Abstract
Background
Public access defibrillation with automated external defibrillators (AEDs) can improve survival from out-of-hospital cardiac arrests (OHCA) occurring in public. Increasing the effective range of AEDs may improve coverage for public location OHCAs.
Objective
To quantify the relationship between AED effective range and public location cardiac arrest coverage.
Methods
This was a retrospective cohort study using the Resuscitation Outcomes Consortium Epistry database. We included all public-location, atraumatic, EMS-attended OHCAs in Toronto, Canada between Dec. 16, 2005 and July 15, 2010. We ran a mathematical model for AED placement that maximizes coverage of historical public OHCAs given pre-specified values of AED effective range and the number of locations to place AEDs. Locations of all non-residential buildings were obtained from the City of Toronto and used as candidate sites for AED placement. Coverage was evaluated for range values from 10 to 300 meters and number of AED locations from 10 to 200, both in increments of 10, for a total of 600 unique scenarios. Coverage from placing AEDs in all public buildings was also measured.
Results
There were 1,310 public location OHCAs during the study period, with 25,851 non-residential buildings identified as candidate sites for AED placement. Cardiac arrest coverage increased with AED effective range, with improvements in coverage diminishing at higher ranges. For example, for a deployment of 200 AED locations, increasing effective range from 100m to 200m covered an additional 15% of cardiac arrests, whereas increasing range further from 200m to 300m covered an additional 10%. Placing an AED in each of the 25,851 public buildings resulted in coverage of 50% and 95% under assumed effective ranges of 50m and 300m, respectively.
Conclusion
Increasing AED effective range can improve cardiac arrest coverage. Mathematical models can help evaluate the potential impact of initiatives which increase AED range.
1 INTRODUCTION
Out-of-hospital cardiac arrest (OHCA) is responsible for 300,000 deaths annually in North America, making it a leading cause of death and a significant public health issue [1]. Only 5–10% of OHCA patients survive to hospital discharge [2,3].
Early defibrillation can increase the probability of survival for patients with ventricular fibrillation or pulseless ventricular tachycardia[4–6]. However, the benefit of treatment is very time-sensitive. Every minute of delay in cardiopulmonary resuscitation and defibrillation following cardiac arrest can substantially decrease a patient’s chance of survival [7]. Automated external defibrillators (AEDs) can be deployed in public locations to allow bystanders to serve as lay rescuers and administer defibrillatory shocks prior to the arrival of emergency medical service (EMS) responders. Despite evidence to support a survival advantage associated with public access defibrillation programs [8], AEDs are underused. Bystander AED use is observed in less than 3% of all cases of out-of-hospital cardiac arrest episodes [2].
The reasons for this low usage rate are not entirely understood. Possible factors include a lack of bystander awareness, training or willingness to use an AED in an emergency situation. Some bystanders may be willing to use an AED, but are unaware of the location of nearby AEDs at the time of an emergency. Even when the location of an AED is known, there may be visibility and accessibility issues (e.g. AED behind a locked door) that impede timely retrieval. If the time required to retrieve and use an AED exceeds the arrival time of emergency medical service (EMS) responders, the public access defibrillator might not be used.
All of these potential barriers to AED usage can be viewed as influencing the “effective range” of the AED. We assert that each public access defibrillator has a theoretical effective range, which we define, for the purposes of this analysis, as the maximum straight-line distance between the AED and a cardiac arrest such that there is a reasonable probability of retrieval and use prior to EMS arrival.
If an AED is not registered with local EMS authorities and stored in a discreet location with poor visibility and limited access, we would expect the effective range for this AED to be small. That is, we would expect it to be useful only for cardiac arrests in very close proximity to the AED, where bystanders might have it in their line of sight. Conversely, if an AED is registered with local EMS, positioned well, accompanied by signage so that it can be easily seen from a distance and associated with an internal first response plan so that several regular users of the building know where it is, we would expect to have a larger effective range.
