Abstract
Objective
To determine whether an immediate reporting service for musculoskeletal trauma reduces interpretation errors and positively impacts on patient referral pathways.
Methods
A pragmatic multicentre randomised controlled trial was undertaken. 1502 patients were recruited and randomly assigned to an immediate or delayed reporting arm and treated according to group assignment. Assessment was made of concordance in image interpretation between emergency department (ED) clinicians and radiology; discharge and referral pathways; and patient journey times.
Results
1688 radiographic examinations were performed (1502 patients). 91 discordant interpretations were identified (n=91/1688; 5.4%) with a greater number of discordant interpretations noted in the delayed reporting arm (n=67/849, 7.9%). In the immediate reporting arm, the availability of a report reduced, but did not eliminate, discordance in interpretation (n=24/839, 2.9%). No significant difference in number of patients discharged, referred to hospital clinics or admitted was identified. However, patient ED recalls were significantly reduced (z=2.66; p=0.008) in the immediate reporting arm, as were the number of short-term inpatient bed days (5 days or less) (z=3.636; p<0.001). Patient journey time from ED arrival to discharge or admission was equivalent (z=0.79, p=0.432).
Conclusion
Immediate reporting significantly reduced ED interpretive errors and prevented errors that would require patient recall. However, immediate reporting did not eliminate ED interpretative errors or change the number of patients discharged, referred to hospital clinics or admitted overall.
Advances in knowledge
This is the first study to consider the wider impact of immediate reporting on the ED patient pathway as a whole and hospital resource usage.
Emergency department (ED) activity in England continues to increase, with 21.3 million attendances recorded in 2010–11, an increase of 3.9% from the previous year, the large majority (20.7 million) being new rather than follow-up attendances [1]. Musculoskeletal (MSK) injuries account for over 60% of recorded ED primary diagnoses in England [2] and range from simple abrasions to amputations. Radiography plays an important role in the diagnosis of many of these injuries, with 22–50% of ED patients being referred for radiographic examination [3-6] and a smaller, but increasing, number of patients being referred directly for cross-sectional imaging, typically CT [7]. Importantly, these increasing demands for both ED and radiology services are occurring at the same time as healthcare organisations in the UK are being asked to evaluate the quality of care provided and constrain service costs. Specifically, the National Health Service (NHS) quality, improvement, productivity and prevention (QIPP) strategy [8] and new ED quality indicators [9] demand that emphasis is placed on improving patient outcomes and service efficiency. One previously suggested radiology intervention that may support such improvements across trauma care is the provision of immediate ED reporting [10,11].
In the UK, the initial interpretation of ED radiographic images is undertaken by either medical staff or emergency nurse practitioners (ENPs). Previous studies have raised concerns regarding the accuracy of interpretation achieved by junior medical staff and ENPs, with reported interpretive discrepancy rates between ED and radiology ranging from 1.2% to 7.8% [12-17]. Undiagnosed injuries, or a delay in diagnosis, can predispose patients to long-term morbidity and have the potential for litigation [15,17,18]. Consequently, UK radiology departments have endeavoured to issue definitive reports within 1 working day of patient attendance at ED [19,20]. Although this has not been universally adopted across all NHS hospitals [21], where undertaken, a delay of at least 72 h before reports are available to ED clinicians and changes to patient treatment or management are implemented may still occur [22].
Over the last decade, the reporting of ED radiographs has been increasingly delegated to appropriately qualified radiographers, and previous studies have demonstrated that the quality and accuracy of radiographer reports are similar to those of consultant radiologists [23,24]. Yet, despite the increasing reporting capacity as a consequence of radiographer involvement, the publication of national guidance on report turnaround times [25] and the widespread implementation of digital imaging technology and communication systems, the timeliness of report availability appears to be unchanged. This is perhaps a consequence of traditional workload organisation, which often precludes the implementation of immediate reporting in practice. However, if we consider the wider hospital economy, the lack of progress in developing immediate reporting systems for ED may directly impact on service quality and throughput, with real implications for the achievement of the ED quality indicators [9]. This article presents the findings of a multicentre randomised controlled trial funded by the National Institute of Health Research (Research for Patient Benefit Programme PB-PG-0407-13033) and considers the impact of immediate reporting on interpretive discrepancies and patient referral pathways within the ED.
