Abstract
Objective:
Test a novel health monitoring approach by engaging an international online diabetes social network (SN) in consented health surveillance.
Methods:
Collection of structured self-reports about preventive and self-care practices and health status using a software application (“app”) that supports SN-mediated health research. Comparison of SN measures by diabetes type; and, SN with Behavioral Risk Factor Surveillance System (BRFSS) data, for US-residing insulin dependent respondents, using logistic regression.
Results:
Of 2,414 SN app users, 82% (n=1979) provided an A1c and 41% (n=996) completed a care survey of which 931 have diabetes. Of these: 65% and 41% were immunized against influenza and pneumonia respectively, 90% had their cholesterol checked, 82% and 66%, had their eyes and feet checked, respectively. Type 1/LADA respondents were more likely than Type 2/pre-diabetic respondents to report all five recommended practices (Adjusted OR (95% CI) 2.2 (1.5, 3.2)). Past year self-care measures were: 58% self-monitored their blood glucose (SMBG) ≥ 5 times daily, 37% saw their diabetes nutritionist, 56% saw a diabetes nurse educator, 53% saw a doctor for their diabetes ≥ 4 times. Reports of health status did not differ by diabetes type in the SN sample. The SN group was more likely than the BRFSS comparator group to use all five preventive care practices (Adjusted OR (95% CI) 1.8 (1.4, 2.1) and SMBG ≥ 5 times daily (Adjusted OR (95% CI) 10.1 (6.8, 14.9).
Conclusions:
Rapid assessment of diabetes care practices using a novel, SN-mediated approach can extend the capability of standard health surveillance systems.
Keywords: diabetes, healthcare quality, social networks, surveillance, social networking, chronic illness
Introduction
Traditional health surveillance programs, for example the Behavioral Risk Factor Surveillance System (BRFSS) and the National Health and Nutrition Examination Survey (NHANES), depend on increasingly unreliable channels for communication such as landline-based telephone surveys and household interviews. These approaches have enriched our understanding of population patterns of disease and illuminated the increasing morbidity and mortality burdens imposed by chronic illnesses (1, 2). However, standard approaches face challenges to obtain and retain participants, accommodate rapidly shifting patterns of disease, and balance breadth with depth of data collected in a fashion that supports assessment of disease prevalence and also healthcare and self-care practices of important affected subgroups (3).
Recently, we reported about our efforts to engage participants in an international online diabetes social network (SN) in consented public health monitoring of their disease (4). Using a software application (“app”) we launched into their Facebook-like community, SN members could report about and share their diabetes health data and participate in research as part of a distributed public health research cohort. The project falls within the rubric of new ‘citizen science’ efforts (5) to engage populations—including online social networks—in advancing public health through contributing data and observational energies to research (6, 7). This SN- mediated approach to health monitoring may address some of the challenges facing standard surveillance systems by engaging a population of interest in bidirectional communication about important and often overlooked aspects of their disease vital to targeted interventions.
For this report, we investigated diabetes health status and adherence with diabetes-specific recommended preventive and self-care practices among SN members using this novel app and approach. A primary focus of the investigation was to characterize care patterns in the sample overall and by diabetes type, an important stratification variable for understanding diabetes—a heterogeneous disorder originating in different biologic and sociologic processes (8–10). Type data are not collected in BRFSS (11) nor NHANES (12), limiting the utility of these systems for informing targeted response. A secondary focus of the investigation was to compare care metrics reported by the SN sample to those reported by respondents from a standard health surveillance system to ascertain the extent to which patterns resemble each other.
