Summary
Background:
Strongyloidiasis, a common intestinal parasitic infection, is endemic in tropical and subtropical regions and occurs sporadically in temperate areas. It is endemic in Guilan province, Iran, and especially affects the rural population.
Case Report:
We report the case of a 43-year-old woman living in Anzali (in the north of Iran), with dyspepsia and epigastric pain for 2 years, unresponsive to H2 receptor antagonists and proton pump inhibitors. Upper gastrointestinal endoscopy was done and showed multiple small nodules at the stomach. The pathologist reported Strongyloides. Treatment with Ivermectin and antibiotic triple therapy was done. She responded well to treatment and 6 months later an upper gastrointestinal endoscopy revealed no significant lesions and all nodules had disappeared.
Strongyloidiasis is usually not severe and frequently is nonspecific. For this reason, the infection is easily ignored by both the patients and physicians.
Conclusions:
Although gastric involvement shows nonspecific symptoms, the possibility should be carefully considered by clinicians who practice in endemic areas.
Keywords: Strongyloides stercoralis, stomach, strongyloidiasis
Background
Strongyloidiasis, a common intestinal parasite infection, is endemic in tropical and subtropical regions and occurs sporadically in temperate areas. In tropical and subtropical regions the overall regional prevalence may exceed 25% [1,2]. It is a prevalent parasitic infection in some rural areas in the north of Iran [3]. The human infection begins when human skin contacts the infective filariform larvae of Strongyloides stercoralis, which are found in soil or other materials contaminated with human feces [4,5]. The filariform larvae penetrate the skin and migrate hematogenously to the lungs where they penetrate into the alveolar sacs. The larvae then ascend the airways into the tracheobronchial tree and are swallowed. The larvae mature into adult worms in the mucosa of the duodenum and jejunum. Adult female worms parasitizing the human small intestine lay eggs in the intestinal mucosa that hatch into rhabditiform larvae, which are shed in the stool [6].
Clinical manifestations of infection can range from asymptomatic eosinophilia in the immunocompetent host [7] to disseminated disease with sepsis in the immunocompromised host [8]. The adult worms in the small bowel induce duodenitis, which can lead to upper abdominal pain and some non-specific symptoms [7]. Although S. Stercoralis may infect many organs in hyperinfection, the involvement of the stomach is relatively rare [9,10].We report the case of a patient with involvement of the stomach by S. stercoralis, and we review the literature.
Case Report
A 43-year-old female farmer living in Anzali (northern Iran), sought medical attention for dyspepsia and epigastric pain for 2 years unresponsive to H2 receptor antagonists and proton pump inhibitors. The pain radiated to her back and mimic an upper gastrointestinal ulcer. Food ingestion aggravated the pain. She was referred to our center for further evaluation including an upper gastrointestinal endoscopy. Her medical history revealed that she had mild and intermittent asthma responsive to bronchodilator therapy. A physical examination revealed mild epigastric tenderness and she had a mild eosinophilia. All other investigations were unremarkable. An upper gastrointestinal endoscopy revealed multiple small nodules at the fundus and body (Figure 1). Multiple biopsies were taken from nodules and other parts of the stomach. The duodenum was normal endoscopically but biopsies were taken from the 1{st and 2{nd parts. The pathologists reported that many strongyloid larvae had invaded the gastric (Figure 2) and duodenal mucosa (Figure 3). Helicobacter pylori infection was also reported. Treatment was begun with Ivermectin 200 {mg/kg orally. Antibiotic triple therapy by Amoxicillin 500 mg twice daily, Omeprazole 20 mg daily and Clarithromycin 500 mg twice daily was started and continued for 14 days. She responded well to this treatment and 6 months later an upper gastrointestinal endoscopy revealed no significant lesions and all nodules had disappeared.
Figure 1.