Methods and Materials
Design and setting
This study was a pragmatic multicentre randomised controlled trial, the complete protocol for which has been published elsewhere [26]. To control for local variation in practice and sociodemographic influences on patient ED attendance patterns, five hospitals from three NHS Trusts across the north of England were used. Each hospital operated a 24-h ED service, and the delayed reporting of ED radiographs by a radiologist or reporting radiographer was standard practice. Ethical approval for the study was obtained (08/H1003/168) alongside approval from the Research and Development Committee at each participating hospital trust. The trial was also registered with the Comprehensive Local Research Network (CLRN) as a portfolio study (UKCRN ID: 4821).
To determine the impact of immediate reporting, each hospital site committed to implementing an immediate reporting service for ED (led by the reporting radiographer team at each site) for a period of 4 weeks. This service operated over 7 days [2 weeks during daytime hours (8 am to 6 pm) and 2 weeks during evening/twilight hours (6 pm to 2 am)] to take account of variations in patient attendance patterns, injury presentation and availability of senior staff cover in both the ED and radiology departments.
Participants
A convenience sampling approach to recruitment was adopted and all patients attending the ED with an MSK injury experienced in the preceding 48 h requiring radiographic examination to assist in diagnosis and who were able to provide informed consent were eligible to participate in the study. Patients were excluded from the study where the injury was sustained more than 48 h prior to ED attendance in order to control for potential alteration in the standard treatment pathway as a result of the delay in time to diagnosis. Patients were also excluded from the study if the radiographic referral included examination of visceral structures (chest/abdomen) as the scope of the majority of radiographers providing the immediate reporting service was restricted to MSK examinations. No exclusion was made based upon patient demographic variation (e.g. age, gender). Assuming a 5% difference in the proportion of discrepant interpretations between the 2 arms, a sample size of 1242 patients (621 in each arm) was calculated (90% power). To allow for loss to follow-up, it was planned to recruit 800 patients into each arm.
Recruitment
Patients eligible for participation in the study were identified on arrival at the radiology department and invited to participate in the study while they waited for their imaging examination. An age-appropriate information leaflet was used to explain the purpose of the study, implications for treatment and follow-up data collection processes. The study information was available in languages other than English relevant to the clinical sites and also as a verbal recording to maximise inclusion. Those who agreed to participate were asked to provide written informed consent.
Intervention
This study adopted a parallel group approach and participants were randomly assigned to the immediate or delayed reporting arm and treated according to group assignment. Patients randomised to the immediate reporting arm were asked to wait in the radiology department following radiographic examination while the report was generated. The X-ray report was returned to the ED at the same time as the patient (electronically or on hard copy as was appropriate locally) for the ED clinician to review alongside the images. Patients randomised to the delayed reporting arm were asked to return to the ED following radiographic examination to await review of the images by the referring ED clinician. For these patients the X-ray report was issued by the radiology department at a later time and returned to the ED as was standard practice at each site. In both arms, the ED clinician was able to discuss the case with the examining radiographer and any member of the radiology team normally available to the ED clinician for consultation. Where a radiographer abnormality detection scheme was in operation (e.g. red dot, commenting or similar), this continued as was normal practice.
Outcome measures
The primary outcome measure was concordance in the interpretation of radiographs between radiology and ED. While it may be argued that ED interpretations are influenced by the provision of an immediate report, the report itself does not replace the autonomy and responsibility of the clinician managing the patient's care, and no identified research has established what level of influence a radiology report has on clinical decision making. Where discordant interpretations were recorded, independent image review and scrutiny of patient hospital, ED and radiology notes were undertaken 3–6 months post presentation to identify the results of further clinical tests and specialist referral. In this way, definitive injury status and origin of interpretive error could be determined independently of reports. ED journey time and discharge or referral pathway were also recorded for each patient. All patients discharged from the ED were followed up to identify unplanned reattendance for the same injury, to a hospital within the same Trust, within 2 weeks of initial presentation (self- or GP referral). A pilot study was undertaken at each clinical site to establish the acceptability and appropriateness of the data collection strategy.