Methods
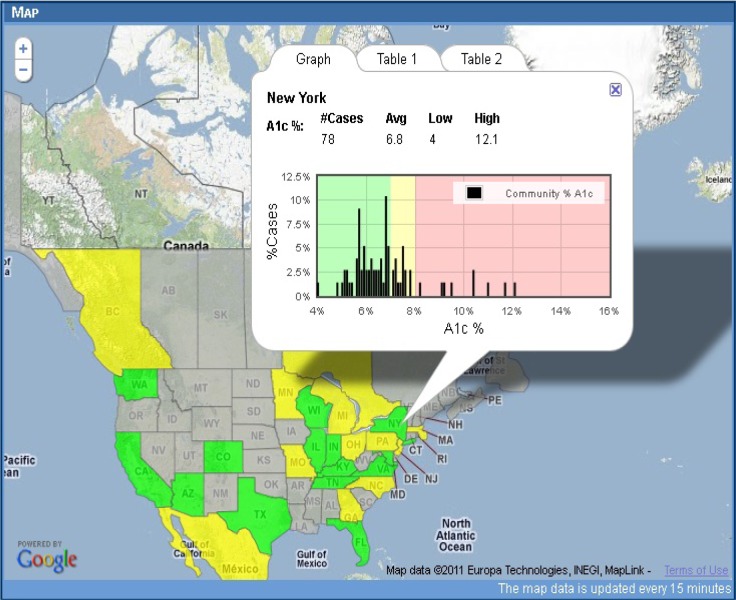
We used the TuAnalyze app (4) to survey participating members of the TuDiabetes community about their preventive and self-care practices. Members report and share their diabetes data and obtain both contextualized views of personal measures of glcyemic control (A1c%) (Figure 1), and summary reports about the health status and care patterns of all application users (Figure 2). The application is available in English and Spanish language versions. Its use is voluntary. Study activities were reviewed and approved by the Children’s Hospital Boston Institutional Review Board. Details about the application design, technology platform, operations and early adoption/use patterns are published elsewhere (4).
Figure 1.
Contextualized map view of A1c% data visible in the TuAnalyze application.
Users of the TuAnalyze application who self-report measures of glycemic control (A1c%) using the application are able to view near real-time summary data of their A1c% charted against the frequency distribution of other members’ shared A1c% measures, by geographic area (state, province or country). Map views of contextualized A1c% measures are delivered on a geographic information system display in which only a given user can see her personal data arrayed against summary data.
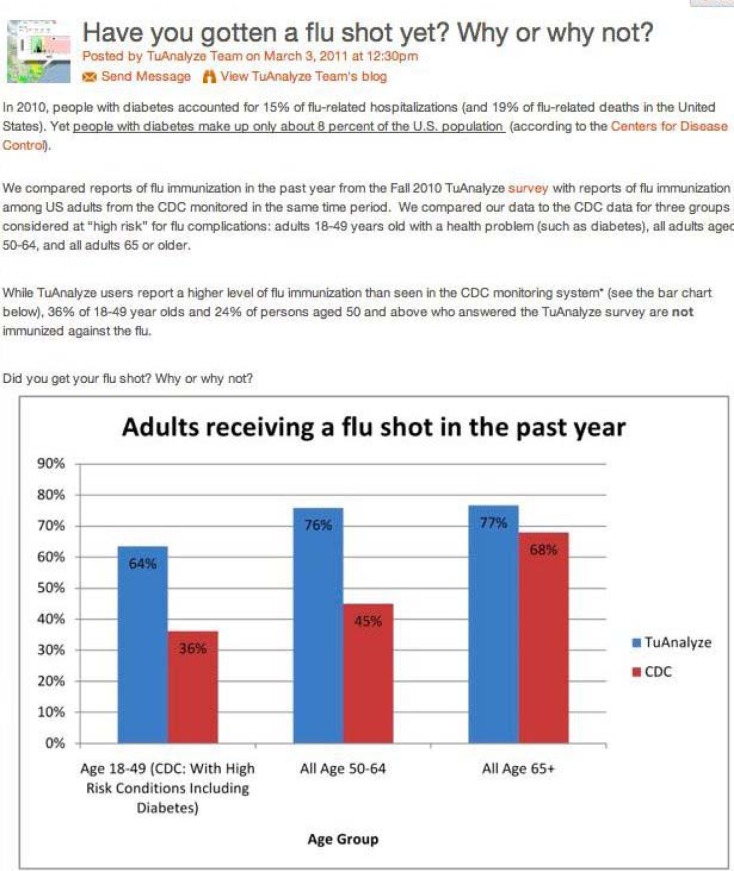
Figure 2.
Illustration of a TuAnalyze blog post and feedback report in which aggregate TuAnalyze data were shared with the TuDiabetes community and TuAnalyze users.
