Abstract
Hematopoietic stem cell gene therapy for neurological disorders relies on transmigration of donor-derived monocytes to the brain, where they can engraft as microglia and deliver therapeutic proteins. Many mouse studies use whole-body irradiation to investigate brain transmigration pathways, but chemotherapy is generally used clinically. The current evidence for transmigration to the brain after chemotherapy is conflicting. We compared hematopoietic donor cell brain engraftment after bone marrow (BM) transplants in busulfan- or irradiation-conditioned mice. Significantly more donor-derived microglial cells engrafted posttransplant in busulfan-conditioned brain compared with the irradiated, in both the short and long term. Although total Iba-1+ microglial content was increased in irradiated brain in the short term, it was similar between groups over long-term engraftment. MCP-1, a key regulator of monocyte transmigration, showed long-term elevation in busulfan-conditioned brain, whereas irradiated brains showed long-term elevation of the proinflammatory chemokine interleukin 1α (IL-1α), with increased in situ proliferation of resident microglia, and significant increases in the relative number of amoeboid activated microglia in the brain. This has implications for the choice of conditioning regimen to promote hematopoietic cell brain engraftment and the relevance of irradiation in mouse models of transplantation.
Introduction
After bone marrow transplantation (BMT), donor cells are able to repopulate the hematopoietic system and transmigrate to tissues where they differentiate into macrophages,1 or microglial cells in the brain.2,3,4 Transmigration across the blood–brain barrier (BBB) is tightly regulated and involves stimulation of MCP-1 (CCL2), the key driver of homing and engraftment to the brain.5,6
In parabiosis experiments, where the circulatory systems of two mice are connected, no transmigration to adult brain was observed under normal conditions.2 Even after irradiation of the parabiotic recipient, no cells were found to transmigrate across the BBB compared with the fully irradiated mice receiving BMT.2 After irradiation with brain protection, no brain engraftment was observed after transplant,3 which may be attributed to low chimerism because the lymph nodes are also protected.7,8 Overall, the literature suggests that brain irradiation, followed by delivery of a surplus of BM cells, is necessary for transmigration to occur.3,9 Irradiation has been shown to stimulate in situ proliferation of microglia,2 disrupt the BBB,10,11 and upregulate cytokines12,13 that may facilitate trafficking across the BBB.
This transmigration pathway has been exploited to deliver gene-modified hematopoietic stem cells to mouse models of severe neuropathic lysosomal storage disorders with promising results.14,15,16 Many mouse studies use whole-body irradiation for myeloablation; however, chemotherapy with drugs such as busulfan, are used clinically. Irradiation and busulfan differ in the way they influence hematopoietic function; ionizing radiation has an apoptotic effect, resulting primarily from misrepair of double stranded DNA breaks; whereas, busulfan, an alkylating agent that cross-links DNA and also DNA and proteins, acts principally via an alternative pathway promoting senescence.17,18 It is thought that busulfan induces senescence via a p53 independent pathway, the extracellular signal-regulated kinase (Erk) and p38 mitogen-activated protein kinase (MAPK) pathways, in slowly proliferating and nonproliferating cells, but it can also induce apoptosis in tumor cells.18 As little is known about how busulfan affects brain engraftment, we hypothesize that these effects may influence monocyte transmigration after BMT.
Two other groups have compared brain engraftment after irradiation or busulfan conditioning with conflicting results. Lampron et al. observed no transmigration to busulfan-conditioned brain, which could be caused by the nonmyeloablative dose of busulfan (80 mg/kg) used;19 whereas, recent work by Capotondo et al. demonstrated brain engraftment after busulfan conditioning, which was increased compared with the irradiation in two out of five timepoints.20 However, Capotondo et al. used a mixture of wild type (WT) and metachromatic leukodystrophy mice as recipients despite showing significant genotype differences in brain engraftment.20 Furthermore, engrafted microglia were quantified using flow cytometric analysis of CD11b and CD45 surface markers, which are also expressed on monocytes and neutrophils, thus confounding the specific identification of microglia in the brain.
To unravel these inconsistencies, we compared donor cell engraftment in the brains of WT mice after syngeneic BMT using fully myeloablative whole body irradiation or busulfan conditioning with quantitative immunohistochemistry, which allows us to identify and accurately enumerate donor microglia by both cell morphology and specific microglial markers. We found that busulfan significantly increased donor cell migration and engraftment in the brain both in the short and long term; whereas, irradiation increased long-term activation of both donor-derived and resident microglia and preferentially stimulated proliferation of resident microglia. Both busulfan and irradiation stimulated neuroinflammation but act via different pathways: busulfan stimulates long-term MCP-1 production that drives transmigration, and irradiation produces an activated, interleukin 1α (IL-1α) inflammatory environment.
