Summary
Background:
Technical problems such as graft and vascular size are more common in living donor liver transplantation (LDLT) than in deceased donor liver transplantation. It is usually possible to get enough length of vessels on the graft, but the opposite situation is devastating. Finding the suitable vessel graft is life-saving in those situations. In this paper we present a case of gonodal vein interpositioning for hepatic artery reconstruction in an LDLT recipient. To the best of our knowledge, this is the first such case to be reported in the literature.
Case Report:
A 36-year-old man with cirrhosis secondary to hepatitis B underwent LDLT. Within minutes after completing the anastomosis, the artery was thrombosed. Disrupting the anastomosis showed subintimal dissection of the recipient right hepatic artery extending to the gastro-duodenal junction. A 4 cm segment of gonodal vein, which matched the diameter of the recipient hepatic artery, was used as a bridge. The patient’s postoperative recovery was excellent and Doppler ultrasonography demonstrated sufficient hepatic arterial blood flow. At long-term follow-up (18th months), the patient’s graft is still functioning.
Conclusions:
Gonodal vein interposition for hepatic artery reconstruction in living donor liver transplantation has not been previously reported. In light of the urgency of this situation, we believe it can be a life-saving reconstruction.
Keywords: liver transplantation, hepatic artery, gonodal vein
Background
Living donor liver transplantation (LDLT) is a realistic solution for end-stage cirrhotic patients in countries with a shortage of deceased donor organs, such as in Turkey [1–3]. To overcome this obstacle, many transplantation centers have started living donor programs in our country. Technical problems such as graft and vascular size are more common in living donor liver transplantation than in deceased donor liver transplantation. Adequate hepatic arterial reconstruction is essential and critical for successful liver transplantation [2,4]. With microsurgical techniques, the vascular anatomy has become a rare reason for excluding someone from donation [3]. Suitable length of vascular structures is essential for reconstruction of vessels. It is usually possible to get enough length of vessels on the graft, but the opposite situation is devastating. In those situations, to find the suitable vessel graft is life-saving. Various options are available when recipient hepatic arteries are not suitable for reconstruction [2]. The length and diameter of the vessels of these grafts may necessitate complex reconstruction, including interposition grafts [3]. In this paper we present the first case of gonodal vein interpositioning for hepatic artery reconstruction due to subintimal dissection of the right hepatic artery in a living donor liver transplantation recipient.
Case Report
A 36-year-old man with cirrhosis secondary to hepatitis B was admitted to our center for living related donor liver transplantation. The organ was from his blood type-compatible 20-year-old son. Both patients were evaluated by our transplant team. Pre-transplantation assessment did not reveal any pathological findings. Computerized tomography angiography showed that the right lobe of the liver was 1055 grams (total: 1590 grams).
The donor operation was performed through bilateral subcostal incision. Preoperative Doppler ultrasonography (US) examination and cholangiography were obtained. Parenchymal transection was performed with crush-clamp technique without any blood product transfusion required. The graft was taken to a back table and flushed with 250 cc of Euro Collins solution via the portal vein and hepatic artery. Any leaks from the cut surface were checked during perfusion of the biliary system.
In the recipient operation, each structure in the portal hilus was dissected separately but not divided until the graft was ready to be taken out, with the exception of the cystic duct, which was divided at the beginning of the portal dissection. The native liver was removed by piggy-back technique. During the unhepatic phase, hepatitis B immunoglobulin (2000 IU) (Hepatect-CP Flakon 500 IU/10 ml, Kansuk) was given intramuscularly. After retrograde perfusion of the graft, the right hepatic artery was anastomosed to the graft artery under a microscope with 12× magnification (Zeiss S8, Germany). Within minutes after completing the anastomosis, the artery was thrombosed. Disrupting the anastomosis showed that there was a subintimal dissection of the right hepatic artery extending to the gastro-duodenal junction. Then the artery was dissected from beneath this junction where the intima was intact.
