Abstract
Osteotomies may be life saving procedures for patients with rigid severe spinal deformity. Several different types of osteotomies have been defined by several authors. To correct and provide a balanced spine with reasonable amount of correction is the ultimate goal in deformity correction by osteotomies. Selection of osteotomy is decided by careful preoperative assessment of the patient and deformity and the amount of correction needed to have a balanced spine. Patient’s general medical status and surgeon’s experience levels are the other factors for determining the ideal osteotomy type. There are different osteotomy options for correcting deformities, including the Smith-Petersen osteotomy (SPO), pedicle subtraction osteotomy (PSO), bone-disc-bone osteotomy (BDBO) and vertebral column resection (VCR) providing correction of the sagittal and multiplanar deformity. SPO refers to a posterior column osteotomy in which the posterior ligaments and facet joints are removed and a mobile anterior disc is required for correction. PSO is performed by removing the posterior elements and both pedicles, decancellating vertebral body, and closure of the osteotomy by hinging on the anterior cortex. BDBO is an osteotomy that aims to resect the disc with its adjacent endplate(s) in deformities with the disc space as the apex or center of rotational axis (CORA). VCR provides the greatest amount of correction among other osteotomy types with complete resection of one or more vertebral segments with posterior elements and entire vertebral body including adjacent discs. It is also important to understand sagittal imbalance and the surgeon must consider global spino-pelvic alignment for satisfactory long-term results. Vertebral osteotomies are technically challenging but effective procedures for the correction of severe adult deformity and should be performed by experienced surgeons to prevent catastrophic complications.
Keywords: Adult, Spine, Deformity, Osteotomy
Introduction
Adult spinal deformity is a complex and dynamic process that occurs in both the sagittal and coronal planes of the thoracolumbar spine. Adult scoliosis is defined as a spinal deformity in a skeletally mature patient with a Cobb angle of more than 10° in the coronal plane. The spinal deformities in adults differ from those in adolescents. As a general rule the adult curves tend to be more rigid, whereas adolescent curves are more flexible. In addition to cosmetic concerns, adult patients frequently present with pain and neurological symptoms, whereas, adolescents usually do not experience this degree of pain or neurological symptoms. Bone quality can be a major concern in the elderly population with deformity. The treatment of adult spinal deformity differs substantially from that of adolescent deformity. Surgery in adult deformities tends to be more complex procedures associated with higher rates of intra and perioperative complications. The goals of surgery in the adult are, to obtain a satisfactory balance in both sagittal and coronal planes, have a solid fusion with a balanced spine, relieve pain, and prevent further deformity. These can be achieved by anterior-only, anterior and posterior combined (circumferential) and posterior-only approaches. Surgeons should choose the most appropriate surgical approach and the type of corrective methods according to the type of deformity, curve magnitude, stiffness, bone density, operative goals, and surgeon’s experience and comfort level [1–7].
Osteotomies can be life saving procedures for rigid severe adult deformities which otherwise may not be treated by standard approaches. Development of vertebral osteotomies has certainly contributed significantly to the advancement of deformity surgery, allowing the surgeon to obtain more correction in rigid deformities with the use of pedicle screw fixation systems and intraoperative neuromonitoring.
Vertebral osteotomies are indicated when the deformity is too rigid to be corrected either with instrumentation alone or with the addition of posterior ligament and simple facet joint releases. Posterior-only approaches became very popular in recent years. Numerous studies supporting the safety and efficacy of a posterior-only approach for the treatment of all spinal deformities have been published. There are different osteotomy options for correcting deformities, including the Smith-Petersen osteotomy (SPO), pedicle subtraction osteotomy (PSO), bone-disc-bone osteotomy (BDBO) and vertebral column resection (VCR) providing correction of the sagittal and multiplanar deformity. Each osteotomy has a different potential in terms of the amount of correction obtained. Therefore, each osteotomy is indicated in a separate situation [2, 3, 5–7]. The purpose of this article is to introduce each osteotomy type and discuss their indications, prerequisites and complications.
General indications
Osteotomies are indicated for severe, rigid coronal and sagittal plane deformities. Other factors that need to be considered during the decision to perform an osteotomy are bone density, operative goals, and the surgeon’s experience and comfort level. Among these, the type of deformity is one of the most important factors in determining the method and amount of correction [3, 7].
It is important to understand the deformity when determining who is an appropriate candidate for a vertebral osteotomy. The type of deformity (scoliosis/kyphosis/lordosis) and any associated coronal/sagittal/combined spinal imbalance should be assessed for determining the type and extent of deformity. The type of deformity can be classified into one of the two categories: predominantly sagittal imbalance or multiplanar deformity with coronal and sagittal imbalance. Bridwell classified coronal plane deformity as flexible, partially flexible and rigid. Completely flexible deformity does not require any osteotomy, whereas rigid deformities definitely necessitate osteotomies [8].
Sagittal imbalance can be classified as type 1 (segmental) and type 2 (global). This type of classification is important to determine the type of osteotomy. Radiological sagittal balance is defined as C7 plumb line falling either through the sacrum or within 2 cm anterior to the sacrum. This assumes that the patient is standing in a natural position without knee flexion or hip hyperextension. In type 1 deformities, C7 plumb line is within 5 cm of the posterior superior corner of sacrum. In type 2 deformities, the regional hyperkyphosis is such that the patient cannot balance by hyperextending the mobile segments above or below the area of kyphosis. Type 1 deformities can be treated by SPO or sometimes by PSO while type 2 deformities usually require PSO or VCR. Sagittal imbalance may be coupled with coronal imbalance. There are two types of coronal imbalance. In the first type, the right shoulder is high and the right pelvis is low. In this circumstance, the coronal deformity can be corrected by simply shortening the right-hand side of the spine. In the second type, association of the shoulders to the pelvis is such that it cannot be corrected simply by shortening one side of the spine. In this circumstance (Type 2), a VCR is necessary. In the first type (Type 1), an asymmetric PSO will potentially achieve correction [8].
