Abstract
Introduction
Obtaining a fusion, especially to the sacrum for adult deformity correction remains a challenge. Prior to modern fixation techniques, the reported fusion rates for adult scoliotic deformities were low. However sacropelvic fixation techniques for adult deformity continue to evolve. As a result, modern day pelvic fixation techniques have improved fusion rates at the base of long constructs. The purpose of this article is to discuss the history, indications, and modern fixation techniques for pelvic fixation in the surgical management of adult scoliosis patients.
Methods
We searched PUBMED using the search terms pelvic fixation, deformity, lumbopelvic, sacropelvic, and iliac fixation. Linkage or association studies published in English and available full-text were analyzed specifically regarding techniques and innovations in pelvic fixation.
Results
Sacropelvic fixation should be considered in any patient with a long construct ending in the sacrum, those patients with associated risk factors for loss of distal fixation or high risk for pseudarthrosis at L5–S1, and those undergoing three column osteotomies or vertebral body resections in the low lumbar spine. Current pelvic fixation techniques with iliac screws, multiple screw/rod constructs, and S2-alar-iliac screws are all viable techniques for achieving pelvic fixation.
Conclusions
There is growing evidence that pelvic fixation may become the standard for obtaining long fusions in adult scoliosis. Although technically challenging, in selected cases the use of four pelvic screws and/or four rods across the lumbosacral pelvis can help address pseudarthroses, implant breakage, and screw pullout secondary to osteoporosis. Ultimately, indications and techniques should be individualized to the patient and based on surgeon preference and experience.
Keywords: Adult deformity, Scoliosis, Pelvic fixation, Lumbopelvic, Sacropelvic, Iliac fixation
Introduction
Tremendous advances have been made to improve fusion rates and outcomes in adult deformity patients. With modern fixation techniques, the reported pseudarthrosis rates in adult deformity patients managed with long construct fusions are as low as 3–5 % [1]. Sacropelvic fixation is constantly evolving and the optimal technique and indications are still being developed and redefined. Despite the controversies that exist, pelvic fixation remains a viable method for achieving fixation at the base of long construct fusions. There is growing evidence that pelvic fixation may become the standard for obtaining long fusions in adult scoliosis. The purpose of this article is to discuss the history, indications, and modern fixation techniques for pelvic fixation in the surgical management of adult scoliosis patients [2–4].
History
Obtaining a fusion, especially to the sacrum, for adult deformity correction remains a challenge. Prior to modern fixation techniques, the reported fusion rates for adult scoliotic deformities were low [5]. Historically, due to the difficulty with obtaining a solid fusion at the lower lumbar levels and lumbosacral junction many surgeries involving long construct fusions resulted in poor outcomes [1, 3, 4].
Prior to modern instrumentation, fusions relied primarily on body casting, resulting in secondary complications due to prolonged immobilization. Furthermore, frequently fusions were not obtained [6, 7]. Instrumentation of the spine became common with the development of Harrington rod instrumentation in the 1960s and 1970s.
However, Harrington rod fixation utilized limited fixation points and this fact, combined with the use of distraction for correction of deformities resulted in a high incidence of flatback deformities and loss of lumbar lordosis. Kostuik et al. [8] reported a rate of pseudarthrosis and flatback deformities as high as 40 and 50 %, respectively, in their series of 48 adult scoliotic patients who underwent fusion to the sacrum. Similarly, in 1986 Balderston et al. [5] reported on their experience with a nonparalytic adult scoliosis patients and noted that 37 % of their patients developed a flatback deformity.
Late in the 1970s, pelvic fixation was improved when Luque developed a technique to obtain multiple points of fixation using sublaminar wiring connecting to L-shaped rods to prevent rod migration [9, 10]. This concept of “segmental instrumentation” improved pelvic fixation and allowed for better correction of the deformity because it reduced the required distraction for correction, and subsequently improved sagittal balance.
Further progress for sacropelvic fixation came about when Allen and Ferguson described their experience with the Galveston technique in 1976 [11]. The technique involved placing an L-shaped rod between the inner and outer tables of the pelvis which significantly increased the stiffness and biomechanical stability at the lumbosacral junction in both flexion and side bending. Bradford reported a 7 % pseudarthrosis rate with the Galveston technique [7].
Another major advance in sacropelvic fixation was the Cotrel–Dubousset system, which achieved sacropelvic fixation using a hybrid construct with hooks and caudal pedicle screw fixation [12–15].
Considerations for pelvic fixation in adult deformity
Clinical challenge and goals
Several clinical challenges exist in the surgical management of the patient with adult deformity. Correction of both sagittal and coronal plane deformities frequently requires long posterior constructs. In particular, long constructs that extend from the thoracic spine into the distal lumbar spine and/or sacrum result in large lever arms and cantilever forces that result in high stresses at the base of the construct. Furthermore, in the sacrum, the S1 and S2 pedicles are largely cancellous, and in the elderly patient frequently osteoporotic, which can result in distal implant pullout.
Therefore, the main goal for pelvic fixation is to achieve a stable base and maintain the surgical correction of the spinal deformity until a solid fusion is obtained. Philosophically, whenever possible preserving motion segments and avoiding fixation to the sacrum should be the goal. Maintaining the L5–S1 segment can help preserve significant motion because the L5–S1 segment is responsible for the largest amount of flexion/extension [31, 32]. However, frequently this is not possible and in patient with multiple risk factors for pseudarthrosis (i.e., smoking, diabetes, previous pseudarthrosis, osteopenia, etc.) then strong consideration should be given to increasing the biomechanically stability of the construct with distal fixation into the sacropelvis [26].