Although the theoretical nature of AED effective range makes it difficult to calculate precisely, determining the association between effective range and coverage of cardiac arrests in a community is an important analysis. For example, if a health services intervention increases the effective range of every AED in the community by 100 meters, what is the impact on cardiac arrest coverage? This knowledge may contribute to a better understanding of how various interventions aiming to increase effective range may impact the overall effectiveness of public access defibrillation -- for example, smartphone applications or signs which direct bystanders to the location of AEDs are two such interventions which may increase effective range. Therefore, we undertook this analysis to characterize the association between public access defibrillator effective range and cardiac arrest coverage. We use historical cardiac arrest locations, city planning data and an AED registry from Toronto, Canada to conduct this analysis.
2 METHODS
2.1 Study setting
The City of Toronto is Canada’s largest city and the fifth most populous city in North America. It has over 2.7 million inhabitants[9]. A single EMS serves the entire city, though neighbouring EMS will occasionally respond to emergencies in Toronto. A tiered response system is used for dispatching EMS and fire fighting units for medical emergencies, with cardiac arrest belonging to the highest priority category.
Study design
We conducted a retrospective analysis of a population-based out-of-hospital cardiac arrest registry. We used data from the Resuscitation Outcomes Consortium (ROC) Epistry Cardiac Arrest database [10].
Selection of cardiac arrest episodes
We included consecutive public location, non-traumatic, EMS-attended OHCA episodes in the City of Toronto captured by the Toronto coordinating centre of ROC between December 16, 2005 and July 15, 2010. Patients were identified as having OHCA if they were evaluated by EMS personnel and had attempts at external defibrillation by lay responders or EMS personnel, chest compressions by EMS personnel, or were pulseless and did not receive CPR or attempts to defibrillate[10]. “Public locations” were defined as all areas that were not private dwellings. For instance, we included cardiac arrests occurring in public transportation buildings, commercial, civic and industrial sites, hotels, hostels, schools, public spaces and recreational areas, but did not include episodes occurring in single family homes, apartments, nursing homes or retirement residences. “Non-traumatic” was defined as any cardiac arrest not caused by obvious blunt or penetrating trauma or burns. Episodes occurring in medical clinics were excluded. This study was approved by our institutional Research Ethics Board.
2.2 Data sources
Cardiac arrests
The ROC Epistry - Cardiac Arrest is a large, population-based prospective registry of consecutive, EMS-attended OHCAs from 11 Regional Coordinating Centers across Canada and the United States of America. This study used data from the Toronto coordinating center only. Cardiac arrest locations are stored in Epistry as street addresses. We converted the data into the Universal Transverse Mercator coordinate format to perform our analysis.
Candidate sites for AED placement
Data from the City of Toronto Employment Survey (2009), administered by the City of Toronto’s Planning Division, was used to identify potential locations for public access defibrillator placement [11]. The Toronto Employment Survey is a tool used by the City of Toronto Planning Division to monitor progress of planning policies and the City’s economic health. This survey has been used as a data source to characterize urban infrastructure in other published epidemiologic analyses, for example, exploring neighborhood environments and resources for healthy living in patients with diabetes[12].
Data in the Toronto Employment Survey is updated annually by a team of trained surveyors, and includes the geographic location of all non-residential buildings in Toronto. In our analysis, we consider each of these buildings as a candidate site for placing a public access defibrillator.
2.3 Analysis of cardiac arrest coverage potential
The primary outcome for this analysis was the cardiac arrest “coverage potential” for various hypothetical deployments of AEDs in Toronto. We define “coverage” for a particular deployment as the percentage of historical public OHCAs within the effective range of at least one AED. For instance, if the effective range of an AED is assumed to be 100m, then we deem any cardiac arrest within a 100m radius of the AED’s location as being “covered” by that AED. The coverage provided by a set of AEDs deployed in a community will vary depending on where they are placed. Therefore, we focused on determining the maximum coverage possible, which we refer to as coverage potential, for a given effective range and number of AED locations. This allowed us to consistently compare the best-case coverage across all 600 combinations of effective range and number of AEDs.
