Abstract
Setting
Mwanza, Phalombe and Zomba districts in the Southern Region of Malawi.
Background
Radios have been installed in many health centers in the Southern Region of Malawi but communication is often indirect. Messages get re-channeled from one health center to another before reaching district hospitals. In an attempt to strengthen the obstetric referral system, the Safe Motherhood Project installed a repeater-based VHF radio communication system in three pilot districts. The overall goal of the new network was to enable the health centers to communicate directly to their district health offices (DHOs) for an ambulance when they have an emergency obstetric complication for referral to the hospital.
Aim
This study aimed to determine whether or not improving the radio communications system reduces the delay in referral of obstetric emergencies from health center to hospital.
Materials and methods
Data collection was conducted between 2001 and 2003 using a range of data collection methods. Radio communications register books were placed at each participating health center to record information on all women with emergency obstetric complications referred to the hospital for further management. An obstetric referral form was completed on each woman referred to the hospital. And using the same referral form, the referral hospital was required to give feedback to the health centers on discharge of the patient. Existing maternity registers or HMIS registers were reviewed to obtain additional information not captured in radio communication registers. Interviews with health center staff were conducted to obtain their communication experiences before and after the new network was installed.
Results
The average number of obstetric admissions per month and the proportion of referrals in the participating health centers significantly increased during the post-intervention period. Significantly more emergency obstetric referrals were collected under 1 hour between decision to refer by the midwife at the health center and arrival of transport from the DHO or base station in the post-intervention period than pre-intervention period (p<0.02). However, some patients still waited for more than 13 hours for transportation in the post-intervention period. The median time interval between decision to refer and arrival of transport was 3 h. versus 2 h. 3 min. in the pre- and post-intervention periods respectively.
Conclusion
This study has demonstrated that the new VHF radio network system has, without doubt, improved the radio communication system in the three pilot districts. However, although the time interval between the decision to refer and arrival of transport significantly improved after the intervention, the majority of transportation still took too long, particularly for someone with postpartum hemorrhage. It is very important to improve the management/control of obstetric ambulances at district level so as to complement efforts of an improved radio communication system in reducing delays in the referral of obstetric emergencies.

Introduction
It is widely accepted that substantial reductions in maternal mortality and severe morbidity are impossible to achieve without an effective referral system for complicated cases. An effective referral system means access to transport and communication. Box 1 below lists some of the pre-requisites for a “well functioning” referral system.
Indeed, transport and communication are vital in ensuring access to emergency obstetric care because of the unpredictability and rapid progression of maternity complications. There are three types of delays on the pathway to essential obstetric care. 2–4 These delays can be categorized as (a) Type 1 delay: women and their families delay in deciding to seek obstetric care; (b) Type 2 delay: women do not reach appropriate care on time; and (c) Type 3 delay: women do not receive prompt care at health facilities. This report looks at efforts that ensure women do reach appropriate care on time (reduction of Type 2 delay). Table 1 highlights the estimated average interval from onset to death for major obstetric complications.
Table 1.
Estimated average interval from onset to death for major obstetric complications
| Complication | Hours | Days |
| Hemorrhage | ||
| • Postpartum | 2 | |
| • Antepartum | 12 | |
| Ruptured uterus | 1 | |
| Eclampsia | 2 | |
| Obstructed labour | 3 | |
| Sepsis | 6 |
Source: (Starrs 1997)3
Although radios have been installed in many health centres in all the twelve districts of the Southern Region of Malawi, communication is often indirect. Messages get re-channelled from one health centre to another before reaching district hospitals. In an attempt to strengthen the obstetric referral system, the Safe Motherhood Project installed a VHF radio communication system in three pilot districts. The radio communication system comprised PRF10 repeaters and SRM9000 transceivers linking groups of health centres with district and / or referral hospitals. The new system ensured that health centres are able to place a call directly to the district health office (DHO) for an ambulance when they have an emergency obstetric complication for referral to the hospital.
Box 1: Some requirements of an effective referral system.
An adequately resourced referral centre
Communications and feedback systems
Designated transport
Agreed setting-specific protocols for the identification of complications
Personnel trained in their use
Teamwork between referral levels
An unified records system
Source: (Murray et al. 2001)1
We carried out a study to determine the effect of such an improved radio communications system on the referral of obstetric emergencies in the three pilot districts.