Iliac screws have an attractive biomechanical profile because they are divergent from the proximal fixation points in the coronal plane and, therefore, “out of line” from the rest of the bone anchors, which unlike S1 and S2 sacral screws, allows them to better resist distal pullout. Furthermore, they are frequently long screws that place them anterior to the access of the rotation of the pelvis, which further helps to resist distal pullout. McCord showed that iliac screws and Galveston Rods were the best at resisting flexion moments [22].
Although covered in a separate chapter in this journal issue, placement of anterior column support with interbody fixation at L5–S1 should be considered as well. The ability to achieve anterior column support combined with sacropelvic fixation may further reduce the rates of pseudarthrosis, screw pullout, and implant breakage.
Indications
Indications for sacropelvic fixation continue to evolve (Table 1). Commonly reported indications for pelvic fixation include patients with high-grade spondylolisthesis, unstable sacral fractures, sacral tumors, and insufficiency fractures [16–18, 33]. However, by far the most common reason for pelvic fixation remains for the management of long constructs in adult deformity patients. Although there are no absolute indications for pelvic fixation, certainly poor fixation in the sacrum and sacral fractures that preclude sacral fixation are strong indications for extension to the pelvis.
Table 1.
Relative indications for pelvic fixation
| High-grade spondylolisthesis |
| Unstable sacral fractures |
| Sacral tumors |
| Long constructs around/past the TL junction |
| Osteoporosis and/or poor sacral fixation requiring pelvic fixation |
| Three column osteotomy/vertebral column resection at lumbosacral junction |
Furthermore, any patient who requires extension of the construct to the sacrum, should be considered for extension to the pelvis. Although currently there is no literature that identifies a transition point from sacral fixation to the pelvis, it is typical in our practice to consider pelvic fixation in any patient where the proximal construct is at L2 or proximal [4, 19–21]. Other considerations include any patient with significant coronal and sagittal plane deformities where ending the distal construct at L5 would result in residual coronal tilt or sagittal kyphosis would warrant consideration of extension to the sacropelvis.
As discussed above, any patient with long construct with associate risk factors for either loss of distal fixation or high risk for pseudarthrosis at L5–S1 should be considered as a candidate for pelvic fixation. Finally, patients undergoing three column osteotomies or vertebral body resections in the low lumbar spine and/or lumbosacral junction should be considered for pelvic fixation to maintain distal fixation points and achieve rigid distal fixation.
Insufficiency fractures of the sacrum can be an indication for lumbopelvic fixation. These are fractures emanating from the sacral ala bilaterally and typically complete between adjacent sacral body segments causing focal kyphosis. They are becoming a more recognized etiology of groin, low back, and buttock pain, and a high index of clinical suspicion should be maintained as delays to this diagnosis can result in neurologic compromise in up to 2 % of patients [33, 34]. Usually this occurs in osteoporotic patients, patients with metabolic derangements, and in patients after previous lumbosacral fixation of the spine [35, 36].
Although controversial, if conservative treatment fails to obtain a united fracture, improve pain, or if neurologic compromise and progressive deformity occurs then lumbopelvic fixation has been shown to help reverse patients neurologic symptoms, improve pain, and allow for physiologic fracture healing [36, 37]. Further prospective studies are needed to determine when to transition from conservative measures to possibly sacroplasty or augmented instrumented lumbopelvic fixation [37, 38].
Relative contraindications include patients with poor anatomy or previous surgery precluding safe placement of pelvic fixation. Interestingly, history of previous iliac crest bone harvest frequently does not necessarily preclude pelvic fixation.
Sacropelvic fixation
Sacral fixation
Although not technically pelvic fixation, S1, S2, and alar screws are part of the concept of “sacropelvic” fixation, and, therefore, worth describing briefly here. A full description is provided elsewhere.
S1 screws are placed through a wide pedicle with less cortical bone to allow for screw purchase; as a result, when used alone in long constructs, are prone to pullout failure or allow for motion increasing the rates of pseudarthrosis especially at the L5–S1 level. Tricortical fixation with the screws directed toward the sacral promontory improves the biomechanical stability [23].
S2 pedicle screws can be placed as well to allow for improved lumbosacral fixation; however, they have not been shown to significantly increase construct stiffness [24, 25]. Furthermore, these screws are technically demanding due to a narrow safe zone. Since they do not significantly increase the stability at the base of the construct, coupled S1–S2 screw constructs offer limited protection of the S1 pedicle screws when compared to coupled S1-iliac screw constructs [24, 25].
Alar screws similarly have a narrow safe zone and although may improve the stability of the construct base, they have not been shown clinically to significantly reduce pseudarthrosis rates [24]. As a result, these screws are typically not used in isolation, but more recently S2 and alar screw trajectories have been modified to achieve pelvic fixation in the form of S2-alar-iliac (S2AI) screws.
Pelvic fixation
Iliac screws/bolts
Modern day segmental instrumentation has allowed for fixation points in the ilium independent of the proximal construct. As a result, iliac screws/bolts are now commonly used. The addition of iliac screws can help to protect S1 pedicle screws [25]. Furthermore, coupled S1-iliac screws at the base of long constructs have been shown to enhance fusion rates [26].
Technically, the starting point for the iliac screw is identified by exposing the posterior superior iliac spine (PSIS). In the attempt to reduce the incidence of prominent screw heads, the entry point for iliac screw is typically placed slightly deep to the PSIS along the medial aspect of the inner table of the ilium. The muscular attachments and soft tissue is carefully detached, and this area is exposed using electrocautery. The starting point is obtained either with a rongeur or a high-speed burr. Using an iliac probe the pathway of the screw trajectory is identified.