After removal of that subintimal dissected segment of the artery, a gap appeared between the graft and the recipient hepatic artery. Since the diameter of hepatic artery was 3 mm, it was decided to interpose with gonodal vein. The right colon was mobilized, a 4 cm segment of the right gonodal vein, which matched the diameter of the recipient hepatic artery, was removed. Proximal and distal anastomosis of the graft was made under microscope with 8/0 interrupted Prolene sutures (Figure 1). Finally, duct-to-duct anastomosis of the common bile duct over a T-tube was performed, 2 drainage tubes were placed and the abdomen was closed. The patient was transferred to the intensive care unit. The first Doppler US examination showed an excellent arterial flow. Twelve hours later, the patient was transferred to the transplantation floor. Again, Doppler US showed normal arterial blood flow to the grafted liver through the gonadal vein interposition. For the first 3 days, Doppler US examination was performed twice daily. The patient was given low molecular weight heparin 0.4 cc per day for 2 weeks. Tacrolimus-based triple immunosuppressive regimen was started with tapering of steroids. After discharge the patient was given only acetyl salicylic acid 100 mg per day. On the third day Doppler US examination was as shown in Figure 2. At 18-month follow-up the patient’s graft is still functioning.
Figure 1.
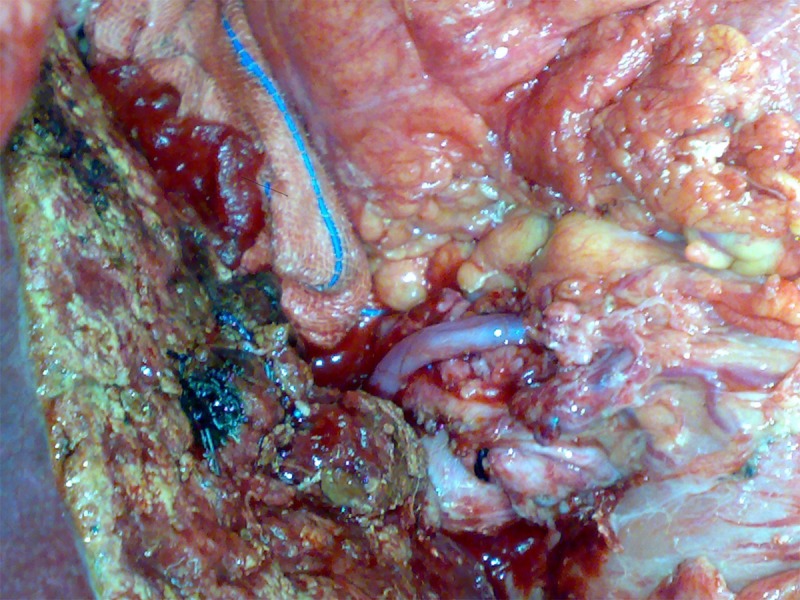
Hepatic artery reconstruction with right gonodal vein.
Figure 2.
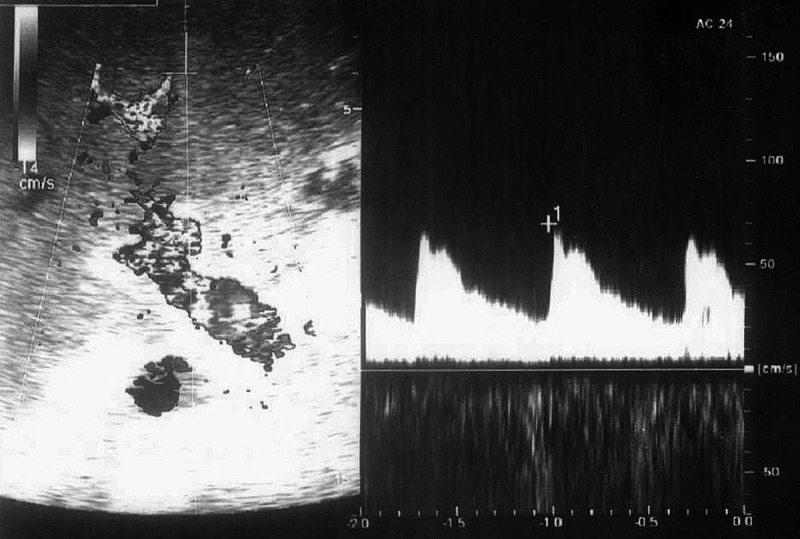
Doppler examination.
