Abstract
Background
The prolonged survival of patients with thalassemia major as a result of the novel therapeutic strategies introduced in the last decade makes patient quality of life an important issue. This study investigated the changes occurring in overall quality of life in patients with thalassemia in the last decade.
Methods
This was a population-based cross-sectional survey of quality of life in the entire population with thalassemia major resident in the Liguria region of Italy from 2001 to 2009. The self-administered Short Form-36 (SF-36) questionnaire was used to measure quality of life in patients with thalassemia.
Results
Forty-nine and 52 eligible patients were assessed in 2001 and 2009, respectively. A total of 43 patients were assessed in both 2001 and 2009. Almost 40% of these 43 patients received deferasirox in 2009, a drug which was not available in 2001. The distribution of ferritin levels was lower in 2009 (median 730) as compared with 2001 (median 1107). Analysis of the raw differences between the two years did not show a significant difference. An improvement was observed in most SF-36 scales in 2009 as compared with 2001, particularly in the Mental Health scale (mean difference in Z score +4.0; 95% confidence interval 0.4–7.5; P = 0.030) and in the Mental Component Summary scale (mean difference in Z score +3.2; 95% confidence interval 0.2–6.2; P = 0.039).
Conclusion
The challenge associated with new therapies and improvement in mental quality of life dimensions indicates that implementation of effective interventions for screening and evaluation of quality of life is now urgent.
Keywords: thalassemia major, quality of life, survey, Short Form-36
Introduction
The more thalassemia major develops into a chronic disease with an expanding life expectancy, the more patient quality of life (QoL) is becoming an important dimension of care. Improved survival in patients with thalassemia major has been associated with better control of iron overload, better adherence with therapy, younger age at starting therapy,1 progressive emergence of a new generation of oral chelation therapy, availability of T2* magnetic resonance imaging to measure cardiac iron overload, and availability of specialized centers.2–4
Deferoxamine was the first iron chelator introduced into clinical practice. The drug was effective, but the mode of administration via slow daily subcutaneous infusion can result in noncompliance and potential impairment in one or more dimensions of QoL. Deferiprone and deferasirox were introduced into clinical practice in the 1990s and in the first years of the new millennium. Both are oral iron chelators, and there is evidence to support their use in the treatment of chronic iron overload. Deferiprone and deferasirox have different pharmacokinetic and adverse effect profiles. Deferiprone requires a weekly check of the white cell count because of the risk of agranulocytosis. Between 2001 and 2009, deferasirox, administered once daily, entered common use for the majority of patients.1–3
The impact of the disease on dimensions of QoL in patients with thalassemia major has not been consistently evaluated. Most studies were focused on specific QoL dimensions, such as the psychologic burden on children and their caregivers,5–7 or were performed in selected populations of patients.8–12 Moreover, no studies have investigated the changes in QoL that occurred during the last decade, when therapeutic strategies changed substantially. The availability of oral chelating agents has markedly impacted the course of the disease and the everyday life of patients with thalassemia.
In 2001, we surveyed the adult population with thalassemia major in Liguria, with the purpose of describing and analyzing their QoL. The survey was repeated with the same methodology in 2009, to identify any changes in QoL that occurred during this decade. We report here the results of this study.
Materials and methods
This study was a repeated cross-sectional population survey of QoL changes in people with thalassemia major resident in the Liguria region in northwest Italy between 2001 and 2009. The study was approved by the ethics committee at Ospedale Galliera. All participants gave their written informed consent before entering the study.
In both surveys, subjects were included according to the following eligibility criteria: diagnosis of thalassemia major, age ≥ 18 years, and residence in Liguria at the time of evaluation according to data provided by the Liguria regional registry of patients with thalassemia. All eligible patients were contacted by the clinical team and asked to fill in questionnaires during visits at the center.
Sociodemographic and clinical information was collected by the physician from WebThal®, an electronic clinical records system designed for thalassemia. For each patient, the following data were collected: age, gender, concomitant chronic comorbidities, iron chelation therapy, and average serum ferritin levels in the previous year.