Materials And Methods
Study area
The study was conducted in three pilot districts selected for the upgrading of their radio communication system; namely: Zomba, Phalombe and Mwanza districts. In Zomba and Phalombe districts, the new radio communication system was installed in April 2003 while in Mwanza the radio communication network was upgraded in July 2003. Four to five health centres per district were purposively selected to participate in the survey. Only those health centres that did not have any radio communication before or those that had the radio system but were communicating indirectly with their DHO or base station of the ambulance were included in the study. A total of 14 health centres were enrolled into the study. Of these, 6 health centres did not have any radio communication system while 8 had a radio but were unable to communicate directly with their district health office.
Study period
The study was conducted between September 2001 and November 2003. However, only data recorded from May to November before and after radio installation/upgrading were analysed. This enabled the study team to remove one of the confounding factors to the study -the rainy season when rural roads sometimes become impassable to vehicles including the ambulances.
Data collection
The data were collected using a range of data collection methods. A radio communications register book was placed at each participating health centre to record information on all women with emergency obstetric complications referred to the hospital for further management. An obstetric referral form was completed on each woman referred to the hospital. And using the same form, the referral hospital was required to give feedback to the health centres on discharge of the patient. Existing maternity registers or HMIS registers were reviewed to obtain additional information not captured in radio communication registers. Interviews with health centre staff were conducted to obtain their communication experiences before and after the new network was installed.
Results
Pregnancy-related admissions and referrals
The sources of data on pregnancy-related admissions and referrals were maternity registers and radio communication registers at the 14 health centres. Pregnancy-related admissions and referrals recorded during the study period are summarized in Table 2 below. This table also shows the number of emergency obstetric referrals recorded in survey registers that had time indicated between decision to refer by the midwife at the health centre and arrival of transport.
Table 2.
Pregnancy-related admissions and referrals by study period
| Study period | |||
| Variable | Pre-intervention | Post-intervention | Total |
| No. of admissions recorded in maternity register |
3460 | 3482 | 6942 |
| Total No. of emergency obstetric referrals in maternity register |
209 | 263 | 472 |
| No. of emergency obstetric referrals recorded in radio register |
123 | 157 | 280 |
| No. of emergency obstetric referrals in radio register with time indicated between decision to refer by midwife and arrival of transport |
69 | 96 | 165 |
A review of maternity registers revealed that there were a total of 6942 admissions, among which 472 were referred to the hospitals due to various obstetric reasons. Of these 6942 women admissions, 3460 occurred during the pre-intervention period and the remainder during the post-intervention period. Data further show that of 3460 maternity admissions that occurred during the pre-intervention period, 209 (6.0%) were referred to the hospitals. Furthermore, of 3482 admissions that occurred during the post-intervention period, 263 (7.6%) were referred to hospital for further management. There is evidence to suggest that there was a significant increase in the proportion of referrals during the post-intervention period (c2 = 5.25, p <0.02).
Table 2 also shows that of 209 referrals that occurred during the pre-intervention period, 123 (59%) were recorded in radio communications registers by the midwives at the health centres. Of these, 69 referrals (56%) had the time indicated between decision to refer by the midwife and arrival of transport. Furthermore, 157 out of 263 (60%) referrals that occurred during the post-intervention period were recorded in the survey registers. Of these, 96 (61%) had time indicated between the decision to refer and arrival of transport.
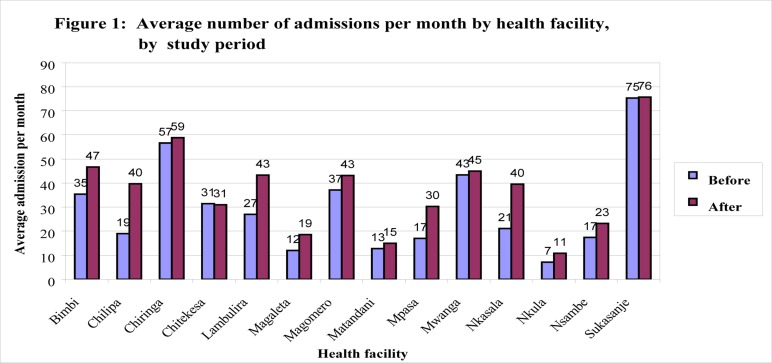
Figure 1 compares the average number of admissions per month in the study health centres during the pre-intervention and post-intervention periods. Overall, results showed a statistically significant increase in the average number of admissions per month at the health centres following the intervention (p <0.001).