The trajectory is highly variable, but typically is angled approximately 20–45 degrees caudal and 30–45 degrees lateral. Gently advancing the probe should allow for the trajectory to stay between the inner and outer tables of the ilium. In selected cases, placement of two pelvic screws per ilium can be performed as well. In these cases, careful planning of the first screws will make placement of the second screw easier (Fig. 1a).
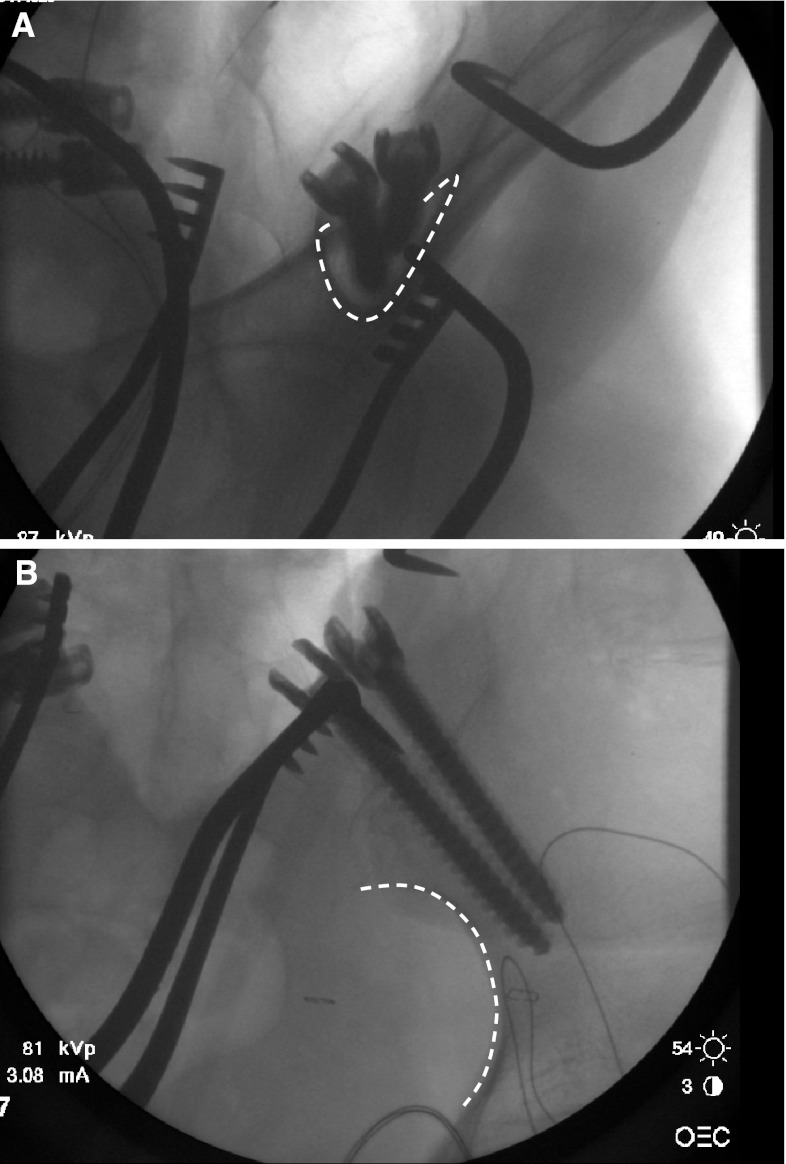
Fig. 1.
a Obturator oblique radiograph demonstrating two iliac screws. Dotted line outlines the “tear drop,” which is the thick supra-acetabular column of bone. b Iliac oblique radiograph demonstrating two iliac screws in the supra-acetabular column of bone above the greater sciatic notch (dotted line)
Depending on surgeon preference and comfort, the use of intraoperative fluoroscopy, or intraoperative 3D or CT imaging, or computer image guidance can be helpful as well. In complex cases, revision pelvic cases, and patients with unusual pelvic morphology, the use of a preoperative CT can be helpful to identify the patient specific anatomy, but is not routinely necessary. In addition, previous history of iliac crest bone graft harvest does not preclude placement of iliac screws.
At our institution, in selective cases, the use of intraoperative fluoroscopy has been helpful in confirming proper trajectory. The use of the obturator oblique view helps to identify the thick column of bone just above the greater sciatic notch also known as the “teardrop” (Fig. 1a). Placement of the iliac screw approximately 1 cm above the greater sciatic notch, in the supra-acetabular region allows for better screw purchase in the thickest part of the ilium.
The iliac oblique view places the iliac wing en face and confirms that the screw trajectory is above the neurovascular structures in the greater sciatic notch (Fig. 1b). There is potential for injury to the sciatic nerve or superior gluteal artery if the sciatic notch is entered but this is a rare complication.
Confirmation that the screw remains outside the hip joint is also important and can typically be seen on routine AP or lateral radiographic views. However, when in doubt, combination of inlet, outlet, and/or obturator views can help confirm that the hip joint has not been violated.
S1/iliac screw alignment technique
One of the challenges involving iliac screw placement is obtaining longitudinal alignment of the S1 screw with the more proximal screw. Using a medial–lateral connector between the iliac screw and S1 screw allows for an easier connection to the longitudinal rods, but introduces another potential interface for loosening or implant failure.
Alternatively, if a connector is not used, direct placement of the longitudinal rod into a polyaxial iliac screw and S1 screw can be achieved by creating a more dramatic lordotic bend in the longitudinal rod combined with potentially leaving the S1 screw head slightly more lateral and prominent can help with completing this connection. The disadvantage of this technique is that there is increased risk of implant prominence if the iliac screw is not left deep and flush within the iliac bone.