To determine coverage potential, we used a mathematical model for AED placement based on the Maximal Covering Location Problem (MCLP) [13]. This model is designed to determine the maximum cardiac arrest coverage possible for a given number of AEDs and their effective ranges. The MCLP model has been previously used to study other healthcare location problems [14,15]. The model requires two sets of data as input: the coordinates of historical cardiac arrest locations and the candidate sites for AED placement. For these two inputs, we used cardiac arrest episodes from Epistry and non-residential building locations from the Toronto Employment Survey, respectively.
The AED effective range and the number of AEDs to be deployed are parameters in the model. Values for effective range between 10m and 300m were tested in increments of 10 meters. At each assumed effective range, the number of locations in which AEDs are placed was adjusted between 10 and 200, also in increments of 10. This resulted in 600 (30 × 20) unique combinations of effective range and total AEDs being tested. For each of these 600 runs, the output of the model provided the resulting coverage potential along with the corresponding AED locations.
We also measured the coverage potential associated with placing an AED in every single non-residential building from the Toronto Employment Survey, again for effective ranges between 10 and 300m, in increments of 10m. This analysis did not require use of the mathematical model.
3 RESULTS
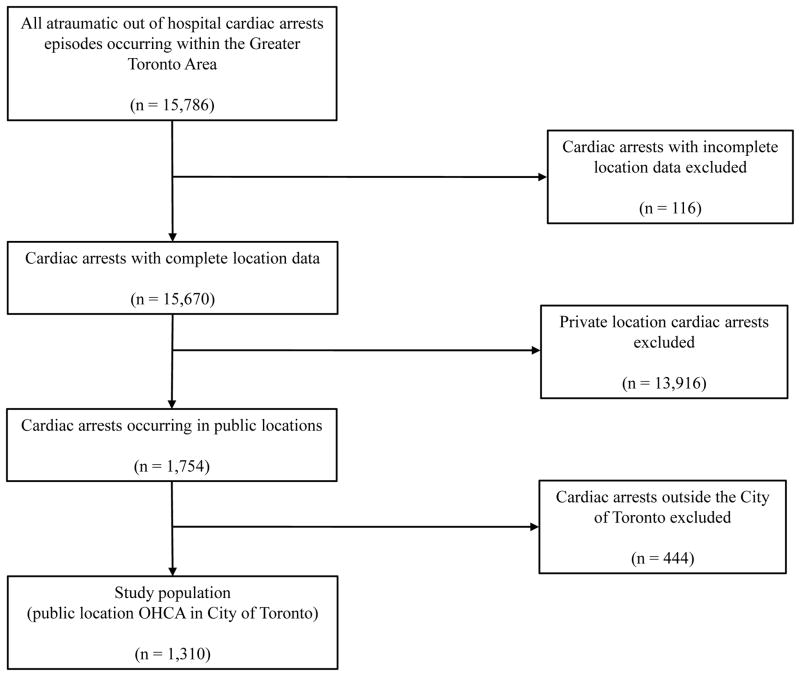
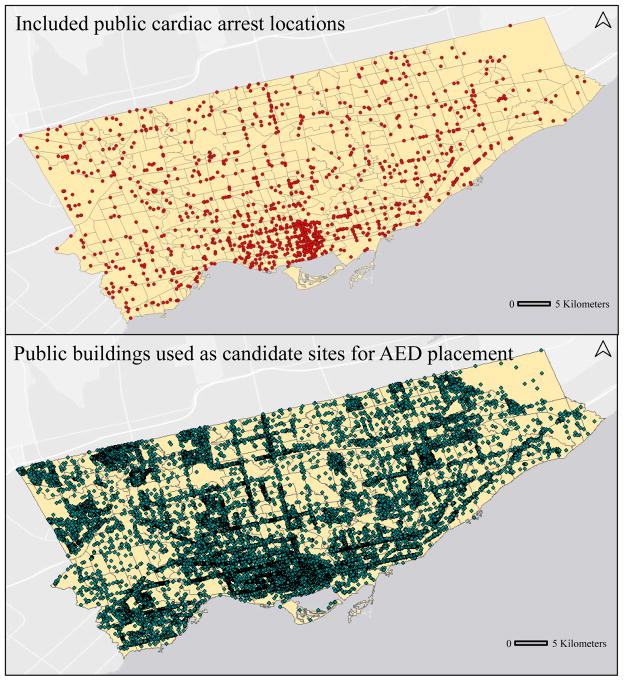
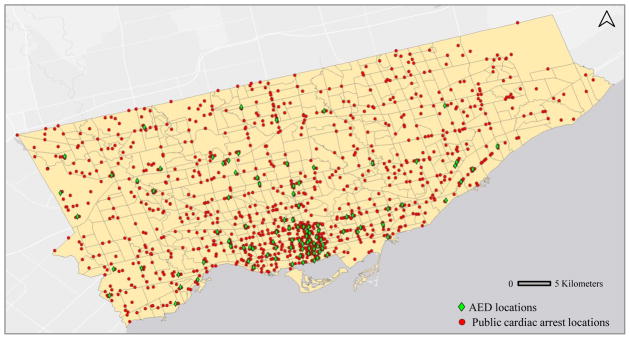