Figure 1.
Average number of admissions per month by health facility, by study period
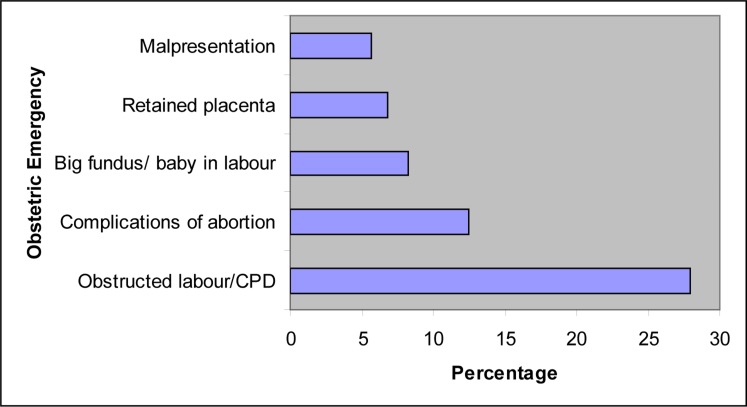
Referral indications
As shown in Figure 2, the major indication for referral was prolonged labour/cephalopelvic disproportion/obstructed labour, accounting for 28% of the total number of referrals recorded in survey registers (n = 280) during the study period. Surprisingly, none of the midwives recorded foetal distress as an indication for emergency obstetric referral.
Figure 2.
Five most common indications for emergency obstetric referral during study period (61% of 280 referrals)
Referral communication
Table 3 shows the various means of communication used during the study period to call for an ambulance from its base station to pick up women with obstetric emergencies. Results show that radio message was the major means of communication, accounting for 66% of all calls during the study period. Radio calls increased from 37% to 88% during the post-intervention period. This increase was highly significant (p <0.001). Use of a courier by letter was the second common means of communication used only during the pre-intervention period. Its use dropped to zero in post-intervention period.
Table 3.
Types of communication with base station for ambulance services during the study period
| Study Period | |||
| Type of communication | Pre-intervention | Post-intervention | Total |
| Radio message | 46 (37.4%) | 138 (87.9%) | 184 (65.7%) |
| Courier by letter | 29 (23.6%) | 0 (0.0%) | 29 (10.4%) |
| Telephone | 4 (3.3%) | 5 (3.2%) | 9 (3.2%) |
| Verbal* | 7 (5.7%) | 0 (0.0%)** | 7 (2.5%) |
| Not stated | 37 (30.1%) | 14 ( 8.9%) | 51 (18.2%) |
| Total | 123 (100%) | 157 (100%) | 280 (100%) |
When use of a CHAM ambulance was required, the midwives simply sent a word to the parish father to escort the patient to the referral hospital.
Although CHAM ambulances were still used in the post-intervention period (Table 5), the type of referral communication to parish fathers was not indicated. We suppose it was verbal, too.
When the ambulance took too long to collect the patient from the health centre, the midwife was forced to make repeat calls to the DHO. Of 184 radio messages, 102 calls (55%) were not repeated while 68 (37%) were repeated once, 9 (5%) repeated twice and 5 (3%) repeated three times. Table 4 compares the frequency of repeating radio messages between the pre- and post-intervention periods.
Table 4.
Frequency of repeating radio messages for ambulance services by study period
| Study Period | |||
| Message period |
Pre-intevention | Post-intervention | Total |
| Not at all | 23 (50.0%) | 79 (57.2%) | 102 (55.4%) |
| Once | 19 (41.3%) | 49 (35.5%) | 68 (37.0%) |
| Twice | 0 (0.0%) | 9 (6.5%) | 9 (4.9%) |
| Thrice or more | 4 (8.7%) | 1* (0.7%) | 5 (2.7%) |
| Total | 46 (100%) | 138 (100%) | 184 (100%) |
Box 2 presents a case study of a woman for whom the midwife had to repeat radio communication four times before transport arrived to collect her in the post-intervention period
Referral transport
Table 5 shows that a government ambulance was the major mode of transport used for the referral of obstetric emergencies during the study period, accounting for 70% of all forms of transportation used.