Recently, Lafage et al. [9] have reported the fundamental role of pelvis as the main regulator of a chain of correlation between spine and lower limbs. Therefore sagittal evaluation must include spino-pelvic parameters such as the sagittal vertical axis (SVA), the pelvic tilt (PT) and the relationship between pelvic incidence (PI) and lumbar lordosis (LL), expressed as PI–LL. Especially PT was shown to be of great importance because it represents a compensatory mechanism in the chain of correlation of sagittal alignment. These parameters have been shown to be highly correlated with pain and disability, and were used in order to set thresholds of correction during realignment procedures. Ideal sagittal alignment is described as SVA <50 mm, PT <25°, PI–LL = 10° [10]. Bernhard and Bridwell [11] found that a well-balanced spine, in general, has between 10º and 30º more lumbar lordosis than thoracic kyphosis. Ideal sagittal alignment parameters should be taken into account while selecting the osteotomy type for a particular patient.
Important points for deciding on the type and number of osteotomy are prediction of amount of correction needed to correct the deformity and determination of the size of wedge resection. This can be calculated and measured by templates or mathematical calculations. Ondra et al. [12] described a mathematical calculation using the tangent function to predict the necessary degree of correction and convert this result into intraoperative height measurements to obtain an ideal spinal reconstruction.
Preoperative evaluation
Appropriate preoperative clinical and radiographic evaluations are mandatory for best results. Flexibility of the spine should be assessed clinically and radiologically. Patients’ standing coronal and/or sagittal deformity may decrease in supine or prone position due to mobile segments. Standing long-cassette anteroposterior and lateral radiographs, supine bending, lateral fulcrum and lateral flexion and extension radiographs demonstrate the flexibility of the deformity. Traction radiography under general anaesthesia provides additional information about the flexibility.
Preoperative surgical planning is critically important since one surgery does not fit to all deformities. The surgeon must consider the global spinopelvic alignment in the surgical planning. Patient’s chief complaint, neurological status, medical comorbidities, and the predicted natural course of the deformity are other main factors for the preoperative plan. Careful consideration should be given to especially older patients due to the high incidence of pseudarthrosis and complications [3, 5, 7–9].
Osteotomies
Ponte osteotomy, Smith-Petersen osteotomy (SPO)
The first description of an SPO was in 1945 by Smith-Petersen [13] as a one- or two-level osteotomy for ankylosing spondylitis. Subsequently, multilevel SPO was advocated by many authors for kyphosis correction due to ankylosing spondylitis as well as other pathologies. Ponte [14] described Ponte procedure as, which included multiple chevron osteotomies with spinal instrumentation in Scheuermann’s kyphosis.
Smith-Petersen osteotomy refers to a posterior column osteotomy in which the posterior ligaments and facet joints are removed and a mobile anterior disc is required for correction. The surgical technique involves removal of the all posterior ligaments (supraspinous, intraspinous, and ligamentum flavum) and facets to produce a posterior release, thereby aiding in coronal correction and sagittal plane realignment (Fig. 1). Compression of the osteotomy sites provides correction of kyphosis. Additionally, compression leads to narrowing of the neural foramina, which necessitates a preceding wide facetectomy to prevent nerve root impingement [7]. In SPOs, trajectory of osteotomy and closure of osteotomy site can be done asymmetrically to correct coronal imbalance as well as sagittal imbalance (Fig. 2).
Fig. 1.
Smith-Petersen osteotomy (SPO). Left figure demonstrates resection of ligaments and facet joints and right figure demonstrates the closed osteotomy site
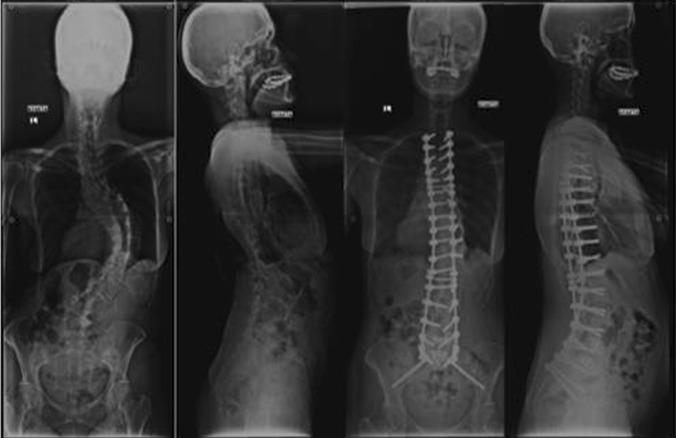
Fig. 2.
