Abstract
Watanabe et al. report that Nox4 NADPH oxidase catalytic moiety and the subunit p22phox mediate the increase in oxidative stress and human tubular epithelial cell injury induced by p-cresyl sulfate, a protein-bound uremic toxin. These findings could be instrumental for the design of novel therapeutic intervention utilizing small molecule inhibitors specifically targeting Nox oxidases to prevent or slow down the progression of chronic kidney disease and the associated disorders due to uremic toxicity.
Most patients with chronic kidney disease (CKD) experience a progressive loss of glomerular filtration that result in the reduction of the kidneys’ ability to remove uremic toxins from the blood stream, leading to their accumulation in the kidney and the body (1). As several of the uremic toxins are biochemically/biologically active compounds, their accumulation in the kidney will directly alter renal cell function, including tubulointerstitial cells, aggravating renal pathologies via enhancement of inflammatory or fibrotic processes (2). The classification of the uremic toxins is mainly based on the physico-chemical characteristics of the molecules that influence solute removal by dialysis or related strategies (1). Particular attention has been given to protein-bound uremic toxins and in particular to the prototypes compounds of this group, the phenols and indoles. Among the phenolic compounds, a growing interest was recently fostered for the biological activity of p-cresyl sulfate in CKD. It should be noted that while the original research on phenolic compounds has focused on the precursor of p-cresyl sulfate, p-cresol (4-Methylphenol), recent work using modern analytic methods indicated that p-cresol is present only at very low concentrations in patients with CKD or renal failure (1, 3). This seems to be due to the fact that most of the p-cresol generated as a product of phenylalanine or tyrosine metabolism by the intestinal anaerobic bacteria becomes conjugated to sulfate to form p-cresyl sulfate (1, 3). Recent studies reported that the accumulation of p-cresyl sulfate is associated with progression of CKD and that levels are correlated with patient mortality rate, suggesting that p-cresyl sulfate may be a reliable predictor for the prognosis of CKD (4). Unlike p-cresol, the biological activity of p-cresyl sulfate is not well understood. It is important to specifically investigate the effects of p-cresyl sulfate since it appears that p-cresol and p-csyl sulfate exhibit distinct, if not opposing, biological activities as a result of the conjugation (1, 3). Although investigation performed in rat cortex or cultured human proximal epithelial tubular epithelial cells indicated that p-cresyl sulfate is a substrate of organic anion transporters and can thereby accumulate in renal cells, the molecular mechanisms underlying p-cresyl sulfate-based toxicity are unclear.
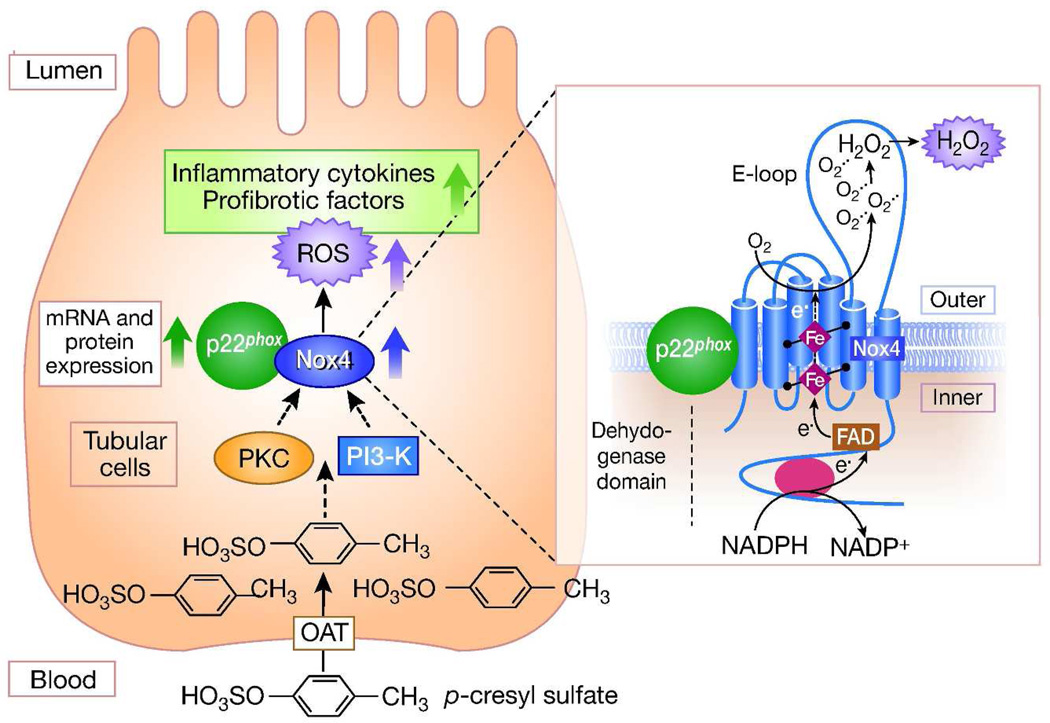
The work of Watanabe et al. (5) (this issue) sheds light on the molecular mechanisms that may mediate p-cresyl sulfate-induced human tubular epithelial cell injury. The authors identified reactive oxygen species (ROS) derived from a Nox4- and p22phox-based NADPH oxidase as mediators of human tubular cell damage and increased expression of inflammatory cytokines and profibrotic factors such as transforming growth factor-β. The study also shows that accumulation of p-cresyl sulfate contributes to renal tubular injury and extracellular matrix deposition in the 5/6 nephrectomized rat model of CKD associated with an increase in oxidative stress and Nox4 and p22phox expression (Figure 1).
