Abstract
In India, care seeking for reproductive health among women is inadequate. This poses a unique challenge to researchers recruiting cohorts for studies in clinic-based settings. The purpose of this paper is to describe the recruitment process used in a prospective cohort study investigating the relationship between bacterial vaginosis and acquisition of HSV-2 among sexually active women in Mysore, India. Participants were initially recruited from an obstetrics/gynaecology outpatient clinic. Results were compared with a ‘community supported’ enrolment process, which included community preparation and reproductive health education followed by screening of potential participants. During November 2005, 1,054 women were screened in the clinic. Of the total screened, 246 (23%) were eligible and only 78 (7%) enrolled. Between December 2005 and April 2006, investigators adopted a community supported enrolment process. During that period, 1,077 potential participants were screened, 947 were eligible, and 918 (85%) enrolled. Fifty-six (72%) participants recruited from the clinic returned for their first follow-up visit, compared with 795 (97%) participants recruited using the community supported enrolment process. Since obstetrics/gynaecology departments in India are poor places to recruit non-pregnant women of reproductive age, a community supported process yields more eligible potential participants to screen, and results in significantly better study retention.
Keywords: India, recruitment, research, reproductive health, women
Background
General context
Effective participant recruitment is essential to conducting good clinical research. Many studies are underpowered because they fail to enrol an adequate number of subjects. Little research has been done to compare different recruitment models, especially in developing countries like India. Finding effective ways to enrol participants in the face of uneven access to healthcare and low utilization rates among certain groups, is an important concern for investigators conducting clinical research. During the last several decades, under-representation of women in clinical trials has been the subject of considerable research, political debate, and public scrutiny (Vannicelli and Nash 1984, Larson 1994, Institute of Medicine 1999, Vidaver et al. 2000). There is evidence that their exclusion has compromised both the quality of health information available to women and the healthcare provided to them (Public Health Reports 1985). Nowhere is this a greater problem than in developing countries like India, where women have historically been excluded from medical treatment because of lack of access to resources (Deogaonkar 2004), limited decision making power (National Family Health Survey 2000), restricted autonomy (Dyson and Moore 1983), and reduced freedom of movement (Mason 1997). Recruiting healthy non-pregnant women as research participants is always difficult. In India, the social context and gender traditions surrounding health-seeking activities present additional challenges. Developing effective methods to recruit and retain women in clinical studies is a critical first step to ensuring that women are adequately represented in study populations and benefit from the improved healthcare access clinical research can provide.
Materials and methods
The HSV-2 study
The HSV-2 study is being conducted in Mysore, India, among a cohort of 898 at-risk women, to investigate the relationship between bacterial vaginosis and seroconversion to herpes simplex virus 2 (HSV-2) infections. Recruitment of participants into the study occurred between November 2005 and April 2006. After being screened and recruited, women were interviewed and detailed physical exams were performed at baseline, 3 months, and 6 months.
To be included in the study, participants had to be between the ages of 15 and 30 years, sexually active (defined as having had vaginal intercourse at least once in the past 3 months prior to enrolment), willing to undergo a pelvic examination and blood draw, and willing to stay in the area for the next 6 months. Women who were pregnant or who had vaginal bleeding were excluded from the study. All participants recruited into the study received a 100 INR (2.27 USD) time and travel reimbursement for each completed visit to the study site.
Human subjects
The study was approved by the Committee for protection of Human subjects of the University of California, Berkeley, and Asha Kirana Hospital Institutional Review Board, in compliance with all Federal regulations governing the protection of human subjects. Data were collected from all eligible participants who gave written informed consent to participate in the study.
Clinic-based recruitment
Potential participants were recruited during the month of November 2005 from the Outpatient Clinic of the Obstetrics and Gynaecology (ObGyn) Department at CSI Holdsworth Memorial Hospital (HMH). HMH is a 330-bed tertiary care facility with 150 beds assigned for ObGyn services. The population accessing care is predominantly from the middle and lower socioeconomic strata in Mysore, and is almost equally divided between Hindus and Muslims living in this middle-sized Indian city (population 820,000). The outpatient clinic operates 4 days per week, with approximately 150 women attending each day.