Results
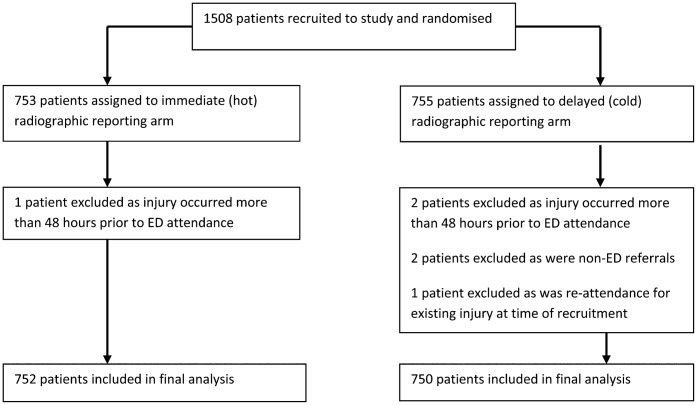
Recruitment took place between July 2009 and January 2010. A total of 1508 patients were recruited, although 6 were subsequently excluded (Figure 1), resulting in 1502 patients (1688 MSK X-ray examinations) in the final analysis. 752 patients (839 examinations) were recruited to the immediate reporting arm and 750 patients (849 examinations) were recruited to the delayed reporting arm.
Figure 1.
Recruitment flow chart. ED, emergency department.
The majority of patients were adults aged 18–64 years (64.3%), although the age range was wide (0–92 years). The characteristics of the sample group within each arm were similar in terms of the distribution of patient age (χ2=0.002; 2 df; p=0.999) and gender (χ2=0.961; 1 df; p=0.350) (Table 1).
Table 1. Characteristics of study sample.
| Sample characteristics | Immediate (hot) reporting arm number (%) | Delayed (cold) reporting arm number (%) | Total number (%) |
| Age (years) | |||
| Child (0–17) | 201 (26.7) | 201 (26.8) | 402 (26.8) |
| Adult (18–64) | 484 (64.4) | 482 (64.3) | 966 (64.3) |
| Elderly (65+) | 67 (8.9) | 67 (8.9) | 134 (8.9) |
| Gender | |||
| Male | 424 (56.4) | 404 (53.9) | 828 (55.1) |
| Female | 328 (43.6) | 346 (46.1) | 674 (44.9) |
Of the 1688 radiographic examinations performed, the large majority were of the appendicular skeleton (n=1550/1688; 91.8%). A total of 500 examinations (n=500/1688; 29.6%) were reported as positive for trauma by radiology with no significant difference in proportions across the study arms [proportional difference 0.4%; 95% confidence interval (CI) (−0.040, 0.047); p=0.875]. Discordant interpretations between radiology and ED were noted for 91 examinations (n=91/1688; 5.4%) and a significantly greater proportion of discordant interpretations occurred in the delayed reporting arm (n=67/849; 7.9%) compared with the immediate reporting arm (n=24/839; 2.9%) [proportional difference 5.0%; 95% CI (0.029, 0.072); p<0.001]. However, a number of discordant interpretations were related to the scaphoid clinical pathway (i.e. scaphoid injuries being treated clinically as abnormal even where radiographic examination is normal [27]) and errors in terminology (e.g. incorrect digit numbering; describing triquetrum as trapezium). Consequently, 79 true discrepant interpretations were identified (n=79/1688; 4.7%) (Table 2).
Table 2. Examination characteristics.
