Summary
Background:
Pregnancy can precipitate cardiac arrhythmias not previously present in seemingly well individuals. Atrial and ventricular premature beats are frequently present during pregnancy and are usually benign. Supraventricular tachycardia and malignant ventricular tachyarrhythmias occur less frequently. Maternal and fetal arrhythmias occurring during pregnancy may jeopardize the life of the mother and the fetus.
Case Report:
A 32-year-old pregnant women at 26 weeks gestation presented to the emergency department with palpitation. She had mild chest discomfort after a supraventricular tachycardia (SVT) episode but did not have syncope. After monitoring and access of an IV line, vagal manoeuvres were applied but the rhythm was resistant. Then she was treated with 5 mg metoprolol IV, but the SVT persisted. Then after IV infusion of adenosine triphosphate 6 to 12 mg, the rhythm was resistant. Synchronized cardioversion with 100 joules was performed. Patients’ rhythm was normalized to a sinus rhythm. She was discharged from hospital without any adverse effects following 24-hour monitoring.
Conclusions:
All pregnant patients with SVT require careful maternal and fetal monitoring during treatment, and close collaboration between the managing obstetrician and the cardiologist is essential.
Keywords: supraventricular tachycardia, pregnancy, clectrical cardioversion
Background
Cardiac arrhythmias are frequently seen during pregnancy. Among these, supraventricular arrhythmias are of great concern, especially when the patient is pregnant. Arrhythmias that occur during pregnancy are almost always benign and require no treatment [1]. Nonetheless, severe symptomatic arrhythmias require immediate and accurate management. Maternal arrhythmia incidence is expected to be 1.2 per 1000 in the pregnant population [2]. This article describes a case of supraventricular arrhythmia during pregnancy and its treatment with electrical cardioversion.
Case Report
A 32-year-old patient, 26 weeks pregnant, was admitted to the emergency department with mild chest pain and tachycardia lasting for an hour. She had an uncomplicated pregnancy with a history of thyroidectomy 3 years ago. She was on a daily 75 mg levothyroxine medication and had no previous history of cardiac or thrombo-embolic disease. Physical examination was normal except for a tachycardic pulse. Blood pressure was 110/70 mmHg and oxygen saturation was 98%. There was no peripheral edema. Anaemia and other systemic disorders were excluded. Tyroid function tests were within normal limits. There was no diameter difference between calves. The patient was not tachypneic. Her arterial blood gases revealed no hypoxemia and hypocarbia. Echocardiogram showed no structural abnormalities. The electrocardiographic record revealed a supraventricular tachycardia with a rate of 230 beats per minute (Figure 1).
Figure 1.
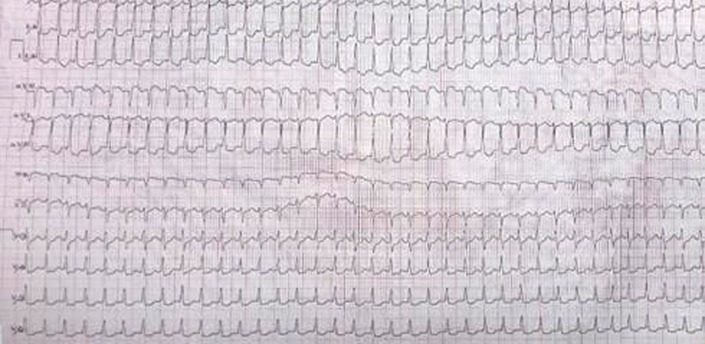
Supraventricular tachycardia with a rate of 230 beats.
Patient was monitored and hydrated and vagal maneuver was applied immediately, but the rhythm was resistant. Five mg of metoprolol was administered as a second step to control supraventricular rate, but there was no change in arrhythmia. Then after IV infusion of adenosine triphosphate 6 to 12 mg, the rhythm was resistant.
