Abstract
Purpose
The purpose of this study was to review the preliminary results of an original fusionless method of treatment for progressive scoliosis in young children.
Methods
This study retrospectively reviewed the clinical records and radiographs of 23 children with progressive scoliosis who failed to respond to conservative treatment and underwent fusionless surgery using a single solid growing rod construct. All of them were ambulatory and had a follow-up of minimum 2 years. Sixteen patients were treated by consecutive distraction of a single intramuscular rod, and seven patients with rodding and anterior apical convex fusion. The etiology of the scoliosis included 11 idiopathic, 6 syndromic, 4 congenital, and 2 neurofibromatosis. At initial surgery, the average age was 9.3 ± 2.8 years, with a mean Cobb angle of 68° ± 32°. Six patients underwent progressive scoliosis correction in a Stagnara cast prior to surgery, and one patient with an external halo-pelvic Ilizarov device.
Results
Fusionless single rodding allowed to maintain scoliosis correction in all patients. At an average of 3.5 ± 0.9 years after initial surgery, the 23 patients showed a correction of 57 % in the magnitude of the original curvature. Trunk height increase was documented in all patients and ranged from 1.5 to 11.9 cm. Rod failure was found in three patients and two patients had hardware infection. Only four cases of proximal junctional kyphosis were found at last follow-up.
Conclusions
Preliminary results from these series of patients show that the presented fusionless single growing rod technique allows to maintain correction of progressive early onset scoliosis while permitting spinal growth, with low complication rate. With this technique, lengthening procedures are used only once in every 10 months and patients are more comfortable as no brace is needed in most cases. This technique does not require any specific spine device. The procedure is simple and efficacious as long as some guidelines are respected.
Keywords: Early onset scoliosis, Growing rod, Fusionless surgery, Single submuscular rod, H3S2 construct
Introduction
Treatment of severe progressive scoliosis in skeletally immature patients is very challenging, whatever the etiology of the scoliosis. When bracing treatment is not possible or fails to prevent scoliosis progression, segmental spinal fusion has been the standard treatment [13, 31], but this type of procedure has been shown to be inappropriate for young children with considerable growth remaining [8, 11, 14, 20, 21, 33, 35]. Therefore, instrumentation without fusion has been proposed in those patients with immature spine in order to halt scoliosis progression and delay the definitive surgical procedure until spinal growth is sufficient [7, 25]. Nowadays, fusionless surgery is the most common method of management of immature children with progressive scoliosis who fail to respond to non-operative treatment [34]. Several techniques of rodding without fusion have been described (single growing rod, dual growing rods, hybrid growing rod with rib anchors proximally and spine anchors distally, Vertical Expandable Prosthetic Titanium Rib implant) [5, 36], but usually with a high complication rate [15]. Implant failure, infection, and unintended autofusion are the most common complications [4, 37] and are influenced by the number of lengthening procedures [2]. Most authors recommend concomitant brace treatment to decrease the risk of implant failure [3, 16, 23, 34]. Spine autofusion prevents from maintaining deformity correction and can lead to early surgery with unsatisfactory correction at the time of definitive fusion.
Excessive kyphosis has presented special challenges to fusionless techniques leading to failure of instrumentation and fixation either proximally or distally, especially, rib-to-rib constructs are known to be ineffective in controlling hyper-kyphosis [27, 30].
The current study describes the preliminary results of an original fusionless technique that allowed to obtain and maintain deformity correction while preserving spinal growth and lung development with a low complication rate in a series of 23 consecutive patients with progressive scoliosis. The purpose of this study was to assess the preliminary clinical and radiological results of this original technique and to compare these results with those from other techniques.
Materials and methods
From February 2005 to January 2010, 23 consecutive patients (15 girls, 8 boys) with progressive scoliosis underwent correction and fusionless curve fixation using a single solid growing rod construct. All the patients were followed up until January 2012. All the surgical procedures were performed by the senior author (L. M.). Scoliosis was diagnosed before 5 years of age in all patients. A conservative treatment was first applied in every patient. Mean age at the time of initial surgery was 9.3 ± 2.8 years (range 2–13 years). There were 11 patients with idiopathic scoliosis, 6 with different syndromes, 4 with congenital scoliosis, and 2 with neurofibromatosis.
Surgery was performed when documented progression of scoliosis occurred despite adequate bracing, or when scoliotic deformity was associated to a severe thoracic hypo-kyphosis. When main curve Cobb angle was superior to 50°, patients were prepared to surgery with a preoperative correction of their scoliosis. Anterior convex epiphysiodesis was performed at the same time when the Cobb angle after preparation was more than 70° in eight pre-adolescent patients, whose residual spinal growth would not have been sufficient to expect a satisfactory correction of the curve with a single growing rod. In young children before 8 years of age, only the single posterior growing rod procedure was performed, even when the spinal deformity was more than 100°. In these young patients, the preoperative correction of the scoliosis, the growing rod insertion and the consecutive lengthening procedures were able to allow a good correction of the scoliotic deformity without the need of additional anterior procedure.