Illustrative case for SPO. 58-year-old female patient with adult scoliosis deformity. Correction in sagittal and coronal planes was achieved with multi-level asymmetrical SPOs
Type 1 sagittal plane deformity such as a long, rounded, smooth kyphosis in Scheuermann’s kyphosis, either a primary case or with a previous fusion and malunion, often is an ideal candidate for multiple SPOs. SPO along the apex of a rigid coronal curve helps to enhance curve flexibility and correction. SPO should be considered for patients with C7 plumbline that is in the range of 6–8 cm positive [8]. Amount of correction provided by SPO is in the range of 9.3–10.7° per level. One degree of correction is achieved per millimeter of bone resected (1°/mm bone). In most cases, if a moderate correction is achieved at each level and the posterior column is closed bone-on-bone centrally and laterally, the SPO is likely to heal and anterior grafting and reconstruction are not needed [7–9, 15]. In some cases, if substantial correction is achieved with an SPO opening anterior disc level extensively (greater than 10 mm in height), it may be necessary to graft the disc space anteriorly [8].
Smith-Petersen osteotomy is technically easier and safer than other osteotomies. Compared with other osteotomies, SPO offers a reduction in operative time, blood loss and risk of neurological complications. SPO provides less sagittal plane corrections and may create coronal decompensation, which seems to be the major disadvantage of the technique. Cho et al. [15] compared three levels of SPO with single level pedicle substraction osteotomy (PSO) in a series of 71 patients, and found that single level PSO caused nearly twice as much bleeding than three levels of SPO. In the same study, there was no difference between osteotomy types in terms of fusion rates and ODI. The mean correction of kyphotic angle was 10.7° per level. The authors concluded that PSO created greater sagittal imbalance correction and reduced the risk of coronal decompensation when compared to SPO. SPO on the other hand had a greater tendency towards coronal decompensation than PSO. A trapezoidal wedge type resection or performing SPO’s at neutral and stable vertebral segments have been suggested by the authors to prevent decompensation [15].
Pedicle subtraction osteotomy
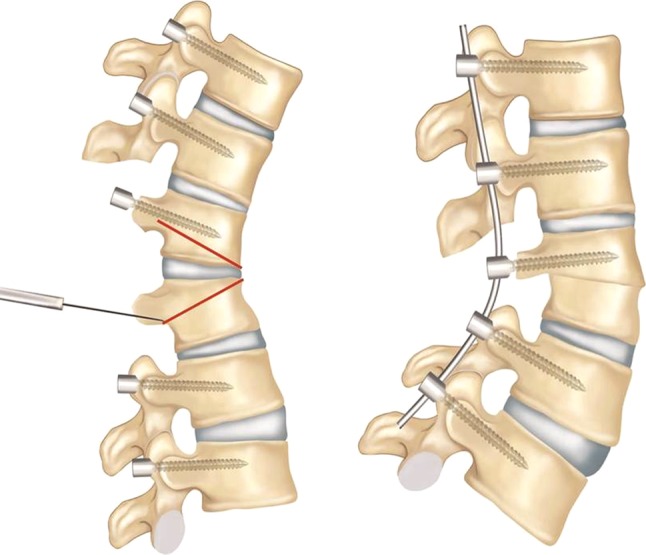
A pedicle subtraction osteotomy (PSO) is a transpedicular V shaped wedge osteotomy, which was first described by Thomasen [16] in 1985. In the same year, Heining et al. [17] described an eggshell osteotomy as a variant of the PSO, which was also a transpedicular decancellation closed wedge osteotomy. PSO is performed by removing the posterior elements and both pedicles, decancellating vertebral body, and closure of the osteotomy by hinging on the anterior cortex (Fig. 2). PSO has the advantage of obtaining correction through all three columns, thereby maximizing the healing potential while avoiding stretch on the major vessels and viscera anterior to the spine [18]. While the posterior and middle columns shorten, this osteotomy does not lengthen the anterior column, does not create an anterior bone defect, and provides a more stable correction. If performed in an asymmetric fashion, the osteotomy can provide significant coronal correction as well (Fig. 3). PSO can be performed for thoracic deformities as well as thoracolumbar and lumbar deformities. When it is performed in the thoracic spine, it is important not to retract the thecal sac. An average of 30° to 40° correction can be achieved with one level PSO [7, 8, 15, 18].
Fig. 3.
Pedicle subtraction osteotomy (PSO). Left figure demonstrates the osteotomy site and right figure demonstrates the correction after the closure of the osteotomy site
The ideal candidates for PSO are type 2 sagittal deformity patients with a substantial sagittal imbalance more than 12 cm (SVA > 12 cm), sharp, angular kyphosis, and those patients who have circumferential fusion along multiple segments, which would preclude performing SPOs. It is feasible to perform a PSO through areas of rotation and prior laminectomy, but this may increase the complication rate and make the procedure more technically demanding. If the patient has a type 1 coronal and type 2 sagittal imbalance, PSO can be performed asymmetrically with a more aggressive resection on one side, which categorizes the osteotomy between a standard PSO and a VCR [8].
In the surgical technique, after pedicle screw fixation, a wide laminectomy is performed for upper and lower level of the planned osteotomy site. Upper and lower exiting nerve roots are identified bilaterally and protected during the procedure. Osteotomy is carried out through the pedicles until reaching the anterior vertebral body. The anterior cortex of the body should be preserved to act as a hinge and avoid translation during closure of the osteotomy site. Osteotomy line should be horizontal to the sacrum to avoid any translation. Then the posterior cortex of the vertebral body is pushed down towards the vertebral body cavity with reverse curettes or osteotomes. Placing the temporary rod on the contralateral side while working on one side will avoid any translocation during osteotomy. Then the osteotomy site is closed over the rods while the hips and knees are hyperextended to facilitate closure of the osteotomy. Additional compression will help bone-to-bone closure of the osteotomy site. After closing the osteotomy site, any dural buckling or nerve impingement should be controlled to avoid neurological injury.