Due to persistence of arrhythmia, a fall in blood pressure to 60 mmHg systolic and 40 mmHg diastolic, and an altered state of consciousness, the patient was referred to a cardiologist. Synchronized cardioversion with 100 joules was performed and the patient’s rhythm was normalized to a sinus rhythm of 90 beats per minute (Figure 2). The patient was stabilized and admitted to the intensive care unit. Obstetric ultrasonography revealed a healthy fetus with normal cardiac activity.
Figure 2.
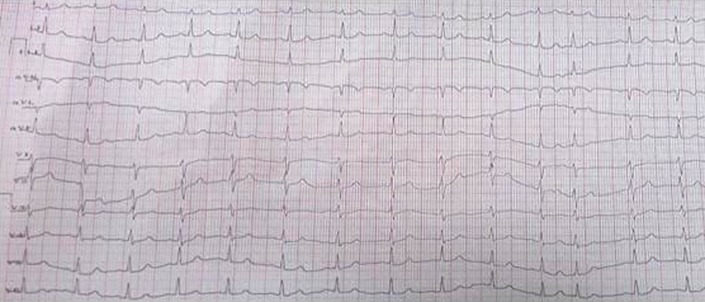
Sinus rhytm after synchronized with 100 joules.
Discussion
There are substantial changes in hormonal and hemodynamic states of pregnant women that may lead to arrhythmias [3,4]. Atrial and ventricular premature beats are frequent during pregnancy and are generally benign. Supraventricular tachycardias and malign ventricular arrhythmias are less frequent. Arrhythmias such as atrial, ventricular or nodal complex tachycardias, sinoatrial arrest, wandering atrial pacemaker, sinus tachycardia and paroxysmal ventricular tachycardias occur during pregnancy [5].
Supraventricular tachycardia is generally seen in women of reproductive age. Its relationship with pregnancy and mechanism of exacerbation are unclear, but a hyperdynamic state of pregnancy may be a key factor [5].
There is generally no need for drug therapy in supraventricular and ventricular premature beats,; however, potential stimulants like caffein and alcohol should be avoided. Acute treatment of arrhythmias in pregnant patients is similar to that of non-pregnant women, except for a few exceptional cases [4,5]. The first-line of treatments for benign arrhythmias are conservative approaches like observation, rest and vagal maneuvers. Drugs that have no fetal effects should be used in more severe and symptomatic arrhythmias. Drugs with relatively low risk and good tolerability should be preferred, as no antiarrhythmic drug is safe during pregnancy [1,3,6,7].
Arrhythmias disturbing hemodynamic stability should be treated due to potential harm to fetus as a result of maternal hypotension [5,7]. Adenosine is a safe and preferred drug in the treatment of supraventricular tachycardias in pregnancy. Digoxin is another choice for treatment of arrhythmias in pregnant patients [8,9]. Among the many medications used in the treatment of supraventricular tachycardias, only calcium channel blockers have tocolytic effects [10].
Electrical cardioversion is effective in the treatment of maternal supraventricular arrhythmias and should be used immediately when drugs fail [1,6,11]. Electrical cardioversion of 50–100 joules is indicated in the acute treatment of all patients with unstable hemodynamics [2,8] and the energy applied varies from 50 to 400 J [12]. However, 2 maternal deaths assumed to be due to electrical cardioversion have been reported [13,14]. Radiofrequency ablation of arrhythmogenic substrate, which has rarely been performed during pregnancy, is an effective treatment of drug-refractory maternal supraventricular tachycardias in advanced pregnancy [15].
Conclusions
Treatment of rhythm disturbances during pregnancy must be well justified. No antiarrhythmic drug is absolutely safe in pregnancy. Arrhythmias during pregnancy should initially be managed conservatively. Antiarrhythmics should be reserved for symptomatic cases. Electrical cardioversion is an effective method, with favorable tolerability.