After the original procedure, patients were seen every 6 months. Only three patients had to wear a brace postoperatively, one patient because of bone fragility and two other patients because of repetitive rod failures.
The following parameters were evaluated in every patient: patient age at initial surgery, type and magnitude of the scoliotic curve, spinal growth, preoperative treatment, date of every surgical procedure, complications, and correction of the scoliotic curve at every follow-up visit.
The mean follow-up period was 3.5 ± 0.9 years (range 2–5 years). If the curve had progressed, with a loss of correction of 10° or more, the rod was lengthened. The interval between two procedures was initially 7.5 months, but was then increased to 10 months.
Children were evaluated clinically and by radiographic review. Preoperative and postoperative radiological imaging included standing postero-anterior and lateral radiographs of the full spine. Angles were measured on these radiographs using the Cobb method [6]. The angles of main scoliotic curves, compensatory cranial and caudal curves, thoracic kyphosis, and lumbar lordosis were measured and recorded. Thoracic kyphosis was measured from T4 to T12. Lordosis was measured from L1 to L5. The trunk height was measured as the vertical distance between the superior endplate of T1 and the superior endplate of the sacrum. The growth of the instrumented spine was measured as the distance between the endplate of the upper instrumented vertebra and the endplate of the lower instrumented vertebra. The proximal junctional kyphosis was measured as the angle between the inferior endplate of the vertebra two levels caudal to the upper instrumented vertebra and the superior endplate of the vertebra two levels cephalad to the upper instrumented vertebra. This angle was considered as significant when measuring 10° greater than preoperative value [32]. The rod obliquity was measured as the angle between the long axis of the rod and the vertical line.
Measurements were performed on plain X-rays and digital X-rays, by two different observers (A. J. and M. M.).
Of the 23 patients, 14 had a single thoracic curve and 5 had a single thoracolumbar curve, 3 had a double major curve and 1 had a double thoracic curve. The average preoperative Cobb angle was 68° ± 32° (range 30°–142°).
There were 65 growing rod surgeries performed on 23 patients including 23 primary growing rod implantations, 8 implant exchanges, and 34 lengthenings.
Breath tests were performed in three patients who had respiratory failure. The evolution of the vital capacity was recorded in those three patients.
Preoperative treatment
Two patients whose scoliotic curve measured from 50° to 70°, were placed in a Cotrel permanent traction device for 3 days, prior to the surgical procedure. In six patients whose Cobb angle was more than 70°, scoliosis was progressively corrected with a Stagnara cast during 4 weeks. In one case, Stagnara cast was not possible because of ribs impingement on the iliac crests, and a halo-pelvic external device (Ilizarov type) was used for 5 weeks.
The purpose of this preoperative treatment was to obtain a progressive correction of the rigid scoliotic deformity in an awakened patient.
Surgical technique
All surgeries were performed on a Cotrel spine surgery table with traction. The traction was gradually applied both at the head and the lower limbs at an average force of 100 N (70–120 N). The purpose of this traction was to obtain a progressive and optimal correction of the scoliosis in patient under general anesthesia, so that the single rod could be inserted without any excessive constraints.
Intraoperative spinal cord monitoring was used for every patient.
The same construct was used on almost all patients. It was a unilateral construct that consisted in a 5.5 mm titanium rod, three hooks proximally and two pedicle monoaxial screws distally. At the proximal end of the planned construct, two supralaminar hooks and one pedicle hook formed a solid “claw”. This construct was called H3S2 (3 hooks, 2 screws).
The choice of the proximal and distal anchor sites was made on the initial standing PA and lateral full spine X-rays and full spine X-ray after preoperative scoliosis correction. The proximal and distal anchor sites were chosen so that the rod had a strictly vertical position, parallel to the coronal plumb line. In single curve scoliosis, the pedicle hook and the upper pedicle screw position usually corresponded to neutral vertebrae of the scoliotic curve. In most patients with thoracic curve, the two supralaminar hooks were placed at T2 and T3, and the pedicle hook at T4. In cases of scoliosis with two curves, the rod had to cross the midline at the transition zone between the two scoliotic curves, giving a “dollar shape” appearance to the spine-rod assembly. The CD Legacy device (Medtronic, Memphis, TN) was used on all patients.