Female recruiters from the HSV-2 study approached patients appearing to fit the eligibility criteria of the study (non-pregnant women between 15 and 30 years of age) in the waiting room of the ObGyn outpatient clinic. They introduced themselves and explained the general purpose of the study in Kannada or Urdu, the languages most often spoken among the population coming into the hospital. Women were given a multilingual flier outlining the study and were asked a series of questions to assess their eligibility. Eligible potential participants expressing interest were directed to the study office, where an interviewer explained the research study in greater detail, answered questions, and obtained informed consent. Participants were interviewed using a structured pre-tested questionnaire, underwent a pelvic exam, had vaginal fluid and blood collected for laboratory diagnosis of bacterial vaginosis (BV), trichomoniasis (TV), candida infection, gonorrhoea (GC), and HSV-2 infection, and were treated according to the CDC treatment guidelines. At the end of the visit, participants were asked to return for two follow-up sessions at 3-month intervals and were given a wall calendar marked with follow-up dates. Additional recruitment materials included full colour posters prominently displayed in the outpatient clinic and other public areas of the hospital, and a heavily illustrated brochure for participants with limited literacy.
Community supported recruitment process
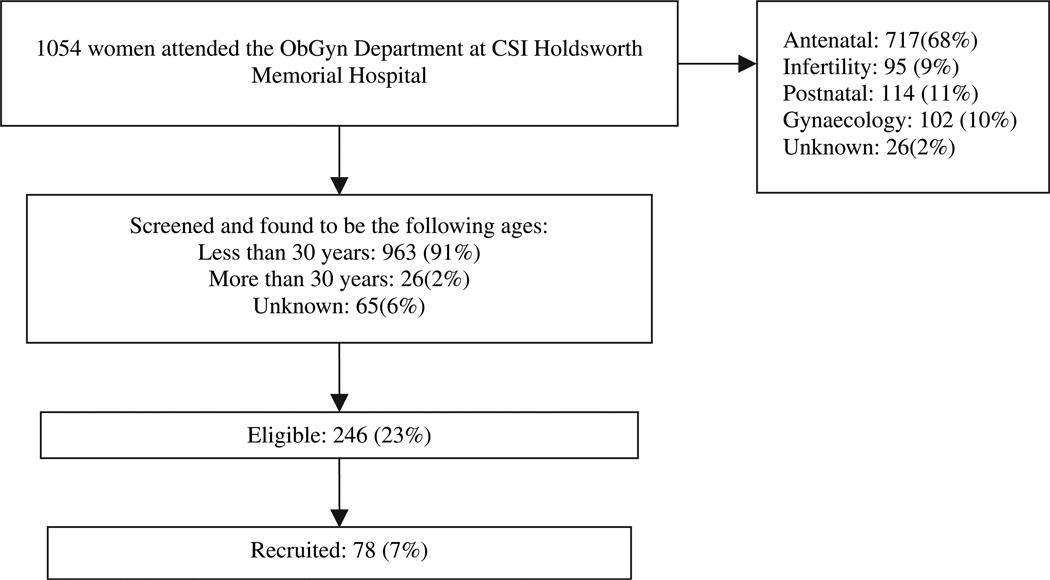
In response to slow study enrolment (see Figure 1), investigators adopted a new model for recruitment at the beginning of December 2005. Study staff met with three nongovernmental organizations (NGOs) involved in women’s health in the Mysore area. NGO staff suggested that recruiters utilize existing networks to reach women in the community, provide general reproductive health education to encourage health care seeking, and build relationships with local gatekeepers including public health nurses and Anganwadi workers, community-based employees working for the Government of India’s Integrated Child Development Services Programme (ICDS), to provide nutrition and medical support for low-income children.
Figure 1.
Reason for visits to ObGyn Department in month of November 2005 to CSI Holdsworth Hospital.
Investigators decided the main focus of recruiting efforts would be women’s microeconomic self-help groups (SHG). Within Mysore city limits there are more than 450 such groups engaged in a variety of small businesses including agriculture, incense rolling, crafts, and food preparation. With an average membership of 15 women in each group, they formed a potential pool of almost 7,000 prospective participants for study recruitment. Because SHG are loosely associated in large federations that meet monthly, study staff were able to make presentations to more than 400 leaders during the month of December.
In addition, investigators felt that the ICDS programme would provide a pool of young eligible women because the children served are below the age of 5 years, so most mothers would be younger than 30 years of age. Furthermore, Anganwadi workers are well respected in the community, so they could provide enhanced access to potential participants. Study staff met with more than 30 ICDS staff to explain the study.