Medical outcome survey Short-Form 36
The Short Form-36 (SF-36) is a self-administered generic questionnaire that measures two major subjective health concepts, ie, physical and mental health, using 36 multichoice questions. Eight multi-item scales can be generated from these items for evaluation of health-related QoL, including four related to physical health (physical functioning, role limitations due to physical problems, bodily pain, general health perception) and four related to mental health (vitality, social functioning, role limitations due to emotional problems, mental health).13 For each scale, the raw scores were then linearly transformed to 0–100 scales, with higher scores indicating better health.
The standardized summary scores for the physical component scale and the mental component scale were constructed from the eight SF-36 scales using recommended standard (US derived) scoring algorithms.14
The Italian version was translated and validated following the standard methodology of the International Quality of Life Assessment.15 The Italian version showed good psychometric properties, with Cronbach’s alpha ranging from 0.70 to 0.90 for the eight scales.16 Normative data for Italy were obtained in a survey in which the Italian version of the SF-36 was administered to 7000 subjects between 1991 and 1995.16
Statistical analysis
The characteristics of the 43 patients assessed in 2001 and 2009 were compared using nonparametric statistics for paired data, the McNemar’s test for binary variables, and the Wilcoxon test for continuous variables (Table 1). The raw SF-36 scores were expressed as the mean ± standard deviation in 2001 and 2009 (Table 2). For each year, the expected SF-36 mean scores, according to gender and age characteristics of the study samples (Figure 1) were estimated using the normative Italian data.16
Table 1.
Clinical and demographic characteristics of patients with thalassemia major in Liguria during 2001 and 2009
| 2001 (n = 43) | 2009 (n = 43) | P value* | |
|---|---|---|---|
| Age, years (mean ± SD) | 28.5 ± 6.0 | 36.5 ± 6.1 | |
| Gender | |||
| Males | 21 (48.8) | 21 (48.8) | |
| Chronic comorbidities | |||
| Active chronic hepatitis | 34 (79.1) | 31 (72.1) | 0.250 |
| Cirrhosis | 2 (4.7) | 3 (7.0) | 0.999 |
| Hypogonadism | 42 (97.7) | 42 (97.7) | 0.999 |
| Hypothyroidism | 10 (23.3) | 12 (27.9) | 0.500 |
| Diabetes requiring insulin | 4 (9.3) | 4 (9.3) | 0.999 |
| Osteoporosis | 25 (58.1) | 28 (65.1) | 0.375 |
| Heart failure | 5 (11.6) | 9 (20.9) | 0.125 |
| Iron chelation therapy | |||
| Deferoxamine | 24 (55.8) | 7 (16.3) | |
| Deferiprone | 19 (44.2) | 16 (37.2) | |
| Deferasirox | – | 16 (37.2) | |
| Combined treatment | – | 3 (7.0) | |
| Alternate treatment (DFP-DFX) | – | 1 (2.3) | <0.001 |
| Serum ferritin levels | |||
| Mean ± SD | 1235 ± 874 | 951 ± 754 | |
| Median (range) | 1107 (240–3880) | 730 (100–3500) | 0.127 |
Notes: If not specified otherwise, data are expressed as the number and proportion;
estimated by nonparametric tests.
Abbreviations: SD, standard deviation; DFP, deferiprone; DFX, deferasirox.
Table 2.
