Abstract
Purpose
To review the literature on the use of extreme lateral interbody fusion (XLIF) in adult spinal deformity, to discuss on its limits and advantages and to propose a guide to surgical strategy.
Methods
Surgical technique XLIF is a minimally invasive surgery (MIS) technique to anteriorly access the spine from midthoracic to L5. Important aspects of the technique are a muscle splitting approach through the psoas, use of advanced neuromonitoring to detect the lumbar plexus within the psoas, bilateral annulus release and large footprint interbody cages, supported by the stronger bone of ring apophyses. Large, laterally inserted cages provide strong correction of coronally asymmetrical disc spaces. Literature review MEDLINE database, the Web using Google Scholar and proceedings of the Society for Lateral Access Surgery meetings were searched for relevant articles on technique, results and complications.
Results
XLIF with posterior percutaneous pedicle screw instrumentation provides 40–75 % correction of coronal curves, with modest increase of lordosis. Only anterior XLIF can provide less correction. Self-limited thigh symptoms are frequent after transpsoas access. Permanent neural deficit and visceral complications have also been reported. Combined XLIF–MIS could have a lower complication compared to open circumferential surgery in historical series.
Conclusions
XLIF is a promising MIS option for adult deformity. Specific surgical strategies are needed to avoid imbalance and define ideal fusion levels and methods. An XLIF-based MIS strategy with a reduced number of levels of lumbar scoliosis can lead to significant advantages. Evaluation of the incidence, complications, their avoidance and real impact on patients’ outcomes is necessary to better understand the advantages of this approach. Studies comparing effectiveness and safety of traditional versus XLIF approaches are needed to assist evidence-based decision making.
Keywords: Adult scoliosis, Sagittal balance, Lateral interbody fusion, XLIF, Minimally invasive surgery
Introduction
Adult and elderly scoliosis surgery is an expanding field in spinal surgery. A higher expectation of life and pain-free functioning during aging have caused a steep increase in the number of candidates for deformity correction in the adult and elderly years of life. In the last decade, impressive effort has been made to increase the knowledge on this field. It has been demonstrated that this extensive surgery, previously considered to have poor balance between risk and outcomes, causes dramatic increases in health-related quality of life [1, 2]. The relative impact of curve magnitude, coronal imbalance and sagittal imbalance on outcomes has been well established [3–5]. Modern instrumentations now permit obtaining satisfactory stability in bone of poor quality. Normative values for spinal balance parameters [6, 7], harmony between those parameters [8] and outcomes research on the contribution of correction of some of these parameters to final clinical results now permit creating a preoperative surgical planning that reliably produces good results [9–14].
Still, adult deformity surgery remains extremely challenging. The current systems of clinical classification, though scientifically constructed and predictive of likelihood of undergoing surgery [15], are of little help regarding the choice of surgical strategy. As opposed to adolescent idiopathic scoliosis, adult deformity is frequently associated with neural entrapment, segmental instability, previous fractures, sagittal imbalance and painful disc disease. Comorbidity is the rule rather than the exception in this group of patients. Curves are frequently rigid and bone stock can be poor, compromising the stability of fixation. Surgical indication is frequently given to elderly patients who cannot always tolerate extensive surgery, and rules that take into account the extent of surgery and risks of complications versus limited surgery and risks of decompensation or imbalance have not been established. Complications are frequent during and after surgery for adult deformity, and their frequency differs depending on the age group considered. One large study [1] found a major complication and overall complication incidence of 6 and 17 % in the group 25–44 years of age, 15 and 42 % in patients 45–64 years of age and of 29 and 71 % in patients older than 65 years (again, complications are the rule rather than the exception). Older patients may need more frequently complex procedures (decompression, osteotomy and pelvic fixation). Interestingly, the same study found that at baseline, older patients had higher levels of disability and worse health status, but had improved, more than in the younger, back disability score and leg pain score. In this group there was a trend toward greater improvement in general health and back pain. After surgery, mean pain, function and health status scores were the same in younger and older patients.
More rigid and severe deformities can need a combined posterior and anterior approach or only posterior three-column reconstruction to obtain release of the deformity, correction, stability and anterior column support. Circumferential surgery has recently demonstrated to be an independent predictor of favorable outcome in adult deformity [1].
Extreme lateral interbody fusion (XLIF) [16] is a novel technique developed to provide a safe and reproducible method to obtain minimally invasive anterior spinal fusion. It has been demonstrated as safe in elderly patients, including octogenarians, and, in this age group, has compared favorably to open TLIF historical controls for complication rates, blood loss and transfusion rates, hospital stay and 6 months postoperative survival [17].
The scope of this paper is to review the literature on the use of lateral approach interbody fusion for surgical correction of adult spinal deformity, to discuss its limits and advantages and to propose a guide to the use of this novel approach in adult deformity surgery.
Methods
Surgical technique
XLIF is a minimally invasive technique that approaches the spine through a 90° lateral pathway. It is a true anterior retroperitoneal (or, in higher levels, transdiaphragmatic, retropleural or transthoracic) access to the spine from the thoracic (T5 is the upper level that can be usually approached) to L5. In the lumbar spine, the working channel passes through the psoas muscle. Important aspects of the technique [18] are a muscle splitting approach with progressive dilators to create a working channel through the psoas that uses neuromonitoring of the motor component of the lumbar plexus within the psoas, which is directional and provides real-time feedback on the position and relative distance of the nerve roots in the field, bilateral annulus release prior to implant delivery, and the availability of specific retractors and large footprint interbody cages. Such cages are designed to support the strong ring apophysis of the vertebral endplate. The lumbar plexus covers laterally the posterior part of the vertebrae and discs; its position is posterior at L1–L2 to displace progressively anteriorly toward L4–L5. Thus, the risk of encountering branches of the lumbar plexus in the lateral pathway to the spine is higher at lower levels, making necessary nerve root detection tools. Considerations on the plexus anatomy related to the lateral approach have been previously published [19–21]. Innervation of the abdominal wall related to lateral approach has also been described as an aid to prevent abdominal wall palsy after lateral approach [22]. Detailed description of the technique has been previously published [18].