Intraoperative radiographs were taken to confirm the levels. At the proximal and distal anchor sites, minimal unilateral extraperiosteal paraspinal muscle dissection was performed through two short posterior midline incisions. Two supralaminar hooks and one pedicle hook were placed proximally. Insertion of the supralaminar hooks was carefully performed without opening the spinal canal, with both hooks in close contact with the lamina. To respect the rod verticality, both monoaxial screws were inserted so that their heads were aligned along the vertical line. A single rod was then contoured to create thoracic kyphosis and lumbar lordosis. The length of the rod corresponded to the distance between the first thoracic vertebra and the most distal lumbar vertebra. The reserve for future rod lengthening was located distally in most cases. Care was taken to create enough kyphosis at the proximal part of the rod to decrease the mechanical strain on the proximal hooks and decrease the risk of junctional kyphosis. The lumbar lordosis was usually less important to avoid rod subcutaneous protrusion with forward bending. This rod was inserted throughout the paravertebral muscles from the distal to the proximal incision with the rod concavity facing backwards, and then positioned along the plane of the scoliotic curve. The rod was then engaged in the three proximal hooks and the two distal screws. A 90°-derotation maneuver was then applied to the rod so that the thoracic scoliotic curve was changed to thoracic kyphosis and the lumbar scoliotic curve to lumbar lordosis. When the rod was in the good position, the proximal screw was first locked. The pedicle hook was then locked while applying a careful distraction on this hook. The two supralaminar hooks were locked without any compression maneuver not to damage bone laminae and to allow future growth of those anchor laminae. Finally, the most distal pedicle screw was locked while applying distraction between the two screws in order to respect the future growth of both distal anchor vertebral bodies. No bone fusion was performed at both anchor sites.
Each patient was allowed to stand up the day after the surgical procedure without any brace treatment, except particular cases. No physiotherapy was needed except for patients with respiratory failure.
Lengthening procedures were performed when the loss of correction was more than 10°. At each lengthening, bipolar traction and intraoperative neuromonitoring were used. Intraoperative controlled traction allowed to obtain maximum curve correction and to avoid excessive stress on the hardware. Only small incision at the distal anchor site was needed.
The same distal incision was made. The head of the two screws were exposed through a transmuscular approach. The rod-holder was placed proximal to the first pedicle screw. The two screws were unlocked and distraction was applied between the rod-holder and the proximal screw so that 1–2 cm lengthening was performed. The proximal screw was then locked. The distal screw was locked while performing a careful distraction between the two screws for the same reasons than those discussed above.
Results
The average operating time for the rod insertion procedure was 67 ± 19 min (range 45–105 min).
One to five lengthening procedures were performed in each patient.
The average operating time for lengthening procedure was 26 ± 9 min (range 15–50 min).
At last follow-up, the mean age of the patients was 12 years 10 months (range 6 years 6 months–17 years).
Main scoliotic curve was corrected from 68° ± 32° (range 31°–142°) before surgery, to 33° (range 11°–71°) after surgery, and 29° (range 15°–63°) on the average at the last follow-up. This represents a 57 % improvement. The average improvement in Cobb angle after each rod-lengthening procedure was equal to the loss of correction due to the spine growth between two rod lengthenings, with an additional improvement of 2.9° (range −10°–18°).
For the sagittal plane evaluation, patients were categorized into three groups according to their initial thoracic kyphosis (Table 1):
Group 1, (10 patients): hypo-kyphotic patients with a thoracic kyphosis measuring from 0° to 24°. The thoracic kyphosis averaged 9.5° ± 6.2° (range 0°–20°) before surgery, and 23.8° ± 6.2° (range 16°–37°) at last follow-up, which means an average improvement of 151 %. Lumbar lordosis was 32.6° ± 8.9° (range 20°–48°) before surgery, 33.3° ± 12.2° (range 18°–55°) at last follow-up.
Group 2, (9 patients): patients with normal kyphosis ranging from 25° to 50°. The thoracic kyphosis averaged 28.4° ± 5.9° (range 27°–39°) before surgery, and 26.6° ± 12.5° (range 12°–44°) at last follow-up, which means an average improvement of 6 %. Lumbar lordosis was 34.9° ± 7.9° (range 30°–50°) before surgery, 26.8° ± 13.7° (range 20°–40°) at last follow-up.
Group 3, (4 patients): hyper-kyphotic patients with kyphosis measuring more than 50°. Thoracic kyphosis averaged 92.7° ± 15.2° (range 81°–115°) before surgery, and 55.2° ± 30.3° (range 34°–77°) at last follow-up, which means an average improvement of 40 %. Lumbar lordosis was 54.2° ± 9.9° (range 40°–60°) before surgery, 32.5° ± 8.8° (range 25°–38°) at last follow-up.