Score distribution and differences in SF-36 scales between 2001 and 2009
| SF-36 scales | 2001 | 2009 | 2009–2001 | P value | |||
|---|---|---|---|---|---|---|---|
|
|
|
|
|||||
| n | Mean ± SD | n | Mean ± SD | Mean difference | 95% CI | ||
| Physical functioning | 43 | 87.3 ± 17.0 | 43 | 86.1 ± 16.6 | −1.2 | −5.7, +3.4 | 0.611 |
| Role-physical | 43 | 83.1 ± 24.8 | 43 | 79.1 ± 31.8 | −4.1 | −13.8, +5.7 | 0.406 |
| Bodily pain | 43 | 69.7 ± 26.6 | 43 | 72.7 ± 25.9 | +2.9 | −6.3, +12.1 | 0.524 |
| General health | 42 | 50.8 ± 24.5 | 42 | 47.2 ± 23.2 | −3.6 | −10.0, +2.9 | 0.268 |
| Vitality | 42 | 64.4 ± 17.6 | 42 | 65.8 ± 14.8 | +1.4 | −3.7, +6.5 | 0.585 |
| Social functioning | 43 | 77.9 ± 23.4 | 43 | 81.7 ± 17.8 | +3.8 | −3.8, +11.4 | 0.323 |
| Role-emotional | 42 | 74.6 ± 37.4 | 42 | 78.6 ± 33.6 | +4.0 | −8.4, +16.4 | 0.522 |
| Mental health | 42 | 69.2 ± 18.8 | 42 | 74.2 ± 17.4 | +5.0 | −1.0, +11.0 | 0.098 |
Notes: Data are presented as the mean score for the population of patients with thalassemia in 2001 and 2009 and are not adjusted for gender or age. For each 0–100 scale, higher scores indicate better health.
Abbreviations: CI, confidence interval; SD, standard deviation; SF-36, Short-Form 36.
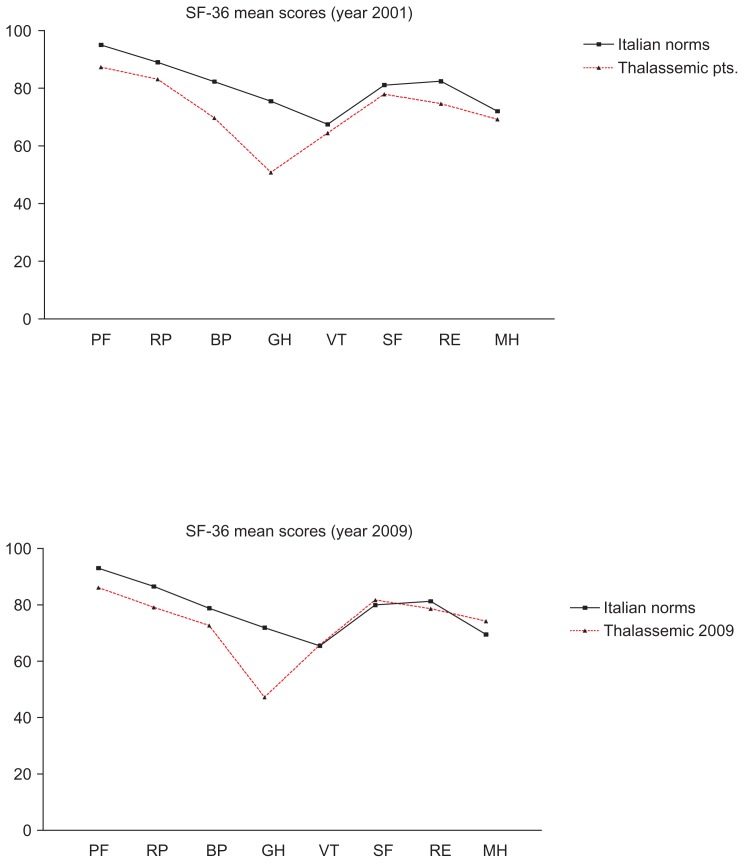
Figure 1.
Quality of life profile for patients with thalassemia in 2001 (A) and 2009 (B).
Notes: Data are presented as the mean score for the population of patients with thalassemia and of the corresponding (for gender and age) normative Italian population. For each 0–100 scale, higher scores indicate better health.
Abbreviations: PF, physical functioning; RP, role-physical; BP, bodily pain; GH, general health; VT, vitality; SF, social functioning; RE, role-emotional; MH, mental health.