Table 5.
Utilization of various modes of transport during emergency obstetric referrals by mode of transport, by study period
| Study Period | |||
| Mode of transport |
Pre-intervention | Post-intervention | Total |
| Government ambulance |
66 (53.7%) | 129 (82.2%) | 195 (69.6%) |
| CHAM ambulance | 23 (18.7%) | 9 ( 5.7%) | 32 (11.4%) |
| Private vehicle | 14 (11.4%) | 6 ( 3.8%) | 20 ( 7.1%) |
| Bicycle | 13 (10.6%) | 6 (3.8%) | 19 (6.8%) |
| Walking | 0 (0.0%) | 3 (1.9%) | 3 (1.1%) |
| Bus | 1 (0.8%) | 0 (0.0%) | 1 (0.4%) |
| Push ambulance* | 1 (0.8%) | 0 (0.0%) | 1 (0.4%) |
| Matola | 1 (0.8%) | 0 (0.0%) | 1 (0.4%) |
| Not stated | 4 (3.3%) | 4 (2.5%) | 8 (2.9%) |
| Total | 123 (100%) | 157 (100%) | 280 (100%) |
A pushed stretcher of a bicycle ambulance. By definition, a bicycle ambulance consists of a bicycle that is hooked to a stretcher.
Table 5 compares the utilization of various modes of transport by obstetric emergencies during the pre- and post-intervention periods. Utilization of government ambulances significantly increased from 54% in the pre-intervention period to 82% in the post-intervention period (c2 = 26.51, p <0.001). During the post-intervention period, there was a statistically significant drop in the use of CHAM ambulances (c2 =11.46, p <0.001), private vehicles (c2 = 5.94, p <0.02) and bicycles (c2 = 4.96, p <0.03). However, despite a higher use of government ambulance, still three referred obstetric patients walked during the post-intervention period.
Box 2: Case study 1.
Mrs. E.K was admitted at Nkasala Health Centre at 8 am on 27 July 2003 in labour. However, her labour took too long till the following day when the midwife decided to refer her to Zomba Central Hospital. The midwife made the first ambulance call at 2.20 pm on 28 July 2003. After waiting for the first 1 hour, she repeated the call at 3.40 pm but still the ambulance did not come to collect the patient. The midwife was informed that there was not enough fuel at Zomba DHO; hence, only one ambulance was on the road. She made subsequent repeat calls at 4.40 pm, 6.00 pm and 8.00 pm. Each time she repeated the call, she was told that the ambulance had gone to other health centres for patients. It was not stated what type of patients these were. Finally, at 9.00 pm on 28 July 2003, the ambulance came to collect Mrs. E.K to Zomba Central Hospital, after she had waited for almost 7 hours. At the referral hospital it was confirmed that she had prolonged labour and a CS was performed. Fortunately, both the mother and child were fine after CS despite the serious delay in referral.
Referral transport cost
The government of Malawi offers free health services, including ambulance services. However, when a government ambulance was not available to transport an obstetric emergency, guardians had no choice but to hire some other mode of transport within their reach. When a CHAM ambulance was used, the hiring cost ranged from US $4.59 to $16.53, with a mean cost of $9.72. Hiring charges for a private vehicle ranged from $3.49 to $22.96, with a mean cost of $11.65.
Referral time
As shown in Table 2, of 280 referrals recorded in radio communication registers during the study period, only 165 referrals (59%) had the times recorded between the decision to refer by the midwife at the health centre and arrival of transport at the health centres. Of these referrals, data show that 16% were collected in less than 1 hour during the preintervention period and 31% in post-intervention period (Figure 3). This difference was statistically significant; i.e. more emergency obstetric referrals were collected within 1 hour during the post-intervention period than during pre-intervention period (c2 = 5.04, p <0.02).
Two referrals waited for more than 13 hours for transportation in the post-intervention period. The case study in Box 3 demonstrates extreme delay in referral.