Although technically challenging, using a convergent lateral starting point 5 mm outside the SI joint allows for side openings in the iliac screw to line up perfectly with the proximal screws and still allows for a deeply buried screw head [40]. The rod should be placed first into the iliac screw and then into the S1 screw head.
Unilateral pelvic screw fixation
Although not routinely performed at our institution, the use of unilateral pelvic fixation has the potential to improve clinical outcomes without compromising biomechanical stability [39]. Although theoretically this has the potential to decrease operative time, soft tissue dissection, blood loss, and implant hardware prominence, further studies with long-term outcomes are needed to truly determine if there is equivalent difference between pseudarthrosis and construct failures.
S2-alar-iliac screw for pelvic fixation
More recently, Kebaish [3] described the use of a S2AI screw, which allows for fixation into the pelvis while utilizing a S2 starting point (Fig. 2). This technique still allows for placement of large diameter, long pelvic screws without the prominence of the PSIS starting point. By utilizing a S2 starting point, the head of the S2AI pedicle screw is placed both deeper and more medial than the PSIS starting point of the traditional iliac screw. As previously described, the staring point is typically 2–4 mm lateral and 4–8 mm distal to the S1 foramen [3].
Fig. 2.

Axial CT scan demonstrating path of S2-alar-iliac screw. Notice the more medial starting point in the S2 pedicle with the screw traversing the SI joint into the ilium laterally
This has several advantages. First, the more medial starting point puts the screw directly in line with the S1 screw and, therefore, makes linkage of the longitudinal rod to the bony anchors more direct and typically avoids the need for medial-to-lateral connectors. Second, the S2AI screw is more deeply placed and, therefore, avoids the common problem of painful implants from the limited overlying tissue.
One concern of this technique is associated with the fact that by design the S2AI screw starts from the sacrum and is placed across the SI joint and into the ilium. If this affects long-term patient outcomes due to SI joint arthritis or pain is yet to be determined. Despite this concern, increasing familiarity with this technique has shown that percutaneous placement of the S2AI screw is technically feasible [27, 28].
Four-rod technique
Besides pedicle screw pullout, rod and screw failure remains a common and potential problem in patients, particularly those with pseudarthrosis. In these cases, achieving solid bony fixation may address the issue of implant pullout, however does not necessarily reduce the risk of implant breakage. Newer titanium alloy metals along with the use of cobalt chrome or stainless steel has reduced this complication, however has not eliminated it. In these cases, novel constructs, such as the use of 4-rod technique as described by Shen et al. [18] or placement of 4 iliac screws can be considered as well (Figs. 3, 4, 5).
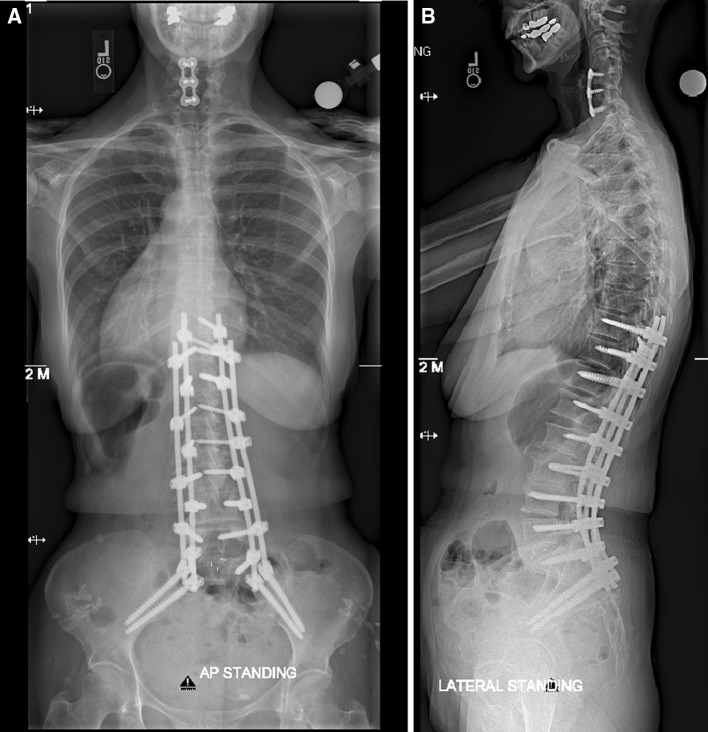
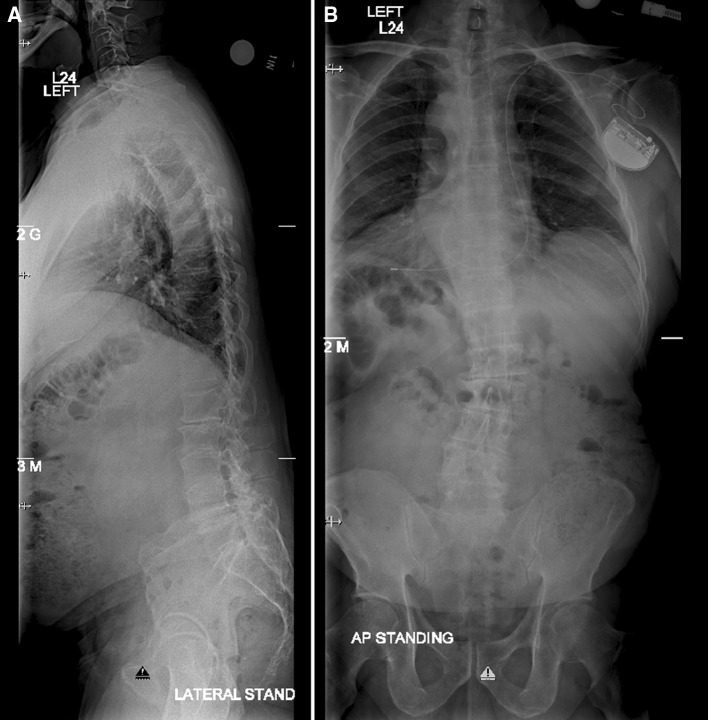
Fig. 3.