In the TuAnalyze application, members of the TuDiabetes.org host online social network as well as users of the TuAnalyze app, can read summary reports generated from data entered into the application by the community of users and shared as a means of communicating “results” and sparking engagement with the technology. Comments and questions posted by users are reviewed and incorporated into the study agenda as part of the participatory research approach.
TuAnalyze Sample Eligibility
Eligibility criteria for TuAnalyze and the larger TuDiabetes social network include being age 18 or older (younger users may join with a parent/guardian), affected by diabetes, ability to read and write English and/or Spanish, and having Internet access. Persons who do not have diabetes and are using the application as a proxy for another person, such as family members (N=65), were not included in these analyses.
Response Rate
During the study period, 996 out of 2,414 TuAnalyze users (response rate 41.2%) took a survey about their diabetes and associated care patterns, a response rate considered high for web surveys (13). The final sample consisted of 931 users who had completed the survey and have some form of diabetes. 105 users completed the survey but did not enter an A1c measure into the application; these were excluded from all analyses of A1c but otherwise included. Survey respondents who had not entered an A1c value were less likely than those who had to be white, to reside in the US, to have health insurance, and to use the English language version of the application.
Measures
Analyses draw on two sets of data: self-reported data from TuAnalyze users including A1c% values and surveys administered in the application environment; and self-reported health and demographic data from a US national sample surveyed for the 2009 Behavioral Risk Factor Surveillance System (BRFSS). The surveys administered in TuAnalyze were constructed from questions adapted to the application and taken from national health surveys, including the BRFSS (1, 12), and the National Health and Nutrition Examination Study (NHANES) (14).
TuAnalyze users indicated their diabetes type by selecting from a dropdown list in the survey with options for self-identifying as having Type 1, Type 1.5 (LADA), Type 2, pre-diabetes and gestational diabetes. We dichotomized diabetes type into two main groups, based on the underlying disease mechanism, as Type 1 or LADA and Type 2 or pre-diabetes. No respondents indicated gestational diabetes and this type is therefore not included.
Recommended diabetes preventive care practices were defined consistent with the 2010 American Diabetes Association (ADA) clinical practice recommendations, and included any history of a pneumonia vaccination, and past year history of an influenza vaccination, dilated eye exam, foot exam, and lipid profile (cholesterol check) (8). Self-care was assessed by reported typical frequency of self-monitoring of blood glucose, dichotomized at the ADA minimum recommended threshold of five or more times per day, and by describing reports of seeing a diabetes nurse educator and nutritionist in the past year and having four or more visits with one’s doctor in the past year.
TuAnalyze respondents were asked to rate their health on a standardized scale. Those who reported “Excellent”, “Very Good” or “Good” health were classified as having better health, compared to those who reported their health as “Fair” or “Poor”. Respondents who had ever been diagnosed with one or more health problem besides depression from a list of chronic conditions provided in the survey (arthritis, asthma, cancer, cardiovascular disease, depression, stroke and “other”) were categorized as having a chronic illness comorbidity; those who reported having been diagnosed with depression from this list were categorized as having experiencing depression. Consistent with ADA standards (8), respondents with a most recent A1c value of 7% or higher were classified as “above target” compared to those with lower values.
For both the TuAnalyze and BRFSS cohorts, we classified as white respondents who identified themselves solely as Caucasian and non-Hispanic. Age at the time of survey was determined from respondents’ date of birth (for TuAnalyze) and reported age at time of survey (for BRFSS). Country location for TuAnalyze users was gathered from data entered upon first engaging with the application; all BRFSS respondents are based in the US.
Data analyses
Reported use patterns of diabetes-specific preventive and self-care practices among the TuAnalyze sample were estimated in aggregate and across diabetes types. TuAnalyze patterns were compared with those found in analyses of the 2009 US BRFSS (15), the most recent US national health monitoring system for which comparable preventive and self-care measures are available. BRFSS data were downloaded at no cost from the US Centers for Disease Control and Prevention website (15). Descriptive statistics characterize the TuAnalyze sample and the Chi-Squared test was used to compare demographics, care behaviors and health outcomes across the two major diabetes type groups; this approach was also followed in comparing preventive and self-care practices across the TuAnalyze and BRFSS samples. Comparative analyses of TuAnalyze and BRFSS samples were undertaken for restricted samples that included respondents with diabetes, who reside in the US and who take insulin—a proxy for disease type given the absence of type data in the BRFSS. Cross-type and cross-sample comparisons are reported for bivariate and multivariate logistic regression models, the latter control for effects of sex, race (white/other), and age (continuous). Analyses were conducted in SAS version 9.2.