Although PSO is technically challenging and known to be more prone to complications, it provides satisfactory clinical and radiologic outcomes in long-term follow-up. Kim et al. [18] reported their results in a series of 35 PSOs with 5 to 8 years follow-up; they observed no significant regional radiological changes between the postoperative second year and final follow-up. Pseudoarthrosis (9 at thoracolumbar and 1 at lumbosacral junction) was identified in 10 (29 %) cases, five of which occured within 2 years and others between 2 and 4 years postoperatively. Patient satisfaction (87 %) and function (69 %) were high after more than 5 years of follow-up. SRS outcome scores were better for the patients with SVA <8 cm at final follow-up.
Cho et al. [15] compared one level of PSO with three levels of SPOs in their study and reported average total correction as 31.7° for PSO in a group of 41 patients with fixed sagittal imbalance. Improvement in the sagittal imbalance (11.2 ± 7.2) and correction of the coronal plane (0.48 ± 1.4 cm) were higher when compared to three levels of SPO group. Blood loss was significantly higher in PSO group. There was no statistical difference between one level PSO and three levels of SPO groups with respect to operating times [15].
Regarding neurological complications, Buchowski et al. [19] showed an intraoperative or post-operative neurological deficit rate of 11.1 % (12 of 108 patients), but only 2.8 % of deficits were permanent over a 10-year period. Deficits were always unilateral and never proximal to osteotomy, often did not correspond to the level of osteotomy, and were not detected by neuromonitoring. Although it was unclear what mechanism was responsible for the development of neurologic deficits, a combination of subluxation, residual dorsal impingement, and dural buckling were considered to be the main causes. In order to decrease the risk of neurological deficits, the authors recommended central canal enlargement, careful osteotomy closure to prevent or limit subluxation across the osteotomy site, performing a wake-up test after osteotomy and examining all motor functions following surgery. Incidence of neurological injury in the series of Yang et al. [20] and Ahn et al. [21] was 3.6 and 12 %, respectively.
In order to avoid pseudarthrosis in a primary case where a PSO is performed, interbody arthrodesis above and below the osteotomy can be carried out. Interbody fusion can be done as either a TLIF or an ALIF procedure (Fig. 4).
Fig. 4.
Illustrative case for PSO. 19-year-old male patient with kyphoscoliosis deformity. PSO was performed at T12 level. Adjacent level interbody fusions were performed via anterior thoracolumbar approach as a second stage
Bone-disc-bone osteotomy
Bone-disc-bone osteotomy (BDBO) is an osteotomy that aims to resect the disc with its adjacent endplate(s). It has three different types each providing different amounts of correction rates ranging from 35° to 60° (Figs. 5, 6, 7). The main indications are deformities with the disc space as the apex or center of rotational axis (CORA) and severe sagittal plane deformities that necessitate correction rates exceeding what a simple PSO can provide.
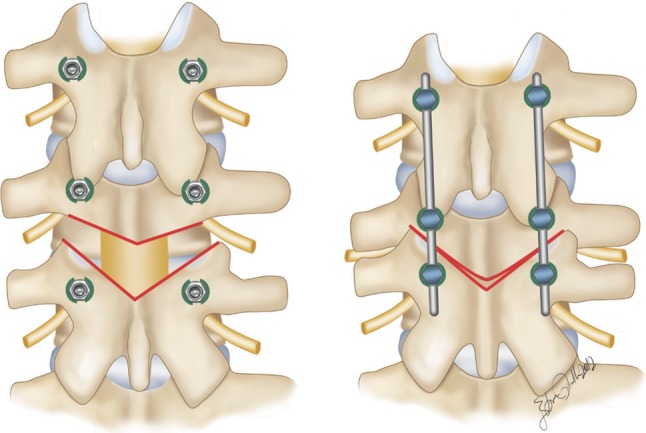
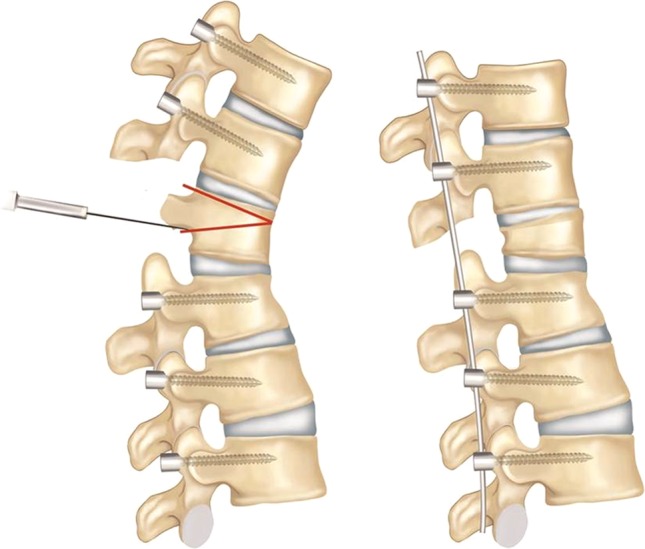
Fig. 5.