Anatomical and surgical technique details on adult deformity have also been described by Mundis et al. [23].
Bilateral annulus release combined with lateral insertion of wide cages in coronally asymmetric (scoliotic) discs provides a strong corrective force to segmentally restore coronal alignment. Further coronal correction in discs surrounded by asymmetrical vertebral bodies can be achieved by the use of coronally asymmetrical cages. Transpsoas lateral interbody fusion causes minimal blood loss and allows for early patient mobilization [24, 25]. The ability of this technique to correct endplate asymmetry virtually bloodlessly and with little tissue trauma has made some surgeons to consider it as a promising technique to correct scoliosis in older patients.
Literature review
Literature review was undertaken using the National Center for Biotechnology Information (NCBI) databases PubMed/MEDLINE. Additional publications published in peer-reviewed, non indexed journals were sought using http://www.scholar.google.com. The following keywords were used: XLIF, extreme lateral interbody, direct lateral interbody, transpsoas fusion, transpsoas interbody, deformity, scoliosis, kyphosis, imbalance, balance, sagittal, coronal, adult. Additional information was gathered from the proceedings of the Society for Lateral Access Surgery (SOLAS).
Results
Effectiveness and complications of XLIF in adult deformity
Akbarnia et al. [26] (Table 1) reported on a series of 16 patients treated with XLIF plus posterior instrumentation for scoliosis of more than 30°Cobb, with a minimum 2-year follow-up. Anterior surgery corrected 45 % of the coronal deformity, and after supplemental posterior instrumentation correction reached 64 %. They found also an average 13° improvement of segmental sagittal deformity. Clinical outcome measurements improved from preoperative to final follow-up (VAS 6.5–2.5; ODI 60–24; SRS-22 2.6–3.8). Half of the patients presented postoperative anterior thigh pain (all transient). Hypo or dysesthesia was observed in 56 % and permanently in 12 %. Weakness was present in 19 %, all transient.
Table 1.
Literature data on results and complications of XLIF in adult scoliosis
| Author | Patients | Surgical technique | Results | Complications |
|---|---|---|---|---|
| Akbarnia et al. [26] | 16 patients | XLIF plus posterior instrumentation in patients with coronal Cobb angle >30° | Anterior corrected 45 % of coronal deformity After posterior surgery, 64 % correction (coronal) Average sagittal improvement 13° VAS 6.5–2.5 ODI 60–24 |
50 % postoperative anterior thigh pain (all transient) Sensory disturbances in 56 % (12 % permanent) Weakness in 12 %, all transient |
| Tormenti et al. [27] | 8 patients | Multilevel XLIF plus posterior instrumentation | 2 motor deficits (one permanent) 6 sensory deficits (5 permanent) One bowel perforation One infection causing meningitis and sepsis One pulmonary embolism One dural tear (in the posterior approach) |
|
| Dakwar et al. [28] | 25 patients | Most XLIF plus lateral plate | One-third of patients did not obtain a good sagittal alignment | One implant failure One cage subsidence Transient anterior thigh numbness in 12 % One case of rhabdomyolysis |
| Wang et al. [29] | 23 patients | XLIF plus percutaneous pedicle screws | Cobb angle corrected from 31° to 10° | Thigh dysesthesia, pain or weakness in 30 %, permanent in one patient No other complications were observed |
| Keshavarzi et al. [30] | 26 patients | Staged XLIF plus posterior instrumentation | Mean correction from 47° to 28° (coronal) after anterior surgery, then to 13° after posterior instrumentation L1–L5 lordosis from 32° to 49° after anterior surgery, then to 51° after posterior After anterior surgery, coronal decompensation that needed correction with posterior instrumentation |
Complications not included in the report |
| Phillips and Kahn [31] | 90 patients | Stand alone or bilateral posterior pedicle instrumentation | Stand alone corrected less (9.8 %) than anterior plus posterior bilateral pedicle screw instrumentation (41.5 %) Open pedicle screw instrumentation corrected more than percutaneous |
|
| Isaacs et al. [32] | 107 patients | Stand alone, XLIF plus lateral plating, XLIF plus percutaneous or open pedicle screw instrumentation | Major complications were more frequent in open posterior instrumentation (20.7 %) than in percutaneous posterior instrumentation (5.8 %) One kidney laceration No major vascular, intestinal or ureteral complications were seen Seven patients had severe or protracted motor deficit (2 of them only after posterior staged surgery) |
Tormenti et al. [27] observed two motor deficits (one permanent) and six sensory deficits (5 permanent) in a series of eight patients treated with multilevel XLIF plus posterior instrumentation. Other complications included one bowel perforation, one infection progressing to meningitis and sepsis, one pulmonary embolism and one dural tear (in the posterior approach).
Dakwar et al. [28] in a series of 25 patients, most of them instrumented with lateral plate, observed one case of implant failure and one of cage subsidence. Transient anterior thigh numbness was present in 12 %. One case presented with rhabdomyolysis. One-third of patients did not obtain a good sagittal profile.
Wang et al. [29] reported on 23 patients undergoing XLIF plus posterior percutaneous pedicle screws. Cobb angle was corrected from 31 to 10°. Thigh dysesthesia and pain or weakness was present in 30 % patients and was permanent in one. No other complications were observed.