Outreach programmes included a presentation by a study physician on general reproductive health. This was followed by a question and answer period that frequently covered a wide range of issues including menstruation and hygiene, sexually transmitted infections, fertility, and myths about childbearing and health. Recruiters gave a group presentation explaining the HSV-2 study, eligibility criteria, and information about how and where women could enrol. Women were encouraged to come to the hospital in groups, and transportation was provided if six or more women visited the study site together. In order to increase participation among SHG members, leaders were encouraged to accompany them to the study site, and they were offered a free examination as general patients if they did not qualify for inclusion in the study. Potential participants were screened and enrolled at HMH with the same protocol used in the clinic-based recruitment method.
Results
Clinic-based recruitment
During November 2005, 1,054 women were screened for the HSV-2 Study at the Outpatient Clinic in the ObGyn Department at CSI Holdsworth Memorial Hospital. Of these, 717 (68%) were pregnant, 95 (9%) were seeking treatment for infertility, 114 (11%) were attending for postnatal care, 102 (10%) had general gynaecological complaints, and 26 (2%) refused to give a reason for their visit. Of the total number screened, 246 (23%) were eligible and only 78 (7%) enrolled. Fifty-six (72%) of the participants that were recruited using this method returned for their first follow-up visit.
Community supported recruitment
From December to April 2006, recruiters from the HSV-2 Study conducted 74 health education programmes for SHG in 58 locations attended by more than 4,900 people, including SHG members, relatives, and residents from communities where outreach was conducted. During this time, 1,077 potential participants visited the study site in response to the ‘community supported’ enrolment process. Of these, 947 (88%) were eligible and 918 (85%) were enrolled in the study. Of the participants enrolled, 820 (76%) women completed all baseline procedures, including informed consent, interview, blood draw, pelvic exam, and specimen collection. Ninety-eight women did not complete all baseline procedures and were excluded from the cohort. A total of 795 (97%) participants recruited using this method returned for their first follow-up visit (see Table 1).
Table 1.
Description of the recruitment process for HSV-2 study.
| Clinic-based method | Community-supported method | Total study | |
|---|---|---|---|
| Screened | 1,054 | 1,077 | 2,131 |
| Eligible | 246 (23%) | 947 (87.9%) | 1,193 |
| Enrolled | 78 (7%) | 918 (85.2%) | 996 |
| Completed baseline visit | 78 (7%) | 820 (76.1%) | 898 |
| First follow-up visit | 56 (72%) | 795 (96.9%) | 851 |
Discussion
Enrolling women in clinical research studies is challenging even in the best of circumstances. In India, gender inequities and health seeking patterns make it even more difficult. This is particularly true of clinic and hospital-based research involving reproductive tract or sexually transmitted infections because women frequently avoid treatment for such conditions due to lack of knowledge (Prasad et al. 2005), shame and embarrassment (Bang and Bang 1998), and stigma and inhibitions regarding sexual and reproductive health (Sharma 2004). One study of health expenditures among young Indian women in Karnataka showed that the proportion of cases in which a practitioner was consulted was highest for problems involving pregnancy/family planning, while an appreciable proportion of genito-urinary problems were completely ignored (Bhatia and Cleland 2001). This is consistent with our experience in a mid-sized tertiary care hospital. Complicating the picture further, many of our youngest participants reported that they avoided ObGyn departments because they feared the stigma associated with infertility. Finding ways to overcome these challenges is crucial to successfully recruiting non-pregnant, reproductive age women into clinical studies.
While there are significant difficulties in enrolling women in clinic and hospital-based settings, the advantages are compelling. Protecting privacy and confidentiality is less challenging than in community venues. Obtaining appropriate examination and interviewing space is easier, and collection and transportation of laboratory specimens presents fewer difficulties. The community supported recruitment process offers enhanced access to eligible potential participants without sacrificing the advantages of clinic-based enrolment. Most importantly, protection of human subjects and higher clinical standards are preserved because potential participants are still screened, enrolled, and examined in a clinic setting.
Our experience suggests that in order to be successful, a community supported recruitment process must include strategies for accessing reproductive age women in settings where personal autonomy and mobility are restricted, must increase general reproductive health knowledge to encourage health seeking, and must address common obstacles to participation, such as limited access to transportation, competing demands on women’s time, and fear of intimidating health settings.
Accessing reproductive age women in India
In India, restricted autonomy and mobility present an important barrier to recruitment of women into research studies. In one study, as many as 75% of married women reported that they had to obtain their husband’s permission even to go out to the market or to visit friends or relatives (Chen 2001). In some communities, seclusion of women is still practiced and prohibitions against unaccompanied travel and contact with unrelated males strictly enforced (Bruce et al. 1995). In such an environment, it is not surprising that women’s health problems are under-researched, and much of the available information on reproductive morbidity comes from hospital and clinic-based studies (Prasad et al. 2005).