Figure 1. Nox4- and p22phox-dependent signaling pathways implicated in tubular cell injury triggered by p-cresyl sulfate.
p-cresyl sulfate accumulates in human tubular cells and promotes Nox4-dependent ROS generation via upregulation of Nox4 and p22phox. PI3-K and PKC activation mediate the stimulatory effect of p-cresyl sulfate on NADPH oxidase. Nox4-derived ROS subsequently enhance expression of inflammatory cytokines and profibrotic factors resulting in cell injury. The right panel illustrates the topology of Nox4 and the enzymatic reaction catalyzed by the enzyme. PI3-K, phosphoinositide 3-kinase; PKC, protein kinase C; OAT, organic anion transporter.
Nox4 belongs to the Nox family of NADPH oxidases and is the most abundant Nox homolog in the renal system. Nox4 was cloned from the kidney, and is highly expressed in renal tubules, renal fibroblasts, glomerular mesangial cells, and podocytes (6). Nox4 is a 578-amino-acid protein that exhibits 39% identity to the phagocyte Nox2 (the founding member of the Nox family) with special conservation in the six membrane-spanning regions and binding sites for NADPH, flavin adenine dinucleotide (FAD), and heme, the electron transfer centers that are required to pass electrons from NADPH to oxygen to form superoxide and hydrogen peroxide (6, 7). Evidence to date suggests that Nox4 heterodimerization with p22phox enhances the enzyme activity and it does not require cytosolic subunits that are essential for other Nox homologues (6, 7). Moreover, it was shown that the Nox4 dehydrogenase domain exists in a conformation that allows the spontaneous transfer of electrons from NADPH to FAD, a property explaining the constitutive activity of the enzyme. Hence, Nox4 has been referred to as a “constitutively active” enzyme that is regulated primarily at the level of its expression in response to various stimuli (6, 7). As a corollary, the overall ROS output of Nox4 may be directly governed by its expression level. Interestingly, it seems that transcriptional regulation is important for the chronic control of Nox4 protein expression, whereas Nox4 is acutely regulated through translational mechanisms without change in its mRNA levels (6, 7). Indeed, it has been reported that Nox4 expression is upregulated by agonists implicated in renal diseases such as high glucose, transforming growth factor-β, angiotensin II, advanced glycation end products, advanced oxidation protein products, insulin or insulin-like growth factor (6, 7). Nox4 also differs from other Nox enzymes because the superoxide produced by Nox4 is rapidly converted to hydrogen peroxide, thereby rendering superoxide release from the enzyme practically undetectable (6, 7). Recent work showed that hydrogen peroxide formation occurs through Nox4 third extracytosolic loop (E-loop) that may obstruct superoxide release as well as provide a source for protons, thus permitting rapid dismutation of superoxide to generate hydrogen peroxide (6, 7). Importantly, both Nox4 and p22phox are required for the alteration of mesangial cell, tubular cell or renal interstitial fibroblast function in response to the factors promoting renal injury mentioned above (6). Noteworthy, among these agonists, advanced glycation end products, advanced oxidation protein products, homocysteine or structural variants of angiotensin II have been also identified as uremic toxins. A causative relationship between Nox4-derived ROS and renal injury, including fibrogenic responses, was demonstrated in vivo in a study that showed that treatment of type 1 diabetic rats with Nox4 antisense oligonucleotides reduced ROS production and prevented extracellular matrix accumulation in glomerular and tubular compartments of the kidney (6). Although Watanabe et al. (5) limited their study to tubular cells, the cell type that is most likely primarily exposed to uremic toxin accumulation, it would be interesting to explore the potential role of Nox4-derived ROS in the effects of p-cresyl sulfate on glomerular cells such as mesangial cells that when activated can cause aberrant extracellular matrix deposition and glomerulosclerosis.
The novel finding that Nox4 NADPH oxidase is required for the injurious effects of p-cresyl sulfate is of particular interest since the oxidase has emerged as a central regulator of fibrotic processes and cell injury in various organ systems. Nox4 seems to be implicated not only in the development of renal injury and fibrotic lesions in diabetes but also the fibrotic processes and cell damages taking place during cardiac, lung or liver pathologies (6, 8–10). Intensive research is currently conducted to develop small molecules inhibitors targeting Nox4 and test their bioefficacy. For instance, numerous preclinical studies performed with orally administrable small molecule Nox4 inhibitors from the Pyrazolo pyridines chemical series in experimental animal models demonstrated that Nox4 targeting effectively attenuates the pathological changes observed in renal complication of diabetes, liver fibrosis and idiopathic pulmonary fibrosis (8–10).
