBV from newspapers was positively associated with perceived benefits (β=0.60, p < 0.001) and self-efficacy (β= 0.28, p < 0.05).
Table III.
Associations between Information Sources and HBM Variables and Knowledge Score, All Ethnicities, n=726
| Self-reported sources of HBV information |
Perceived benefit |
Perceived risk | Perceived severity |
Self-efficacy | Knowledge of HBV transmission modes |
|---|---|---|---|---|---|
| Range of score | 1~7 | 1~10 | 1~7 | 1~7 | 1~10 |
| M (SD) | 5.29 (1.88) | 3.35 (2.61) | 4.72 (1.61) | 5.05 (1.59) | 4.77 (2.40) |
| 1 Physician | 0.11 | 0.47* | −0.18 | 0.64*** | 0.33 |
| 2 Friends | −0.15 | 0.21 | 0.33* | −0.11 | −0.43* |
| 3 Newspaper | 0.60*** | −0.44 | 0.14 | 0.28* | 0.35 |
| 4 TV | −0.12 | 0.08 | 0.15 | −0.10 | −0.28 |
| 5 Internet | −0.31 | −0.33 | −0.02 | −0.22 | 0.40 |
| Control variables | |||||
| Age | −0.005 | 0.006 | 0.01 | 0.008 | −0.02*** |
| Female | −0.01 | 0.79*** | −0.09 | −0.18 | −0.07 |
| College graduate or above |
0.13 | −0.36** | −0.005 | −0.17* | 0.31** |
| Proficient in English |
0.51** | −0.22 | 0.14 | 0.55*** | 0.66** |
| >25% of life in U.S. | −0.29 | 0.08 | 0.06 | −0.11 | −0.42* |
| Have health insurance coverage |
0.29 | −0.18 | 0.19 | 0.09 | 0.13 |
| Family history of HBV infection |
−0.02 | 0.85*** | −0.50** | 0.54*** | 1.02*** |
p<0.05,
p<0.01,
p<0.001
Among four HBM variables and the knowledge score, only self-efficacy and knowledge score had significant associations with screening behavior (OR: 1.14, 95% CI: 1.02, 1.28; OR: 1.15, 95% CI: 1.07, 1.24, respectively; see Table IV). The direct effect of physicians was strong (OR: 3.05, 95% CI: 2.13, 4.42). The standardized total, direct, and indirect effects of the five information sources on the screening behavior are shown in Table V. Among the five sources, learning HBV from friends had marginally significant indirect effects.
Table IV.
Odds Ratios of HBV Screening with HBM variables, Knowledge Score on HBV transmission modes and Sources of Information, All Ethnicities, n=726
| Variables | Unadjusted Odds Ratio |
95% CI | Odds Ratio in Path Analysis Model |
95% CI |
|---|---|---|---|---|
| Source of HBV information | ||||
| Physician | 2.98*** | 2.32, 4.11 | 3.06*** | 2.13, 4.42 |
| Friends or acquaintances | 0.77 | 0.57, 1.05 | 0.71 | 0.49, 1.03 |
| Newspaper | 1.23 | 0.92, 1.67 | 1.27 | 0.85, 1.90 |
| TV | 1.10 | 0.80, 1.51 | 0.86 | 0.57, 1.32 |
| Internet | 1.25 | 0.91, 1.72 | 0.95 | 0.63, 1.43 |
| Mediators | ||||
| Perceived benefit | 1.01 | 0.92, 1.11 | ||
| Perceived risk | 0.94 | 0.88, 1.01 | ||
| Perceived severity | 0.98 | 0.88, 1.09 | ||
| Self-efficacy | 1.14* | 1.02, 1.28 | ||
| Knowledge on transmission modes | 1.15*** | 1.07, 1.24 | ||
| Control variables | ||||
| Age | 1.01* | 1.00, 1.03 | ||
| Sex | ||||
| Male | 1.00 | |||
| Female | 1.25 | 0.89, 1.76 | ||
| Educational level | ||||
| Less than college graduate | 1.00 | |||
| College graduate and plus | 1.36** | 1.11, 1.65 | ||
| English proficiency | ||||
| Poor/so-so | 1.00 | |||
| Well | 1.04 | 0.68, 1.58 | ||
| Proportion of life in U.S. | ||||
| 25% or <25% | 1.00 | |||
| >25% | 0.42*** | 0.29, 0.62 | ||
| Health insurance coverage | ||||
| No | 1.00 | |||
| Yes | 1.18 | 0.80, 1.74 | ||
| Family history of HBV infection | ||||
| No | 1.00 | |||
| Yes | 1.69* | 1.04, 2.73 |
p<0.05,
p<0.01,
p<0.001
Table V.