Type 1 bone-disc-bone osteotomy (BDBO). Left figure demonstrates the osteotomy sites and right figure demonstrates the correction after the closure of the osteotomy site
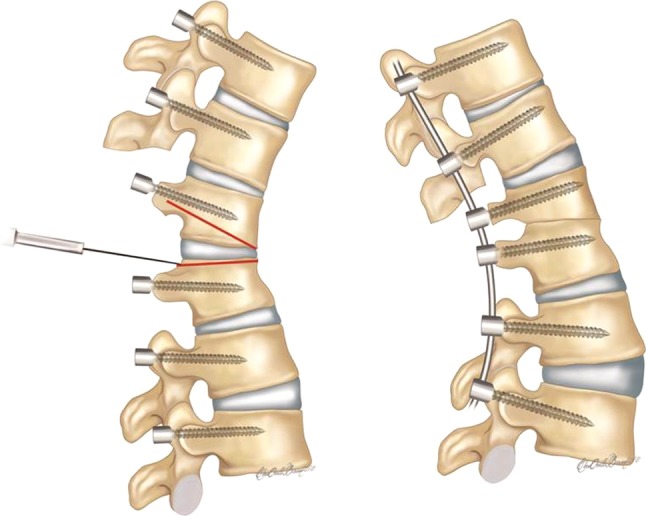
Fig. 6.
Type 2 BDBO. Left figure demonstrates the osteotomy sites and right figure demonstrates the correction after the closure of the osteotomy site
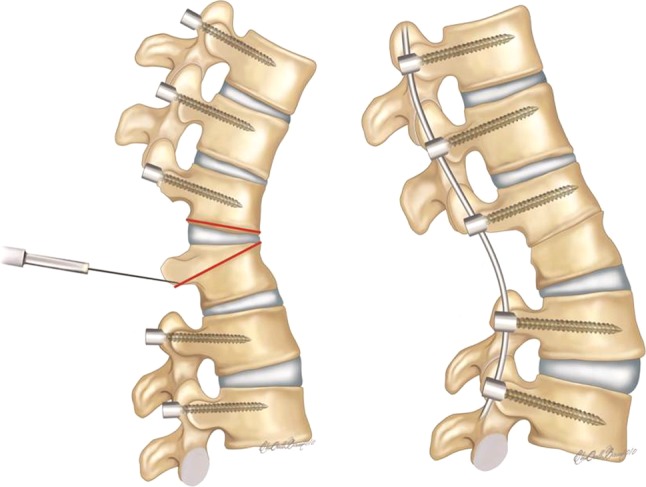
Fig. 7.
Type 3 BDBO. Left figure demonstrates the osteotomy sites and right figure demonstrates the correction after the closure of the osteotomy site
In the surgical technique; pedicle screws are placed at least two levels below and three levels above the planned osteotomy level, followed by wide laminectomies for the vertebrae above and below the disc space planned to be resected. Then, a wedge osteotomy including the disc-endplate(s) with or without the pedicle(s) is performed and the wedge including the disc is removed (Figs. 5, 6, 7). A titanium mesh cage can be placed anteriorly if lengthening of the anterior column is desired. Finally, the osteotomy site is closed bone-to-bone. Bone-to-bone closure of the osteotomy site decreases the risk of pseudoarthrosis. The advantages compared to PSO include correction of the deformity at its apex (CORA), higher correction rates, potential decrease in pseudoarthrosis rate due to disc removal, and better stability in type 1 osteotomies since there are four pedicle screws close to the osteotomy site (Fig. 5). The major advantage compared to PVCR is its applicability at the lumbar spine without sacrificing the nerve roots while providing correction rates closer to PVCR.
In a series of 12 patients with kyphosis and kyphoscoliosis deformity, Ozturk et al. reported an average 38° of correction in sagittal plane without any neurological injury or pseudoarthrosis during a 2-year follow-up after BDBO. Domanic et al. [22] have reported an average of 49° correction with type 3 BDBO in a group of patients who had severe rigid kyphotic deformities. The authors stated that although BDBO was technically difficult and required experience, it could be an alternative to PVCR in patients with thoracolumbar and lumbar severe and rigid deformities, particularly when the apex of deformity is a disc level (Fig. 8).
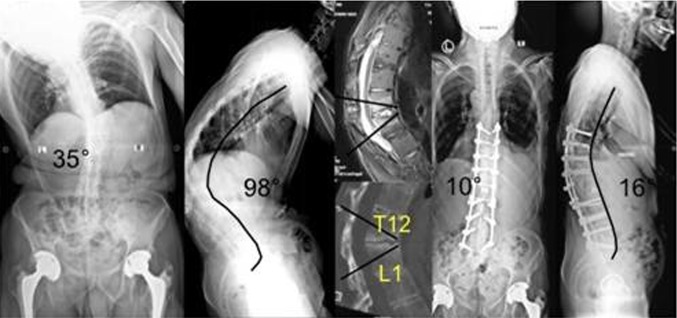
Fig. 8.
Illustrative case for BDBO. 41-year-old male patient with ankylosing spondylitis. CORA of the deformity was T12-L1 disc level. Deformity was corrected via posterior-only approach with BDBO
Vertebral column resection
Among various osteotomy options, vertebral column resection (VCR) provides the greatest amount of correction. VCR is indicated for rigid multiplanar deformities, sharp angulated deformities, hemivertebra resections, resectable spinal tumours, posttraumatic deformities, and spondyloptosis. It is a challenging procedure reserved for severe deformities of the spine with very limited or no flexibility. The VCR technique involves complete resection of one or more vertebral segments with posterior elements and entire vertebral body including adjacent discs (Fig. 9). It can be performed using either combined anterior and posterior approaches or a posterior-only approach [2, 3, 5, 7, 23, 24]. VCR was first described in 1922 by MacLennan [25] as a combined anterior and posterior procedure. Posterior vertebral column resection (PVCR) has first been introduced by Suk et al. [26] and has been popularized by Lenke [27] for severe deformities of the spinal column. It enables translational and rotational correction of the spinal column and provides a controlled manipulation of both the anterior and posterior columns simultaneously through a single approach. PVCR is a technically demanding procedure with a high potential neurological complication rate. However, it is a safe and effective procedure when performed properly by an experienced deformity surgeon under neurological monitoring.