During the approximately 4.5 year study period, there were a total of 15,786 cardiac arrest episodes recorded in the Greater Toronto Area. After applying the inclusion/exclusion criteria (Figure 1), there were a total of 1,310 cardiac arrests that occurred in public locations, with 67% (876/1,310) occurring indoors and 33% (436/1,310) occurring outdoors. Demographic characteristics of these cardiac arrest episodes are described in Table 1. A total of 25,581 non-residential buildings were identified from the Toronto Employment Survey and were used as candidate sites for AED placement. The geographic locations of the included cardiac arrests and all candidate sites are shown in Figure 2.
Figure 1.
Inclusion/exclusion criteria for cardiac arrest episodes
Table 1.
Demographic Characteristics of Included Public Location Cardiac Arrests
| Characteristic | All included cardiac arrests (n = 1310) |
|---|---|
| Average age, y (±SD) | 59.4 ± 17.6 |
| Male | 59.1 ± 17.0 |
| Female | 60.8 ± 19.9 |
| Male sex, n (%)* | 1052 (80.3) |
| Witnessed by bystander, n (%)* | 582 (44.4) |
| Received bystander CPR, n (%)* | 499 (38.1) |
| Received bystander AED, n (%)* | 70 (5.3) |
| Average interval between 911 call to EMS vehicle arrival, median min [IQR]* | 5.7 [2.4] |
| Initial heart rhythm, n (%)*† | |
| Shockable | 421 (32.1) |
| Not shockable | 843 (64.4) |
| Survival to discharge* | 160 (12.2) |
Number of missing/not noted cases: Male sex (17), Witnessed by bystander (13), Received bystander CPR (32), Received bystander AED (76), Average interval between 911 call to EMS vehicle arrival (21), initial heart rhythm (46), Survival to discharge (4).
“Shockable” includes ventricular fibrillation, ventricular tachycardia and patients identified as “shockable” with an AED. “Not shockable” includes Pulseless electrical activity, asystole, and patients identified as “not shockable” by an AED, and patients where the initial rhythm was not obtained because resuscitation was ceased prior to rhythm analysis.
Figure 2.