Standardized total effect, direct effect, and indirect effect, and bias correct confidence interval, Total respondents, n=726
| Total effect | Direct effect | Indirect effect | |
|---|---|---|---|
| Physician | 0.30§ [0.21, 0.38] | 0.28§ [0.19, 0.36] | 0.03 [−0.00∞, 0.06] |
| Friends | −0.11§ [−0.20, −0.02] | −0.09§ [−0.18, 0.01] | −0.02§ [−0.05, −0.00∞] |
| Newspaper | 0.09 [−0.00∞, 0.20] | 0.06 [−0.05, 0.18] | 0.03 [−0.00∞, 0.06] |
| TV | −0.05 [−0.16, 0.06] | −0.04 [−0.14, 0.07] | −0.02 [−0.04, 0.00∞] |
| Internet | −0.00∞ [−0.10, 0.09] | −0.01 [−0.11, 0.08] | 0.01 [−0.01, 0.03] |
Note: Path analysis model included the following as control variables: age, sex, educational level, English proficiency, proportion of life in the U.S., health insurance coverage, and family history of hepatitis B infection. 95% confidence interval range is shown in the brackets.
Statistical significant standardized effects are marked with §.
∞ indicates that the value is very close to zero, but not zero. In such a case, the statistical significance of effects needs to be interpreted with caution.
We also conducted ethnic-specific path analyses (Table not shown1). In the Korean group, physician, friends, newspapers, and the Internet had significant associations with the mediators: physician with self-efficacy (β=0.70, p < 0.001), friends with perceived benefits (β= −0.53, p < 0.05), newspaper with knowledge (β=0.75, p < 0.05), and the Internet with perceived benefits (β= −0.82, p < 0.05). Knowledge of HBV transmission modes had significant associations with screening behavior (OR=1.16, 95% CI: 1.01, 1.32). Only newspapers had significant mediated effect (0.06).
In the Chinese group-specific path analysis, physician, friends, and the Internet had significant associations with the mediators: physician with self-efficacy (β= 0.78, p<0.001) and with knowledge of HBV transmission modes (β= 0.71, p<0.05); friends with the knowledge (β=−1.01, p < 0.001); and the Internet with the knowledge (β= 0.76, p < 0.05). Self-efficacy and knowledge had significant associations with screening behavior (self-efficacy: OR=1.29, 95%CI: 1.03, 1.62; and knowledge OR =1.21, 95%CI: 1.04, 1.41). Physicians and friends had significant indirect effects (0.10 and −0.08, respectively).
In the Vietnamese group-specific path analysis, none of the information sources had significant associations with the mediators. Moreover, none of the mediators was significantly associated with screening behavior. Thus, none of the information sources had significant mediation effects. Across the three ethnic groups, physicians had a strong direct effect on the screening.
Discussion
Our study identified that physicians, friends, newspapers, TV, and the Internet were the most common sources of learning about HBV. There were variations in the type of information sources identified by respondents from different ethnic backgrounds and from other demographic backgrounds.