Keshavarzi et al. [30] studied 26 patients undergoing staged anterior lateral fusion plus posterior instrumentation. Mean preoperative coronal deformity of 47° was corrected to 28° after anterior surgery and then to 13° after posterior instrumentation. L1–L5 lordosis changed from 32° to 49° after anterior surgery and to 51° after posterior stage. Interestingly, after anterior stage, patients were found to consistently increase coronal decompensation toward the convexity of the lumbar curve. Decompensation was corrected by posterior instrumentation. The authors attributed this decompensation to stiffness of the fractional lumbosacral curve (L5–S1). Pain VAS improved by nearly 4.5 points for both back and leg. Complications were not included in the report.
Phillips and Kahn [31] compared the radiographic results by the method of fixation in 90 patients. They found that stand-alone XLIF obtained less correction (9.8 %) of the coronal deformity compared to XLIF plus bilateral pedicle fixation (41.5 %). The incidence of subsidence was greater in patients with stand-alone XLIF than in those with XLIF plus bilateral pedicle screws. In patients with XLIF plus bilateral pedicle screws, those implanted with open posterior technique had better coronal correction than those implanted percutaneously.
A large series of 107 patients with a mean preoperative Cobb angle of 24° has been reported in a prospective multicenter study by Isaacs et al. [32]. The series included stand alone (19 %), lateral plating (6 %), XLIF plus percutaneous or open pedicle screw insertion (75 %) supplementary fixation (65 % of pedicle screw fixation was done percutaneously). Two-thirds of patients had recorded estimated blood loss less than 100 ml. Major complications were more frequent in patients with open pedicle screw fixation (20.7 %) than in those with only anterior or percutaneous pedicle screw fixation (5.8 %). Being a nonrandomized study, bias cannot be excluded (patients with open posterior fixation could be more complex cases). Seven patients had severe or protracted motor deficit. Two of these were observed only after a staged posterior instrumentation. Twenty-six percent of patients had hip flexor weakness that was transient in 86 % and considered an expected effect of surgical wound in the psoas muscle. A correlation was found between hip flexor weakness and length of surgery. No major vascular, ureteral or intestinal complication was observed. One kidney laceration occurred.
Some small series have reported on stand-alone lateral interbody fusion for adult scoliosis. Due to the small numbers of these series or inadequate reporting of surgical technique or outcomes, their results have not been included in this paper.
Discussion
Classification of surgical candidates and indications
Adult deformity includes a miscellaneous of clinical conditions. It includes cases that can mainly be managed as a spinal degenerative disease (as are patients with single or two-level degenerative disease or nerve root entrapment far from the apex of the curve), with little attention to the deformity, other patients with mechanical pain limited to a small number of segments included in a curve, individuals with neurological symptoms mainly caused by deformity with secondary nerve entrapment and subjects with severe curves combining different degrees of coronal imbalance, trunk shift, curve progression and laterolisthesis. Any of the latter three categories can be classified as sagittally balanced, sagittally compensating (imbalanced) and sagittally imbalanced (Table 2). Patients with sagittal imbalance should be considered a different category, as they require a distinct surgical strategy.
Table 2.
Sagittal balance status classification
| Status | Parameters of global sagittal spinal balance | Situation of compensatory mechanisms to regain sagittal balance |
|---|---|---|
| Sagittally balanced | SVA (sagittal vertical axis through center of C7 body) is within 5 cm from the posterior margin of the S1 endplate | Pelvic tilt is less than 1/3 of the pelvic incidence AND femoral shaft axis is vertical |
| Sagittally compensating | SVA (sagittal vertical axis through center of C7 body) is within 5 cm from the posterior margin of the S1 endplate | Increased pelvic tilt (pelvic tilt is less than 1/3 of pelvic incidence) OR femoral shaft axis IS NOT vertical (indicating compensatory knee flexion to increase pelvic tilt or translate center of mass) |
| Sagittally imbalanced | SVA (sagittal vertical axis through the center of the C7 body) is more than 5 cm from the posterior margin of the S1 endplate |
In this section, a new classification of adult lumbar deformity is proposed to assist in the choice of a surgical strategy for XLIF use (Table 3).
Table 3.
