Patients with inflammatory bowel disease (IBD) complain of poor sleep [1,2], specifically of prolonged sleep latency, repeated awakenings, and poorer sleep quality than healthy controls, even in remission [1]. Possible contributors to this poor sleep include abdominal pain, diarrhea, bathroom trips, stress about future flare-ups, conditioned insomnia, altered immune function, and/or systemic inflammation [1,2]. Circadian disruption can also disturb sleep [3] and is linked to increased incidence of ulcers [4], colorectal cancer [5], and IBD [6]. We recently showed that chronic circadian disruption significantly exacerbates chemically induced colitis in mice, leading to greater weight loss, intestinal tissue injury, and colonic inflammation [7]. To date, circadian state has not been assessed in IBD patients. The gold standard measure of the circadian clock in humans is the melatonin rhythm [8]. This pilot study had two aims: (1) to determine if there was any circadian disruption in asymptomatic IBD patients (by examining the relationship between the timing of the melatonin rhythm and sleep) and (2) to determine if circulating melatonin levels were abnormally low, potentially contributing to the chronic inflammation and poor sleep in IBD. This is the first report of comprehensively measured melatonin rhythms in IBD patients.
Four patients (two males, 22–39 years), three with Crohn’s disease and one with ulcerative colitis (clinical and histologically proven) participated. All were symptom free for at least 1 month prior. Patients were of normal weight and were not taking melatonin supplements, sleep aids, or nonsteriodal anti-inflammatory drugs (prescribed medications listed in Figure 1). All patients were nonsmokers and passed a drug screen, except Patient 2 who quit smoking at enrollment (at his own volition) and tested positive for marijuana. All patients had not worked night shifts or crossed time zones in the previous month. The patients wore wrist monitors (Actiwatch-L, Phillips) and followed their habitual sleep schedules for 8–9 days at home before their dim light salivary endogenous melatonin profiles were assessed as per standard procedures [9]. The protocol was approved by the Rush University Medical Center Institutional Review Board and was in accordance with the Declaration of Helsinki.
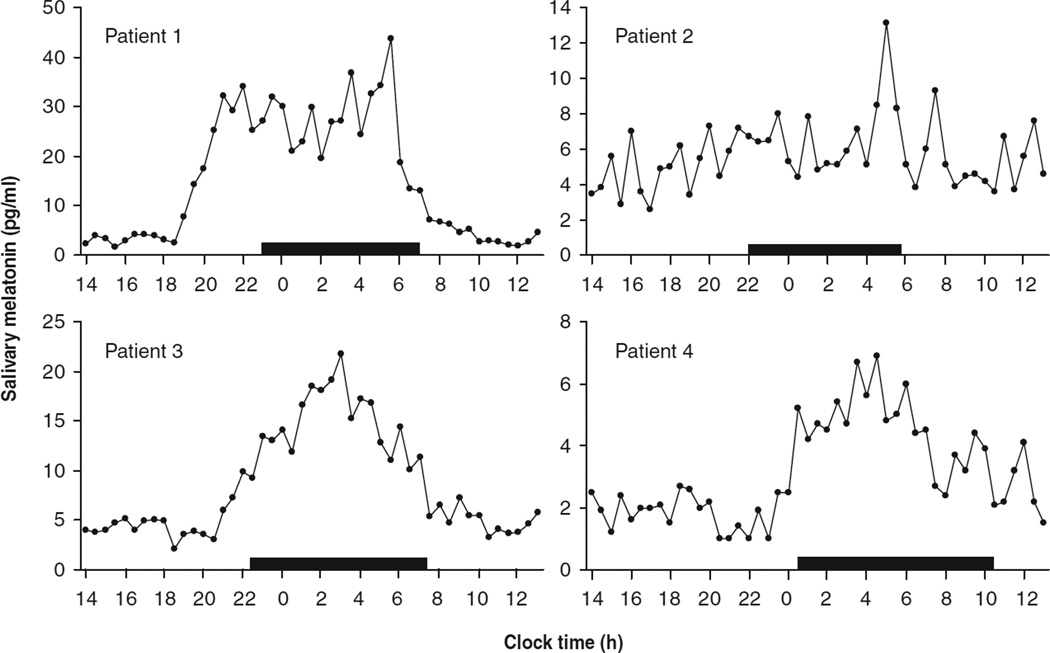
Figure 1.
Salivary melatonin profiles of four patients with asymptomatic inflammatory bowel disease. Each patient’s habitual sleep times are represented by a black rectangle. Patients stopped consuming alcohol and caffeine three days before the melatonin assessment. Patient 1 had ulcerative colitis and was taking buspirone and sulfasalazine. Patient 2 had Crohn’s disease and was taking mercaptopurine, mesalamine, and risedronate sodium. Patient 3 had Crohn’s disease and was taking mesalamine only. Patient 4 had Crohn’s disease and was taking azathioprine and omeprazole.