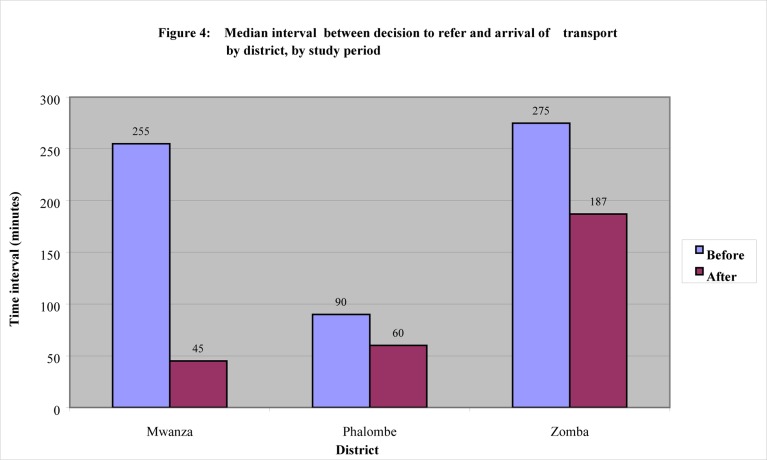
Overall, a median time of 150 minutes (2 hrs 30 minutes) was required between the decision to refer a patient by the midwife and arrival of transport in the three districts during the study period. Median times of 180 minutes (3 hours) and 123 minutes (2 hours 3 minutes) between the decision to refer and arrival of transport were required during the pre-intervention and post-intervention periods, respectively. There is evidence to suggest that there was a statistically significant difference in the median interval between decision to refer and arrival of transport between the pre- and post-intervention periods (p < 0.02).
The time interval and range between decision to refer the patient by the midwife and arrival of transport varied from district to district as shown in Table 6. The distances between the various health facilities are shown in Table 7. In Mwanza district, the distance from health centres under study to the referral district hospital ranged from 35 – 92 km with an average distance of 64 km. Results showed that the interval between decision to refer and arrival of transport ranged from 5 min. to 12h, with a median time of 4 h. 15 min. during the pre-intervention period. In the post-intervention period, the interval ranged from 2 min. to 8h. 20min, with a median of 45 min. There was a statistically significant difference in the median interval between decision to refer and arrival of transport between the pre- and post-intervention periods (p<0.005).
Table 6.
Time interval between decision to refer and arrival of transport by district, by study period
| Interval between decision to refer and arrival of transport | ||||
| Median | Range | |||
| District | Pre-intervention | Post-intervention | Pre-intervention | Post-intervention |
| Mwanza | 4h 15min | 45min | 5min–12h | 2min – 8h 10min |
| Phalombe | 1h 30min | 1h | 15min. – 4h. 45min | 15min – 8h 20min |
| Zomba | 4h 35 min | 3h 7min | 45min – 16h | 30min – 4h 15min |
Table 7.
Distances between the various health facilities
| Distances to Mwanza District Hospital | |
| Magaleta health centre | 35 km |
| Matandani health centre | 61 km |
| Nkula health centre | 67 km |
| Nsambe health centre | 92 km |
| Distances to Phalombe Mission Hospital | |
| Chiringa maternity | 34 km |
| Chitekesa health centre | 47 km |
| Mpasa health centre | 14 km |
| Mwanga health centre | 33 km |
| Sukasanje health centre | 61 km |
| Distances to Zomba Central Hospital | |
| Bimbi health centre | 30 km |
| Chilipa health centre | 33 km |
| Lambulira health centre | 20 km |
| Magomero health centre | 48 km |
| Nkasala health centre | 20 km |
The distance from the health centres to the referral CHAM hospital in Phalombe district ranged from 14 – 61 km, with an average distance of 38 km. During the pre-intervention period, the interval between decision to refer and arrival of transport in Phalombe ranged from 15 min. to 4 h. 45min., with a median of 1h. 30min. The range was from 15 min. to 8 h. 20 min. and a median of 1 h. during the post-intervention period. However, the difference in the median interval between the pre- and post-intervention periods was not significant (p>0.3).
Box 3: Case study 2.