Results
Demographic characteristics of the TuAnalyze sample
As shown in Table 1, of 931 respondents, a majority is white, located in the US, and female. Approximately two-thirds (62%) report having Type 1 diabetes and another 10% have Type 1.5 (LADA); 27% have type 2 diabetes and the remaining 1% report pre-diabetes. Age of the sample ranged from 13 to 81, with an average and median of 43.
Table 1.
Characteristics of the TuAnalyze study sample, in aggregate and by type
| N (%) | ||||
|---|---|---|---|---|
| Total sample 931 (100) | Type 1 & LADA 664 (71.3) | Type 2/Pre-diabetes 267 (28.7) | OR for Type 1/LADA | |
| English Language site | 797 (85.6) | 594 (89.5) | 203 (76) | 2.7 (1.8, 3.9)*** |
| US Location | 664 (71.3) | 505 (76.1) | 167 (62.6) | 1.6 (1.1, 2.2)** |
| White | 745 (80) | 564 (84.9) | 181 (67.8) | 2.7 (1.9, 3.4)*** |
| Male | 367 (39.4) | 235 (35.4) | 132 (49.4) | .56 (.42, .75)*** |
| Over 40 | 447 (54.1) | 311 (46.8) | 202 (75.7) | .28 (.21, .39)*** |
p<.05
p<.01
p<.001
Use of recommended diabetes preventive and self care practices
Use of recommended preventive care practices was high to very high among respondents. Upwards of four-fifths of the sample reported having an annual check for cholesterol and a check for retinopathy in the past year. Upwards of two-thirds reported having an annual check of their feet for circulatory problems and neuropathy, and an influenza vaccination, in the past year. In contrast, two fifths reported having ever been immunized for pneumonia. Despite these prevalence levels for individual care practices, less than one third of respondents reported obtaining all five preventive care practices, a signifier of comprehensive preventive care.
Use of preventive care practices varied by diabetes type. Users reporting Type 1 or LADA diabetes were more likely than their peers with other diabetes types to report they were ever immunized for pneumonia and to report receiving an influenza vaccine, eye exam and foot exam in the past year. There was no difference in reporting a cholesterol check in the past year by diabetes type. Type 1 and LADA respondents had twice the odds of obtaining all five recommended preventive care practices as Type 2 and pre-diabetes respondents, controlling for age, sex and race (adjusted OR 2.2, 95% CI 1.5, 3.2, p <.001).
In terms of self-care, a majority of Type 1 and LADA respondents reported checking their blood glucose five or more times per day; these respondents are far more likely than their peers with other diabetes types to report doing so. Slight majorities reported seeing a diabetes nurse educator in the past year and meeting with their diabetes physician in the past year. These patterns did not differ by diabetes type. Fewer reported meeting with a nutritionist with no difference across type.
Health status
A minority of users reported fair or poor health and approximately one-third report a most recent A1c that is above the recommended target of 7%. One-quarter report a history of depression and nearly half report any other comorbidity. No differences in health indicators across type were found in adjusted analyses. Type 1 and LADA users were less likely to report a chronic comorbid condition and more likely to have an above-target A1c in unadjusted analyses only. Health status did not differ in relation to use of recommended preventive care measures in analyses that adjusted for age, sex, race and type.
Comparison of TuAnalyze and BRFSS samples
In analyses of US-residing insulin-dependent respondents from both samples, TuAnalyze users were more likely to be white and less likely to be over the age of 40 than the BRFSS sample, confirming the extension of health monitoring into a different demographic. There was no difference in the sex distribution across the two samples.