Table 1.
Sagittal plane correction
| Preop kyphosis (°) | Postop kyphosis (°) | Improvement (%) | Preop lordosis (°) | Postop lordosis (°) | Improvement (%) | |
|---|---|---|---|---|---|---|
| Group 1 | 9.5 | 23.8 | 151 | 32.6 | 33.3 | 2 |
| Group 2 | 28.4 | 26.6 | 6 | 34.9 | 26.8 | 23 |
| Group 3 | 92.7 | 55.2 | 40 | 54.2 | 34.5 | 36 |
Four patients showed a significant proximal junctional kyphosis at last follow-up.
After the original surgery, the trunk height increase averaged 3.8 cm (range 1.4–7.9 cm), which means a mean increase in T1–S1 length of 1.35 cm per year.
The spine growth of the instrumented region was 0.85 ± 0.8 cm per year (range 0.4–4.8 cm).
Initial vital capacity of the three patients with respiratory failure and severe deformity was 396 ml on average. At last follow-up it increased to 653 ml. Thus the average increase in vital capacity was 257 ml (range 110–280 ml), which means an improvement of 65 %.
No patient had complaint and no bone impingement was noticed at the distal end of the rod on the follow-up X-rays.
At the last follow-up 18 patients are still undergoing the rod-lengthening program. Two patients have undergone the definitive arthrodesis and three patients are at the end of the lengthening procedure. The mean age at the time of spine arthrodesis was 15 years 6 months (range 14 years 6 months–16 years 10 months). Mean Cobb angle was 55° (range 52°–58°) before arthrodesis and 24.5° (range 1°–48°) after surgery, which means a correction of 55 %.
Complications
At the last follow-up five (22 %) out of the 23 patients had at least one complication: one complication in three cases, and two or more complications in two cases. A total of 11 unplanned procedures were thus performed on these five patients. In one case, the rod was broken a day before a scheduled lengthening.
There was no neurological complication. One patient had a superficial infection and two patients had a deep posterior wound infection, which required wound debridement, and resolved successfully with antibiotics. Rod breakage occurred in three patients: one time in one patient, three times in another patient and four times in the third patient. The fracture site occurred at 27.7 ± 21 mm of the upper screw. The repeated rod fractures were observed in two patients whose growing rod was not perfectly vertical. In those two patients, the rod obliquity was 13° (range 11°–14.8°). In the other patients, the mean rod obliquity was 5.27° ± 4.7° (0°–13.8°).
No hook dislodgement was observed. A pedicle screw misplacement was observed in two patients, but did not necessitate an unplanned surgery. They were changed during a rod-lengthening procedure.
Only four patients had a significant proximal junctional kyphosis at last follow-up, without any hook dislodgement necessitating an unplanned surgery.
Discussion
Different growing rod techniques have been described in the literature to treat evolutive scoliosis in young children [1, 5, 9, 12, 15, 17, 19, 22–24, 26, 34]. Every described technique has the same goals: to correct and prevent the evolution of the main scoliotic curve and to prevent the development of secondary structural curves while allowing spinal and lung growth. Nevertheless no technique has shown a real superiority and complication rate remains high. This study reports the preliminary results of an original growing rod construct.
In the present study, spinal growth was documented in all patients but with a wide range, from 1.4 to 7.9 cm. We think that this may be explained by the different etiologies of scoliosis and the wide range of ages at initial surgery (from 2 to 13 years) in our series.
In Mineiro and Weinstein [23] study, apical rotation did not show any significant improvement in most patients. The same observation was made in our series, but no increase in the apical vertebral rotation was observed with the growth of the spine in the treated patients.
In our series, three patients had severe spine deformity associated with respiratory failure. At last follow-up, their vital capacity was improved. It has been demonstrated that our technique does not change the volume of the rib cage but improves its shape [28]. This might positively influence the pulmonary function, particularly in patients with respiratory failure. Improvements in spine sagittal morphology were also observed, with progressive correction of thoracic hypo-kyphosis and hyper-kyphosis.
Most authors do not propose preoperative correction of the scoliosis before inserting the growing rods [1, 5, 9, 12, 15, 17, 19, 22–24, 26, 34]. The correction of the scoliotic curve is then obtained progressively by lengthening the rod [23]. In our series, patients with severe or rigid scoliosis had preoperative reduction of their scoliosis, and intraoperative traction was applied in all patients, whatever the severity of the scoliotic curves. This reduction prior to the insertion of the growing rod, allowed to obtain maximum curve correction while avoiding excessive stress on the foundation sites of the rod. This may explain the absence of mechanical complications at the rod fixation points in our series. As reduction of the scoliosis was achieved before inserting the rod, rod lengthening was performed with the sole aim of allowing spine growth. Therefore, rod-lengthening procedures were less frequent in our series, every 10 months on average, compared to others [1].