The overall path analysis showed that learning HBV from physicians, friends, and newspapers had significant associations with several mediators, after controlling for the potential confounders. However, only the path from friends, the knowledge of HBV transmission modes, to screening behavior turned out to be marginally significant. On the other hand, the influence of learning about HBV from physicians on the screening behavior was not mediated by any of the mediators in the model and physicians had the strongest direct effects on the screening behavior. Newspapers did not have significant direct effects or mediation effects. Contrary to initial expectations, perceived benefit, risk, and severity did not play a great role in mediating effects. Learning HBV from physicians, friends, or newspapers had some association with these HBM-specific constructs; however, the constructs were not associated with the screening behavior. Thus, mediating effects by these constructs were overall insignificant. Self-efficacy and the knowledge of HBV transmission modes were important factors for HBV screening. This is somewhat contrary to the previous study of Vietnamese immigrants in the East Coast that found that perceived risk was associated with screening [14]. Differences in study participants and HBM measures could explain these differences; however, both studies indicated that perceived ability to overcome barriers is pivotal for completion of the screening. Future studies should further explore roles of perceived benefit, risk, and severity in HBV screening among AIs.
Ethnicity-specific path analyses also confirmed that physicians had strong and direct effects on the screening behavior. There was generally a similar pattern of mediation paths among total respondents, and among Korean and Chinese respondents; however, mediation effects were greater among Chinese respondents. Vietnamese respondents exhibited no mediation effect. These differences could be explained by variations in the quality of physician-provider communication, individual’s information-seeking behaviors, perceived credibility of information sources, and message contents disseminated through the information sources to specific ethnic groups. Our study suggests that a physician-based approach would be an effective model. How effectively physicians communicate HBV transmission modes, and severity of HBV infection, however, remain suboptimal.
Because many respondents identified other information sources as their source of learning about HBV, there is room for improving self-efficacy for completing the screening and knowledge of HBV transmission modes through these information sources. Community-level public health campaigns can certainly take advantage of using mass media (ethnic TV and newspapers), interpersonal communications with friends, and Internet to disseminate HBV information. Community-level public health campaigns would be an important alternative to target individuals without regular access to care who do not benefit from a physician-based approach for promoting HBV screening. Our knowledge of the information sources commonly accessed by individuals with different sociodemographic backgrounds will also help practitioners tailor effective campaigns.
There are four limitations in our study. First, although the study was a cluster randomized trial, self-selection for participating in the study might have caused selection bias. The findings of our analyses may be limited to Program participants. Second, our study had to rely on self-reported HBV screening behavior because the Program did not collect medical records to verify self-reported behavior. Self-reported behaviors are subject to social desirability and other biases. Third, the path analysis with cross-sectional data may give biased results because it is difficult to establish temporal order of events [27]. Forth, the question related to whether they had ever heard of HBV was not specific to preventive measures or screening behaviors [28]. This might have made it difficult for some respondents to recall their experiences or to make clear connections with that question.
This study provides useful insights on how information sources, psychosocial mediators, and screening behaviors are associated in the theoretical framework. To the best of our knowledge, this study is the first to examine the influence of information sources on HBV screening behavior among AIs [28]. In addition, we applied a behavioral theoretical framework to analyze the associations between information sources and screening behavior. We also employed path analysis to assess what individuals learn from common information sources and how they relate to HBV screening behavior. This novel approach helped us build our knowledge base for designing a national campaign on HBV which the U.S. Department of Health and Human Services (DHHS) plans to launch in 2012 and 2013 [29].
Acknowledgements
We would like to thank the participants in the study. We appreciate our research assistants’ dedicated efforts to collect data from the participants. This study was supported by the National Cancer Institute, Award Number R25CA129042. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Cancer Institute or the National Institutes of Health.
Footnotes
Tables of ethnicity-specific analyses are not shown in the manuscript. They are available upon request from the corresponding author.
References
- 1.U.S. Census Bureau. American FactFinder. 2011 Retrieved May 31, 2011, from http://factfinder2.census.gov/faces/nav/jsf/pages/index.xhtml.