In analyses that controlled for age, sex and race, TuAnalyze respondents were more likely than BRFSS respondents to report they received an influenza immunization, eye exam, and all five care practices in the past year. BRFSS respondents were more likely than the TuAnalyze respondents to report they received an annual foot exam. The two samples differed greatly on self-monitoring of blood glucose; nearly three quarters of the TuAnalyze sample and less than one tenth of the national sample reported checking their blood sugar five or more times per day. No difference was found in the history of pneumonia vaccination, annual lipid profile, or frequency of doctor visits. Comparisons of diabetes educator or nutritionist visits were precluded by the absence of these data in the BRFSS sample.
Discussion
Using a novel health monitoring approach, we collected information about preventive and self-care practices from members of an international online diabetes social network. While a majority of respondents appear to follow practice guidelines for specific preventive care services, less than one third of the SN sample reported all five recommended practices—suggesting substantial room for improvement in quality of care and disease management. Patterns vary by diabetes type with higher levels of preventive care reported by respondents with Type 1 or LADA compared to Type 2 or pre-diabetes. A similar pattern was seen for reports of appropriate SMBG. Results are consistent with reports of type-based differences in service use, adherence and self-care generated from studies of traditionally sampled cohorts (16–19).
Adherence to select healthcare practices reported by US-residing insulin dependent users of TuAnalyze was mixed in relation to patterns found in a restricted comparator sample created from the US national BRFSS. For the majority of comparison measures, SN application users reported better use of preventive and self-care practices. This finding is not surprising given that users of TuAnalyze and its host community TuDiabetes may include disproportionate percentages of persons concerned with their health and with managing their diabetes—an artifact of the self-selecting nature of the sample. It is notable however that even in this context there were no differences across samples in levels of adherence to recommended quarterly doctor visits, possibly reflecting insurance eligibility requirements in the US. Even allowing for the healthy subject selection effect of the SN sample, there are sizeable gaps in care practice use especially with regard to the composite measure of adherence to the five recommended care practices.
Stepping back, this report adds to our previous finding that the SN mediated surveillance approach can be used to engage distributed populations in health research by reporting about current healthcare and self-care patterns by diabetes type. These measures are not available through standard reporting systems. Learning how to monitor these issues using novel approaches is, we contend, of high importance to public health given the large and growing burden imposed by chronic illness. Effective monitoring of chronic as opposed to contagious illness may benefit from tracking care patterns and management in detail and preservation of a bidirectional communication channel with study samples for follow-up. Ensuring patient (or sample) engagement may be especially important in this model.
Patient engagement in disease focused social networking is strong and growing (20). Growth reflects the appeal of this organic and grassroots phenomenon, and patients’ need for community (21), information and support (22–24). Harnessing this engagement for public health research may be an important new direction for population health monitoring. Social networking is increasingly common in the area of diabetes—about which there are many active online communities of varying quality and safety (25). Opportunities are manifold to extend health surveillance into these motivated and high value samples. The TuAnalyze approach accomplishes this without sacrificing privacy, safety or the autonomy of individuals and their communities.
Our approach is novel and findings should be read in the context of important limitations. Biases in participation and validity of self-reported data are a focus of our research and they are intrinsic to the model. Moreover, selection and participation biases are also present in more traditional health monitoring systems. Comparisons of TuAnalyze and BRFSS data are novel however they rely on assumptions about the adequacy of using self-reported insulin use as a proxy measure for diabetes type and they reflect fundamentally different approaches to surveillance. We recognize that these approaches are different and likely to yield different results. The social networking medium is inherently open and dynamic and affords a bidirectional communication channel with subjects. Application use and survey completion happen on a rolling basis that is in part indexed to the overall growth of the community and changing uptake of the application. Given this, it is challenging to ascertain a denominator that describes persons exposed to the site or active during a given time period (4). This is acceptable when the goal is rapid and not representative health surveillance—as befits this complementary monitoring mechanism.
Conclusion
Rapid assessment of preventive care practices and diabetes management strategies using a novel, SN-mediated approach is feasible and can be used to fill gaps in traditional public health monitoring of care practices by diabetes type. Our ability to harness this engagement without sacrificing privacy or user control may provide an important new direction for public health surveillance.
Table 2.