Some authors recommend to perform limited fusion about the hooks and/or pedicle screws foundation [18, 24]. In our procedure, this end fusion was not performed. The proximal claw created by the hooks, and the two distal pedicle screws were strong enough to support mechanical stress induced by scoliosis correction and daily living.
Rod failure is one of the most common complications described in the literature after growing rod procedure despite full-time bracing [1, 23, 37]. In Mineiro study, of the 21 rods used, 9 (42 %) failed during treatment. With our procedure, only 3 rod failures were observed although most of the patients were not placed in a brace after the original procedure. This may be explained by the use of a solid titanium single rod and by the fact that the reserve for future lengthening is located distally. Most of the other constructs described in the literature use two rods connected by a side-to-side or end-to-end rod connector (rod–rod construct) [10]. This connector represents a weakness in the growing construct.
The good mechanical resistance of the H3S2 construct allowed to avoid external orthotic support in most patients. In Mineiro and Weinstein study [23], after surgery, all patients had to wear a thoracolumbar sacral orthosis for full-time external support until definitive spinal arthrodesis was performed. In our series, only 3 patients out of 23 had rod fractures, several times in 2 of them. These repetitive rod fractures occurred although both patients were wearing a brace. In those cases, the rod was not perfectly vertical and we had to change the distal anchor position to improve the rod verticality. Therefore we think that rod verticality is of paramount importance for the rod mechanical resistance.
With rod–rod constructs, each lengthening procedure necessitates a large surgical exposure at the level of the rod connector. These repeated procedures lead to the appearance of scars in the surrounding soft tissues and to increasing concave fibrosis, which can finally have a negative impact on the curve flexibility, leading to the “law of diminishing returns” described by Sankar et al. [29], and limiting the final curve correction. With our growing construct, there is no surgical exposure in the concavity of the curve and each lengthening procedure is performed through the same previous incision at the level of the distal pedicle screws.
Submuscular placement of the rod and the very low profile of the construct reduce wound and implant-prominence complications, and reduce the number of unplanned operations.
Implant complications have been recognized to be more frequent in hyper-kyphotic patients [27, 30]. In our series, four patients were hyper-kyphotic (thoracic kyphosis measuring from 81° to 115°). None had implant complication and all patients demonstrated progressive partial correction of their hyper-kyphosis with lengthening procedures (Figs. 1a–g, 2a–d).
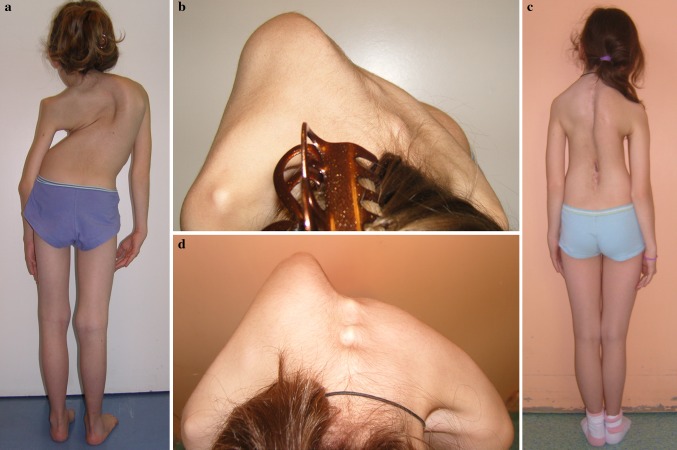
Fig. 1.
A 12-year-old girl with congenital thoracic scoliosis. Initial PA (a) and lateral (b) radiographs with hyperrotatory kyphosis. After Stagnara cast correction (c). Post anterior convex epiphysiodesis and rod insertion: PA (d), and lateral (e). After two rod lengthenings (1 proximal and 1 distal), 2 years later: PA (f) and lateral (g), with a good improvement of frontal and sagittal planes
Fig. 2.
Clinical pictures of the same patient and her thoracic gibbus, preoperatively (a, b), and 3 years postoperatively (c, d)
Furthermore, only four patients demonstrated a proximal junctional kyphosis, which may be explained by the strong proximal foundation site using two supralaminar hooks and one pedicle hook.
Another complication frequently described is spine autofusion because of the proximity of the growing rod [4]. The consequence is an increasing rigidity of the spine deformity, preventing further rod lengthening and obliging to perform spine arthrodesis in relatively young patients [36]. In our series no autofusion was observed at the spine, except in the three patients with dollar-shaped construct. In those patients, ossifications were observed at the crossing of the rod with the spine. Therefore, rod lengthenings could be performed until the skeletal maturity or complete correction of the curve (Figs. 3a–i, 4a–b).