| Examination characteristics | Immediate (hot) reporting arm number (%) | Delayed (cold) reporting arm number (%) | Total number (%) |
| Anatomy | |||
| Upper limb (including shoulder girdle) | 452 (53.9) | 438 (51.6) | 890 (52.7) |
| Lower limb (including hip) | 304 (36.2) | 336 (39.6) | 640 (37.9) |
| Axial skeleton | 83 (9.9) | 75 (8.8) | 158 (9.4) |
| Radiographic examination interpretations between radiology and Emergency Department | |||
| Concordant | 815 (97.1) | 782 (92.1) | 1597 (94.6) |
| Discordant | 24 (2.9) | 67 (7.9) | 91 (5.4) |
| Reason for discordant interpretation | |||
| Scaphoid clinical pathway | 4 (16.7) | 4 (6.0) | 8 (8.8) |
| Terminology | 1 (4.2) | 3 (4.5) | 4 (4.4) |
| Discrepant interpretation | 19 (79.2) | 60 (89.6) | 79 (86.8) |
Although a greater proportion of discrepant interpretations related to the appendicular skeleton (n=67/79; 84.8%), when considered as a proportion of total examinations undertaken, no significant difference in the proportion of discrepant interpretations was noted between the appendicular and axial skeleton [proportional difference 3.2%; 95% CI (−0.010, 0.075); p=0.068] (Table 3). Independent image review and scrutiny of patient hospital, ED and radiology notes for patients with discrepant interpretations identified that interpretive errors were made by both radiology and ED staff, although a significantly greater number of interpretive errors (n=62/79; 78.5%) were made by ED clinicians [proportional difference 57.0%; 95% CI (0.442, 0.698); p<0.001] (Table 3). Importantly, interpretive errors were significantly reduced within the immediate reporting arm for both radiology (χ2=6.170; 1 df; p=0.013) and ED (χ2=15.576; 1 df; p<0.001) staff.
Table 3. Discrepant interpretations.
| Characteristics of discrepant interpretations | Immediate arm number (%) | Delayed arm number (%) | Total number (%) |
| Anatomy | |||
| Upper limb (inc. shoulder girdle) | 13 (68.4) | 24 (40.0) | 37 (46.8) |
| Lower limb (inc. hip) | 3 (15.8) | 27 (45.0) | 30 (38.0) |
| Axial skeleton | 3 (15.8) | 9 (15.0) | 12 (15.2) |
| Interpretive errors | |||
| Emergency department false positive | 14 (73.7) | 35 (58.3) | 49 (62.0) |
| Emergency department false negative | 1 (5.3) | 12 (20.0) | 13 (16.5) |
| Radiology false positive | 3 (15.8) | 11 (18.3) | 14 (17.7) |
| Radiology false negative | 1 (5.3) | 2 (3.3) | 3 (3.8) |
12 patients within the delayed reporting arm were incorrectly diagnosed as negative for injury by ED staff, and immediate recall of 7 patients to the ED on receipt of the report was necessary to implement a change in patient management. As no patient recalls occurred within the immediate reporting arm, this represented a significant difference (z=2.66; p=0.008). Of the patients discharged from the ED (Table 4), seven patients in each arm (n=14/810; 1.7%) reattended an ED within the same trust with the same injury within 2 weeks of initial presentation. For all of these, initial ED and radiology interpretations of the radiographic images were concordant and, although four patients underwent further radiographic examination as part of the reassessment process, the diagnostic decision remained unchanged and all patients were discharged again.
Table 4. Patient referral pathways.
| Initial patient referral pathways | Immediate arm number (%) | Delayed arm number (%) |
| All patients | ||
| Discharged | 415 (55.2) | 395 (52.7) |
| Admitted | 44 (5.9) | 58 (7.7) |
| Onward referral to hospital clinic | 286 (38.0) | 288 (38.4) |
| Did not wait to complete treatment | 6 (0.8) | 4 (0.5) |
| Disposal data not recorded | 1 (0.1) | 5 (0.7) |
| Total | 752 | 750 |
| Patients with discrepant reports | ||
| Discharged | 5 (26.3) | 17 (28.3) |
| Admitted | – | 2 (3.3) |
| Onward referral to hospital clinic | 14 (73.7) | 41 (68.3) |
| Total | 19 | 60 |
Despite a significant reduction in interpretive discrepancies within the immediate reporting arm, no significant difference was noted in the overall number of patients discharged, referred to hospital clinics or admitted (Table 4). Similarly, no significant difference in the overall number of admitted bed days was noted across the two arms using the Wilcoxon rank-sum test (z=−1.621; p=0.105). However, when length of stay was divided into short stay (≤5 days) or long stay (>5 days), a highly significant difference was noted between the two arms, with patients in the delayed reporting arm more likely to be admitted for stays of 5 days or less (z=−3.63; p<0.001). No significant difference was noted between the arms for stays of 6 days or more (z=−0.22; p=0.83) (Table 5).