Reported use of recommended diabetes preventive care practices, by diabetes type
| N (%) | OR for Type 1/LADA (95% CI) | ||||
|---|---|---|---|---|---|
| All TuAnalyze users N=931 | Type 1 and LADA N=664 (71.3) | Type 2/Pre-Diabetes N=267 (28.7) | Unadjusted | Adjusted for age, sex, race | |
| Pneumonia shot ever | 380 (40.8) | 275 (41.4) | 105 (39.3) | 1.1 (.8, 1.5) | 1.6 (1.1, 2.3)** |
| Flu shot/past year | 606 (65.1) | 459 (69) | 148 (55.4) | 1.8 (1.3, 2.4)*** | 2.3 (1.6, 3.3)*** |
| Cholesterol check/past year | 837 (89.9) | 595 (89.6) | 242 (90.6) | .9 (.5, 1.4) | 1.7 (1, 3.1) |
| Eye exam/past year | 766 (82.3) | 580 (87.3) | 186 (69.7) | 3 (2.1, 4.3)*** | 4.8 (3.1, 7.5)*** |
| Foot exam/past year | 611 (65.6) | 454 (68.4) | 157 (58.8) | 1.5 (1.1, 2)** | 2.3 (1.6, 3.3)*** |
| All 5 care practices | 251 (30) | 193 (29.1) | 58 (21.7) | 1.5 (1.1, 2.1)* | 2.2 (1.5, 3.2)*** |
| Self-monitors blood glucose (SMBG) 5 or more times per day | 535 (57.5) | 477 (71.8) | 58 (21.7) | 9.2 (6.6, 12.9)*** | 10.1 (6.8, 14.9)*** |
| Nutrition visit/past year | 343 (36.8) | 241 (36.3) | 102 (38.2) | .9 (.7, 1.2) | .7 (.5, 1) |
| DNE visit/past year | 525 (56.4) | 383 (57.7) | 142 (53.2) | 1.3 (.9, 1.6) | 1 (.7, 1.4) |
| 4 or more MD visits/past year | 489 (52.5) | 345 (52) | 144 (53.9) | .9 (.7. 1.2) | 1 (.7, 1.4) |
p<.05
p<.01
p<.001
Table 3.
Health status, in aggregate and by type
| N (%) | OR for Type 1 (95% CI) | ||||
|---|---|---|---|---|---|
| All users (N=931) | Type 1 & LADA N=664 (71.3) | Type 2 & Pre-Diabetes N=267 (28.7) | Unadjusted | Adjusted for age, sex, race | |
| Poor self-rated health | 149 (16) | 111 (16.7) | 38 (14.2) | 1.2 (.8, 1.8) | 1.5 (.93, 2.3) |
| Depression | 216 (23.2) | 143 (21.5) | 73 (27.3) | .7 (.5, 1) | .72 (.5, 1) |
| Any other comorbidity | 411 (44.2) | 275 (41.4) | 136 (50.9) | .7 (.5, .9)** | 1.1 (.78, 1.5) |
| A1c>7% (N=826) | 277 (33.5) | 212 (35.8) | 65 (27.8) | 1.5 (1.04, 2)* | 1.2 (.85, 1.8) |
Table 4.
Demographics of the TuAnalyze sample and the BRFSS subsample
| TuAnalyze (N=577) | BRFSSa (N=9,832) | OR for TuA (95% CI) | |
|---|---|---|---|
| White | 510 (88.4) | 6,693 (68.1) | 3.6 (2.8, 4.6)*** |
| Male | 222 (38.5) | 4,030 (41) | .9 (.76, 1.1) |
| Over 40 | 325 (56.3) | 9,245 (94) | .08 (.07, .1)*** |
Note that the BRFSS subsample comprises that portion of a national probability sample that self-reports diabetes and insulin use.
Table 5.