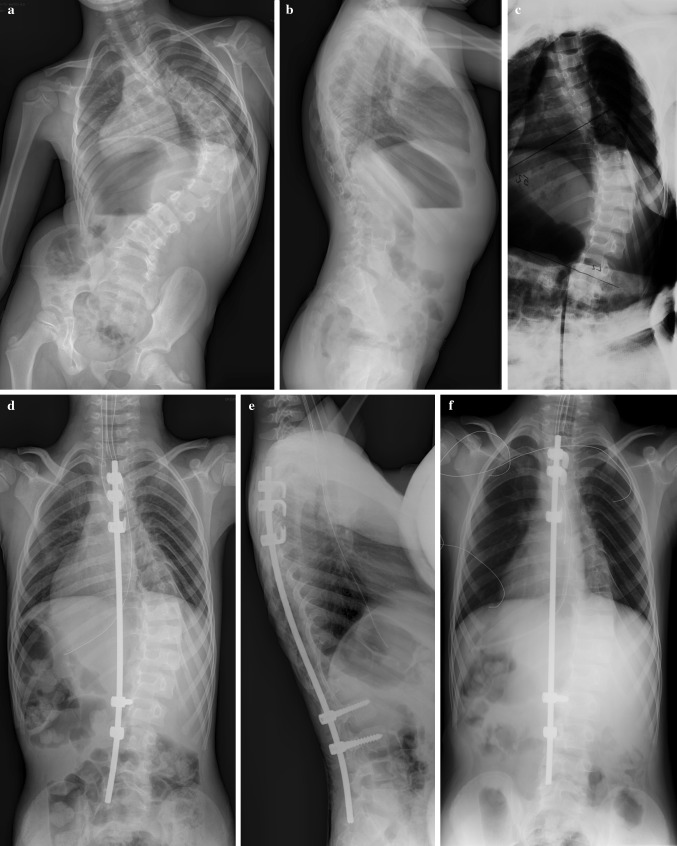
Fig. 3.
A 7-year-old boy with infantile idiopathic scoliosis. Initial PA (a) and lateral (b) radiographs. After Stagnara cast correction (c). Post initial surgery, PA (d) and lateral (e) X-rays; post first lengthening (f); post second lengthening (g); post third lengthening and broken rod replacement (3 years later): PA (h) and lateral (i). A good correction was obtained without any fibrosis or spontaneous fusion. It must be noted that the distal pedicle screw was badly inserted and was changed at the same time than the broken rod change (h)
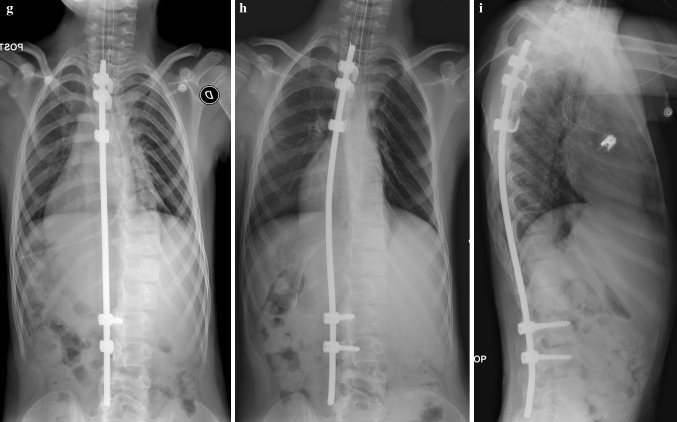
Fig. 4.

Clinical pictures of the same patient, preoperatively (a), and 2 years later (b) (first day after the second rod lengthening)
In our series, three patients (mean age 16 years 5 months) have reached the end of the lengthening procedure without fusion. In those patients, the mean Cobb angle at last follow-up was 22° (range 16°–28°). It was initially 74° (range 38°–92°), which means a correction of 70 %.
Conclusion
The described procedure was found to be safe and effective in maintaining scoliosis correction while allowing spinal growth along with a low rate of complications. The H3S2 construct does not need a long learning curve but requires the respect of certain important technical rules. It was found to have some advantages over the other growing rod techniques described in the literature: no brace treatment, less lengthening procedures, lower complication rate. Nevertheless these results have to be confirmed in a larger group of patients, with a longer follow-up.
Conflict of interest
None.
Contributor Information
Lotfi Miladi, Phone: +33-0171196282, FAX: +33-0144381522, Email: l.miladi@nck.aphp.fr.