Results
Busulfan conditioning significantly increases short- and long-term donor cell brain engraftment compared with the irradiation after BMT
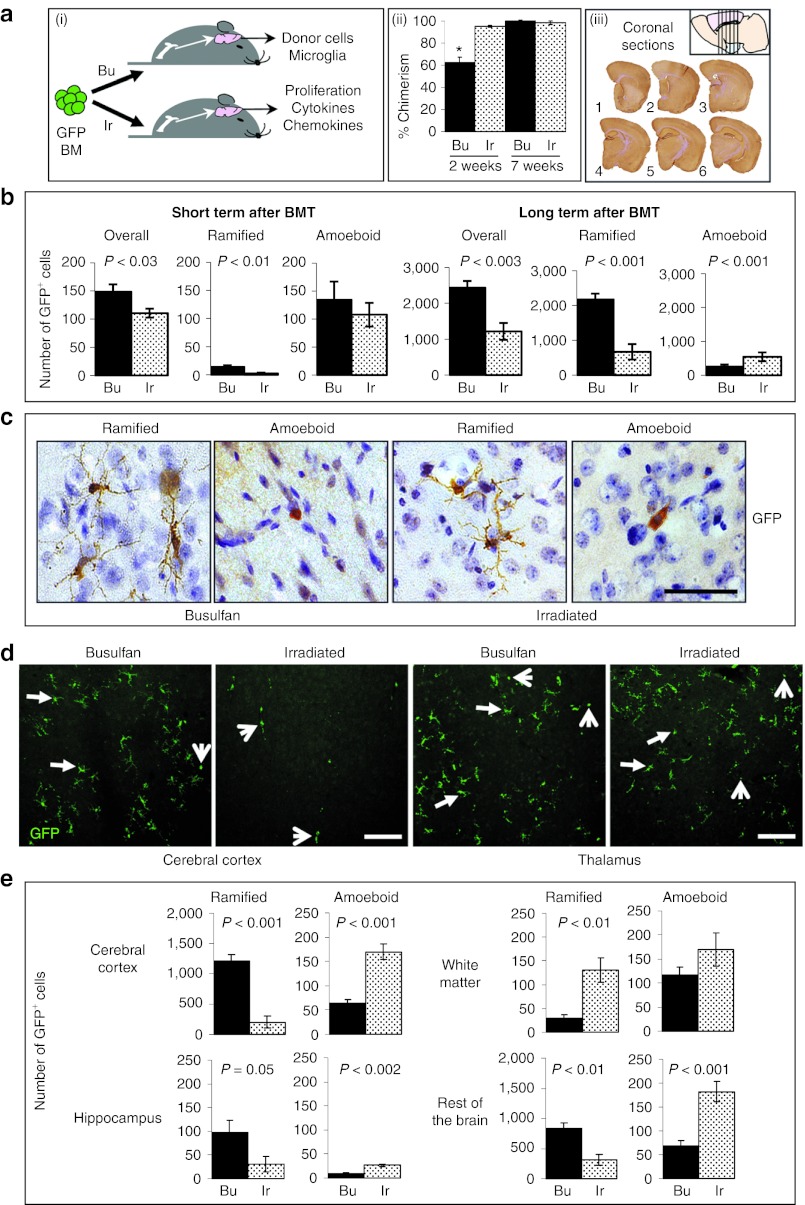
Mice were fully myeloablated with either busulfan (see Supplementary Figure S1 for myeloablative dose selection) or whole-body irradiation and transplanted with enhanced green fluorescent protein (GFP+) BM (Figure 1a; (i)). Donor blood chimerism was significantly lower in busulfan-conditioned recipients (62%) compared with the irradiated (95%; P < 0.0001) 2 weeks after BMT, with full chimerism (>98%) achieved in both transplant groups by 7 weeks (Figure 1a; (ii)).
Figure 1.
Quantification of total, resting, and activated donor-derived microglia in the brains of busulfan- and irradiation-conditioned transplant recipients. (a) (i) GFP+ bone marrow (BM) was delivered via the tail vein into mice that had undergone full myeloablative conditioning, using either busulfan (Bu) or irradiation (Ir), to investigate the level of brain engraftment after BMT. (ii) Peripheral blood donor cell chimerism (GFP) was significantly lower in busulfan-conditioned recipients compared with the irradiated (*P < 0.0001) 2 weeks after BMT with full chimerism reached in both groups by 7 weeks (n = 6/group). (iii) 6 to 9 months after BMT, the number of GFP+ cells were counted from six coronal sections of brain taken from Bregma 0.98, 0.26, −0.46, −1.18, −1.94, and −2.62 mm (1 to 6; n = 6 mice/group). (b) GFP+ cells (brown; nuclei stained blue) were counted according to their morphology; (c) ramified or amoeboid (bar = 50 µm) in both the short (2 weeks) and long term (6–9 months) after BMT. The overall number of GFP+ cells and number of ramified donor-derived GFP+ cells in busulfan-conditioned brain was significantly higher than irradiated brain at both timepoints (P < 0.03). Irradiated brain contained significantly more activated amoeboid GFP+ donor-derived cells long term after BMT (P < 0.001). (d) Distribution of GFP+ cells (green) in the primary motor, somatosensory and parietal areas of the cerebral cortex and the submedial and ventromedial thalamic nucleus of irradiated and busulfan-conditioned brains taken from the same area of Bregma (−0.46 mm) were visualized using confocal microscopy (bar = 100 µm). Arrows show ramified cells and arrow heads show amoeboid GFP+ cells. Ramified GFP+ cells were more likely to be detected in the submedial and ventromedial thalamic nucleus. (e) Significantly more ramified GFP+ cells were detected in all regions of busulfan-conditioned brain (cerebral cortex, hippocampus, and the rest of the brain; P = 0.05) except in the white matter, long term after BMT. By contrast, significantly more amoeboid GFP+ cells were detected in all regions of irradiated brain (P < 0.001) except in the white matter. Error bars represent the SEM and P values are from Student's t-test (b and e) or one-way analysis of variance with Tukey's multicomparison test (a (ii)). BMT, bone marrow transplantation; GFP, green fluorescent protein.