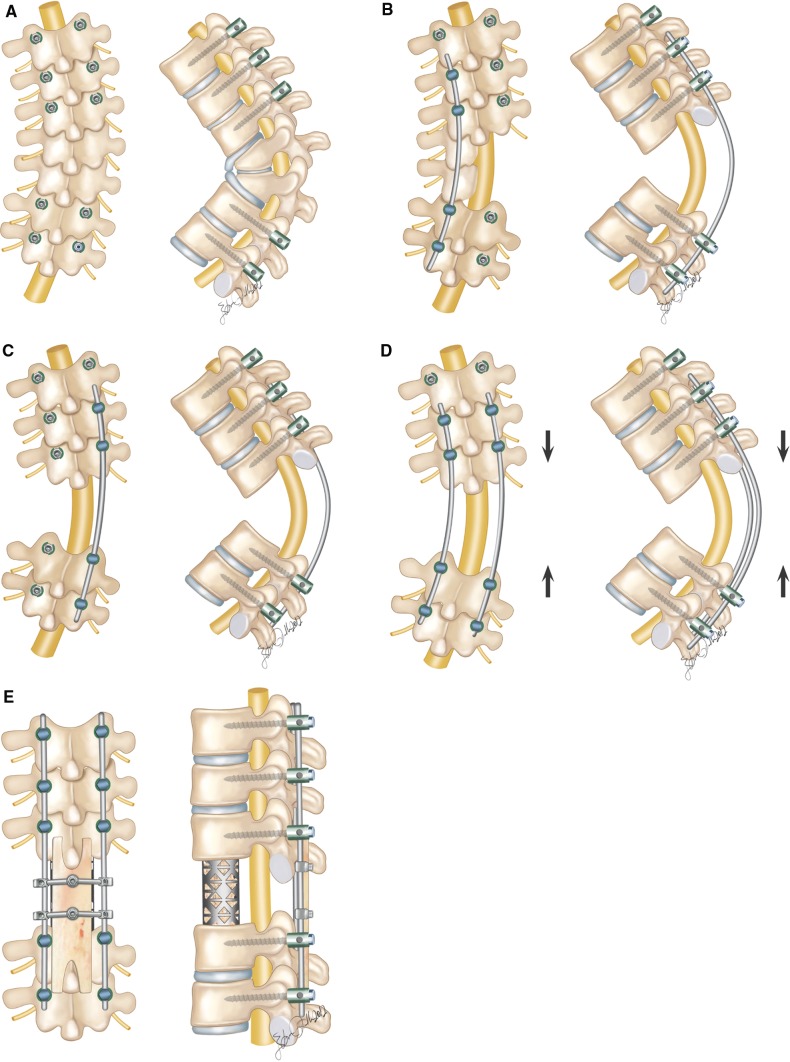
Fig. 9.
Posterior vertebral column resection (PVCR). a Pedicle screws are inserted segmentally, except for the resected levels. b Posterior neural arches, vertebral body and the discs are removed on one side after fixation with a temporary rod on contralateral side. c Temporary rod is moved on the other side and the same resection procedure is carried out on the left side. d Deformity is corrected gradually by compression, in situ bending and changing the temporary rods alternately. e A mesh cage is usually placed anteriorly to prevent too much shortening of the spinal column. An H-shaped femoral allograft is placed over the laminectomy side between the spinous processes and a final compression is done to secure the stabilization
In the surgical technique, the pedicle screws are inserted segmentally, except for the resected levels (Fig. 9a). The screws are connected on one side with a temporary rod contoured to the shape of the deformity without any attempt for correction. After a wide laminectomy (one level above and one level below the resected level, to prevent neural impingement after correction), and bilateral foraminotomies to decompress the neural elements, resection of the vertebral column at the apex of the deformity is performed. In the thoracic spine, the exposed nerve roots are sacrificed to facilitate exposure, and the corresponding rib heads are removed to expose the lateral walls of the pedicle. The stabilizing rod is then placed at one side (usually convex side at coronal plane deformities) (Fig. 9b). Careful subperiosteal dissection is used on the working site (opposite to the stabilizing rod) to follow the lateral wall of the vertebral body until the anterior aspect is easily palpable. The discs above and below the planned resection level are then removed, followed by resection of the pedicle and vertebral body on one side using osteotomes and a high speed drill. A thin shell of bone at the anterior part along with the anterior longitudinal ligament is preserved to protect translation. A reverse curette is usually used to remove the thin shell of the posterior bone at the working side and adjacent to the dural tube. After resection of the posterior wall on the working side, another temporary rod is inserted at this side and securely locked to the screws with slight compression to shorten the vertebral column (Fig. 9c). The temporary rod on the opposite side is then removed to allow resection of the remaining vertebra. The same sequence of resection is performed on the remaining vertebra. After completion of the resection, the second rod is placed at this side. A final evaluation of the spinal canal is then performed to confirm that there is no residual bone or disc tissue anterior to the dura. Deformity correction is performed gradually by compression, in situ contouring, and replacing the kyphotic rods with rods precontoured to the physiological contours (Fig. 9d). A mesh cage is usually placed anteriorly to prevent too much shortening of the spinal column, which may cause a dural buckling that risks the spinal cord. An H-shaped structural allograft can be placed over the laminectomy side between the spinous processes and a final compression is done to secure the stabilization (Fig. 9e) [23]. Closure of the osteotomy side using an H-shaped allograft may help prevent haematoma formation and may increase the fusion rate.