Preoperative a AP and b lateral 36-inch standing scoliosis films demonstrating an adult scoliosis with loss of lumbar lordosis. Patient had four previous decompressions with in situ fusions
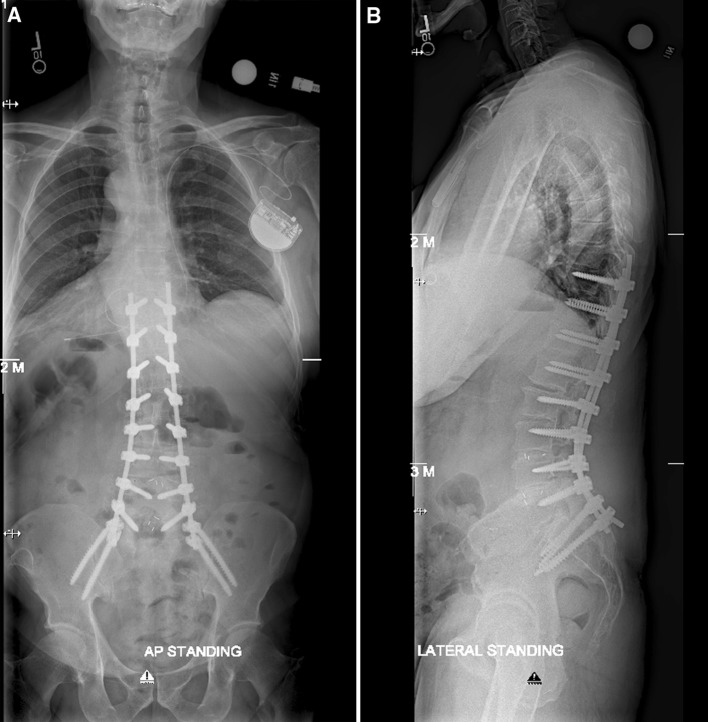
Fig. 4.
Coronal CT reconstruction view demonstrating solid posterior lateral fusion mass (arrowheads) from L3 to sacrum confirms a rigid, stiff lumbar curve
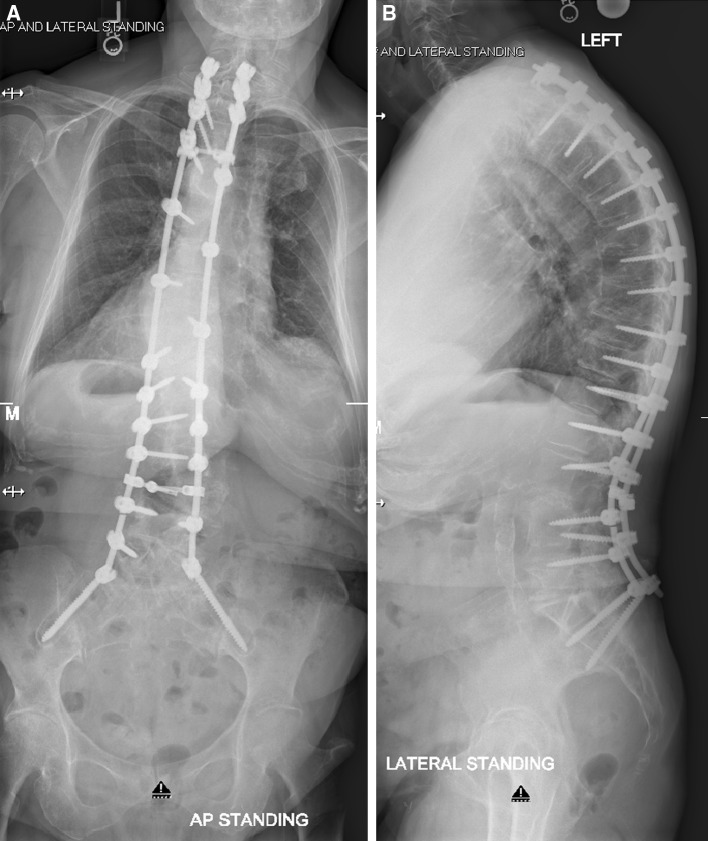
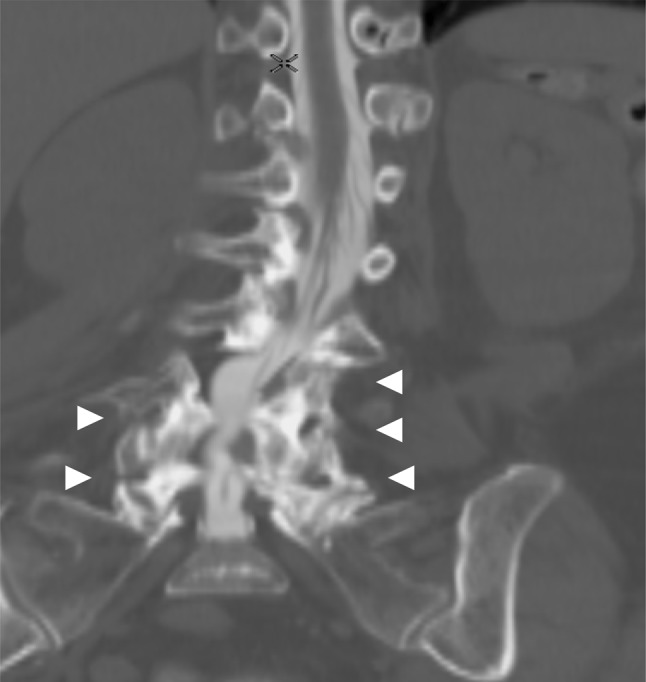
Fig. 5.