The development of the SHG movement in India offers researchers a promising new avenue for access to reproductive age women. In the last 15 years more than 450,000 women’s groups have been formed in India to facilitate savings and micro-credit activities. This represents a potential pool of almost seven million women countrywide (Seibel and Dave 2002). Our experience shows that leaders and members of women’s SHGs are not only willing to consider participating in programmes beyond the scope of microfinance, they have a strong interest in health-related initiatives of potential benefit to their members. During 4 months of outreach, the HSV-2 study staff made presentations to more than 340 SHGs in 58 locations, and eventually enrolled 820 eligible participants.
Increasing knowledge and health seeking among reproductive age women
With the exception of studies on contraception, little research has been done on reproductive health knowledge and attitudes among older women. Studies among adolescent females suggest that younger women (ages 15–19) generally have low levels of awareness and information about reproductive health, puberty, and sexual health (Nanda 2003). Our experience in conducting community trainings supports the view that, at least in the communities where we worked, women of all ages had limited access to information about reproductive health, and many expressed a strong desire to learn more. Presentations were generally attended by overflow crowds, sometimes as many as 150 women in a small community hall. Most came with specific questions about a wide range of issues, including menstruation, hygiene, vaginal discharge, infertility, contraception, and HIV. Not surprisingly, few had ever visited a hospital, and fewer yet had ever undergone a pelvic exam or been treated for a reproductive tract infection.
Our experience shows that once women were informed about the symptoms of reproductive tract infections, and the adverse sequelae associated with non-treatment, most expressed a willingness to seek care. Importantly, women were more likely to enrol in the study if trainings were conducted by a woman physician directly involved in participant care. In addition, the presence of community leaders at reproductive health trainings significantly enhanced recruitment efforts.
Overcoming obstacles that prevent women from participating in research
In India, obstacles to women’s participation in clinical research are numerous, and include fear of intimidating healthcare settings, concerns about being examined by male doctors or attendants, apprehensions about cost, limited time because of heavy childcare responsibilities, fear of domestic violence, and difficulties with transportation. In order to successfully recruit women into a study, researchers must be sensitive to these needs and address both real and perceived obstacles in outreach activities and in study procedures.
A large part of the focus of our outreach activities was addressing these issues. Study physicians and interviewers were an integral part of all training programmes. All staff were required to introduce themselves and explain that they would be at the study site when participants arrived. We found this was particularly important because many women were apprehensive about visiting large hospitals; the knowledge that there would be familiar faces allayed these fears. Being able to meet women physicians who would be conducting examinations was also essential because many of our participants and their families’ feared examination or molestation by male doctors.
Our recruiters also actively encouraged ‘group health seeking’ in our study. Members of the same SHG or residents of the same village would come as a group for their study visits. We found that women were empowered to access and seek health services in the company of their peers. Seeing that a friend had already undergone a particular procedure also reduced apprehension among women waiting for examinations. All study waiting rooms were designed to be child-friendly because many women did not have provisions for childcare. Toys were provided for a range of ages from infants to toddlers, and mats were spread on floors for sleeping children. Women often shared responsibility for watching children so participants were able to attend interviews and examinations without the added burden of childcare. Providing transportation for study participants was also important in several respects. First, the study benefited from being able to schedule staffing around group visits. Participant satisfaction was also enhanced, and this was reflected in high retention of participants in the study. Additionally, many women faced the possibility of domestic violence if they failed to return home by a certain time, so providing transportation also seemed to us to be a moral imperative.
Conclusion
In India, obstetrics/gynaecology departments are poor places to recruit non-pregnant reproductive age women for research studies. In this paper we have described two different methods used to recruit a cohort of young, sexually active, women to investigate the relationship of BV and incident HSV-2 infections. This was not a rigorous comparison of the two strategies but a description of our efforts to recruit women in a difficult developing world setting. Our experience suggests that a community-supported recruitment process may facilitate access to young women in the community, increase general knowledge and health seeking on reproductive health issues, and produced better overall study retention. More research is needed to confirm the benefits of using such a strategy to recruit women for reproductive health studies.