Table 5. Patient admission days.
| The number of hospital inpatient days | No. of patients immediate arm | No. of patients delayed arm |
| 1 | 27 | 19 |
| 2 | 3 | 10 |
| 3 | 1 | 8 |
| 4 | 1 | 6 |
| 5 | 0 | 1 |
| 6 | 1 | 1 |
| 7 | 1 | 1 |
| 8 | 1 | 0 |
| 9 | 0 | 1 |
| 10 | 1 | 2 |
| 11 | 1 | 0 |
| 12 | 1 | 0 |
| 13 | 1 | 0 |
| 14 | 1 | 0 |
| 18 | 0 | 1 |
| 19 | 0 | 2 |
| 22 | 1 | 0 |
| 24 | 1 | 0 |
| 26 | 1 | 1 |
| 31 | 0 | 1 |
| 52 | 1 | 0 |
| 58 | 0 | 1 |
| Data missing | – | 3 |
| Total days | 245 | 305 |
The mean report turnaround time in the delayed reporting arm was 1.09 days (range 0.02–9.53 days) and was calculated as the average time from completion of radiographic examination to time of availability of a verified report. To determine the mean report turnaround time in the immediate reporting arm, the average time spent in radiology (from patient arrival at X-ray reception to patient referral back to the ED) was calculated for each arm and compared. In the delayed reporting arm, patients spent an average of 0.33 h (19.8 min) in the X-ray department compared with 0.41 h (24.6 min) in the immediate reporting arm. Consequently, the mean immediate report turnaround time was estimated to be 5 min (the difference in time between the two arms).
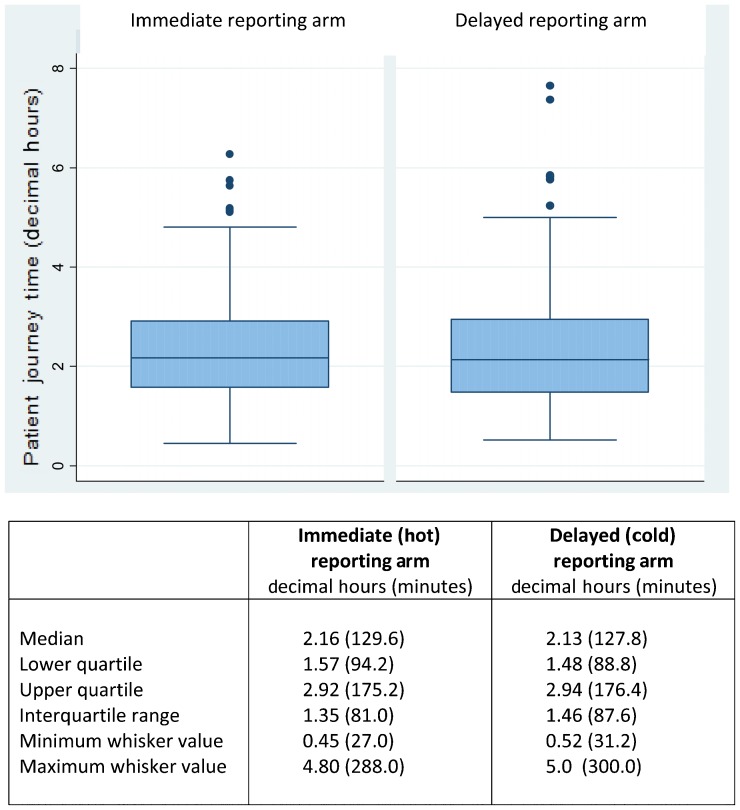
The distribution of overall patient journey time from ED arrival to discharge/referral in both arms (immediate vs delayed) was slightly positively skewed, although similarity was noted in both the mean (137 vs 136 min) and median (130 vs 128 min) journey times and interquartile ranges (81 vs 88 min). Analysis of equality of distributions showed no significant difference in journey times between the two arms (z=0.79; p=0.432) (Figure 2).
Figure 2.
Distribution of patient journey times.
Discussion
The results of this study provide new insight into the impact of immediate reporting on ED clinical decision making and patient treatment pathways. The prevalence of positive (abnormal) radiographic examinations as reported by radiology (n=501/1688; 29.7%) is similar to previous studies, suggesting that the sample is representative of practice [23,28].