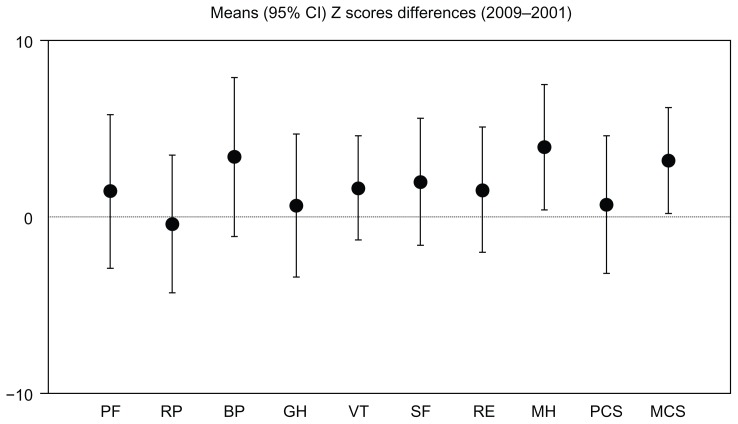
To enable a valid comparison of the two samples, the SF-36 scores were adjusted for the standardized gender and age distribution of the Italian population according to the gender and age of each study patient in 2001 and 2009. The standardized SF-36 scores were converted to Z scores (the patient’s mean score minus the adjusted Italian population score divided by the standard deviation of the population). Differences in the distribution between the two years (for the SF-36 scores in Table 2 and for the Z scores in Figure 2) were expressed as mean differences and their 95% confidence intervals (CI), so that a positive value means an improvement in QoL in 2009 as compared with 2001.
Figure 2.
Differences in Z scores (2009–2001) for the specific and summary SF-36 scales.
Notes: The data are presented as the difference in mean Z scores (95% confidence interval) adjusted for gender and age. A positive Z score denotes an improvement in quality of life in 2009 as compared with 2001.
Abbreviations: CI, confidence interval; PF, physical functioning; RP, role-physical; BP, bodily pain; GH, general health; VT, vitality; SF, social functioning; RE, role-emotional; MH, mental health; PCS, physical component summary; MCS, mental component summary; SF-36, Short-Form 36.
Results
In the 2001 survey, 50 eligible patients with a diagnosis of thalassemia major were identified. One patient refused to participate, leaving a sample of 49 patients evaluable for assessment in 2001. Between 2001 and 2009, four patients died (three because of heart failure, one as a result of sepsis), five patients became eligible for age (≥18 years), and four patients migrated to Liguria from another region. As a consequence, in the 2009 survey, 55 eligible patients with a diagnosis of thalassemia major were identified. Three patients refused to participate, leaving a sample of 52 patients evaluable for assessment in 2009. Overall, 43 patients were assessed in both 2001 and 2009.
The demographic and clinical characteristics of the evaluable patients who participated to the study in 2001 and 2009 (n = 43) are reported in Table 1. All patients were affected by one or more comorbidities. In 2009, as compared with 2001, a smaller proportion of patients were affected by a chronic active hepatitis and a higher proportion by heart complications.
A significant change (P < 0.001) in iron chelation therapies was observed in the study period. In 2001, 55.8% of patients received deferoxamine and 44.2% received deferiprone. Eight years later, only 16.3% received deferoxamine, 37.2% received deferiprone, and 37.2% received deferasirox, the new oral chelator approved by the European Medicines Agency in 2006. A deferoxamine-deferiprone combination was administered to 7.0% and a daily deferiprone-deferasirox alternating treatment to 2.3%. The distribution of ferritin levels was lower in 2009 (median = 730) as compared with 2001 (median = 1107, P = 0.127, by Wilcoxon test for paired data).
Most of the SF-36 scales in 2001 and in 2009 scored lower in comparison with the normative Italian data (Figure 1). The largest differences were observed for the general health scale, both in 2001 and in 2009.