Alexandre Journe, Email: alexandre.journe@wanadoo.fr.
Maryline Mousny, Email: Maryline.Mousny@uclouvain.be.
References
- 1.Akbarnia BA, Breakwell LM, et al. Dual growing rod technique followed for three to eleven years until final fusion: the effect of frequency of lengthening. Spine. 2008;33:984–990. doi: 10.1097/BRS.0b013e31816c8b4e. [DOI] [PubMed] [Google Scholar]
- 2.Bess S, Akbarnia BA, et al. Complications of growing-rod treatment for early-onset scoliosis. J Bone Jt Surg Am. 2010;92:2533–2543. doi: 10.2106/JBJS.I.01471. [DOI] [PubMed] [Google Scholar]
- 3.Blakemore LC, Scoles PV, et al. Submuscular Isola rods with or without limited apical fusion in the management of severe spinal deformities in young children: preliminary report. Spine. 2001;26:2044–2048. doi: 10.1097/00007632-200109150-00021. [DOI] [PubMed] [Google Scholar]
- 4.Cahill PJ, Marvil S, et al. Autofusion in the immature spine treated with growing rods. Spine. 2010;35:1199–1203. doi: 10.1097/BRS.0b013e3181e21b50. [DOI] [PubMed] [Google Scholar]
- 5.Campbell RM, Jr, Smith MD, et al. The effect of opening wedge thoracostomy on thoracic insufficiency syndrome associated with fused ribs and congenital scoliosis. J Bone Jt Surg Am. 2004;86:1659–1674. doi: 10.2106/00004623-200408000-00009. [DOI] [PubMed] [Google Scholar]
- 6.Cobb JR (1948) The American academy of orthopedic surgeons instructional course lectures, vol 5. Edwards, Ann Arbor, MI
- 7.Conner AN. Early onset scoliosis: a call for awareness. Br Med J (Clin Res Ed) 1984;289:962–963. doi: 10.1136/bmj.289.6450.962-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dubousset J, Herring J, Shufflebarger H. The crankshaft phenomenon. J Pediatr Orthop. 1989;9:541–550. doi: 10.1097/01241398-198909010-00008. [DOI] [PubMed] [Google Scholar]
- 9.Emans JB, Caubet JF, et al. The treatment of spine and chest wall deformities with fused ribs by expansion thoracostomy and insertion of vertical expandable prosthetic titanium rib: growth of thoracic spine and improvement of lung volumes. Spine. 2005;30:S58–S68. doi: 10.1097/01.brs.0000175194.31986.2f. [DOI] [PubMed] [Google Scholar]
- 10.Farooq N, Garrido E, et al. Minimizing complications with single submuscular growing rods. Spine. 2010;35:2252–2258. doi: 10.1097/BRS.0b013e3181ecf41a. [DOI] [PubMed] [Google Scholar]
- 11.Goldberg CJ, Moore DP et al (2002) Long-term results from in situ fusion for congenital vertebral deformity. Spine (Phila Pa 1976) 27:619–628 [DOI] [PubMed]
- 12.Harrington PR. Treatment of scoliosis: correction and internal fixation by spine instrumentation. J Bone Jt Surg Am. 1962;44:591–610. [PubMed] [Google Scholar]
- 13.Herring J, Wenger D. Segmental spinal instrumentation: a preliminary report of 40 consecutive cases. Spine. 1982;7:285–298. doi: 10.1097/00007632-198205000-00015. [DOI] [PubMed] [Google Scholar]
- 14.Karol LA, Johnston C, et al. Pulmonary function following early thoracic fusion in non-neuromuscular scoliosis. J Bone Jt Surg Am. 2008;90:1272–1281. doi: 10.2106/JBJS.G.00184. [DOI] [PubMed] [Google Scholar]
- 15.Klemme WR, Denis F, et al. Spinal instrumentation without fusion for progressive scoliosis in young children. J Pediatr Orthop. 1997;17:734–742. [PubMed] [Google Scholar]
- 16.Li Q, Zhang J, et al. Primary effect of dual growing rod technique for the treatment of severe scoliosis in young children. Chin Med J (Engl) 2010;123(2):151–155. [PubMed] [Google Scholar]
- 17.Luque E, Cardosa A. Segmental spinal instrumentation in growing children. Orthop Trans. 1977;1:37. [Google Scholar]
- 18.Marchetti PG, Faldini A. End fusions in the treatment of severe progressing or severe scoliosis in childhood or early adolescence. Presented to the Scoliosis Research Society, 1977. Orthop Trans. 1978;2:271–275. [Google Scholar]