Previous studies considering the accuracy of radiograph interpretations by ED staff have often used the radiological interpretation as the reference (gold) standard [18,23,29] despite sensitivity and specificity being variable and dependent on the imaging examination and experience of the reporting radiographer or radiologist [30,31]. In this study, a compound reference standard was applied equally in both arms and concordant interpretations between ED and radiology staff were assumed to be correct. Although this approach may be criticised for not determining the accuracy of concordant interpretations, it does reflect clinical practice standards, and further research is required to determine the error level in concordant interpretations. Investigation of discrepant interpretations was undertaken through independent review of images and assessment of patient hospital, ED and radiology notes to determine the accuracy of ED and radiology interpretations. As could be expected, a greater proportion of interpretative errors were made by ED clinicians (n=62/79; 78.5%). However, a significant reduction in the number of false-positive and false-negative interpretive errors by both ED and radiology clinicians was noted in the immediate reporting arm. With respect to the ED, this suggests that the availability of a report at the time of patient attendance positively influences ED patient management decisions, although it does not replace autonomy in decision making as a number of interpretive discrepancies were still recorded. Importantly, the provision of immediate reporting within this study eliminated the need to recall patients to the ED for a change in management as a consequence of false-negative diagnosis. In contrast, the reduction in radiology interpretive errors within the immediate reporting arm suggests that accessibility to the patient and ability to influence the imaging examination improves interpretive accuracy. This supports the findings of previous studies which demonstrated that the interpretive accuracy of radiology is maintained in the immediate reporting environment [32] and may even improve with speedier reporting processes [33], although further research is required to accurately determine the influential factors.
The value of reducing false-positive interpretations has been acknowledged by a small number of authors [12,31], but has often been overlooked in previous research as its impact on patient morbidity or mortality and hospital risk management strategies is limited. With increasing financial constraints, healthcare organisations are being compelled to evaluate resource utilisation, and within the context of trauma care a reduction in false-positive diagnoses may prevent unnecessary costs at both patient and service levels. However, within this study, no significant difference was noted in the number of patients discharged or referred to hospital clinics despite a significant reduction in both false-positive and false-negative interpretations within the immediate reporting arm. This suggests that factors beyond the availability of an image report are influential in patient management decision making. Despite this, data from this study do suggest that service costs associated with short-stay patient admissions could be reduced, although further work is required to corroborate this.
An important factor to consider when implementing service change is its impact on wider hospital standards and targets. In relation to ED care, patient journey time (from ED arrival to discharge or admission) is under continual scrutiny and the 4-h care standard remains one of the ED quality indicators [9]. The findings of this study demonstrate no difference in patient journey times across the two arms, despite patients in the immediate reporting arm experiencing an estimated 5 min additional wait in radiology due to radiology report generation. This may be as a result of research participation influencing reporting practice. However, it may also suggest that the availability of a radiology report reduces the need and time for ED clinicians to seek advice from colleagues on image appearances, although, again, further research is required to confirm this. For patients in the delayed arm, the mean report turnaround time was just over 1 day, although a wide range was noted (0.02–9.53 days). Importantly, the turnaround time recorded was based upon radiology report verification and availability to view electronically and not the time of actual report review by an ED clinician. Consequently, it is likely that the time to any change in ED decision making as a result of a radiology report extends beyond those recorded in this study. As the shortest report turnaround time in the delayed arm was less than 1 h, it is possible that the availability of a reporting radiographer for an extended period of time during data collection influenced reporting behaviours in the delayed reporting arm. As a result, it is suggested that actual mean report turnaround times in clinical practice may be greater, although variation across clinical sites will occur depending on reporting capacity.
Within this study, the immediate reporting service was led by reporting radiographers whose scope of practice is often limited to MSK examinations [34]. However, published evidence suggests that the findings of this study would be similar were the service to have been delivered by radiologists due to similar reporting standards [23,24]. Greater discordance is known to exist between radiology and clinicians in the interpretation of visceral radiographs [6,13,35]. Consequently, the extension of an immediate reporting service to include these examinations may further reduce interpretive errors and improve ED service quality, although further research is required to explore the impact of such a pathway.