Criteria to classify adult scoliosis regarding type of lateral access fusion strategy
| Type of deformity | Criteria | Surgical Strategy |
|---|---|---|
| Type I: localized nerve entrapment in adult scoliosis | Spinal stenosis at 1–2 levels and Two discs remaining between the upper level to be included in decompression/fusion and the apex of the curve and No severe degeneration or instability (including laterolisthesis) in the disc over the level to be decompressed or fused and sagittally balanced |
Selective decompression or Selective decompression and fusion if instability is present or surgery will create instability |
| Type II: limited disc disease within the curve | Painful discs within the curve (i.e., Modic I changes in some of the discs, laterolisthesis at one or two discs, vacuum phenomenon in discs with severe collapse) and Mostly sagittally balanced. (Lumbar lordosis > pelvic incidence) and Coronal imbalance < 4 cm and Nonprogressive curve and Less severe curve (<30°) Ideally, painful discs around (over and below) the apex of the lumbar curve |
Selective fusion with partial correction (do not correct over adjacent curve correction in bending films to avoid decompensation) Consider anterior XLIF alone (when little or no correction is needed) or XLIF and posterior instrumentation to improve and maintain correction, to improve sagittal balance or to restore coronal balance after anterior procedure |
| Type III: severe coronal deformity | Pain all over the curve or Progressive curve or More severe curve (>30°) or Coronal deformity with moderate sagittal imbalance or sagittally compensating |
Fusion of the entire curve (as dictated by coronal and sagittal plane deformity): XLIF at all levels or at the more rigid segment plus posterior instrumentation. Eventually posterior correction of coronal imbalance if present after XLIF If discs in the extremes of the curve are preserved and mobile in lateral bending, consider XLIF at the apex (2 discs if apex is a vertebra, 3 discs if apex is a disc) with derotation of the apex through posterior instrumentation and compression in the convexity |
| Type IV: sagittal imbalance | No or minor coronal deformity Sagittally imbalanced or Sagittally compensating with severe back pain or Sagittally compensating with stenosis |
Posterior instrumentation and fusion with osteotomies as needed. Consider adding XLIF (same day or staged) to increase stiffness around PSO or in open discs after SPO In case of severe sagittal deformity with large deformity coronal, consider XLIF at all levels or a the more rigid segment and at the levels of planned posterior osteotomy (see below) plus posterior instrumentation and fusion with osteotomies as needed In selected cases requiring less than 30° of sagittal correction, consider XLIF complete release and lengthening with hyperlordotic cage, followed by posterior instrumentation (currently under evaluation) |
Surgical decompression without fusion or with fusion limited to one or two segments can be an acceptable option in Type I (Table 3) adult deformity patients, if adjacent discs are not degenerated and decompression or selective fusion are not performed at the level or adjacent to the level with strong torsional or lateral shearing forces. If these forces are present, limited surgery can result in postoperative instability at the same or adjacent level, leading in some cases to progression or decompensation of the curve and clinical impairment. Thus, patients needing decompression and/or fusion at or near the apex of the lumbar curve should rather be classified into Type II or III.
The authors have identified at least three clinical scenarios in adult deformity surgery, in which lateral access can be useful. The first scenario is represented by those patients with mechanical pain in lumbar scoliosis with pain generator limited to few discs in the curve (Type II, Table 3). These patients are well balanced in the coronal and sagittal plane, and generally their curves do not need to be significantly corrected in magnitude. Anterior only fusion can be considered, depending on bone quality, patient compliance, endplate preservation during surgery and ability to achieve good stability of the implants with integrity of the anterior longitudinal ligament.
The second scenario is that of patients with painful and progressive lumbar scoliosis, with relatively well-conserved sagittal balance (Type III, Table 3). XLIF is a powerful method to make curves more flexible, allowing for better correction, to promote fusion with a strong anterior support and large surface for graft contact and to provide modest increase of lumbar lordosis. Posterior fixation is necessary to gain better correction and to maintain it postoperatively.
Open posterior fixation is most helpful, especially associated with posterior osteotomies, to achieve large corrections in the coronal plane and to substantially increase lumbar lordosis. In selected cases, a complete anterior release during lateral access fusion can produce strong corrections in the coronal and sagittal plane with short segment, percutaneous posterior fixation. It is the belief of the authors that, under some conditions, this combined technique can save fusion levels compared to posterior procedures.
The third scenario and application of XLIF in deformity are in patients with significant sagittal imbalance (Type IV, Table 3). In these cases, our current approach is correction of the deformity by open posterior surgery, usually with lumbar PSO, complemented in some cases by SPO. Minimally invasive XLIF fusion is performed after posterior correction to increase construct stiffness, anterior column continuity and fusion area. Two different situations can present in these cases. At the levels where Smith Petersen Osteotomy has been performed, XLIF allows restoring the continuity of the anterior column, avoiding a large empty space in it and probably decreasing the risk of implant failure and loss of correction. After pedicle subtraction osteotomy, XLIF above and below the osteotomized vertebra is performed to provide bone continuity for fusion mass where posterior surgery has altered the bony anatomy, creating a discontinuity in the surface for the fusion mass.
Recently, Akbarnia et al. [33] have described a lateral access MIS technique with complete anterior release, interbody fusion with large, hyperlordotic cages that lengthen the anterior column, followed by posterior instrumentation without osteotomies. This promising technique is currently under evaluation and, if it demonstrates to be safe and effective, could be an alternative to posterior osteotomies in moderate (20°–30°) deficit of lumbar lordosis.
Lateral access fusion can provide a method for obtaining a good fusion mass with increased stability in revision surgery for PSO failure. These patients typically present with rod breakage or hardware pullout and loss of correction at the level of the osteotomy or below. A constant finding in these cases has been a loss of continuity of posterolateral graft at the level of the discs above and below the osteotomy, with pseudartrhrosis.