There are several advantages of PVCR for correction of rigid severe deformity. It enables manipulation in every direction under a simultaneous control of both anterior and posterior sites of the spinal column and provides better correction than the other types of osteotomies (Fig. 10). It is a single procedure compared to combined anterior and posterior VCR reducing the total operating time and the amount of blood loss and also avoiding opening of the thoracic cage and pleura. Avoiding anterior surgery may be very beneficial for patients with severe pulmonary function compromise because of severe thoracic deformity.
Fig. 10.
Illustrative case for PVCR. 43-year-old female patient with severe kyphoscoliosis deformity. PVCR was performed at T10 vertebra level. A titanium mesh cage was used for anterior column reconstruction
Hamzaoglu et al. [23] reported an average correction rate of 62 % in coronal and 72 % in sagittal plane in their series of 102 severe adult deformity patients. Suk et al. [26] reported a correction of 61.9° in the coronal plane and 45.2° in the sagittal plane in their series of 70 patients. In a series of 35 children, Lenke et al. [27] noted major curve improvements as 51 % in scoliosis cases, 55 % in global kyphosis cases, 58 % in angular kyphosis cases, 54 % in kyphoscoliosis cases, and 60 % in congenital scoliosis cases after PVCR. The same authors reported another series of PVCR including a slightly larger number of adults and children with severe deformity. Correction rates were 69 % for scoliosis, 54 % for global kyphosis, 63 % for angular kyphosis, and 56 % for kyphoscoliosis [23, 26, 27].
One major concern with PVCR technique is the potential for neurologic complications, which may result from direct neurologic injury during bone resection or deformity correction. Neurologic complications may also result from subluxation of the spinal column, dural buckling and compression of the spinal cord by residual bone or soft tissues in the canal after correction. Suk [26] reported a 34.3 % overall rate of complications and a 17.1 % rate of neurologic complications. Lenke et al. [27] reported a similar 40 % overall rate of complications and a 11.4 % rate for neurological complications. Hamzaoglu et al. [23] reported a 7.84 % overall complication rate including transient nerve palsies in 1.96 % of patients.
In conclusion, PVCR is the most powerful posterior osteotomy method providing a successful correction of stiff complex deformities. It also entails longer operating time and blood loss than less invasive osteotomies. It is a technically demanding procedure with possible risks for major complications. Therefore, only a highly experienced surgical team should perform it. Spinal cord neuromonitoring is mandatory to prevent catastrophic neurologic injuries.
Conclusions
Osteotomies in spinal deformity are powerful techniques, enabling the spine surgeon to correct and balance the decompensated, rigid spinal deformities. Balance is the ultimate goal in deformity correction, depending on the type of deformity this can be reached through a variety of osteotomy techniques. Preoperative assessment of the deformity can help to determine which osteotomy is best suited and how much angular correction is needed. Patient’s general medical status and surgeon’s experience levels are the other factors for determining the ideal treatment.
It is important to understand sagittal imbalance and the surgeon must consider global spino-pelvic alignment for satisfactory long-term results. Vertebral osteotomies are technically challenging but effective procedures for the correction of adult deformities.
Conflict of interest
None.
References
- 1.Schwab FJ, Smith VA, Biserni M, Gamez L, Farcy JP, Pagala M (2002) Adult scoliosis: a quantitative radiographic and clinical analysis. Spine (Phila Pa 1976) 27:387–392 [DOI] [PubMed]
- 2.Heary RF. Evaluation and treatment of adult spinal deformity. J Neurosurg Spine. 2004;1:9–18. doi: 10.3171/spi.2004.1.1.0009. [DOI] [PubMed] [Google Scholar]
- 3.Cho W, Lenke LG. Vertebral osteotomies—review of current concepts. Musculoskeletal Rev. 2010;5:46–49. [Google Scholar]
- 4.Aebi M. The adult scoliosis. Eur Spine J. 2005;14:925–948. doi: 10.1007/s00586-005-1053-9. [DOI] [PubMed] [Google Scholar]
- 5.Silva FE, Lenke LG. Adult degenerative scoliosis: evaluation and management. Neurosurg Focus. 2010;28(3):1–10. doi: 10.3171/2010.1.FOCUS09271. [DOI] [PubMed] [Google Scholar]
- 6.Birknes JK, White AP, Albert TJ, Shaffrey CI, Harrop JS. Adult degenerative scoliosis a review. Neurosurgery. 2008;63(3):94–103. doi: 10.1227/01.NEU.0000325485.49323.B2. [DOI] [PubMed] [Google Scholar]