Postoperative a AP and b lateral 36-inch standing scoliosis films demonstrating four-rod with four pelvic screw fixation for restoration of coronal alignment and lumbar lordosis
Although technically challenging, the 4-rod technique uses differing insertion angles of pedicle screws to allow for placement of two rods on each side of the construct. This has been shown to be biomechanically superior to the standard two-rod technique [26]. Similarly, placement of 4-pelvic screws has increased distal pullout and screw breakage (Figs. 6, 7, 8). As a result, several variations have been used by the authors to help address various spinal pathologies with good results (Figs. 9, 10).
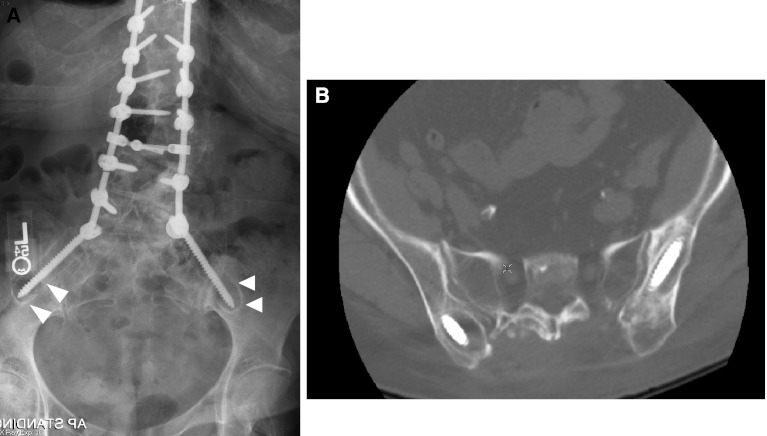
Fig. 6.
a AP and b lateral 36-inch standing radiographs demonstrating marked loosening of pelvic fixation with loss of both coronal and sagittal alignment
Fig. 7.
a AP lumbar radiograph confirming lucency around pelvic screw with surrounding “halo” (arrowheads). b Axial CT scan confirming loose pelvic fixation
Fig. 8.
Postoperative a AP and b lateral 36-inch standing radiographs with four-rod technique demonstrating restoration of coronal and sagittal alignment. Notice that 4 pelvic screws were cement augmented to increase purchase within the ilium
Fig. 9.
Preoperative a AP and b lateral 36-inch standing scoliosis films demonstrating an adult scoliosis with loss of lumbar lordosis and positive sagittal balance
Fig. 10.
Postoperative a AP and b lateral 36-inch standing scoliosis films demonstrating standard two-rod with four pelvic screw fixation for restoration of coronal and sagittal alignment. Four pelvic anchors were utilized distally secondary to extensive osteoporosis
The four-rod technique may obviate the need for multiple level anterior column support given the biomechanical superiority [26]. Further biomechanical and clinical studies would be beneficial to determine indications for the addition or exclusion of anterior column support to obtain similar fusion rates and improve clinical outcomes.
Complications of fixation
Overall complication rates have not been frequently reported. Cho et al. reported an 11 % major failure rate overall failure rate in patients with pelvic fixation used in adult deformity patients [41]. Major failures were defined as rod breakage between L4 and S1, failure of S1 screws (breakage, halo formation, or pullout), and prominent iliac screws requiring removal.
One common complication associated with pelvic fixation is prominent and painful implants. The reported rates of clinically significant prominent implants has been reported as high as 20 % [29, 30]. This complication can be reduced by preparing a wide trough at the entry point near the PSIS to accommodate the iliac screw head. Alternatively, utilizing the S2AI technique can also help reduce implant prominence as well [3, 27].
Infection is a common complication associated with adult deformity surgery and is due to the extensive surgical exposure that is typically required and not specifically secondary to the use of pelvic fixation with reported rates around 4 % [30]. Although unclear, evolving surgical techniques such as minimally invasive techniques and image-guided surgery can reduced surgical trauma and soft tissue injury which may further reduce wound complications and infections, while improving patient recovery and outcomes.
One common complication of unknown importance is whether or not radiographic evidence of loosening of pelvic fixation is of clinical significance. Theoretically motion across the SI joint is common, even after a solid fusion has occurred across the lumbosacral junction and, therefore, some amount of haloing around the iliac screw, or even rod breakage between the S1 screw and iliac screw, can be expected. In a review of 67 adult deformity patients, Cho et al. [41] demonstrated that patients with haloing or even rod breakage around pelvic fixation had improved outcomes similar to the control group without haloing. However, these findings were noted at 2 years after surgery, and intermediate and long-term results remain unknown.
Conclusion
Pelvic fixation and more specifically sacropelvic fixation for adult deformity continues to develop and evolve. Fusion rates at the base of long constructs have improved with modern day pelvic fixation techniques. As a result, absolute and relative indications for pelvic fixation have yet to be defined. Traditional pelvic fixation with iliac screws, multiple screw/rod constructs, and S2-alar-iliac screws are viable techniques for achieving pelvic fixation. Therefore, sacropelvic fixation should be considered in any patient with long construct ending in the sacrum, those patients with associated risk factors for loss of distal fixation or high risk for pseudarthrosis at L5–S1, and those undergoing three column osteotomies or vertebral body resections in the low lumbar spine. Ultimately, indications and techniques should be individualized to the patient and based on surgeon preference and experience.