Analysis of the raw differences between the two years (Table 2) did not show any significant differences. After adjusting for age and gender, through analyses of the Z scores difference (Figure 2), an improvement in most SF-36 scales was observed in 2009 as compared with 2001. A significant improvement in the mental health scale (Z score mean difference +4.0; 95% CI 0.4–7.5; P = 0.030) and in the mental component summary scale (Z score mean difference +3.2; 95% CI 0.2–6.2; P = 0.039) was observed. An improvement that did not reach statistical significance was observed for the bodily pain scale (Z score mean difference +3.4; 95% CI −1.1 to 7.9; P = 0.132), and for three scales related to mental health, ie, the vitality scale (mean difference in Z score +1.6; 95% CI −1.3 to 4.6; P = 0.275), social functioning scale (mean difference in Z score +2.0; 95% CI −1.7 to 5.6; P = 0.277) and role-emotional scale (mean difference in Z score +1.5; 95% CI −2.0 to 5.1; P = 0.395, Figure 2).
Discussion
To the authors’ knowledge, this is the first population study to describe and analyze QoL changes occurring during the last decade in a population of patients with thalassemia. The relatively small sample is counterbalanced by the high degree of representativeness of the study samples and by adherence with the procedures for QoL assessment. The surveys include virtually all individuals suffering from this disease in a specific geographic area.
According to the results of our study, people with thalassemia major scored significantly lower on all eight health status domains as compared with the general Italian population both in 2001 and in 2009.17 Between 2001 and 2009, an improvement in all mental dimensions was observed.
With all the limitations inherent in the study design, these results might reflect the challenge associated with the new therapeutic approaches introduced during the last decade and the resulting prolonged survival of patients with thalassemia major. Recent studies provide good evidence that new oral chelating agents along with novel noninvasive methods to assess cardiac iron overload are effective in preventing deaths related to iron overload, introduce brighter prospects of survival, and improve adherence with therapy.1 The association between the changed patterns of therapy and improvement in mental health could not be assessed in this survey because of the small sample size. However, this point is of interest, and would require further specific studies with larger samples providing enough power to detect significant differences.
Health-related QoL refers to the subjective assessment of physical and mental aspects of health, and is influenced by human experiences, beliefs, expectations, and perception. The positive change in self-assessed physical and mental health by people with thalassemia major is important and supports the validity of the new therapeutic strategies. Moreover, as already described,4 treatment of patients with thalassemia major in specialized centers of excellence plays an important role in improving their survival.
Overall, these findings show that the majority of patients diagnosed with thalassemia major do not experience psychosocial and mental problems, and are in contrast with studies conducted in Italy8 and other countries18,19 that show striking impairments in social functioning, role-emotional, and mental component summary scores. Some researchers have identified and studied the characteristics of the psychosocial burden of thalassemia, focusing on social isolation, self-esteem, family adjustment, education, and sporting activity. Psychosocial problems associated with thalassemia include feelings of distress, poor social functioning, such as integration into school and work,16 and expression of guilt, denial, and overprotectiveness of families.20,21
Poor QoL in patients with thalassemia major is probably due to a complex combination of living with a chronic disease17 and new challenges related to improved life expectancy in thalassemia. It is important to bear in mind that QoL is a social construct influenced by cultural and contextual variables. One possible explanation for our findings could be that treatment in a specialized center, which is able to guarantee the best care for patients with thalassemia major, could increase the perception of QoL in these patients.4
One potential limitation of this study is related to the exclusive involvement of patients from Liguria. However, we do not have evidence suggesting that the results of this study cannot be considered valid in other populations of patients with characteristics similar to those of patients participating in this study.
It is possible that other factors, such as introduction of psychiatric or psychologic counseling, might have contributed to improvement in the mental QoL dimension. Between 2001 and 2009, no specific psychiatric or psychologic support was available for these patients at the treatment center. However, it is impossible to exclude the possibility that some patients have been followed by other services or by health professionals in the private sector. Further surveys, focused on identifying factors associated with this improvement, will need to be performed.