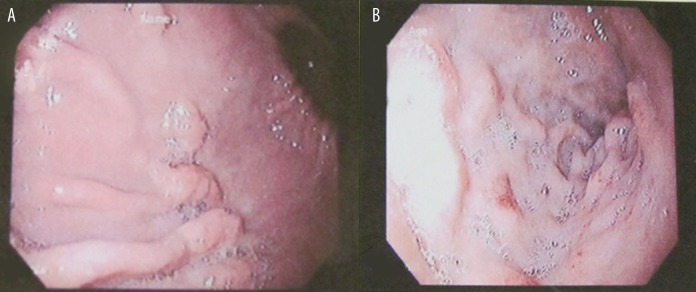
Endoscopic finding evidenced (A) multiple gastric nodules in stomach as an infiltrative lesion (B) Duodenal erosions.
Figure 2.
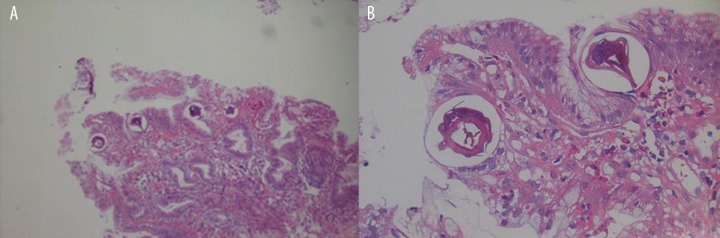
Histological aspects of gastric strongyloidiasis: (A) section of parasite adult worm in gastric biopsy is observed (hematoxylin-eosin, magnification ×250). (B) gastric biopsies revealed the presence of larvae within glandular lumens (hematoxylin-eosin, magnification ×400).
Figure 3.
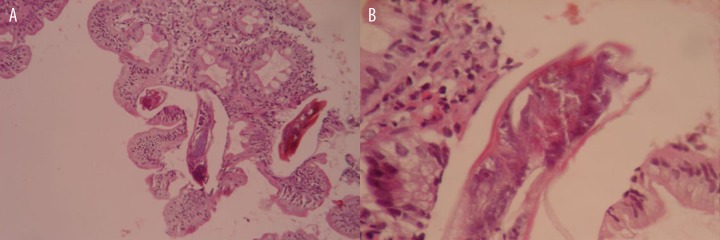
Histologic aspects of duodenal strongyloidiasis: (A) section of parasite larvae in duodenal biopsy is observed (hematoxylin-eosin, magnification ×100). (B) gastric biopsies revealed the presence of larvae (hematoxylin-eosin, magnification ×400).
Discussion
Strongyloidiasis is a worldwide parasitic infection distributed in humid and hot areas of the world. The intestinal Strongyloides has a great importance because the filariform larvae can be disseminated by autoinfection in immunocompromised hosts [11]. Gastrointestinal symptoms are most common but are nonspecific. Some case reports do not mention any gastrointestinal symptoms [12] but symptoms such as abdominal pain, often described as “crampy”, bloating, watery diarrhea, constipation, anorexia, weight loss, nausea and vomiting have been reported [13].