Discussion
Intimal dissection of hepatic artery is a devastating complication for liver transplant recipients, and is even worse in living donor liver transplantation due to the absence of sufficient and available artery grafts. Once the intimal dissection and thrombosis of the hepatic artery occurs it must be re-canalized during the operation, otherwise the graft will be lost in most cases. Since the dissected segment of the artery is the main cause of the thrombosis, it has to be excised to where normal intima exists. The distance between native and graft artery has to be bridged with proper grafts.
In the history of the living donor liver transplantation, many kinds of artery and vein grafts have been used, such as deceased donor arteries (fresh or stored), autogenous saphenous vein, right gastroepiploic artery, splenic artery, sigmoid artery, recipient inferior mesenteric vein, and jejunal arterial arcade of Roux-en – Y limb [1–5].
The use of the gonadal vein for reconstruction has some advantages. Its removal does not require a separate incision, which may increase the morbidity such as saphenous vein and radial artery harvesting, and it is less time consuming [6]. Minimal morbidity in excising the gonadal vein can be anticipated due to the extensive cross-communication available. Absence of valves in the spermatic vein is another advantage [7].
The outcome of the vein grafts under high arterial pressure has always been a concern for vascular surgeons due to risk of graft aneurysm and rupture. Although very low risk has been reported for saphenous vein grafts, limited data exist for rupture risk of gonodal vein graft. Wall thickness of gonodal vein is better than brachial vein, which we may assume lower rupture rate considering brachiocephalic arteriovenous fistulas. The other concern is kinking of the graft, which is weaker than artery under pressure of the intraabdominal organs after closure of the abdomen. We believe this complication can be avoided by keeping the graft length short enough. We are planning to follow our patient with routine Doppler US control of graft monthly for the first year unless there is rapid dilatation of the diameter.
Conclusions
To our knowledge, gonodal vein interposition for hepatic artery reconstruction in living donor liver transplantation has not been previously reported. Since a size-matched artery graft is not always found during surgery, gonodal vein grafts can be used safely. In light of the urgency of this situation, we believe it can be a life-saving reconstruction.
Footnotes
Competing interests
The authors declare that they have no competing interests.
References:
- 1.Lee KW, Lee DS, Lee HH, et al. Interpostion vein graft in living donor liver transplantation. Transplant Proc. 2004;36:2261–62. doi: 10.1016/j.transproceed.2004.08.079. [DOI] [PubMed] [Google Scholar]
- 2.Ikegami T, Masuda Y, Ohno Y, et al. Arterial reconstruction in a case of subintimal dissection of celiac arterial tributaries in living donor liver transplantation: a case report. Transplant Proc. 2008;40:3794–96. doi: 10.1016/j.transproceed.2008.06.083. [DOI] [PubMed] [Google Scholar]
- 3.Margreiter C, Aigner F, Orozco H, et al. Hepatic artery reconstruction with inferior mesenteric vein graft in pediatric living donor liver transplantation. Pediatr Transplant. 2008;12:324–28. doi: 10.1111/j.1399-3046.2007.00868.x. [DOI] [PubMed] [Google Scholar]
- 4.Cherqui D, Riff Y, Rotman N, et al. The recipient splenic artery for arterialization in orthotopic liver transplantation. Am J Surg. 1994;167:327–30. doi: 10.1016/0002-9610(94)90210-0. [DOI] [PubMed] [Google Scholar]
- 5.Inomoto T, Nishizawa F, Terajima H, et al. The use of the recipient sigmoid artery for a revision of hepatic arterial reconstruction after thrombosis in living related liver transplantation. Transplantation. 1995;60:881–82. [PubMed] [Google Scholar]
- 6.Ohwada S, Ogawa T, Ohya T, et al. Gonadal vein graft for hepatic artery reconstruction. Hepatogastroenterology. 1999;46:1823–26. [PubMed] [Google Scholar]
- 7.Wishahi MM. Detailed anatomy of the internal spermatic vein and the ovarian vein. Human cadaver study and operative spermatic venography: clinical aspects. J Urol. 1991;145:780–84. doi: 10.1016/s0022-5347(17)38450-1. [DOI] [PubMed] [Google Scholar]