Locations of included cardiac arrests from December 16, 2005 to July 15, 2010 (top) and candidate sites for AED placement (bottom)
3.1 Coverage potential for combinations of effective range and total AED locations
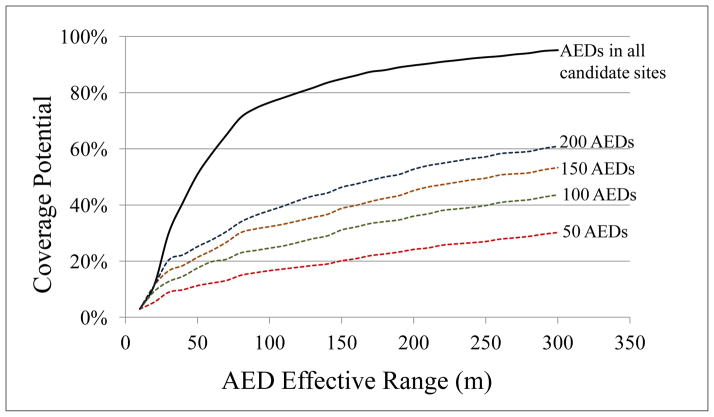
Figure 3 shows the coverage potential for all effective ranges tested, for deployments of 50, 100, 150 and 200 AEDs. In general, for a fixed quantity of AEDs, coverage potential increases as AED effective range increases, though this gain diminishes at higher values of effective range. An example of the model output is shown in Figure 4, for the case where 100 AEDs are optimally placed at an effective range of 100m. In this case, each AED covers at least two cardiac arrests.
Figure 3.
Coverage potential from placing AEDs in all 25,851 candidate sites in Toronto and coverage potential of 50, 100, 150 and 200 optimal AED locations
Figure 4.
Example model output showing historical cardiac arrests and optimal 100 AED locations for effective range of 100m
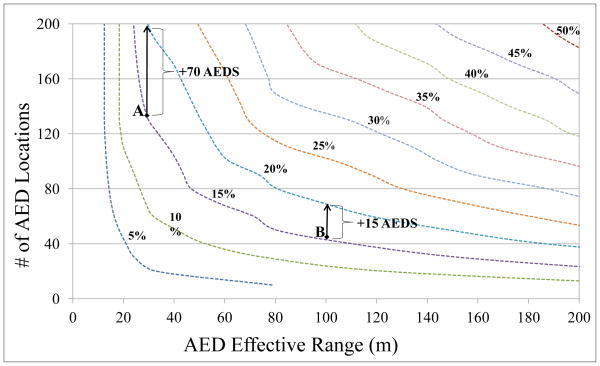
Figure 5 shows the combination of total AED locations and effective range required to achieve fixed coverage levels between 5% and 50%, in increments of 5%. Two points on the same curve represent the same coverage potential. For example, points A and B represent two deployment schemes that both achieve coverage of 15% of all historical public cardiac arrests, each under different combinations of radius and AED locations.
Figure 5.
Combinations of total AEDs and effective range required to achieve constant coverage potentials between 5% and 50%; points A and B show 70 and 15 additional AEDs are needed to increase coverage from 15% to 20%, respectively
3.2 Coverage potential from placing AEDs in all non-residential buildings
At an assumed effective range of 30m, placing an AED in each of the 25,851 candidate sites covers 29.9% of historical cardiac arrests. At 50m, coverage potential is 50.9%. In general, the coverage potential associated with placing an AED in all 25,851 candidate sites increases rapidly with effective range at low values (< 70m), but levels off quickly beyond 100m (Figure 3).
4 DISCUSSION
In the present study, we calculated the maximum cardiac arrest coverage attainable for various hypothetical deployments of public access defibrillators. To our knowledge, this is the first study to examine the sensitivity of cardiac arrest coverage to AED effective range. We examined the best-case coverage scenario for various combinations of AED effective range and total AED locations by using a mathematical model to optimize AED placement. We also quantified the cardiac arrest coverage resulting from placing an AED in every non-residential building in a large urban setting, at various assumed values of effective range.
4.1 Limitations
First, we designated all non-residential buildings as candidate sites for AED placement. In reality, some of these locations may not be suitable for placing AEDs. Second, we use straight-line distances in all measurements, which is not necessarily representative of the distance a lay rescuer would have to travel to retrieve an AED. Third, in our spatial analysis we used the UTM coordinate system to consider the location of a cardiac arrest in only two dimensions – data on the altitude of these cardiac arrest episodes was unavailable (for example, if a cardiac arrest had occurred in an office tower).