Mrs. E.S was admitted at Chilipa Health Centre at 8 pm on 8 May 2003. She had been in labour and complained of severe abdominal pains. The midwife suspected that she might have a ruptured uterus or peritonitis. At 8.15pm that day, she decided to refer her to Zomba Central Hospital. Using the new radio communication equipment, she communicated directly with the district health office for an ambulance. After waiting for the ambulance for close to 2 hours, she repeated the ambulance call at 10 pm, but disappointingly it never came.
On 9 May 2003, she again repeated the ambulance call at 2 am. At around 9.45 am, the Safe Motherhood Project Technical Advisor arrived at Chilipa Health Centre on her routine follow up visits on the radio communications study in Zomba district. When the midwife was asked on how the new radio was working, she replied: “This new radio your project installed for us is working very fine. We are now able to talk to the district health office directly unlike in the past when we had to pass the message to St Luke's hospital that in turn had to pass our message for an ambulance to the district health office. However, there is a patient in the postnatal ward who needs to go to Zomba Central Hospital. We called for an ambulance yesterday but up to now it has not come. We are told the ambulance has gone to Balaka.”
At around 10 am, after examining the patient and confirming the provisional diagnosis, the Technical Advisor picked up the radio receiver and called the district health office for an ambulance and asked for the District Nursing Officer (DNO). The DNO assured the Technical Advisor that the ambulance would be sent to Chilipa to collect the patient as soon as possible. Indeed, after 30 minutes, the ambulance arrived at Chilipa Health Centre and this critically ill patient left at 10.35 am after waiting for transport for more than 14 hours.
In Zomba district, the distance from the health centres to Zomba Central Hospital ranged from 20 – 48 km, with an average distance of 30 km. Results showed that the interval between decision to refer and arrival of transport ranged from 45 min. to 16 h., with a median of 4 h. 35 min. during the pre-intervention period. During the post-intervention period, the time interval ranged from 30 min. to 14 h. 15 min., with a median of 3 h. 7 min. There was a statistically significant difference in median time interval between decision to refer and arrival of transport during the pre- and post-intervention periods (p<0.03).
Figure 4 compares the time intervals between decision to refer and arrival of transport among the three study districts during the pre- and post-intervention periods.
Figure 4.
Median interval between decision to refer and arrival of transport by district, by study period
Reported reasons for any delay in referral are outlined in Table 8. In this report, the word “delay” has been operationalized to mean a time interval of more than one hour between decision to refer and arrival of transport. Reasons for any delays in referral were not known for 79 cases. The leading reported reason for delay was that the ambulance at the base station had gone to other health centres to collect patients.
Table 8.
Known reasons for delay in transportation of obstetric emergencies by study period (n = 122*)
| Study Period | |||
| Reason for delay |
Pre-intervention | Post-intervention | Total |
| Ambulance had other calls |
6 (10.2%) | 17 (27.0%) | 23 (18.9%) |
| Indirect communication with base |
8 (13.5%) | 0 (0.0%) | 8 (6.6%) |
| Lack of fuel | 4 (6.8%) | 2 (3.2%) | 6 (4.9%) |
| No network coverage |
4 (6.8%) | 0 (0.0%) | 4 (3.3%) |
| Message delivered by hand |
1 (1.7%) | 0 (0.0%) | 1 (0.8%) |
| No ambulance service at night |
1 (1.7%) | 0 (0.0%) | 1 (0.8%) |
| Not stated | 35 (59.3%) | 44 (69.8%) | 79 (64.7%) |
| Total | 59 (100%) | 63 (100%) | 122 (100%) |
165 women had time recorded between decision to refer and arrival of transport. 43 women are known to have experienced no delays in referral; hence excluded to make n = 122
Discussion
Obstetric admissions and referrals
The study shows that the average number of obstetric admissions per month in the study health centres increased following the upgrading/installation of the radio communication system (Figure 1). The Rescuer Project in Uganda found a similar result. 3 This positive result is even more striking as; overall, there is a decrease in skilled attendance at birth not only in the Southern Region but also in Malawi as a whole (MOHP 2003). Some of the increase is perhaps explained by the fact that most pregnant women are now assured of a reliable means of communication for referral transport should they develop complications whilst in labour at the health centre. In addition, the fact that half of the health centres studied had benefited from infrastructure improvements by the project, the new environment at the renovated maternity units may have played a role too. This study also shows a significant proportional increase in referrals in the post intervention period, which may have been the result of better communication.