Case studies
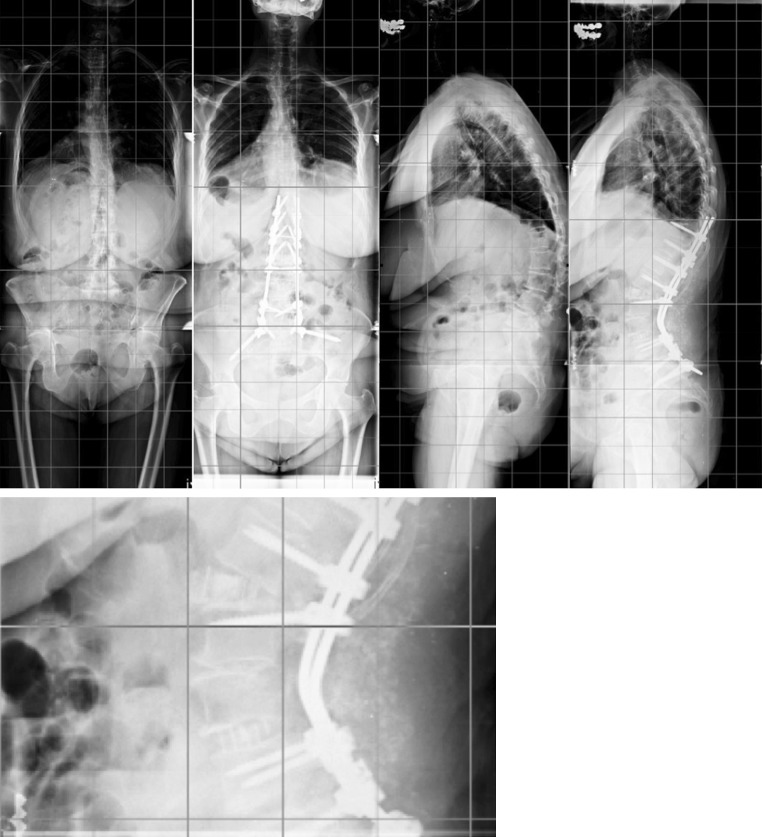
Type II deformity
A 74-year-old lady with previous L4–S1 posterolateral fusion (with peek rods) ending near the apex of the lumbar coronal curve presented 3 years after surgery with severe back pain and junctional disease (Fig. 1). Good sagittal and coronal balance was present at that time. No symptoms or signs of neural entrapment were observed. This is a case of a balanced spine with painful degenerative disease within a curve that needs no or slight correction. An only-anterior procedure was performed at three levels. Only one of the cages was additionally instrumented with lateral plate due to concerns about immediate stability. Though only slight curve correction was present at the final follow-up, the patient went on to fusion and is pain free at the 2-year follow-up. Excessive correction of the curve over a rigid lumbosacral area could have led to imbalance.
Fig. 1.
A type II deformity case. Only anterior fusion, with limited correction was the chosen strategy (see text). Preoperative bending and full standing and postoperative detail and full standing films are shown
Type III deformity
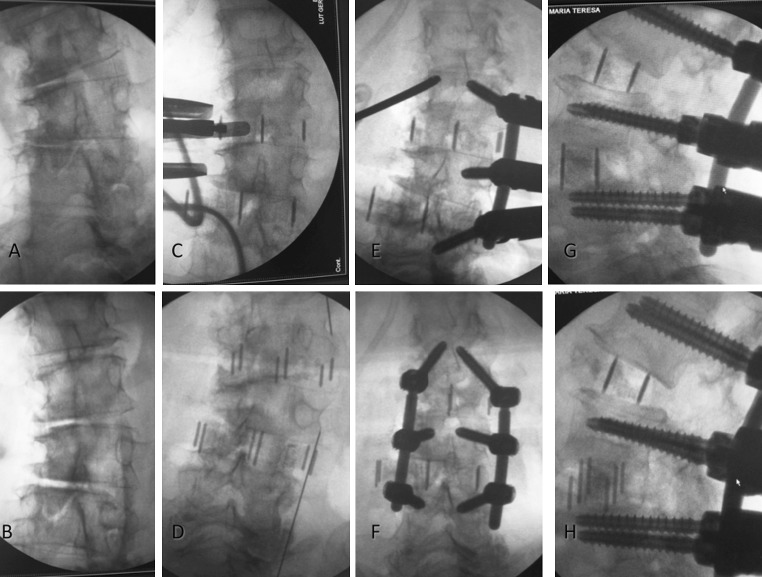
A 67-year-old patient presented with severe back pain preventing her from standing and walking except for very short distances. Figure 2a, b shows the preoperative films, with a short L1–L5 curve and severe rotation at the apical (L4) vertebra. Lumbar lordosis was partially preserved (at the L4–S1 segment). After one stage (Fig. 2c, d), two level lateral access anterior ligament release and fusion with lordotic cages and posterior percutaneous pedicle screw instrumentation (with apical derotation and posterior compression; see Fig. 3), coronal plane deformity and apical rotation were almost completely corrected at the instrumented levels; lordosis in the two instrumented levels was increased by 30°.
Fig. 2.
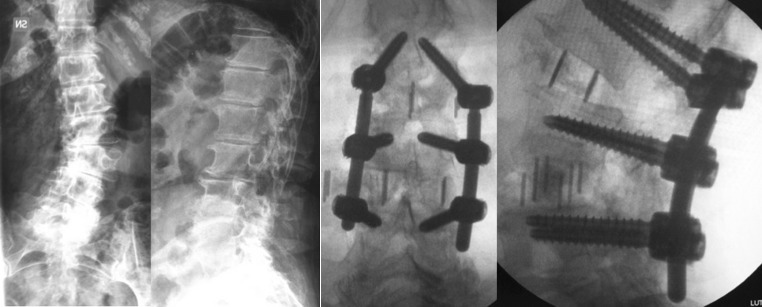
Type III de novo scoliosis. Lateral access anterior release and interbody fusion, posterior percutaneous instrumentation (with apex derotation)
Fig. 3.
The same case presented in Fig. 2. Effect of surgical steps on deformity (see text)
The effect of surgical steps on deformity is illustrated in Fig. 3. After positioning the patient in the lateral decubitus position (Fig. 3a), the apex of the coronal deformity had narrow disc spaces in the concavity (rotation was changed by patient tilt to have a true AP view on the apical vertebra). After table break, discs opened in the concave side (Fig. 3b). Annulus release and XLIF cage placement further corrected coronal deformity, and the vertebrae included in fusion were almost parallel (Fig. 3c). After positioning the patient prone, some of the corrections seen in C were lost (Fig. 3d). The rod on the convex side was placed first, the superior and inferior screws were slightly overinserted and the central screw was slightly underinserted. The nut in center screw was tightened first (Fig. 3). The concave screws were placed with slight overinsertion of the central screws (Fig. 3g). A concave rod is then inserted. Superior and inferior nuts were tightened. Simultaneous tightening of the central concave screw nut and the extreme convex screw nuts (with the use of persuaders) created a derotating force on the apex (pushing the apical vertebra in the convexity and pulling it on the concavity). Final compression (more on the convex side) loads the cages and improves lordosis (Fig. 3f, h).