This was a retrospective cohort study, and did not attempt to identify the locations of future cardiac arrests. It should be noted, however, that the geographic distribution of cardiac arrests is not random, but rather determined by underlying epidemiological factors such as traffic flow and the demographic composition of the study region, which tend to be relatively stable over time [16]. As a result, we believe the data collected over the 4.5 years of this study reasonably reflect longer term geographic risk of cardiac arrest events within the study region. Several previous studies have interpreted historical cardiac arrest patterns as being representative of future cardiac arrest locations [16,17].
4.2 Main findings
Our results suggest that the benefit of increasing the number of locations in which AEDs are deployed depends on the effective range of the AEDs. If the effective range of each public access defibrillator in a community is low, then the deployment of even thousands of additional AEDs may still result in low cardiac arrest coverage, which may then lead to infrequent AED usage during OHCA. Notably, even in the extremely idealized and optimistic scenario where an AED is placed in each of the 25,851 non-residential buildings in Toronto, the closest AED would have still been more than 50m away in roughly half (49.1%) of the cardiac arrest episodes considered (Figure 3). This suggests that even a large supply of “short-range” AEDs (i.e., within a bystander’s line-of-sight) may be insufficient for covering most public location cardiac arrests. This result also highlights the reality that there are a finite number of suitable locations to place AEDs. This physical constraint may be mitigated by increasing the effective range of public access defibrillators. This would allow AEDs to provide coverage for nearby areas that may not suitable for direct AED placement, such as the outdoor locations where one-third of the cardiac arrests included in this study occurred. There may also be value in exploring whether AEDs can be placed in non-traditional places, for example, in bus shelters or at major road intersections.
Whether an AED can be successfully used in a cardiac arrest emergency depends in part on how quickly the AED can be transported to the site of the cardiac arrest by a bystander. As a result, technologies that reduce the retrieval time for an AED have the potential to increase its effective range. For example, an AED registry that allows EMS dispatchers to communicate the precise location of a nearby AED over the phone to a lay rescuer can save precious minutes during a cardiac arrest emergency. Smartphone applications that recruit lay rescuers in real-time to perform CPR have also been developed [19]. A similar GPS-based smartphone application that is linked to EMS systems could notify laypersons in close proximity of an AED that a cardiac arrest has occurred nearby. This could allow for AEDs to be transported to the victim in a one-way trip, relieving immediate bystanders from having to make a round-trip to retrieve a defibrillator, thereby potentially doubling the AED’s effective range.
For a fixed number of AEDs, the incremental improvement in coverage potential associated with expanding AED range diminishes as effective range increases (Figure 3). This may be a consequence of how cardiac arrest events are spatially distributed – once hotspots for cardiac arrest are covered by an AED, expanding the range of that AED yields diminishing returns on total coverage. Therefore, when AED effective range is already known to be relatively large, it may be more fruitful to deploy additional AEDs in uncovered areas rather than investing in expanding AED range.
Figure 5 shows that the benefit of increasing the number of AEDs increases with effective range. For example, points A and B in Figure 5 both mark AED deployment scenarios that achieve coverage potentials of 15%. At point A, where effective range is low (30m), increasing coverage potential to 20% requires 70 additional AEDs. At point B, where effective range is higher (100m), increasing coverage potential to 20% only requires 15 additional AEDs. This suggests that a small number of long-range AEDs may achieve the same improvement in coverage as a large number of short-range AEDs. The savings that would result from requiring fewer AEDs to achieve the same target cardiac arrest coverage could help to defray the costs of investing in technologies which increase the effective range of the AEDs. A more thorough economic assessment of increasing AED range may play an important role in deciding how to most cost-effectively improve cardiac arrest coverage, and could be the focus of future work.