Referral communication
Radios have been installed in many health centres in the Southern Region, but communication is often indirect. Messages get re-channelled from one health centre to another before reaching district hospitals. The same was the experience of the health centres in the three districts before the intervention. The problem was worst in Phalombe district because until about five years ago, Phalombe and Mulanje was one district and hence shared a single radio communication system. For example, radio messages from Chiringa Health Centre were reaching the DHO's office after going first via health centres in Zomba district, then to Chiradzulu District Hospital, and then to Mulanje District Hospital that finally had to telephone the DHO Phalombe to send an ambulance to Chiringa. This resulted in long delays and often no ambulance was sent to the referring health centre. This study has shown, without doubt, that in the three pilot districts, the new radio network has improved the communication between health centres and their district health offices where the ambulances are based. The new radio network allows the health centres to communicate directly with their DHOs and ambulance drivers.
Referral transport
Another important finding of this study is that 82% of women with obstetric complications from health centres travelled by an ambulance from the DHO after the intervention compared to just over half (54%) in the period before. This increase could be attributed to the direct means of communication to the DHO offered by the new network. However, it is worrying to note that three referred women with obstetric emergencies walked during the post-intervention period. All these patients were from Chitekesa Health Centre in Phalombe district. Chitekesa is near to Matiya Health Centre in Zomba district. Because government hospitals offer free health services, most patients around Chitekesa opt to go to Matiya from where a radio message is sent to the DHO in Zomba for an ambulance to pick them up to Zomba Central Hospital. Although the midwife at Chitekesa can directly communicate with the DHO in Zomba, the latter is not prepared to send an ambulance to Chitekesa, which is in Phalombe district. It would appear that some district health management teams (DHMTs) rigidly adhere to district borders. This situation can be highly detrimental to women who develop emergency obstetric complications in a remote health centre.
Referral transport cost
This study has shown that the mean cost of transport to obstetric referred patients was US$10 for hiring a CHAM ambulance and US$12 for a private vehicle. This is very expensive against the per capita annual income in Malawi. According to DFID's Malawi Country Assistant Plan, the per capita GNI in 2000 was estimated at US$170. This translates to a per capita average monthly income of US$14. It can therefore be argued that women spent almost their whole monthly income on transport during referral, if forced to hire a vehicle.
Referral time
The main objective of this study was to assess whether or not the new radio network would reduce delays in the referral of women with emergency obstetric complications from health centre to the hospital. Obstetric haemorrhage is the third leading cause of institutional maternal deaths in Southern Malawi. 5Although the interval between the decision to refer by the midwife at the health centre and arrival of transport improved after the intervention, only a third of women with obstetric complications (31%) were collected in less than 1 hour. Postpartum haemorrhage (PPH) is the fastest killer of women. Table 1 shows that PPH kills on average in just 2 hours. Therefore this result indicates that lives of most women could not have been saved if they would have been referred due to severe PPH. However, Mwanza and Phalombe districts would be able to save lives of women with PPH as shown in Table 8. In Zomba district, the interval between decision to refer and arrival of transport took far too long (> 3 hours), yet the average distance between the study health centres and the referral hospital was the least among the three districts.
Although the Safe Motherhood Project has provided each district in the project area with an obstetric ambulance, most obstetric emergencies took too long to be collected from health centres despite the radio communication intervention. Such delays might even be greater in the rainy season when many rural roads become impassable.
Guidelines on use of the obstetric ambulances have been given to all districts but are not strictly followed. A study on the management of obstetric ambulances found that obstetric ambulances are often misused. 6 In many circumstances, the study found that the obstetric ambulances were being used for administrative purposes such as picking up of staff. Unless transport managers and DHOs minimize the high level of abuse of obstetric ambulances, transport will still remain a major constraint affecting the referral system for obstetric emergencies in the Southern Region.