Comparison of reports of obtaining recommended diabetes preventive care practices between insulin dependent TuAnalyze and BRFSS respondents
| N (%) | OR for TuAnalyze (95% CI) | |||
|---|---|---|---|---|
| TuAnalyze (N=577) | BRFSS (N=9,832) | Unadjusted | Adjusted for age, sex, race | |
| Pneumonia shot ever | 291 (50.4) | 6,262 (64.6) | .56 (.47, .66)*** | 1 (.84, 1.2) |
| Influenza immunization/past year | 415 (71.9) | 6,537 (66.5) | 1.3 (1.1, 1.6)* | 1.9 (1.6, 2.3)*** |
| Cholesterol check/past year | 525 (91) | 8,769 (93.1) | .75 (.56, 1) | 1.1 (.78, 1.5) |
| Eye exam/past year | 509 (88.2) | 7,415 (75.4) | 2.4 (1.9, 3.2)*** | 3.5 (2.6, 4.5)*** |
| Foot exam/past year | 420 (72.8) | 7,777 (79.7) | .68 (.56, .82)** | .65 (.52, .79)*** |
| All 5 care practices | 208 (36.1) | 3,264 (33.2) | 1.1 (.95, 1.4) | 1.8 (1.4, 2.1)*** |
| SMBG 5 or more times per day | 422 (73.1) | 903 (9.2) | 26.9 (22.1, 32.8)*** | 13.3 (10.8, 16.5)*** |
| Nutrition visit/past year | 343 (36.8) | -- | -- | -- |
| DNE visit/past year | 525 (56.4) | -- | -- | -- |
| 4+ MD visits/past year | 314 (54.4) | 5,638 (57.3) | .89 (.75, 1.05) | .98 (.82, 1.2) |
p<.01
p<.001
p<.0001
Acknowledgments
This work was supported by PO1HK000088-01 from the Centers for Disease Control and Prevention (CDC).
References
- (1).Ramsey F, Ussery-Hall A, Garcia D, McDonald G, Easton A, Kambon M, Balluz L, Garvin W, Vigeant J. Prevalence of selected risk behaviors and chronic diseases--Behavioral Risk Factor Surveillance System (BRFSS), 39 steps communities, United States, 2005. MMWR. Surveillance summaries : Morbidity and mortality weekly report. Surveillance summaries / CDC. 2008 Oct 31;57(11):1–20. [PubMed] [Google Scholar]
- (2).Yach D, Hawkes C, Gould CL, Hofman KJ. The global burden of chronic diseases: overcoming impediments to prevention and control. Jama. 2004 Jun 2;291(21):2616–2622. doi: 10.1001/jama.291.21.2616. [DOI] [PubMed] [Google Scholar]
- (3).Bonander J, Gates S. Public health in an era of personal health records: opportunities for innovation and new partnerships. Journal of medical Internet research. 2010;12(3):e33. doi: 10.2196/jmir.1346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (4).Weitzman ER, Adida B, Kelemen S, Mandl KD. Sharing data for public health research by members of an international online diabetes social network. PloS one. 2011;6(4):e19256. doi: 10.1371/journal.pone.0019256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (5).Hand E. Citizen science: People power. Nature. Aug 5;466(7307):685–687. doi: 10.1038/466685a. [DOI] [PubMed] [Google Scholar]
- (6).Van Noort SP, Muehlen M, Rebelo de Andrade H, Koppeschaar C, Lima Lourenco JM, Gomes MG. Gripenet: an internet-based system to monitor influenza-like illness uniformly across Europe. Euro Surveill. 2007 Jul;12(7):E5–6. doi: 10.2807/esm.12.07.00722-en. [DOI] [PubMed] [Google Scholar]
- (7).Brownstein JS, Freifeld CC, Madoff LC. Digital disease detection--harnessing the Web for public health surveillance. N Engl J Med. 2009 May 21;360(21):2153–2155. 2157. doi: 10.1056/NEJMp0900702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (8).A.D.A. Standards of Medical Care in Diabetes—2010. Diabetes Care. 2010;33(Supplement 1):S11–S61. doi: 10.2337/dc10-S011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (9).Leslie RD, Kolb H, Schloot NC, Buzzetti R, Mauricio D, De Leiva A, Yderstraede K, Sarti C, Thivolet C, Hadden D, Hunter S, Schernthaner G, Scherbaum W, Williams R, Pozzilli P. Diabetes classification: grey zones, sound and smoke: Action LADA 1. Diabetes/metabolism research and reviews. 2008 Oct;24(7):511–519. doi: 10.1002/dmrr.877. [DOI] [PubMed] [Google Scholar]