Existing AEDs in Toronto were intentionally omitted from this study, since our objective was to quantify a theoretical relationship between AED effective range and cardiac arrest coverage. However, it may be beneficial to investigate the coverage resulting from existing AEDs in a future study.
Although AED effective range is a theoretical concept, this study demonstrates the importance of considering AED effective range in designing public access defibrillation strategies. Previous studies on public access defibrillation have focused on identifying the locations that have a high incidence of cardiac arrest [20,21]. These efforts should be complemented with further research into the effective range of public access defibrillators. Consideration of AED effective range may improve understanding of why the frequency of AED use in OHCA is low and what interventions may improve it.
5 CONCLUSION
The potential improvement in cardiac arrest coverage from adding AEDs in a community depends on the effective range of the AEDs. If effective range is small, cardiac arrest coverage may be low, regardless of how many AEDs are deployed. Health interventions which increase the effective range of AEDs may increase the number of cardiac arrest victims who receive bystander defibrillation, and may also lead to fewer AEDs being required to achieve desired coverage levels.
Acknowledgments
Sources of support
Auyon Siddiq was supported through an NSERC Canada Graduate Scholarship (Master’s) and an Ontario Graduate Scholarship (Master’s).
Dr. Brooks was supported through a Jumpstart Resuscitation Research Scholarship from the Heart and Stroke Foundation of Canada for his work on this manuscript. The Resuscitation Outcome Consortium (ROC) is supported by a series of cooperative agreements to 10 regional clinical centers and one data Coordinating Center (5U01 HL077863, HL077881, HL077871 HL077872, HL077866, HL077908, HL077867, HL077885, HL077885, HL077863) from the National Heart, Lung and Blood Institute in partnership with the National Institute of Neurological Disorders and Stroke, The Canadian Institutes of Health Research (CIHR) - Institute of Circulatory and Respiratory Health, Defense Research and Development Canada, The National American Heart Association, and the Heart and Stroke Foundation of Canada.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Nichol G, Thomas E, Callaway CW. Regional variation in out-of-hospital cardiac arrest incidence and outcome. JAMA. 2008;300:1423–1431. doi: 10.1001/jama.300.12.1423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Weisfeldt ML, Sitlani CM, Ornato JP, Rea T, Aufderheide TP, Davis D, Dreyer J, Hess EP, Jui J, Maloney J, Sopko G, Powell J, Nichol G, Morrison LJ for the ROC Investigators. Survival after application of automatic external defibrillators before arrival of the emergency medical system: Evaluation in the Resuscitation Outcomes Consortium population of 21 million. J Am Coll Cardiol. 2010;55:1713–1720. doi: 10.1016/j.jacc.2009.11.077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nichol G, Stiell IG, Laupacis A, et al. A Cumulative metaanalysis of the effectiveness of defibrillator-capable emergency medical services for victims of out-of-hospital cardiac arrest. Ann Emerg Med. 1999;34:517–525. [PubMed] [Google Scholar]
- 4.Valenzuela TD, Roe DJ, Nichol G, Clark LL, Spaite DW, Hardman RG. Outcomes of rapid defibrillation by security officers after cardiac arrest in casinos. N Engl J Med. 2000;343:1206–1209. doi: 10.1056/NEJM200010263431701. [DOI] [PubMed] [Google Scholar]
- 5.Page RL, Joglar JA, Kowal RC, Zagrodzky JD, Nelson LL, Ramaswamy K, Barbera SJ, Hamdan MH, McKenas DK. Use of automated external defibrillators by a U.S. airline. New Engl J Med. 2000;343:1210–1216. doi: 10.1056/NEJM200010263431702. [DOI] [PubMed] [Google Scholar]
- 6.Caffrey SL, Willoughby PJ, Pepe PE, Becker LB. Public use of automated external defibrillators. New Engl J Med. 2002;347:1242–1247. doi: 10.1056/NEJMoa020932. [DOI] [PubMed] [Google Scholar]
- 7.Larsen M, Eisenberg M, Cummins RO, Hallstrom AP. Predicting survival from out-of-hospital cardiac arrest: a graphic model. Ann Emerg Med. 1993;22:1652–1658. doi: 10.1016/s0196-0644(05)81302-2. [DOI] [PubMed] [Google Scholar]
- 8.Hallstrom AP, Ornato JP, Weisfeldt M, Travers A, Christenson J, McBurnie MA, Zalenski R, Becker LB, Schron EB, Proschan M Public Access Defibrillation Trial I. Public-access defibrillation and survival after out-of-hospital cardiac arrest. New Engl J Med. 2004;351:637–646. doi: 10.1056/NEJMoa040566. [DOI] [PubMed] [Google Scholar]
- 9.Statistics Canada. 2006 Community Profiles. [Accessed April 7, 2012];2006 Census. 2007 Mar 13; http://www12.statcan.ca/census-recensement/2006/dp-pd/prof/92-591/index.cfm?Lang=E.