Study limitations
The study was faced with two major limitations. Firstly, there was incomplete recording of information in radio communication registers. Not all referrals recorded in the maternity register or HMIS register were recorded in the radio communication registers. These registers captured only about 60% of the total referrals made during the study period despite two follow up visits to the health centres by the research team during the study period. The duration between the time health centre staff placed a call for an ambulance and the pick-up time of the patients was only recorded for 35% of total obstetric referrals made during the study period. This can be understood as many health centres are staffed by only one midwife working 24 hours around the clock, who has also other registers to complete. Referral hospitals in two districts never sent back obstetric referral forms to the health centre so that they could complete the filling of the additional and required information in their registers. In these two districts, only where the mother had gone back to the health centre for either postnatal or under fives clinic services were the midwives able to interview her on the treatment she obtained at the referral hospital and complete the register book. Only Holy Family hospital in Phalombe district returned filled in obstetric referral forms back to the health centres.
Secondly, the other limitation was the study design. Campbell et al. 7 argue that an important factor in determining how convincingly a change is attributable to an intervention is the study design. The 'gold standard' design for testing whether an intervention has an effect is the use of an experimental approach, such as randomised controlled trial (RCT) or the community randomised trial (CRT). Descriptive rather than experimental designs are, however, the most possible and likely options for evaluating efforts in safe motherhood programs because randomised trials are expensive and are usually aimed at communities rather than individuals. A before-and-after study design does not prove that the association between the intervention and observed change is causal. Without a truly comparable control group, it is never entirely possible to isolate the effects due to the intervention from other changes that occurred at the same time. 8 However, the different elements pieced together can present a plausible argument as to why/how the intervention contributes to change.
Conclusion
This study has demonstrated that the new repeater-based VHF radio network system has, without doubt, improved the radio communication system in the three pilot districts. However, although the time interval between the decision to refer and arrival of transport significantly improved after the intervention, the majority of transportation still took too long, particularly for someone with severe postpartum haemorrhage. It is very important to improve the management/control of obstetric ambulances at district level so as to complement efforts of an improved radio communication system in reducing delays in the referral of obstetric emergencies.
Acknowledgements
We would like to express our sincere appreciation to the maternity staff at the 14 participating health centres in Mwanza, Phalombe and Zomba, without whose cooperation data collection would not have been possible. We are also indebted to the District Health Officers in the three districts for allowing their health centres to participate in this operations research study. Special thanks go to Pitronic Limited and Vista Communications for the speedy work on the installation/upgrading of the radio communications network in the three districts thereby allowing us to do this study before the end of the project.
References
- 1.Murray SF, Davies S, Phiri RK, Ahmed Y. Tools for monitoring the effectiveness of district maternity referral systems. Health Policy and Planning. 2001;16(4):353–361. doi: 10.1093/heapol/16.4.353. [DOI] [PubMed] [Google Scholar]
- 2.Ransom E, Yinger N. Making Motherhood Safer: Overcoming obstacles on the pathway to care. Programs that promote maternal health and survival. Population Reference Bureau. 2002:19–21. [Google Scholar]
- 3.Starrs A. The safe motherhood action agenda: priorities for the next decade. Improve access to good quality maternal health services. Family Care International. 1997:36–50. [Google Scholar]
- 4.Thaddeus S, Maine D. Too far to walk: maternal mortality in context. Social Science and Medicine. 1994;38(8):1091–1110. doi: 10.1016/0277-9536(94)90226-7. [DOI] [PubMed] [Google Scholar]
- 5.Ratsma YEC. Why more mothers die: Confidential Enquires into Institutional Maternal Deaths in the Southern Region of Malawi 2001. Malawi Medical Journal. 2005;17(3):75–80. doi: 10.4314/mmj.v17i3.10882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lungu K, Ratsma YEC. Management of obstetric ambulances at government district hospitals in the Southern Region of Malawi (Unpublished Report) Malawi Ministry of Health and Population; 2003. (2003) Skilled Attendance for Every One (Unpublished Report) [Google Scholar]
- 7.Campbell O, Filippi V, Koblinsky M, et al. Lessons learnt: a decade of measuring the impact of safe motherhood programmes. London: London School of Hygiene and Tropical Medicine.; 1997. [Google Scholar]
- 8.Ronsmans C. What is the evidence for the oblique role of audits to improve the quality of obstetric care. In: De Brouwere V, Van Lerberghe W, editors. Safe Motherhood Strategies: a Review of the Evidence. 2001. [Google Scholar]