The parasitic females of S. stercoralis usually live in the crypts of the proximal small intestine, producing eggs that convert into rhabditoid larvae in the mucosa. Due to low gastric pH, the stomach is not an appropriate site for S. stercoralis; achlorhydria and reduced gastric acid secretion might be an important risk factor for this infection [14]. It seems that the organisms reach the stomach via swallowing sputum or retrograde migration from the proximal small intestine [15]. According to patients age and her protracted symptoms unresponsive to H2-receptor antagonist and proton pump inhibitor, she was a candidate for an upper gastrointestinal endoscopy. At gastroscopy, multiple nodules (Figure 1) and decreased gastric dispensability were evidence of gastric infiltrative lesions. The pathologist reported gastric worm infestation compatible with gastric strongyloidiasis. In our case, chronic acid suppression might have been a predisposing condition. We could not find any evidence of immunodeficiency. The patient used both Ranitidine and Omeprazole since 6 months ago. Yaldiz et al. reported another case of gastric strongyloidiasis from Turkey, an elderly man who was treated with antacid and had been a heavy drinker for many years [16]. Wurtz et al. reported another case taking prednisone and an H2 blocker who developed hyperinfection syndrome, with mucosal Strongyloides larvae seen in a gastric biopsy [17]. Kim et al. reported the case of a 69-year-old Korean man with complaints of abdominal pain, vomiting, and diarrhea. His gastric mucosa showed whitish mottled and slightly elevated lesions on the body angle of antrum and many adult worms, larvae, and eggs in cross-sections were located in the crypts. He was treated intravenously with prednisolone and orally with ranitidine 3 weeks before diagnosis [15]. All of the reported cases mentioned above had a history of corticosteroid use, but our patient denied any use of corticosteroid drugs.
Although significant male dominance has been mentioned in the literature and some reported cases were males [15–18], especially old men, our patient was a middle-aged woman.
Rodríguez Calabuig et al. showed that the only occupational activity influencing risk of strongyloidiasis is working in rice fields, with an OR of 2.97 (95% CI: 1.16–7.71) [19]. The most common mode of infection by strongyloid worms is penetration of the Strongyloides larvae through the skin during contact with contaminated soil. Our patient was a farm worker in a rice field and sometimes walked barefoot.
Gastric strongyloidiasis can complicate gastric ulcers and induce massive bleeding, but our patient had mild symptoms [20]. Strongyloidiasis may mimic new-onset asthma or an exacerbation of asthma, COPD, or pulmonary embolism [21]. Our patient had already been treated as an asthmatic patient. Her pulmonary symptoms could be attributed to this infection because her symptoms significantly improved after treatment of infection. Clinicians must maintain a high level of suspicion for patients from endemic areas presenting with new-onset wheezing [21].
In our patient, the microscopic findings included Helicobacter pylori-induced gastritis and a number of parasites in the stomach and duodenum. Unless heavily infected, the clinical features reported in strongyloidiasis are usually not so severe, and frequently are nonspecific.
Conclusions
Strongyloidiasis is easily ignored by both the patients and physicians. Although gastric involvement shows nonspecific symptoms in strongyloidiasis, the possibility should be carefully considered by clinicians who practice in endemic areas.
References:
- 1.Gyorkos TW, Genta RM, Viens P, MacLean JD. Seroepidemiology of Strongyloides infection in the Southeast Asian refugee population in Canada. Am J Epidemiol. 1990;132(2):257–64. doi: 10.1093/oxfordjournals.aje.a115655. [DOI] [PubMed] [Google Scholar]