Conflict of interest
None of the authors or family members of the authors have financial gains or stand to make financial gain associated with topics discussed in this manuscript. All authors were involved with the concept, plan, and writing of this manuscript.
References
- 1.Kostuik JP. Spinopelvic fixation. Neurol India. 2005;53:483–488. doi: 10.4103/0028-3886.22618. [DOI] [PubMed] [Google Scholar]
- 2.Boos N, Webb JK. Pedicle screw fixation in spinal disorders: a European view. Eur Spine J. 1997;6(1):2–18. doi: 10.1007/BF01676569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kebaish KM. Sacropelvic fixation: techniques and complications. Spine. 2010;35(25):2245–2251. doi: 10.1097/BRS.0b013e3181f5cfae. [DOI] [PubMed] [Google Scholar]
- 4.Bridwell KH, Kuklo T, Edwards CC, II, et al. Sacropelvic Fixation. Memphis: Medtronic Sofamor Danek; 2004. [Google Scholar]
- 5.Balderston RA, Winter RB, Moe JH, et al. Fusion to the sacrum for non paralytic scoliosis in the adult. Spine (Phila Pa 1976) 1986;11:824–829. doi: 10.1097/00007632-198610000-00017. [DOI] [PubMed] [Google Scholar]
- 6.Blumenthal S, Gill K. Complications of the Wiltse pedicle screw fixation system. Spine. 1993;18:1867–1871. doi: 10.1097/00007632-199310000-00024. [DOI] [PubMed] [Google Scholar]
- 7.Boachie-Adjei O, Dendrinos GK, Ogilvie JW, Bradford DS. Management of adult spinal deformity with combined anterior-posterior arthrodesis and Luque Galveston instrumentation. J Spinal Disord. 1991;4:131–141. doi: 10.1097/00002517-199106000-00002. [DOI] [PubMed] [Google Scholar]
- 8.Kostuik JP, Hall BB. Spinal fusions to the sacrum in adults with scoliosis. Spine. 1983;5:489–500. doi: 10.1097/00007632-198307000-00006. [DOI] [PubMed] [Google Scholar]
- 9.Luque ER, Cardoso A. Segmental correction of scoliosis with rigid internal fixation, preliminary report. Orthop Trans. 1977;1:136–137. [Google Scholar]
- 10.Luque ER. The anatomic basis and development of segmental spinal instrumentation. Spine (Phila Pa 1976) 1982;7:256–259. doi: 10.1097/00007632-198205000-00010. [DOI] [PubMed] [Google Scholar]
- 11.Allen BL, Jr, Ferguson RL. The Galveston experience with L-rod instrumentation for adolescent idiopathic scoliosis. Clin Orthop Relat Res. 1988;229:59–69. [PubMed] [Google Scholar]
- 12.Devlin VJ, Asher MA. Biomechanics and surgical principles of long fusions to the sacrum. Spine State Art Rev. 1996;10:515–544. [Google Scholar]
- 13.Cotrel Y, Dubousset J. New segmental posterior instrumentation of the spine. Orthop Trans. 1985;9:118. [Google Scholar]
- 14.Cotrel Y, Dubousset J, Guillaumat M. New universal instrumentation in spinal surgery. Clin Orthop Relat Res. 1988;227:10–23. [PubMed] [Google Scholar]
- 15.Camp JF, Caudle R, Ashmun RD, et al. Immediate complications of Cotrel-Dubousset instrumenatation to the sacro-pelvis. A clinical and biomechanical study. Spine (Phila Pa 1976) 1990;15:932–941. doi: 10.1097/00007632-199009000-00018. [DOI] [PubMed] [Google Scholar]
- 16.Mirkovic S, Abitbol JJ, Steinman J, Edwards CC, Schaffler M, Massie J, Garfin SR. Anatomic consideration for sacral screw placement. Spine. 1991;16(6 Suppl):S289–S294. [PubMed] [Google Scholar]
- 17.Matteini LE, Kebaish KM, Volk WR, Bergin PF, Yu WD, O’Brien JR. An S-2 alar iliac pelvic fixation. Technical note. Neurosurg Focus. 2010;28(3):E13. doi: 10.3171/2010.1.FOCUS09268. [DOI] [PubMed] [Google Scholar]
- 18.Shen FH, Harper M, Foster WC, Marks I, Arlet V. A novel “four-rod technique” for lumbo-pelvic reconstruction: theory and technical considerations. Spine. 2006;31(12):1395–1401. doi: 10.1097/01.brs.0000219527.64180.95. [DOI] [PubMed] [Google Scholar]
- 19.Kostuik JP. Treatment of scoliosis in the adult thoracolumbar spine with special reference to fusion to the sacrum. Orthop Clin North Am. 1988;19:371–381. [PubMed] [Google Scholar]
- 20.Devlin VJ, Asher MA. Biomechanics and surgical principles of long fusions to the sacrum. Spine State Art Rev. 1996;10:515–544. [Google Scholar]
- 21.Perra JH. Techniques of instrumentation in long fusions to the sacrum. Orthop Clin North Am. 1994;25:287–299. [PubMed] [Google Scholar]
- 22.McCord DH, Cunningham BH, Shondy Y, Myers J, McAffee PC. Biomechanical analysis of lumbosacral fixation. Spine. 1992;17:S235–S243. doi: 10.1097/00007632-199208001-00004. [DOI] [PubMed] [Google Scholar]