The wrist actigraphy data revealed that three patients had longer wake time after sleep onset than eight age and sex matched controls recruited online [10] (Table I). The patients’ sleep onset latency was significantly longer and sleep efficiency significantly lower than controls (Table I, both p < 0.05). These data are consistent with previous reports of poor sleep in patients with IBD.
Table I.
The sleep parameters of the four IBD patients and eight matched control subjects during 7 days of baseline sleep.
| Sleep onset | Wake time | Sleep onset latency (min) | Sleep efficiency | Wake after sleep onset (min) | Total sleep time (min) | |
|---|---|---|---|---|---|---|
| IBD1 | 23:38 | 7:12 | 34.9 | 74.1 | 78.6 | 375.4 |
| IBD2 | 22:46 | 5:20 | 38.2 | 77.5 | 37.4 | 356.1 |
| IBD3 | 22:40 | 7:09 | 15.2 | 73.9 | 106.3 | 403 |
| IBD4 | 00:35 | 10:22 | 5.4 | 86.6 | 68.4 | 518.1 |
| IBD mean | 23:25 | 7:30 | 23.4* | 78* | 72.7 | 413.2 |
| Control mean | 00:18 | 8:29 | 6.32 | 87 | 54.9 | 436.7 |
Abbreviation: IBD = inflammatory bowel disease.
p < 0.05, Mann-Whitney U test between patients and controls.
Three of the four patients had circadian rhythms in their melatonin secretion. The variability in the timing and amount of melatonin secreted was similar to a large sample of healthy controls [9]. The patients’ various medications did not abolish the melatonin rhythm in three patients. The lack of circadian rhythm in Patient 2’s melatonin secretion may have been due to his recent smoking and marijuana use. Nonetheless, the results indicate that the circadian rhythm in melatonin excretion can be abnormal in some patients with IBD and this should be studied in a larger cohort.
Acknowledgements
HJ Burgess was supported by NIH R01 HL083971. The study was supported in part by a generous special gift to the research program of the Division of Digestive Diseases and Nutrition by Mr. and Mrs. Larry and Barbara Field.
Footnotes
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- 1.Ranjbaran Z, Keefer L, Farhadi A, Stepanski E, Sedghi S, Keshavarzian A. Impact of sleep disturbances in inflammatory bowel disease. J Gastroenterol Hepatol. 2007;22:1748–1753. doi: 10.1111/j.1440-1746.2006.04820.x. [DOI] [PubMed] [Google Scholar]
- 2.Keefer L, Stepanski EJ, Ranjbaran Z, Benson LM, Keshavarzian A. An initial report of sleep disturbance in inactive inflammatory bowel disease. J Clin Sleep Med. 2006;2:409–416. [PubMed] [Google Scholar]
- 3.Reid KJ, Burgess HJ. Circadian rhythm sleep disorders. Prim Care. 2005;32:449–473. doi: 10.1016/j.pop.2005.02.002. [DOI] [PubMed] [Google Scholar]
- 4.Drake CL, Roehrs T, Richardson G, Walsh JK, Roth T. Shift work sleep disorder: prevalence and consequences beyond that of symptomatic day workers. Sleep. 2004;27:1453–1462. doi: 10.1093/sleep/27.8.1453. [DOI] [PubMed] [Google Scholar]
- 5.Schernhammer ES, Laden F, Speizer FE, Willett WC, Hunter DJ, Kawachi I, et al. Night-shift work and risk of colorectal cancer in the nurses’ health study. J Natl Cancer Inst. 2003;95:825–828. doi: 10.1093/jnci/95.11.825. [DOI] [PubMed] [Google Scholar]
- 6.Sonnenberg A. Occupational distribution of inflammatory bowel disease among german employees. Gut. 1990;31:1037–1040. doi: 10.1136/gut.31.9.1037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Preuss F, Tang Y, Laposky AD, Arble D, Keshavarzian A, Turek FW. Adverse effects of chronic circadian desynchronization in animals in a “challenging” environment. Am J Physiol. 2008;295:R2034–R2040. doi: 10.1152/ajpregu.00118.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lewy AJ, Cutler NL, Sack RL. The endogenous melatonin profile as a marker of circadian phase position. J Biol Rhythms. 1999;14:227–236. doi: 10.1177/074873099129000641. [DOI] [PubMed] [Google Scholar]
- 9.Burgess HJ, Fogg L. Individual differences in the amount and timing of salivary melatonin secretion. PLoS One. 2008;3:e3055. doi: 10.1371/journal.pone.0003055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Burgess HJ, Revell VL, Eastman CI. A three pulse phase response curve to three milligrams of melatonin in humans. J Physiol. 2008;586:639–647. doi: 10.1113/jphysiol.2007.143180. [DOI] [PMC free article] [PubMed] [Google Scholar]