Type IV deformity
In severe sagittal imbalance cases, with or without coronal deformity, sagittal plane dictates the priority of surgical strategy (managed mainly by posterior surgery). After posterior instrumentation (T11–ilium), L4 PSO (not achieving in this case enough correction) and L2–L3 Smith Petersen osteotomy (resulting in evident opening of the disc anteriorly), an anterior column discontinuity was created (Fig. 4). Lateral access for anterior fusion at L2–L3, L3–L4 (graft without cage) and L4–L5 was useful to restore the anterior column integrity. The detail shows the cages in place and the large amount of posterior graft at the level of the osteotomies to reduce risk of pseudarthrosis.
Fig. 4.
A Type IV deformity patient. Severe sagittal imbalance, in this case without coronal deformity
Technical details in deformity lateral access surgery
Using XLIF in deformity cases requires great attention to some technical details to get satisfactory results. Before surgery, it is important to discuss with the patient to create reasonable expectations. Lateral access splits muscle fibers in the psoas. This frequently leads to thigh pain and hip flexor weakness that must be distinguished from a root lesion. Patients should know that these symptoms are likely to present and that they will resolve within 2–6 weeks. Thigh paresthesia/dysesthesia is probably related to injury or stretch of the femorocutaneous nerve. Excessive retroperitoneal finger dissection during access and retractor pressure on the iliac crest is a likely factor that can increase the risk. Though this is a frequent complication, patients seldom feel unhappy about this in the long term. Root deficit is a more serious complication. Meticulous use of nerve detection (with triggered EMG) during psoas penetration and after retractor placement, attention to free running EMG during disc preparation and implanting to detect maneuvers that can damage the roots, clean surgical technique (avoiding unnecessary forceful or long retraction on the posterior part of the psoas) and a quick and efficient disc preparation and cage implantation can probably help to reduce this complication.
Patient positioning is critical. The table should be repositioned under fluoroscopy for every disc access to allow for a 90° vertical access parallel to the disc and the posterior wall of the vertebrae. This reduces the risk of canal penetration, contralateral root lesion, cage misplacement and vascular or visceral injury. Discs are usually approached from the concave side. This allows a more comfortable access, reducing the number of incisions (through a single fascial incision two or three discs can be approached in the lumbar spine). One exception is access to L4–L5. Due to the position of the iliac crest, in patients with a coronally oblique L4–L5 disc with a relatively high crest, a convex side approach to L4–L5 can be more convenient. Frequently, L4–L5 is included in the fractional lumbosacral curve; in these cases, the mid lumbar concave approach corresponds to the side of the L4–L5 convex approach. In some cases, this is not the case and a contralateral L4–L5 approach should be considered. Before surgery, the position of vessels and lumbar plexus in axial MRI/CT slices should be checked. This permits to estimate the width of the working window to each space. Depending on the axial anatomy, in some cases, one side could be considered safer for access. Retraction time in the psoas has been related to thigh weakness. An efficient disc access and preparation technique that makes possible a quick and effective disc preparation and cage placement should be mastered before considering treatment of deformity cases. Overcorrection is a real risk when XLIF is used at every level in a lumbar curve [30]. Painful discs within balanced curves near rigid compensatory curves need just fusion. In large curves, posterior staged instrumentation gives the surgeon the chance to evaluate the degree of correction and coronal decompensation, and to correct it by appropriate posterior instrumentation in a second stage. In some cases, surgery limited to few discs around the apex, followed by aggressive posterior correction, can give satisfactory results saving fusion levels (Fig. 2).
Lateral access fusion after posterior fixation (as in sagittal imbalance cases) poses some technical difficulties. Spinous processes resection and posterior instrumentation make it difficult to identify on a–p fluoroscopy the midline, and to obtain a perfect lateral position of the patient. After posterior fixation extending from the lower thoracic spine to the sacrum, table break cannot be used to open the space between the ribs and the iliac crest, so that L4–L5 can be difficult to reach without angled instruments; intercostal or transpleural access can be needed to access L3–L4 and almost constantly L2–L3 and L1–L2. Posterior fixation makes discs undistractable, and endplate penetration is the consequence of attempts to implant large cages. When PSO has been performed at a high level (L2 or L3), the apex of the lumbar lordosis translates anteriorly, making retroperitoneal dissection more difficult and the risk of bowel or kidney injury higher. A lengthy posterior procedure with significant blood loss can impair coagulation, causing more anterior bleeding (which can be a significant problem in a reduced field) and greater difficulty in obtaining adequate hemostasis.
Conclusions
XLIF is a promising minimally invasive option in the management of adult deformity. It can be used combined with standard posterior techniques to improve the amount of correction or the construct stability, or with percutaneous pedicle fixation (or in some cases with just an anterior fixation) to reduce surgical trauma and complications. Due to the mechanical properties of large cages with annulus release, specific surgical strategies are needed to avoid imbalance and define ideal fusion levels and methods. These strategies should be defined and tested. The role of XLIF plus minimally invasive posterior fixation in obtaining satisfactory curve correction while reducing the number of levels fused in lumbar scoliosis can be advantageous over more traditional techniques. An adequate evaluation of the incidence of neural and psoas complications, its avoidance and its real impact on patients’ outcomes is necessary to better understand the advantages of this approach. Studies comparing the effectiveness and safety of traditional versus XLIF approaches for adult deformity are needed to assist evidence-based decision making.