- 23.Lehman RD, Kulkot TR, Anderson RC, Belmont PJ, Polly DW, Orchowski JP, et al. Advantages of pedicle screw fixation directed into the apex of the sacral promontory over bicortical fixation: a biomechanical analysis. Spine. 2002;27:806–811. doi: 10.1097/00007632-200204150-00006. [DOI] [PubMed] [Google Scholar]
- 24.Zindrick MR, Wiltse LL, Widell EH, et al. A biomechanical study of intrapeduncular screw fixation in the lumbosacral spine. Clin Orthop Relat Res. 1986;203:99–112. [PubMed] [Google Scholar]
- 25.Lebwohl NJ, Cunningham BW, Dmitriev A, Boachie-Adjej O, Wagner TD. Biomechanical comparison of lumbo sacral fixation techniques in a calf spine model. Spine. 2002;27:2312–2320. doi: 10.1097/00007632-200211010-00003. [DOI] [PubMed] [Google Scholar]
- 26.Kuklo TR, Bridwell KH, Lewis SJ, Baldus C, Blanke K, Iffrig TM, Lenke LG. Minimum 2-year analysis of sacropelvic fixation and L5–S1 fusion using S1 and iliac screws. Spine. 2001;26:1976–1983. doi: 10.1097/00007632-200109150-00007. [DOI] [PubMed] [Google Scholar]
- 27.Kelly BP, Shen FH, Schwab JS, Arlet V, Diangelo DJ. Biomechanical testing of a novel four-rod technique for lumbo-pelvic reconstruction. Spine (Phila Pa 1976) 2008;33(13):E400–E406. doi: 10.1097/BRS.0b013e31817615c5. [DOI] [PubMed] [Google Scholar]
- 28.Sponseller PD, Zimmerman R, Ko PS, Kebaish KM, Pull ter Gunne A, Mohamed AS, Chang TL (2009) Low Profile Pelvic Fixation Using S2 Alar Iliac (S2AI) Fixation in the Pediatric Population Improves Results at Two Year Minimum Follow Up: Paper #86, Spine: Affiliated Society Meeting Abstracts: 23–26 September 2009. Scientific Program Abstracts, vol 10, p 114
- 29.O’Brien JR, Matteini L, Yu WD, Kebaish KM. Feasibility of minimally invasive sacropelvic fixation: percutaneous S2 alar iliac fixation. Spine (Phila Pa 1976) 2010;35(4):460–464. doi: 10.1097/BRS.0b013e3181b95dca. [DOI] [PubMed] [Google Scholar]
- 30.Kuklo TR, Bridwell KH, Lewis SJ, Baldus C, Blanke K, Iffrig TM, et al. Minimum 2-year analysis of sacropelvic fixation and L5–S1 fusion using S1 and iliac screws. Spine. 2001;26:1976–1983. doi: 10.1097/00007632-200109150-00007. [DOI] [PubMed] [Google Scholar]
- 31.Tsuchiya K, Bridwell KH, Kuklo TR, Lenke LG, Baldus C. Minimum 5-year analysis of L5–S1 fusion using sacropelvic fixation (bilateral S1 and iliac screws) for spinal deformity. Spine. 2006;31:303–308. doi: 10.1097/01.brs.0000197193.81296.f1. [DOI] [PubMed] [Google Scholar]
- 32.White AA 3rd, Panjabi MM (1978) The basic kinematics of the human spine. A review of past and current knowledge. Spine (Phila Pa 1976) 3(1):12–20 [DOI] [PubMed]
- 33.Mörl F, Wagner H, Blickhan R. Lumbar spine intersegmental motion analysis during lifting. Pathophysiology. 2005;12(4):295–302. doi: 10.1016/j.pathophys.2005.09.003. [DOI] [PubMed] [Google Scholar]
- 34.Lourie H. Spontaneous osteoporotic fracture of the sacrum. An unrecognized syndrome of the elderly. JAMA. 1982;248:715–717. doi: 10.1001/jama.1982.03330060055034. [DOI] [PubMed] [Google Scholar]
- 35.Dasgupta B, Shah N, Brown H, et al. Sacral insufficiency fracture; an unsuspected cause of low back pain. Br J Rheumatol. 1998;37:789–793. doi: 10.1093/rheumatology/37.7.789. [DOI] [PubMed] [Google Scholar]
- 36.Gotis-Graham I, McGuigan L, Diamond T, et al. Sacral insufficiency fractures in the elderly. J Bone Joint Surg Br. 1994;76:882–886. [PubMed] [Google Scholar]
- 37.Klineberg E, McHenry T, Bellabara C, et al. Sacral insufficiency fractures caudal to instrumented posterior lumbosacral arthrodesis. Spine (Phila Pa 1976) 2008;33(16):1806–1811. doi: 10.1097/BRS.0b013e31817b8f23. [DOI] [PubMed] [Google Scholar]
- 38.Weber M, Hasler P, Gerber H. Insufficiency fractures of the sacrum. Twenty cases and review of the literature. Spine. 1993;18:2507–2512. doi: 10.1097/00007632-199312000-00021. [DOI] [PubMed] [Google Scholar]
- 39.Garant M. Sacroplasty: a new treatment for sacral insufficiency fracture. J Vasc Interv Radiol. 2002;13:1265–1267. doi: 10.1016/S1051-0443(07)61976-9. [DOI] [PubMed] [Google Scholar]
- 40.Tomlinson T, Chen J, Upasani V, et al. Unilateral and bilateral sacropelvic fixation result in similar construct biomechanics. Spine. 2008;33:2127–2133. doi: 10.1097/BRS.0b013e31817bd8d5. [DOI] [PubMed] [Google Scholar]
- 41.Cho W, Mason J, Wilson A et al (2011) Failure of pelvic fixation after long construct fusions in adult deformity patients: clinical and radiographic risk factors. 46th Annual meeting of scoliosis research society. Louisville, Kentucky, 14–17 Sept 2011