The importance of assessing QoL in patients with thalassemia has been highlighted by other authors.9,22 Further studies are required to establish the relationship between thalassemia and the psychosocial profile of patients with the disease, taking into account demographic, clinical, and therapeutic variables. As we continue to make medical advances and improve the life expectancy of patients with thalassemia, QoL will become an even more important marker of treatment success. The improvement in all scales related to mental health and the significant improvement in the overall mental scale observed in this survey supports the implementation of effective interventions for screening the QoL of patients with thalassemia major and improving the physical and psychosocial well-being of these patients.
The observed improvement in pain control is very interesting. During recent years, the importance of better recognition and treatment of pain in patients affected by chronic disease has been stressed by many international agencies.23 These results suggest that, at least in patients with thalassemia major, an improvement is possible. Further studies are needed to investigate the prevalence of pain and its impact on QoL dimensions in these patients.
The fact that the SF-36 is widely validated and accepted in many countries makes it a good choice for standard assessment of patients with thalassemia. The improvement in mental QoL dimensions that emerges from our findings indicates that implementation of effective interventions for screening and supporting the psychosocial well-being of these patients is now urgent.
Acknowledgment
The authors thank Silvia Caviglia for her help in editing this paper.
Footnotes
Disclosure
The authors report no potential conflicts of interests in this work.
References
- 1.Telfer P. Update on survival in thalassemia major. Hemoglobin. 2009;33( Suppl 1):S76–S80. doi: 10.3109/03630260903347336. [DOI] [PubMed] [Google Scholar]
- 2.Borgna-Pignatti C, Rugolotto S, De Stefano P, et al. Survival and complications in patients with thalassemia major treated with transfusion and deferoxamine. Haematologica. 2004;89:1187–1193. [PubMed] [Google Scholar]
- 3.Modell B, Khan M, Darlison M, Westwood MA, Ingram D, Pennell DJ. Improved survival of thalassaemia major in the UK and relation to T2* cardiovascular magnetic resonance. J Cardiovasc Magn Reson. 2008;10:42. doi: 10.1186/1532-429X-10-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Forni GL, Puntoni M, Boeri E, Terenzani L, Balocco M. The influence of treatment in specialized centers on survival of patients with thalassemia major. Am J Hematol. 2009;84:317–318. doi: 10.1002/ajh.21398. [DOI] [PubMed] [Google Scholar]
- 5.Galanello R. A thalassemic child becomes adult. Rev Clin Exp Hematol. 2003;7:4–21. [PubMed] [Google Scholar]
- 6.Musallam K, Cappellini MD, Taher A. Challenges associated with prolonged survival of patients with thalassemia: transitioning from childhood to adulthood. Pediatrics. 2008;121:e1426–e1429. doi: 10.1542/peds.2007-1944. [DOI] [PubMed] [Google Scholar]
- 7.Anie KA, Massaglia P. Psychological therapies for thalassaemia. Cochrane Database Syst Rev. 2001;3:CD002890. doi: 10.1002/14651858.CD002890. [DOI] [PubMed] [Google Scholar]
- 8.Messina G, Colombo E, Cassinerio E, et al. Psychosocial aspects and psychiatric disorders in young adult with thalassemia major. Intern Emerg Med. 2008;3:339–343. doi: 10.1007/s11739-008-0166-7. [DOI] [PubMed] [Google Scholar]