Since the data presented by Watanabe et al. (5) showing that Nox4 plays a central role in p-cresyl sulfate-induced tubular cell injury were primarily generated in cell culture-based systems, further in vivo studies in which Nox4 function is impaired (e.g. mice with genetic deletion of Nox4), are needed to definitively validate these results and the in vivo relevance of this pathway. Importantly, the eventuality that Nox4 is not the only Nox homologue accounting for the effects of p-cresyl sulfate in human kidney should not be excluded. This concern is justified in regards to recent observations showing that the homologue Nox5, which is not expressed in rodents, seems to be critical for redox-mediated damages in human renal cells, including tubular cells.
However, the observations in this manuscript support the rationale that Nox4 inhibition may have promise as a potential therapeutic intervention to prevent renal injury caused by uremic toxins. Given that other uremic toxins such as indoxyl sulfate, homocysteine, advanced glycation end products and advanced oxidation protein products have been documented to either promote oxidative stress or enhance Nox4-dependent ROS generation, it is tempting to speculate that treatment with Nox4 inhibitors could serve as a common therapy for uremic toxicity associated with CKD. Interestingly, NADPH oxidases of the Nox family were also implicated in the cardiovascular disorders (6, 7). It is therefore plausible that therapeutic potential of Nox inhibition may be extended to dialysis patients to protect them from vascular and endothelial dysfunction caused by accumulation of uremic toxins.
Footnotes
Disclosure
The author declared no competing interests.
References
- 1.Vanholder R, Van Laecke S, Glorieux G. What is new in uremic toxicity? Pediatr Nephrol. 2008;23:1211–1221. doi: 10.1007/s00467-008-0762-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Niwa T. Indoxyl sulfate is a nephro-vascular toxin. J Ren Nutr. 2010;20(Suppl):S2–S6. doi: 10.1053/j.jrn.2010.05.002. [DOI] [PubMed] [Google Scholar]
- 3.Vanholder R, Bammens B, de Loor H, Glorieux G, Meijers B, Schepers E, Massy Z, Evenepoel P. Warning: the unfortunate end of p-cresol as a uraemic toxin. Nephrol Dial Transplant. 2011;26:1464–1467. doi: 10.1093/ndt/gfr056. [DOI] [PubMed] [Google Scholar]
- 4.Liabeuf S, Barreto DV, Barreto FC, Meert N, Glorieux G, Schepers E, Temmar M, Choukroun G, Vanholder R, Massy ZA. European Uraemic Toxin Work Group (EUTox). Free p-cresylsulphate is a predictor of mortality in patients at different stages of chronic kidney disease. Nephrol Dial Transplant. 2010;25:1183–1191. doi: 10.1093/ndt/gfp592. [DOI] [PubMed] [Google Scholar]
- 5.Watanabe H, Miyamoto Y, Honda D, Tanaka H, Wu Q, Endo M, Noguchi T, Kadowaki D, Ishima Y, Kotani S, Nakajima M, Kataoka K, Kim-Mitsuyama S, Tanaka M, Fukagawa M, Otagiri M, Maruyama T. p-Cresyl sulfate causes renal tubular cell damage by inducing oxidative stress through the activation of NADPH oxidase. Kidney Int. 2012 doi: 10.1038/ki.2012.448. this issue. [DOI] [PubMed] [Google Scholar]
- 6.Barnes JL, Gorin Y. Myofibroblast differentiation during fibrosis: role of NAD(P)H oxidases. Kidney Int. 2011;79:944–956. doi: 10.1038/ki.2010.516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lassègue B, San Martín A, Griendling KK. Biochemistry, physiology, and pathophysiology of NADPH oxidases in the cardiovascular system. Circ Res. 2012;110:1364–1390. doi: 10.1161/CIRCRESAHA.111.243972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sedeek M, Gutsol A, Montezano AC, Burger D, Nguyen Dinh Cat A, Kennedy CR, Burns KD, Cooper ME, Jandeleit-Dahm K, Page P, Szyndralewiez C, Heitz F, Hebert RL, Touyz RM. Renoprotective effects of a novel Nox1/4 inhibitor in a mouse model of Type 2 diabetes. Clin Sci (Lond) 2013;124:191–202. doi: 10.1042/CS20120330. [DOI] [PubMed] [Google Scholar]
- 9.Jiang JX, Chen X, Serizawa N, Szyndralewiez C, Page P, Schröder K, Brandes RP, Devaraj S, Török NJ. Liver fibrosis and hepatocyte apoptosis are attenuated by GKT137831, a novel NOX4/NOX1 inhibitor in vivo. Free Radic Biol Med. 2012;53:289–296. doi: 10.1016/j.freeradbiomed.2012.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Laleu B, Gaggini F, Orchard M, Fioraso-Cartier L, Cagnon L, Houngninou-Molango S, Gradia A, Duboux G, Merlot C, Heitz F, Szyndralewiez C, Page P. First in class, potent, and orally bioavailable NADPH oxidase isoform 4 (Nox4) inhibitors for the treatment of idiopathic pulmonary fibrosis. J Med Chem. 2010;53:7715–7730. doi: 10.1021/jm100773e. [DOI] [PubMed] [Google Scholar]