Conflict of interest
None.
References
- 1.Smith JS, Shaffrey CI, Glassman SD, Berven SH, Schwab FJ, Hamill CL, Horton WC, Ondra SL, Sansur CA, Bridwell KH. Risk–benefit assessment of surgery for adult scoliosis: an analysis based on patient age. Spine. 2011;1(36):817–824. doi: 10.1097/BRS.0b013e3181e21783. [DOI] [PubMed] [Google Scholar]
- 2.Bridwell KH, Glassman S, Horton W, Shaffrey C, Schwab F, Zebala LP, Lenke LG, Hilton JF, Shainline M, Baldus C, Wootten D. Does treatment (nonoperative and operative) improve the two-year quality of life in patients with adult symptomatic lumbar scoliosis: a prospective multicenter evidence-based medicine study. Spine. 2009;15(34):2171–2178. doi: 10.1097/BRS.0b013e3181a8fdc8. [DOI] [PubMed] [Google Scholar]
- 3.Schwab F, Patel A, Ungar B, Farcy JP, Lafage V. Adult spinal deformity-postoperative standing imbalance: how much can you tolerate? An overview of key parameters in assessing alignment and planning corrective surgery. Spine. 2010;35:2224–2231. doi: 10.1097/BRS.0b013e3181ee6bd4. [DOI] [PubMed] [Google Scholar]
- 4.Mac-Thiong JM, Transfeldt EE, Mehbod AA, Perra JH, Denis F, Garvey TA, Lonstein JE, Wu C, Dorman CW, Winter RB. Can C7 plumbline and gravity line predict health related quality of life in adult scoliosis? Spine. 2009;34:E519–E527. doi: 10.1097/BRS.0b013e3181a9c7ad. [DOI] [PubMed] [Google Scholar]
- 5.Glassman SD, Berven S, Bridwell K, Horton W, Dimar JR. Correlation of radiographic parameters and clinical symptoms in adult scoliosis. Spine. 2005;30:682–688. doi: 10.1097/01.brs.0000155425.04536.f7. [DOI] [PubMed] [Google Scholar]
- 6.Mac-Thiong JM, Roussouly P, Berthonnaud E, Guigui P. Sagittal parameters of global spinal balance: normative values from a prospective cohort of seven hundred nine Caucasian asymptomatic adults. Spine. 2010;35:E1193–E1198. doi: 10.1097/BRS.0b013e3181e50808. [DOI] [PubMed] [Google Scholar]
- 7.Boulay C, Tardieu C, Hecquet J, Benaim C, Mouilleseaux B, Marty C, Prat-Pradal D, Legaye J, Duval-Beaupère G, Pélissier J. Sagittal alignment of spine and pelvis regulated by pelvic incidence: standard values and prediction of lordosis. Eur Spine J. 2006;15:415–422. doi: 10.1007/s00586-005-0984-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schwab F, Lafage V, Patel A, Farcy JP. Sagittal plane considerations and the pelvis in the adult patient. Spine. 2009;34:1828–1833. doi: 10.1097/BRS.0b013e3181a13c08. [DOI] [PubMed] [Google Scholar]
- 9.Roussouly P, Nnadi C. Sagittal plane deformity: an overview of interpretation and management. Eur Spine J. 2010;19:1824–1836. doi: 10.1007/s00586-010-1476-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Neal CJ, McClendon J, Halpin R, Acosta FL, Koski T, Ondra SL. Predicting ideal spinopelvic balance in adult spinal deformity. J Neurosurg Spine. 2011;15:82–91. doi: 10.3171/2011.2.SPINE1018. [DOI] [PubMed] [Google Scholar]
- 11.Yang BP, Ondra SL. A method for calculating the exact angle required during pedicle subtraction osteotomy for fixed sagittal deformity: comparison with the trigonometric method. Neurosurgery. 2006;59:ONS458–ONS463. doi: 10.1227/01.NEU.0000232628.46247.15. [DOI] [PubMed] [Google Scholar]
- 12.Aurouer N, Obeid I, Gille O, Pointillart V, Vital JM. Computerized preoperative planning for correction of sagittal deformity of the spine. Surg Radiol Anat. 2009;31:781–792. doi: 10.1007/s00276-009-0524-9. [DOI] [PubMed] [Google Scholar]
- 13.Le Huec JC, Leijssen P, Duarte M, Aunoble S. Thoracolumbar imbalance analysis for osteotomy planification using a new method: FBI technique. Eur Spine J. 2011;20:669–680. doi: 10.1007/s00586-011-1935-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lamartina C, Berjano P, Petruzzi M, Sinigaglia A, Casero G, Cecchinato R, Damilano M, Bassani R. Criteria to restore the sagittal balance in deformity and degenerative spondylolisthesis. Eur Spine J. 2012;21:S27–S31. doi: 10.1007/s00586-012-2236-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schwab F, Farcy JP, Bridwell K, et al. A clinical impact classification of scoliosis in the adult. Spine. 2005;30:1670–1673. doi: 10.1097/01.brs.0000170293.81234.f0. [DOI] [PubMed] [Google Scholar]
- 16.Ozgur BM, Aryan HE, Pimenta L, Taylor WR. Extreme lateral interbody fusion (XLIF): a novel surgical technique for anterior lumbar interbody fusion. Spine J. 2006;6:435–443. doi: 10.1016/j.spinee.2005.08.012. [DOI] [PubMed] [Google Scholar]