- (10).Tuomi T. Type 1 and type 2 diabetes: what do they have in common? Diabetes. 2005 Dec;54(Suppl 2):S40–45. doi: 10.2337/diabetes.54.suppl_2.s40. [DOI] [PubMed] [Google Scholar]
- (11).Chowdhury P, Balluz L, Town M, Chowdhury FM, Bartolis W, Garvin W, Akcin H, Greenlund KJ, Giles W. Surveillance of certain health behaviors and conditions among states and selected local areas - Behavioral Risk Factor Surveillance System, United States, 2007. MMWR. Surveillance summaries : Morbidity and mortality weekly report. Surveillance summaries / CDC. 2010 Feb 5;59(1):1–220. [PubMed] [Google Scholar]
- (12).Saaddine JB, Engelgau MM, Beckles GL, Gregg EW, Thompson TJ, Narayan KM. A diabetes report card for the United States: quality of care in the 1990s. Ann Intern Med. 2002 Apr 16;136(8):565–574. doi: 10.7326/0003-4819-136-8-200204160-00005. [DOI] [PubMed] [Google Scholar]
- (13).Cook C, Heath F, Thompson RL. A Meta-Analysis of Response Rates in Web- or Internet-Based Surveys. Educational and Psychological Measurement. 2000 Dec 1;60(6):821–836. 2000. [Google Scholar]
- (14).Hoerger TJ, Segel JE, Gregg EW, Saaddine JB. Is glycemic control improving in U.S. adults? Diabetes Care. 2008 Jan;31(1):81–86. doi: 10.2337/dc07-1572. [DOI] [PubMed] [Google Scholar]
- (15).CDC US Behavioral Risk Factor Surveillance System. 2009.
- (16).Broadbent E, Donkin L, Stroh JC. Illness and treatment perceptions are associated with adherence to medications, diet, and exercise in diabetic patients. Diabetes care. 2011 Feb;34(2):338–340. doi: 10.2337/dc10-1779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (17).Clarke WL. Behavioral challenges in the management of childhood diabetes. Journal of diabetes science and technology. 2011;5(2):225–228. doi: 10.1177/193229681100500203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (18).Kavookjian J, Elswick BM, Whetsel T. Interventions for being active among individuals with diabetes: a systematic review of the literature. The Diabetes educator. 2007 Nov-Dec;33(6):962–988. doi: 10.1177/0145721707308411. discussion 989–990. [DOI] [PubMed] [Google Scholar]
- (19).Peyrot M, Rubin RR, Kruger DF, Travis LB. Correlates of insulin injection omission. Diabetes care. 2010 Feb;33(2):240–245. doi: 10.2337/dc09-1348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (20).Fox S. Peer-to-peer healthcare. Washington, D.C: Pew Research Center; 2011. [Google Scholar]
- (21).Frost JH, Massagli MP. Social uses of personal health information within PatientsLikeMe, an online patient community: what can happen when patients have access to one another’s data. J Med Internet Res. 2008;10(3):e15. doi: 10.2196/jmir.1053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (22).Seeman N. Web 2.0 and chronic illness: new horizons, new opportunities. Healthc Q. 2008;11(1):104–108. 110, 104. [PubMed] [Google Scholar]
- (23).Chou WY, Hunt YM, Beckjord EB, Moser RP, Hesse BW. Social media use in the United States: implications for health communication. J Med Internet Res. 2009;11(4):e48. doi: 10.2196/jmir.1249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (24).Idriss SZ, Kvedar JC, Watson AJ. The role of online support communities: benefits of expanded social networks to patients with psoriasis. Arch Dermatol. 2009 Jan;145(1):46–51. doi: 10.1001/archdermatol.2008.529. [DOI] [PubMed] [Google Scholar]
- (25).Weitzman ER, Cole E, Kaci L, Mandl KD. Social but safe? Quality and safety of diabetes-related online social networks. J Am Med Inform Assoc. 2011 Jan 24; doi: 10.1136/jamia.2010.009712. [DOI] [PMC free article] [PubMed] [Google Scholar]