- 9.Payne KA, Rofail D, Baladi JF, et al. Iron chelation therapy: clinical effectiveness, economic burden and quality of life in patients with iron overload. Adv Ther. 2008;25:725–742. doi: 10.1007/s12325-008-0085-z. [DOI] [PubMed] [Google Scholar]
- 10.Mikelli A, Tsiantis JJ. Depressive symptoms and quality of life in adolescents with b-thalassaemia. J Adolesc. 2004;27:213–216. doi: 10.1016/j.adolescence.2003.11.011. [DOI] [PubMed] [Google Scholar]
- 11.Telfer P, Coen PG, Christou S, et al. Survival of medically treated thalassemia patients in Cyprus. Trends and risk factors over the period 1980–2004. Haematologica. 2006;91:1187–1192. [PubMed] [Google Scholar]
- 12.Di Palma A, Vullo C, Zani B, Facchini A. Psychosocial integration of adolescents and young adults with thalassemia major. Ann N Y Acad Sci. 1998;850:355–360. doi: 10.1111/j.1749-6632.1998.tb10493.x. [DOI] [PubMed] [Google Scholar]
- 13.Ware JE, Sherbourne CD. The MOS 36-Item Short Form Health Survey (SF-36); conceptual framework and item selection. Med Care. 1992;30:473–483. [PubMed] [Google Scholar]
- 14.Ware JE, Jr, Gandek B, Kosinski M, et al. The equivalence of SF-36 summary health scores estimated using standard and country-specific algorithms in 10 countries: results from the IQOLA Project. International Quality of Life Assessment. J Clin Epidemiol. 1998;51:1167–1170. doi: 10.1016/s0895-4356(98)00108-5. [DOI] [PubMed] [Google Scholar]
- 15.Ware JE, Keller SD, Gandek B, Brazier JE, Sullivan M IQOLA Project Group. Evaluating translations of health status questionnaires: methods from IQOLA project. Int J Technol Assess Health Care. 1995;11:525–551. doi: 10.1017/s0266462300008710. [DOI] [PubMed] [Google Scholar]
- 16.Apolone G, Mosconi P. The Italian SF-36 Health Survey: translation, validation and norming. J Clin Epidemiol. 1998;51:1025–1036. doi: 10.1016/s0895-4356(98)00094-8. [DOI] [PubMed] [Google Scholar]
- 17.Sobota A, Yamashita R, Xu Y, et al. Quality of life in thalassemia: a comparison of SF-36 results from the thalassemia longitudinal cohort to reported literature and the US norms. Am J Hematol. 2011;86:92–95. doi: 10.1002/ajh.21896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mednick L, Yu S, Trachtenberg F, et al. Symptoms of depression and anxiety in patients with thalassemia: prevalence and correlates in the thalassemia longitudinal cohort. Am J Hematol. 2010;85:802–805. doi: 10.1002/ajh.21826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Khani H, Majdi MR, Azad Marzabadi E, Montazeri A, Ghorbani A, Ramezani M. Quality of life of Italian β-thalassemia major patients living on the southern coast of the Caspian Sea. East Mediterr Health J. 2012;18:539–545. doi: 10.26719/2012.18.5.539. [DOI] [PubMed] [Google Scholar]
- 20.Masera G, Monguzzi W, Tornotti G, Lo Iacono B, Pertici S, Spinetta J. Psychosocial support in thalassemia major: Monza center’s experience. Haematologica. 1990;75( Suppl 5):181–190. [PubMed] [Google Scholar]
- 21.Mazzone L, Battaglia L, Andreozzi F, Romeo MA, Mazzone D. Emotional impact in beta-thalassaemia major children following cognitive-behavioural family therapy and quality of life of caregiving mothers. Clin Pract Epidemiol Ment Health. 2009;5:5–10. doi: 10.1186/1745-0179-5-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Telfer P, Constantinidou G, Andreou P, Christou S, Modell B, Angastiniotis M. Quality of life in thalassemia. Ann N Y Acad Sci. 2005;1054:273–282. doi: 10.1196/annals.1345.035. [DOI] [PubMed] [Google Scholar]
- 23.Editorial. Pain control – a basic kindness. Lancet. 2012;379:2024. doi: 10.1016/S0140-6736(12)60877-0. [DOI] [PubMed] [Google Scholar]