Conclusion
Although differences in interpretive concordance have previously been investigated, no identified studies have examined the impact of immediate reporting on ED decision making and patient management. The findings of this study suggest that immediate reporting improves the accuracy of ED and radiology interpretations and positively influences ED patient management as a consequence of eliminating false-negative diagnoses with potential for subsequent patient recall. However, the availability of a report at the time of patient attendance did not prevent ED interpretative errors or change the number of patients discharged or referred to hospital clinics from the ED, and further work is required to explore the reasons for this. No significant difference was noted in the number of patients admitted to hospital and, although a small difference was noted in short-term bed stays, further research is required to confirm the significance of this finding on a larger scale. While immediate reporting meets the needs of ED clinicians and delivers the national report turnaround aspirations [25], the impact of implementing immediate reporting should be carefully evaluated to ensure that the anticipated benefits of service change can be achieved in practice.
Acknowledgments
The authors would like to thank Christopher Wyton for his assistance in data collection and Helen Jones and Paul Barker for facilitating local data collections and organising changes to ED reporting services.
Footnotes
The research was funded by the National Institute for Health Research (NIHR) Research for Patient Benefit (RfPB) programme (PB-PG-0407-13033).
Disclaimer
This article presents the results of independent research commissioned by the National Institute for Health Research (NIHR) under the Research for Patient Benefit Programme. The views expressed in this article are those of the authors and not necessarily those of the NHS, NIHR or the Department of Health.
References
- 1.Department of Health. A&E attendances. [cited 20 September 2011]. Available from: http://www.dh.gov.uk/en/Publicationsandstatistics/Statistics/Performancedataandstatistics/AccidentandEmergency/DH_077485. [Google Scholar]
- 2.NHS Information Centre. Accident and emergency attendances in England (experimental statistics) 2009–10. [cited 23 September 2011]. Available from: http://www.ic.nhs.uk/statistics-and-data-collections/hospital-care/accident-and-emergency-hospital-episode-statistics-hes/accident-and-emergency-attendances-in-england-experimental-statistics-2009-10. [Google Scholar]
- 3.de Lacey G. Number of casualty attenders referred for X-ray examination. Br J Radiol 1979;52:52–3. [DOI] [PubMed] [Google Scholar]
- 4.Richards PJ, Tins B, Cherian R, Rae F, Dharmarajah R, Phair IC, et al. The emergency department: an appropriate referral rate for radiography. Clin Radiol 2002;57:753–8. [DOI] [PubMed] [Google Scholar]
- 5.Nolan TM, Oberklaid F, Boldt D. Radiological services in a hospital emergency department—an evaluation of service delivery and radiograph interpretation. Aust Paediatr J 1984;20:109–12. [DOI] [PubMed] [Google Scholar]
- 6.Higginson I, Vogel S, Thompson J, Aickin R. Do radiographs requested from a paediatric emergency department in New Zealand need reporting? Emerg Med Australas 2004;16:288–94. [DOI] [PubMed] [Google Scholar]
- 7.Department of Health. Imaging and radiodiagnostics 9/10. [cited 20 September 2011]. Available from: http://www.dh.gov.uk/en/Publicationsandstatistics/Statistics/Performancedataandstatistics/HospitalActivityStatistics/DH_077487. [Google Scholar]
- 8.Department of Health. The NHS quality, innovation, productivity and prevention challenge: an introduction for clinicians. London, UK: Department of Health; 2010. [Google Scholar]
- 9.Department of Health. A&E clinical quality indicators data definitions. London, UK: Department of Health; 2010. [Google Scholar]
- 10.de Lacey G, Barker A, Harper J, Wignall B. An assessment of the clinical effects of reporting accident and emergency radiographs. Br J Radiol 1980;53:304–9. [DOI] [PubMed] [Google Scholar]
- 11.James MR, Bracegirdle D, Yates DW. X-ray reporting in accident and emergency departments—an area for improvements in efficiency. Arch Emerg Med 1991;8:266–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Benger JR, Lyburn ID. What is the effect of reporting all emergency department radiographs? Emerg Med J 2003;20:40–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Petinaux B, Bhat R, Boniface K, Aristizabal J. Accuracy of radiographic readings in the emergency department. Am J Emerg Med 2011;29:18–25. [DOI] [PubMed] [Google Scholar]