- 19.Mardjetko SM, Hammerberg KW, et al. The Luque trolley revisited: review of nine cases requiring revision. Spine. 1992;17:582–589. doi: 10.1097/00007632-199205000-00018. [DOI] [PubMed] [Google Scholar]
- 20.Marks DS, Iqbal MJ, et al. Convex spinal epiphysiodesis in the management of progressive infantile idiopathic scoliosis. Spine. 1996;21:1884–1888. doi: 10.1097/00007632-199608150-00010. [DOI] [PubMed] [Google Scholar]
- 21.Marks DS, Sayampanathan S, et al. Long-term results of convex epiphysiodesis for congenital scoliosis. Eur Spine J. 1995;4:296–301. doi: 10.1007/BF00301039. [DOI] [PubMed] [Google Scholar]
- 22.McCarthy RE, Sucato D, et al. Shilla growing rods in a caprine animal model: a pilot study. Clin Orthop Relat Res. 2010;468:705–710. doi: 10.1007/s11999-009-1028-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mineiro J, Weinstein SL. Subcutaneous rodding for progressive spinal curvatures: early results. J Pediatr Orthop. 2002;22:290–295. [PubMed] [Google Scholar]
- 24.Moe J, Kharrat K, et al. Harrington instrumentation without fusion plus external orthotic support for the treatment of difficult problems in young children. Clin Orthop. 1984;185:35–45. [PubMed] [Google Scholar]
- 25.Patterson J, Webb J, Burwell The operative treatment of progressive early-onset scoliosis. Spine. 1990;15:809–815. [PubMed] [Google Scholar]
- 26.Pratt RK, Webb JK, et al. Luque trolley and convex epiphysiodesis in the management of infantile and juvenile idiopathic scoliosis. Spine. 1999;24:1538–1547. doi: 10.1097/00007632-199908010-00007. [DOI] [PubMed] [Google Scholar]
- 27.Reinker K, Simmons JW, et al. Can VEPTR control progression of early-onset kyphoscoliosis? A cohort study of VEPTR patients with severe kyphoscoliosis. Clin Orthop Relat Res. 2011;469:1342–1348. doi: 10.1007/s11999-010-1697-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sabourin M, Jolivet E, Miladi L, et al. Three-dimensional stereo radiographic modelling of rib cage before and after spinal growing rod procedures in early-onset scoliosis. Clin Biomech. 2010;25(4):284–291. doi: 10.1016/j.clinbiomech.2010.01.007. [DOI] [PubMed] [Google Scholar]
- 29.Sankar W, Skaggs DL, et al. Lengthening of dual growing rods and the law of diminishing returns. Spine. 2011;36:806–809. doi: 10.1097/BRS.0b013e318214d78f. [DOI] [PubMed] [Google Scholar]
- 30.Schroerlucke SR, Akbarnia BA et al (2011) How does thoracic kyphosis affect patient outcomes in growing rod surgery? Spine (Phila Pa 1976). doi:10.1097/BRS.0b013e318246d8a0 [DOI] [PubMed]
- 31.Shufflebarger H, Kahn A, et al. Segmental spinal instrumentation in idiopathic scoliosis: a retrospective analysis of 234 cases. Orthop Trans. 1985;9:124. [Google Scholar]
- 32.Skaggs D, Myung K, Lee C (2011) Proximal junctional kyphosis in distraction-based growing rods. In: Abstracts from the 5th international congress on early onset scoliosis and growing spine, November, Orlando FL, pp 18–19
- 33.Thompson AG, Marks DS, et al. Long-term results of combined anterior and posterior convex epiphysiodesis for congenital scoliosis due to hemivertebrae. Spine. 1995;20:1380–1385. [PubMed] [Google Scholar]
- 34.Thompson GH, Akbarnia BA, Campbell RM. Growing rod techniques in early onset scoliosis. J Pediatr Orthop. 2007;27:354–361. doi: 10.1097/BPO.0b013e3180333eea. [DOI] [PubMed] [Google Scholar]
- 35.Winter RB, Moe JH. The results of spinal arthrodesis for congenital spinal deformity in patients younger than five years old. J Bone Jt Surg Am. 1982;64:419–432. [PubMed] [Google Scholar]
- 36.Yang JS, McElroy MJ, et al. Growing rods for spinal deformity: characterizing consensus and variation in current use. J Pediatr Orthop. 2010;30:264–270. doi: 10.1097/BPO.0b013e3181d40f94. [DOI] [PubMed] [Google Scholar]
- 37.Yang JS, Sponseller PD, et al. Growing rod fractures: risk factors and opportunities for prevention. Spine. 2011;36(20):1639–1644. doi: 10.1097/BRS.0b013e31822a982f. [DOI] [PubMed] [Google Scholar]