Acknowledgements
Dr Madhivanan is a fellow in the International AIDS Training and Research Program supported by the Fogarty International Center (1-D43-TW00003-16). For their generous assistance on this project, the authors would also like to thank the director of CSI Holdsworth Memorial Hospital, Dr. S.C. Karat, all the NGOs who assisted with outreach programmes, and women in the study for their participation. Special thanks to Anne Ericson, V.H.T. Swamy, B.S. Renuka, K.S. Gururaj, Muralidhar Singh for assisting on the project, and Dr. Srinivas Ghante and Dr. Parthasarathy of Asha Kirana Hospital, Jeanne Moncada of University of California, San Francisco, for providing technical support and helpful suggestions. I would also like to acknowledge the HSV-2 Study Team: Fazila Begum, Prabhavathi, Sathyanarayana, M.M. Shyla, and Rani, without whose hard work the study would not have been possible.
References
- Bang R, Bang A. A community study of gynecological disease in Indian villages: Some experiences and reflections. In: Moore K, editor. Learning About Sexuality: A Practical Beginning. New York: International Women’s Health Coalition and Population Council); 1998. [Google Scholar]
- Bhatia JC, Cleland J. Health-care Seeking and Expenditure by Young Indian Mothers in the Public and Private Sectors. Health Policy Planning. 2001;16:55–61. doi: 10.1093/heapol/16.1.55. [DOI] [PubMed] [Google Scholar]
- Bruce J, Lloyd CB, Leonard A, Engle PL, Duffy N. Families in Focus: New Perspectives on Mothers, Fathers, and Children. New York: Population Council; 1995. [Google Scholar]
- Chen M. A Matter of Survival: Women’s Right to Employment in India and Bangladesh. Oxford: Oxford University Press; 2001. [Google Scholar]
- Deogaonkar M. Socio-economic inequality and its effect on healthcare delivery in India. Electronic Journal of Sociology, ISSN,1198, 3655. 2004 http://www.sociology.org/content/vol8.1/deogaonkar.html.
- Dyson T, Moore M. On Kinship Structure, Female Autonomy, and Demographic Behaviour in India. Population & Development Review. 1983;9:35–60. [Google Scholar]
- Institute of Medicine. Ethical and Legal Issues of Including Women in Clinical Studies. Washington, DC: National Academy Press; 1999. [Google Scholar]
- Larson E. Exclusion of certain groups from clinical research. Image: The Journal of Nursing Scholarship. 1994;26:185–190. doi: 10.1111/j.1547-5069.1994.tb00311.x. [DOI] [PubMed] [Google Scholar]
- Mason KO. CICRED Seminar on Women and the Family. Paris: 1997. How family position influenced married women’s autonomy and power in five Asian countries. [Google Scholar]
- Nanda A. Addressing the reproductive health needs of adolescents in India: Directions for programmes. In: Puri C, editor. Towards Adulthood: Exploring the Sexual and Reproductive Health of Adolescents in South Asia. Geneva: World Health Organization; 2003. [Google Scholar]
- National Family Health Survey. National Family Health Survey (NFHS-2), 1998–99. Mumbai: International Institute for Population Sciences and ORC Macro; 2000. [Google Scholar]
- Prasad J, Abraham S, Kurz K, George V, Lalitha M, John R, et al. Reproductive Tract Infections among Young Married Women in Tamil Nadu, India. International Family Planning Perspectives. 2005;31:73–82. doi: 10.1363/3107305. [DOI] [PubMed] [Google Scholar]
- Public Health Reports. Women’s Health. Report of the Public Health Service Task Force on Women’s Health Issues. 1985;100:73–106. [PMC free article] [PubMed] [Google Scholar]
- Seibel HD, Dave HKR. Seminar on SHG-bank Linkage Programme. New Delhi: 2002. Commercial Aspects of Self-Help-Group Banking in India. [Google Scholar]
- Sharma A. Reproductive Morbidity and Health Seeking Behaviour of AdolescentWomen in Rural India. Population Association of America, 2004 Annual Meeting Program; Boston. 2004. [Google Scholar]
- Vannicelli M, Nash L. Effect of sex bias on women’s studies on alcoholism. Alcoholism. Clinical and Experimental Research. 1984;8:334–336. doi: 10.1111/j.1530-0277.1984.tb05523.x. [DOI] [PubMed] [Google Scholar]
- Vidaver RM, Lafleur B, Tong C, Bradshaw R, Marts SA. Women Subjects in NIH-funded Clinical Research Literature: Lack of Progress in both Representation and Analysis by Sex. Journal of Women’s Health and Gender-based Medicine. 2000;9:495–504. doi: 10.1089/15246090050073576. [DOI] [PubMed] [Google Scholar]