- 10.Morrison LJ, Nichol G, Rea TD, Christenson J, Callaway CW, Stephens S, et al. Rationale, development and implementation of the Resuscitation Outcomes Consortium Epistry--Cardiac Arrest. Resuscitation. 2008;78:161–9. doi: 10.1016/j.resuscitation.2008.02.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Toronto Employment Survey [Internet] Toronto: Policy and Research, City Planning Division, City of Toronto; 1998. [updated 2012; cited July 13,2012]. Available from http://www.toronto.ca/demographics/surveys.htm. [Google Scholar]
- 12.Glazier RH, Booth GL, Creatore MI, Gozdyra P, Glazier RH. Neighbourhood Environments and Resources for Healthy Living – A Focus on Diabetes in Toronto: ICES Atlas. Toronto: Institute for Clinical Evaluative Sciences; 2007. Technical Notes. [Google Scholar]
- 13.Church R, Revelle C. The maximal covering location problem. Papers of the Regional Science Association. 1974;32:101–120. [Google Scholar]
- 14.Verter V, Lapierre S. Location of preventative healthcare facilities. Annals of Operations Research. 2002;110:123–132. [Google Scholar]
- 15.Daskin M, Dean L. Operations Research and Healthcare. Springer; US: 2005. Location of Healthcare Facilities. [Google Scholar]
- 16.Warden CR, Daya M, LeGrady LA. Using geographic information systems to evaluate cardiac arrest survival. Prehosp Emerg Care. 2007;11:19–24. doi: 10.1080/10903120601023461. [DOI] [PubMed] [Google Scholar]
- 17.Engdahl J, Herlitz J. Localization of out-of-hospital cardiac arrest in Goteborg 1994–2002 and implications for public access defibrillation. Resuscitation. 2005;64:171–175. doi: 10.1016/j.resuscitation.2004.08.006. [DOI] [PubMed] [Google Scholar]
- 18.Rea T, Blackwood J, Damona S, Phelps R, Eisenberg M. A link between emergency dispatch and public access AEDs: Potential implications for early defibrillation. Resuscitation. 2011;82:995–998. doi: 10.1016/j.resuscitation.2011.04.011. [DOI] [PubMed] [Google Scholar]
- 19.San Ramon Valley Fire Department. [accessed April 6, 2012];Fire Department iPhone App v2.0. http://www.firedepartment.mobi/
- 20.Becker L, Eisenberg M, Fahrenbruch C, Cobb L. Public locations of cardiac arrest: implications for public access defibrillation. Circulation. 1998;97:2106–2109. doi: 10.1161/01.cir.97.21.2106. [DOI] [PubMed] [Google Scholar]
- 21.Gratton M, Lindholm DJ, Campbell JP. Public-access defibrillation: where do we place the AEDs? Prehosp Emerg Care. 1999;3:303–305. doi: 10.1080/10903129908958958. [DOI] [PubMed] [Google Scholar]