- 2.U.S. Census Bureau. U.S. Census Bureau's presentation on Asian American, Native Hawaiian and Pacific Islander data. Paper presented at the White House Initiative on Asian Americans and Pacific Islanders. George Washington University: Asian American, Native Hawaiian and Pacific Islander Research and Data Convening; 2010. Dec 10, 2010). [Google Scholar]
- 3.Hutton DW, Tan D, So SK, Brandeau ML. Cost-effectiveness of screening and vaccinating Asian and Pacific Islander Adults for Hepatitis B. Annals of Internal Medicien. 2007;147(7):460–469. doi: 10.7326/0003-4819-147-7-200710020-00004. [DOI] [PubMed] [Google Scholar]
- 4.National Cancer Institute [NCI] SEER Cancer Statistics Review 2002–2006. U.S. and SEER Death Rates by Primary Cancer Site and Race/Ethnicity, 2002–2006. Table 1.20. 2010 Retrieved June 22, 2010, from http://seer.cancer.gov/csr/1975_2006/results_single/sect_01_table.20_2pgs.pdf.
- 5.McMahon BJ. The natural history of chronic hepatitis B virus infection. Hepatology. 2009;49(5 Suppl):S45–S55. doi: 10.1002/hep.22898. [DOI] [PubMed] [Google Scholar]
- 6.Institute of Medicine [IOM] Hepatitis and liver cancer : a national strategy for prevention and control of hepatitis B and C. Washington, DC: National Academies Press; 2010. [PubMed] [Google Scholar]
- 7.Ma GX, Shive SE, Toubbeh JI, Tan Y, Wu D. Knowledge, attitudes, and behaviors of Chinese hepatitis B screening and vaccination. Am J Health Behav. 2008;32(2):178–187. doi: 10.5555/ajhb.2008.32.2.178. [DOI] [PubMed] [Google Scholar]
- 8.Taylor VM, Choe JH, Yasui Y, Li L, Burke N, Jackson JC. Hepatitis B awareness, testing, and knowledge among Vietnamese American men and women. J Community Health. 2005;30(6):477–490. doi: 10.1007/s10900-005-7282-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Thompson MJ, Taylor VM, Jackson JC, Yasui Y, Kuniyuki A, Tu SP. Hepatitis B knowledge and practices among Chinese American women in Seattle, Washington. J Cancer Educ. 2002;17(4):222–226. doi: 10.1080/08858190209528842. [DOI] [PubMed] [Google Scholar]
- 10.Wu CA, Lin SY, So SK, Chang ET. Hepatitis B and liver cancer knowledge and preventive practices among Asian Americans in the San Francisco Bay Area, California. Asian Pac J Cancer Prev. 2007;8(1):127–134. [PubMed] [Google Scholar]
- 11.Hu KQ. Hepatitis B virus (HBV) infection in Asian and Pacific Islander Americans (APIAs): how can we do better for this special population? Am J Gastroenterol. 2008;103(7):1824–1833. doi: 10.1111/j.1572-0241.2008.01878.x. [DOI] [PubMed] [Google Scholar]
- 12.Ma GX, Shive SE, Fang CY, Feng Z, Parameswaran L, Pham A. Knowledge, attitudes, and behaviors of hepatitis B screening and vaccination and liver cancer risks among Vietnamese Americans. J Health Care Poor Underserved. 2007;18(1):62–73. doi: 10.1353/hpu.2007.0013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hwang JP, Roundtree AK, Suarez-Almazor ME. Attitudes Toward Hepatitis B Virus among Vietnamese, Chinese and Korean Americans in the Houston Area, Texas. J Community Health. 2012 doi: 10.1007/s10900-012-9543-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ma GX, Fang CY, Shive SE, Toubbeh J, Tan Y, Siu P. Risk perceptions and barriers to Hepatitis B screening and vaccination among Vietnamese immigrants. J Immigr Minor Health. 2007;9(3):213–220. doi: 10.1007/s10903-006-9028-4. [DOI] [PubMed] [Google Scholar]
- 15.Geana MV, Kimminau KS, Greiner KA. Sources of Health Information in a Multiethnic, Underserved, Urban Community: Does Ethnicity Matter? J Health Commun. 2011:1–12. doi: 10.1080/10810730.2011.551992. [DOI] [PubMed] [Google Scholar]