- 14.Berman L, de Lacey G, Craig O. A survey of accident and emergency reporting, results and implications. Clin Radiol 1985;36,483–4. [DOI] [PubMed] [Google Scholar]
- 15.Guly HR. Diagnostic errors in an emergency department. Emerg Med J 2001;18:263–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McLauchlan CA, Jones K, Guly HR. Interpretation of trauma radiographs by junior doctors in accident and emergency departments: a cause for concern? J Accid Emerg Med 1997;14:295–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sharma H, Bhagat S, Gaine WJ. Reducing diagnostic errors in musculoskeletal trauma by reviewing non-admission orthopaedic referrals in the next-day trauma meeting. Ann R Coll Surg Engl 2007;89:692–5. [Google Scholar]
- 18.Sprivulis P, Frazer A, Waring A. Same day X-ray reporting is not needed in well-supervised emergency departments. Emerg Med Australas 2001;13:194–7. [DOI] [PubMed] [Google Scholar]
- 19.Audit Commission. Improving your image. London, UK: HMSO; 1995. [Google Scholar]
- 20.Touquet R, Driscoll P, Nicholson D. Teaching in accident and emergency medicine: 10 commandments of accident and emergency radiology. BMJ 1995;310:642–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hardy M, Barrett C. Interpretation of trauma radiographs by radiographers and nurses in the UK: a comparative study. Br J Radiol 2004;77:57–61. [DOI] [PubMed] [Google Scholar]
- 22.Paterson AM, Price RC, Thomas A, Nuttall L. Reporting by radiographers: a policy and practice guide. Radiography 2004;10:205–10. [Google Scholar]
- 23.Robinson PJA, Culpan G, Wiggins M. Interpretation of selected accident and emergency radiographic examinations by radiographers: a review of 11000 cases. Br J Radiol 1999;72:546–51. [DOI] [PubMed] [Google Scholar]
- 24.Brealey S, Scally A, Hahn S, Thomas N, Godfrey C, Coomarasamy A. Accuracy of radiographer plain radiograph reporting in clinical practice: a meta-analysis. Clin Radiol 2005;60:232–41. [DOI] [PubMed] [Google Scholar]
- 25.National Imaging Board. Radiology reporting times best practice. [cited 20.09.11]. Available from: http://www.improvement.nhs.uk/documents/radiology_reporting_times_best_practice_guidance.pdf. [Google Scholar]
- 26.Hardy M, Snaith B. The impact of radiographer immediate reporting on patient outcomes and service delivery within the emergency department: designing a randomized controlled trial. Radiography 2011;17:275–9. [Google Scholar]
- 27.Shetty S, Sidhathan S, Jacob J, Ramesh B. ‘Clinical scaphoid fracture’: is it time to abolish this phrase? Ann Roy Coll Surg 2011;93:146–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Renwick IGH, Butt WP, Steele B. How well can radiographers triage x ray films in accident and emergency departments. BMJ 1991;302:568–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hallas P, Ellingson T. Errors in fracture diagnoses in the emergency department – characteristics of patients and diurnal variations. BMC Emerg Med 2006;6:4–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Robinson PJA, Wilson D, Coral A, Murphy A, Vernow P. Variation between experienced observers in the interpretation of accident and emergency radiographs. Br J Radiol 1999;72:323–30. [DOI] [PubMed] [Google Scholar]
- 31.Williams SM, Connelly DJ, Wadsworth S, Wilson DJ. Radiological review of accident and emergency radiographs: A 1-year audit. Clin Radiol 2000;55:861–5. [DOI] [PubMed] [Google Scholar]
- 32.Hardy M, Spencer N, Snaith B. Radiographer emergency department hot reporting: An assessment of service quality and feasibility. Radiography 2008;14:301–5. [Google Scholar]
- 33.Edwards AJ, Ricketts C, Dubbins PA, Roobottom CA, Wells IP. The effect of reporting speed on plain film reporting errors. Clin Radiol 2003;58:971–9. [DOI] [PubMed] [Google Scholar]
- 34.Price RC, Le Masurier SB. Longitudinal changes in extended roles in radiography: A new perspective. Radiography 2007;13:18–29. [DOI] [PubMed] [Google Scholar]
- 35.Grosvenor LJ, Verma R, O'Brien R, Entwistle JJ, Finlay D. Does reporting of plain chest radiographs affect the immediate management of patients admitted to the medical assessment unit? Clin Radiol 2003;58:719–22. [DOI] [PubMed] [Google Scholar]