- 7.Dorward GI, Lenke GL. Osteotomies in the posterior only treatment of complex adult spinal deformity: a comparative review. Neurosurg Focus. 2010;28(3):1–10. doi: 10.3171/2009.12.FOCUS09259. [DOI] [PubMed] [Google Scholar]
- 8.Bridwell KH. Decision making regarding Smith-Petersen vs. pedicle subtraction osteotomy vs. vertebral column resection for spinal deformity. Spine. 2006;31(19):171–178. doi: 10.1097/01.brs.0000231963.72810.38. [DOI] [PubMed] [Google Scholar]
- 9.Lafage V, Schwab F, Patel A et al (2009) Pelvic tilt and truncal inclination: two key radiographic parameters in the setting of adults with spinal deformity. Spine (Phila Pa 1976) 34:599–606 [DOI] [PubMed]
- 10.Schwab F, Patel A, Ungar B et al (2010) Adult spinal deformity-postoperative standing imbalance: how much can you tolerate? An overview of key parameters in assessing alignment and planning corrective surgery. Spine (Phila Pa 1976) 35:2224–2231 [DOI] [PubMed]
- 11.Bernhart M, Bridwell KH. Segmental analysis of the sagittal plane alignment of normal thoracic and lumbar spines and thoracolumbar junction. Spine. 1989;14(7):717–721. doi: 10.1097/00007632-198907000-00012. [DOI] [PubMed] [Google Scholar]
- 12.Ondra SL, Marzouk S, Koski T, Silva F, Salehi S. Mathematical calculation of pedicle subtraction osteotomy size to allow precision correction of fixed sagittal deformity. Spine. 2006;25:973–979. doi: 10.1097/01.brs.0000247950.02886.e5. [DOI] [PubMed] [Google Scholar]
- 13.Smith-Petersen MN, Larson EB, AuFranc OE. Osteotomy of the spine for correction of flexion deformity in rheumatoid arthritis. J Bone Joint Surg Am. 1945;27:1–11. [PubMed] [Google Scholar]
- 14.Ponte A, Vero B, Siccardi GL. Surgical treatment of Scheuermann’s kyphosis. In: Winter RB, editor. Progress in spinal pathology: kyphosis. Bologna: Aulo Gaggi; 1984. pp. 75–80. [Google Scholar]
- 15.Cho KJ, Bridwell KH, Lenke GL, Berra A, Baldus C. Comparison of Smith-Petersen versus pedicle substraction osteotomy for correction of fixed sagittal imbalance. Spine. 2005;30(18):2030–2037. doi: 10.1097/01.brs.0000179085.92998.ee. [DOI] [PubMed] [Google Scholar]
- 16.Thomasen E. Vertebral osteotomy for correction of kyphosis in ankylosing spondylitis. Clin Orthop Relat Res. 1985;194:142–152. [PubMed] [Google Scholar]
- 17.Heining CA. Eggshell procedure. In: Luque ER, editor. Segmental spinal instrumentation. Slack: Thorofare; 1984. pp. 221–230. [Google Scholar]
- 18.Kim JY, Bridwell KH, Lenke GL, Cheh GE, Baldus C. Results of lumbar pedicle substraction osteotomies of fixed sagittal imbalance a minimum 5-year follow-up study. Spine. 2007;32(20):2189–2197. doi: 10.1097/BRS.0b013e31814b8371. [DOI] [PubMed] [Google Scholar]
- 19.Buchowski JM, Bridwell KH, Lenke LG, Kuhns CA, Lehman RA, Kim JY, Stewart D, Baldus C. Neurologic complications of lumbar pedicle subtraction osteotomy a 10-year assessment. Spine. 2007;32(20):2245–2252. doi: 10.1097/BRS.0b013e31814b2d52. [DOI] [PubMed] [Google Scholar]
- 20.Yang BP, Ondra SL, Chen LA, et al. Clinical and radiographic outcomes of thoracic and lumbar pedicle subtraction osteotomy for fixed sagittal imbalance. J Neurosurg Spine. 2006;5:9–17. doi: 10.3171/spi.2006.5.1.9. [DOI] [PubMed] [Google Scholar]
- 21.Ahn UM, Ahn NU, Buchowski JM, et al. Functional outcome and radiographic correction after spinal osteotomy. Spine. 2002;27:1303–1311. doi: 10.1097/00007632-200206150-00011. [DOI] [PubMed] [Google Scholar]
- 22.Domanic U, Talu U, Dikici F, Hamzaoglu A. Surgical correction kyphosis; posterior total wedge resection osteotomy in 32 patients. Acta Orthop Scand. 2004;75(4):449–455. doi: 10.1080/00016470410001231-1. [DOI] [PubMed] [Google Scholar]
- 23.Hamzaoglu A, Alanay A, Ozturk C, Sarier M, Karadereler S, Ganiyusufoglu K. Posterior vertebral column resection in severe spinal deformities. Spine. 2011;36(5):340–344. doi: 10.1097/BRS.0b013e3182015712. [DOI] [PubMed] [Google Scholar]
- 24.Ozturk C, Alanay A, Ganiyusufoglu K, Karadereler S, Ulusoy L, Hamzaoglu A (2011) Short term X-ray results of posterior vertebral column resection in severe congenital kyphosis, scoliosis and kyphoscoliosis Spine [Publish Ahead of Print] [DOI] [PubMed]
- 25.MacLennan A. Scoliosis. BMJ. 1922;2:865–866. [Google Scholar]
- 26.Suk SI, Chung ER, Kim JH, et al. Posterior vertebral column resection for severe rigid scoliosis. Spine. 2005;30(14):1682–1687. doi: 10.1097/01.brs.0000170590.21071.c1. [DOI] [PubMed] [Google Scholar]
- 27.Lenke LG, O’Leary PT, Bridwell KH, Sides BA, Koester LA, Blanke KM. Posterior vertebral column resection for severe pediatric deformity: minimum two-year follow-up of thirty-five consecutive patients. Spine. 2009;34:2213–2221. doi: 10.1097/BRS.0b013e3181b53cba. [DOI] [PubMed] [Google Scholar]