- 16.Meissner HI, Potosky AL, Convissor R. How sources of health information relate to knowledge and use of cancer screening exams. J Community Health. 1992;17(3):153–165. doi: 10.1007/BF01324404. [DOI] [PubMed] [Google Scholar]
- 17.Seematter-Bagnoud L, Santos-Eggimann B. Sources and level of information about health issues and preventive services among young-old persons in Switzerland. Int J Public Health. 2007;52(5):313–316. doi: 10.1007/s00038-007-6086-x. [DOI] [PubMed] [Google Scholar]
- 18.Lewallen LP. Healthy Behaviors and Sources of Health Information Among Low- Income Pregnant Women. Public Health Nursing. 2004;21(3):200–206. doi: 10.1111/j.0737-1209.2004.021302.x. [DOI] [PubMed] [Google Scholar]
- 19.Oh KM, Kreps GL, Jun J, Ramsey L. Cancer information seeking and awareness of cancer information sources among Korean Americans. J Cancer Educ. 2011;26(2):355–364. doi: 10.1007/s13187-010-0191-x. [DOI] [PubMed] [Google Scholar]
- 20.Oliver JS, Grindel CG, DeCoster J, Ford CD, Martin MY. Benefits, barriers, sources of influence, and prostate cancer screening among rural men. Public Health Nurs. 2011;28(6):515–522. doi: 10.1111/j.1525-1446.2011.00956.x. [DOI] [PubMed] [Google Scholar]
- 21.Bass SB, Ruzek SB, Gordon TF, Fleisher L, McKeown-Conn N, Moore D. Relationship of Internet health information use with patient behavior and self-efficacy: experiences of newly diagnosed cancer patients who contact the National Cancer Institute's Cancer Information Service. J Health Commun. 2006;11(2):219–236. doi: 10.1080/10810730500526794. [DOI] [PubMed] [Google Scholar]
- 22.Hsu CE, Liu LC, Juon HS, Chiu YW, Bawa J, Tillman U. Reducing liver cancer disparities: a community-based hepatitis-B prevention program for Asian-American communities. J Natl Med Assoc. 2007;99(8):900–907. [PMC free article] [PubMed] [Google Scholar]
- 23.Chen L, Juon HS, Lee S. Acculturation and BMI Among Chinese, Korean and Vietnamese Adults. J Community Health. 2011 doi: 10.1007/s10900-011-9476-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.National Cancer Institute. Health Information National Trends Survey 2005. 2005 Retrieved September 7, 2009, from http://hints.cancer.gov/docs/HINTS_2005_Instrument-English.pdf.
- 25.Taylor VM, Jackson JC, Chan N, Kuniyuki A, Yasui Y. Hepatitis B knowledge and practices among Cambodian American women in Seattle, Washington. J Community Health. 2002;27(3):151–163. doi: 10.1023/a:1015229405765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ender PB. Binary_mediation: command to compute binary mediation. UCLA: Academic Technology Services, Statistical Consulting Group; 2011. Retrieved July 4, 2012, from http://www.ats.ucla.edu/stat/stata/ado/analysis/ [Google Scholar]
- 27.Maxwell SE, Cole DA. Bias in Cross-Sectional Analyses of Longitudinal Mediation. Psychological Methods. 2007;12(1):23–44. doi: 10.1037/1082-989X.12.1.23. [DOI] [PubMed] [Google Scholar]
- 28.Takahashi LM, Kim AJ, Sablan-Santos L, Quitugua LF, Aromin J, Lepule J. Hepatitis B among Pacific Islanders in Southern California: how is health information associated with screening and vaccination? J Community Health. 2011;36(1):47–55. doi: 10.1007/s10900-010-9285-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.U.S. Department of Health and Human Services. Combating the Silent Epidemic of Viral Hepatitis: Action Plan for the Prevention, Care and Treatment of Viral Hepatitis. 2011 Retrieved from http://www.hhs.gov/ash/initiatives/hepatitis.