References:
- 1.Trappe HJ. Acute therapy of maternal and fetal arrhythmias during pregnancy. J Intensive Care Med. 2006;21:305–15. doi: 10.1177/0885066606291433. [DOI] [PubMed] [Google Scholar]
- 2.Tromp CH, Nanne AC, Pernet PJ, et al. Electrical cardioversion during pregnancy: safe or not? Neth Heart J. 2011;19(3):134–36. doi: 10.1007/s12471-011-0077-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Robins K, Lyons G. Supraventricular tachycardia in pregnancy. Br J Anaesth. 2004;92:140–43. doi: 10.1093/bja/aeh004. [DOI] [PubMed] [Google Scholar]
- 4.Wolbrette D. Treatment of arrhythmias during pregnancy. Curr Womens Health Rep. 2003;3(2):135–39. [PubMed] [Google Scholar]
- 5.Gowda RM, Khan IA, Mehta NJ, et al. Cardiac arrhythmias in pregnancy: clinical and therapeutic considerations. Int J Cardiol. 2003;88:129–33. doi: 10.1016/s0167-5273(02)00601-0. [DOI] [PubMed] [Google Scholar]
- 6.Tan HL, Lie KI. Treatment of tachyarrhythmias during pregnancy and lactation. Eur Heart J. 2001;22:458–64. doi: 10.1053/euhj.2000.2130. [DOI] [PubMed] [Google Scholar]
- 7.Chow T, Galvin J, McGovern B. Antiarrhythmic drug therapy in pregnancy and lactation. Am J Cardiol. 1998;82(4A):581–621. doi: 10.1016/s0002-9149(98)00473-1. [DOI] [PubMed] [Google Scholar]
- 8.Joglar JA, Page RL. Treatment of cardiac arrhythmias during pregnancy; safety considerations. Drug Saf. 1999;20(1):85–94. doi: 10.2165/00002018-199920010-00008. [DOI] [PubMed] [Google Scholar]
- 9.Hagley MT, Cole PL. Adenosine use in pregnant women with supravetricular tachycardia. Ann Pharmacother. 1994;28(11):1241–42. doi: 10.1177/106002809402801105. [DOI] [PubMed] [Google Scholar]
- 10.Ou KY, Yang CH, Tsai EM, et al. Choosing calcium channel blockers for pregnant womwn with paroxysmal supraventricular tachycardia and pre-term labor: a case report. Kaohsiung J Med Sci. 2004;20(9):457–60. doi: 10.1016/s1607-551x(09)70185-8. [DOI] [PubMed] [Google Scholar]
- 11.Barnes EJ, Eben F, Patterson D. Direct current cardioversion during pregnancy should be performed with facilities available for fetal monitoring and emergency caesarean section. BJOG. 2002;109:1406–7. doi: 10.1046/j.1471-0528.2002.02113.x. [DOI] [PubMed] [Google Scholar]
- 12.Paziaud O, Piot O, Rousseau J, et al. Predictive criteria of early recurrence of atrial arrhythmia after reduction by electrical cardioversion. Arch Mal Coeur Vaiss. 2003;96:1169–74. [PubMed] [Google Scholar]
- 13.Klepper I. Cardioversion in late pregnancy. The anaesthetic management of a case of Wolff-Parkinson-White syndrome. Anaesthesia. 1981;36:611–16. doi: 10.1111/j.1365-2044.1981.tb10325.x. [DOI] [PubMed] [Google Scholar]
- 14.Meitus ML. Fetal electrocardiography and cardioversion with direct current countershock. Report of a case. Dis Chest. 1965;48:324–25. doi: 10.1378/chest.48.3.324. [DOI] [PubMed] [Google Scholar]
- 15.Bombelli F, Lagona F, Salvati A, et al. Radiofrequency catheter ablation in drug refractory maternal supraventricular tachycardias in advanced pregnancy. Obstet Gynecol. 2003;102(5 Pt 2):1171–73. doi: 10.1016/s0029-7844(03)00119-4. [DOI] [PubMed] [Google Scholar]