- 17.Rodgers WB, Gerber EJ, Rodgers JA. Lumbar fusion in octogenarians: the promise of minimally invasive surgery. Spine. 2010;35:S355–S360. doi: 10.1097/BRS.0b013e3182023796. [DOI] [PubMed] [Google Scholar]
- 18.Berjano P, Lamartina C. Minimally invasive lateral transpsoas approach with advanced neurophysiologic monitoring for lumbar interbody fusion. Eur Spine J. 2011;20(9):1584–1586. doi: 10.1007/s00586-011-1997-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Benglis DM, Vanni S, Levi AD. An anatomical study of the lumbosacral plexus as related to the minimally invasive transpsoas approach to the lumbar spine. J Neurosurg Spine. 2009;10:139–144. doi: 10.3171/2008.10.SPI08479. [DOI] [PubMed] [Google Scholar]
- 20.Moro T, Kikuchi S, Konno S, et al. An anatomic study of the lumbar plexus with respect to retroperitoneal endoscopic surgery. Spine. 2003;28:23–28. doi: 10.1097/01.BRS.0000049226.87064.3B. [DOI] [PubMed] [Google Scholar]
- 21.Park DK, Lee MJ, Lin EL, et al. The relationship of intrapsoas nerves during a transpsoas approach to the lumbar spine: an anatomic study. J Spinal Disord Tech. 2010;23:223–228. doi: 10.1097/BSD.0b013e3181a9d540. [DOI] [PubMed] [Google Scholar]
- 22.Fahim DK, Kim SD, Cho D, Lee S, Kim DH. Avoiding abdominal flank bulge after anterolateral approaches to the thoracolumbar spine: cadaveric study and electrophysiological investigation. J Neurosurg Spine. 2011;15:532–540. doi: 10.3171/2011.7.SPINE10887. [DOI] [PubMed] [Google Scholar]
- 23.Mundis G, Akbarnia BA, Phillips FM. Adult deformity correction though minimally invasive lateral approach techniques. Spine. 2010;35:S312–S321. doi: 10.1097/BRS.0b013e318202495f. [DOI] [PubMed] [Google Scholar]
- 24.Dakwar E, Cardona RF, Smith DA, Uribe JS. Early outcomes and safety of the minimally invasive, lateral retroperitoneal transpsoas approach for adult degenerative scoliosis. Neurosurg Focus. 2010;28:E8. doi: 10.3171/2010.1.FOCUS09282. [DOI] [PubMed] [Google Scholar]
- 25.Rodgers WB, Cox C, Gerber E. Minimally invasive treatment (XLIF) or adjacent segment disease after prior lumbar fusions. Internet J Minim Invasive Spinal Technol. 2009;3:4. [Google Scholar]
- 26.Akbarnia BA, Mundis G, Bagheri R, Kabirian N, Salari P, Pawelek J (2011) Lateral approach for interbody fusion (LIF) is a safe and effective technique to reconstruct the anterior spinal column in complex adult spinal deformity: a minimum 2-year follow-up study. In: Proceedings of the 4th annual SOLAS (Society of Lateral Access Surgery) research meeting, 31 March–2 April, 2011, San Diego, CA
- 27.Tormenti MJ, Maserati MB, Bonfield CM, et al. Complications and radiographic correction in adult scoliosis following combined transpsoas extreme lateral interbody fusion and posterior pedicle screw instrumentation. Neurosurg Focus. 2010;28:E7. doi: 10.3171/2010.1.FOCUS09263. [DOI] [PubMed] [Google Scholar]
- 28.Dakwar E, Cardona RF, Smith DA, Uribe JS. Early outcomes and safety of the minimally invasive, lateral retroperitoneal transpsoas approach for adult degenerative scoliosis. Neurosurg Focus. 2010;28:E8. doi: 10.3171/2010.1.FOCUS09282. [DOI] [PubMed] [Google Scholar]
- 29.Wang MY, Mummaneni PV. Minimally invasive surgery for thoracolumbar spinal deformity: initial clinical experience with clinical and radiographic outcomes. Neurosurg Focus. 2010;28:E9. doi: 10.3171/2010.1.FOCUS09286. [DOI] [PubMed] [Google Scholar]
- 30.Keshavarzi S, Mundis G, Pekmezci M, Akbarnia BA, Weber M, Ames C, Deviren V (2011) The utility and limitations of XLIF in adult scoliosis. In: Proceedings of the 4th annual SOLAS (Society of Lateral Access Surgery) research meeting, 31 March–2 April, 2011, San Diego, CA
- 31.Phillips F, Kahn S (2011) Immediate radiographic correction achievable in adult degenerative scoliosis treated by XLIF: influence of choice of fixation. In: Proceedings of the 4th annual SOLAS (Society of Lateral Access Surgery) research meeting, 31 March–April 2, San Diego, CA
- 32.Isaacs RE, Hyde J, Goodrich A, Rodgers WB, Phillips FM. A prospective, nonrandomized, multicenter evaluation of extreme lateral interbody fusion for the treatment of adult degenerative scoliosis. Spine. 2010;35:S322–S330. doi: 10.1097/BRS.0b013e3182022e04. [DOI] [PubMed] [Google Scholar]
- 33.Akbarnia BA, Mundis G, Moazzaz P, Kabirian N, Eastlack R, Pawelek J (2011) Can less invasive lateral interbody fusion with transpsoas all release (LIFTAR) replace three-column osteotomy for correction of adult focal sagittal plane deformity? In: Proceedings of the 4th annual SOLAS (Society of Lateral Access Surgery) research meeting, San Diego, CA