- 2.Posey DL, Blackburn BG, Weinberg M, et al. High prevalence and presumptive treatment of schistosomiasis and strongyloidiasis among African refugees. Clin Infect Dis. 2007;45(10):1310–15. doi: 10.1086/522529. [DOI] [PubMed] [Google Scholar]
- 3.Koosha S, Kazemi B, Bonyadi F. The 18S Ribosomal DNA Sequence of Strongyloides stercoralis in Iran. Iranian J Parasitol. 2009;4:53–58. [Google Scholar]
- 4.Schupf N, Ortiz M, Kapell D, Kiely M. Prevalence of intestinal parasite infections among individuals with mental retardation in New York State. Ment Retard. 1995;33(2):84–89. [PubMed] [Google Scholar]
- 5.Lindo JF, Robinson RD, Terry SI, et al. Age-prevalence and household clustering of Strongyloides stercoralis infection in Jamaica. Parasitology. 1995;110(1):97–102. doi: 10.1017/s0031182000081099. [DOI] [PubMed] [Google Scholar]
- 6.Merkell EK, John DT, Krotoski WA. Markel Voge’s Medical Parasitology. 8{nd ed. Philadelphia: W.B. Saunders Company; 1999. [Google Scholar]
- 7.Scowden EB, Schaffner W, Stone WJ. Overwhelming strongyloidiasis: an unappreciated opportunistic infection. Medicine. 1978;57(6):527–44. [PubMed] [Google Scholar]
- 8.Shafaghi A, Akhavan K, Hajizade H, Mansour-Ghanaei F. Disseminated strongyloidiasis following high-dose prednisolone administration. The American Journal of Case Report. 2010;11:74–77. [Google Scholar]
- 9.Igra-Siegman Y, Kapila R, Sen P, et al. Syndrome of hyperinfection with Strongyloides stercoralis. Rev Infect Dis. 1981;3:397–407. doi: 10.1093/clinids/3.3.397. [DOI] [PubMed] [Google Scholar]
- 10.Wurtz R, Mirot M, Fronda G, et al. Short report: gastric infection by Strongyloides stercoralis. Am J Trop Med Hyg. 1994;51(3):339–40. doi: 10.4269/ajtmh.1994.51.339. [DOI] [PubMed] [Google Scholar]
- 11.Hong SJ, Han JH. A case of Strongyloides stercoralis infection. Korean J Parasitol. 1999;37(2):117–20. doi: 10.3347/kjp.1999.37.2.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ronan SG, Reddy RL, Manaligod JR, et al. Disseminated strongyloidiasis presenting as purpura. J Am Acad Dermatol. 1989;21:1123–25. doi: 10.1016/s0190-9622(89)70311-x. [DOI] [PubMed] [Google Scholar]
- 13.Liepman M. Disseminated Strongyloides stercoralis. A complication of immunosuppression. JAMA. 1975;231(4):387–88. [PubMed] [Google Scholar]
- 14.Gianella RA, Broitman SA, Zamcheck N. Influence of gastritis acidity on bacterial and parasitic enteric infections. Ann Intern Med. 1973;78:271–76. doi: 10.7326/0003-4819-78-2-271. [DOI] [PubMed] [Google Scholar]
- 15.Kim J, Joo HS, Kim DH, et al. A case of gastric strongyloidiasis in a Korean patient. Korean J Parasitol. 2003;41(1):63–67. doi: 10.3347/kjp.2003.41.1.63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yaldiz M, Hakverdi S, Aslan A, et al. Gastric infection by Strongyloides stercoralis: A case report. Turk J Gastroenterol. 2009;20(1):48–51. [PubMed] [Google Scholar]
- 17.Wurtz R, Mirot M, Fronda G, et al. Short report: gastric infection by Strongyloides stercoralis. Am J Trop Med Hyg. 1994;51(3):339–40. doi: 10.4269/ajtmh.1994.51.339. [DOI] [PubMed] [Google Scholar]
- 18.Shekhar KC, Krishnan R, Pathmanathan R, Fook CS. Gastric strongyloidiasis in a Malaysian patient. Southeast Asian J Trop Med Public Health. 1997;28(1):158–60. [PubMed] [Google Scholar]
- 19.Rodríguez Calabuig D, Igual Adell R, Oltra Alcaraz C, et al. Agricultural occupation and strongyloidiasis. A case-control study. Rev Clin Esp. 2001;201(2):81–84. doi: 10.1016/s0014-2565(01)70755-2. [DOI] [PubMed] [Google Scholar]
- 20.Dees A, Batenburg PL, Umar HM, et al. Strongyloides stercoralis associated with a bleeding gastric ulcer. Gut. 1990;31(12):1414–15. doi: 10.1136/gut.31.12.1414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Newberry AM, Williams DN, Stauffer WM, et al. Strongyloides Hyperinfection Presenting as Acute Respiratory Failure and Gram-Negative Sepsis. CHEST. 2005;128:3681–84. doi: 10.1378/chest.128.5.3681. [DOI] [PMC free article] [PubMed] [Google Scholar]