Brain engraftment was measured by counting GFP+ cells in perfused brains at 2 weeks (short term) and 6–9 months after BMT (long term) (Figure 1a; (iii)). No significant differences were detected in GFP brain engraftment between 6 and 9 months; therefore, the data for these timepoints were combined. GFP+ cells were also counted according to morphology (ramified or amoeboid; Figure 1b–d), to distinguish between surveillant or activated cells respectively,21,22 and by brain location (Figure 1d,e). Significantly more GFP+ cells were observed in busulfan-conditioned brain compared with the irradiated in both the short (P < 0.03) and long term (P < 0.003) after BMT, where engraftment in busulfan-conditioned brain in the long term was double that observed in irradiated. This suggests increased transmigration of donor cells.
Furthermore, busulfan-conditioned brain contained more ramified GFP+ cells (P < 0.01) at both timepoints and in all areas of the brain over the long term (P = 0.05), except in the white matter, whereas irradiated brain contained more amoeboid GFP+ cells overall (P < 0.001) and in all areas of the brain except the white matter (P < 0.001; Figure 1b,d,e) in the long term after BMT, indicating prolonged activation of donor cells. Due to the structure of the white matter tracts, it was more difficult to distinguish between ramified and amoeboid cells and could explain why no significant differences were detected. In irradiated brain, ramified GFP+ cells were more likely to be detected in the submedial and ventromedial thalamic nucleus (Figure 1d) which may be due to its close proximity to the dorsal third ventricle, providing a potential route of entry to the brain. Overall, fewer GFP+ donor cells were detected in the short term after BMT compared with the long term, and more amoeboid GFP+ donor cells were detected in the short term after BMT in both busulfan and irradiated groups suggesting that transmigration of donor cells is incomplete at 2 weeks after BMT.
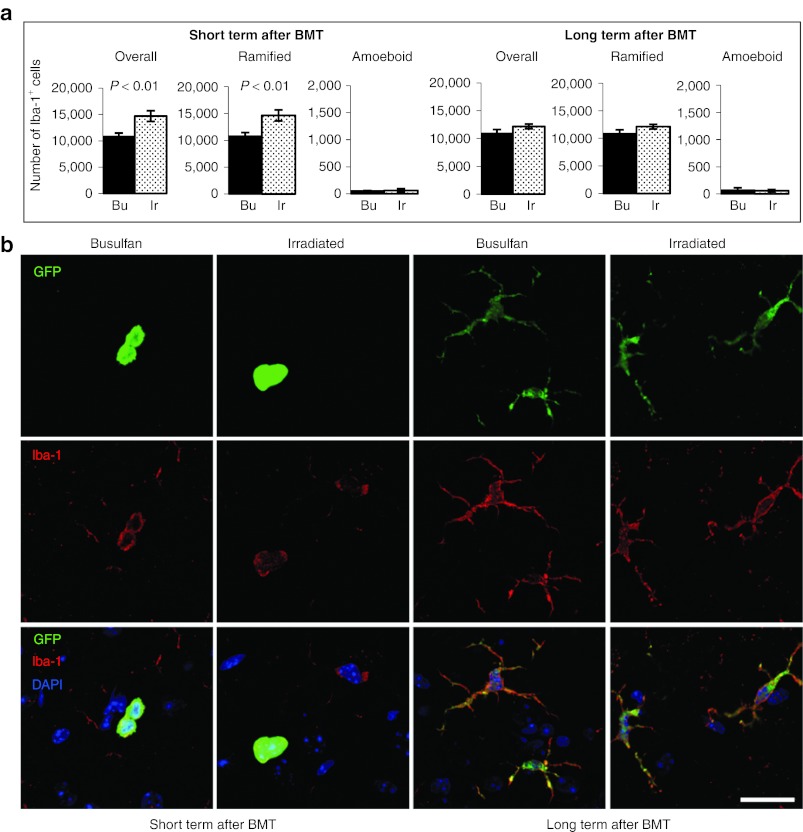
Irradiation significantly increases the total number of microglial cells compared with the busulfan conditioning in the short term
To determine the level of microglial turnover in the niche, the number of resting and activated Iba-1+ microglia23 was counted in a set of adjacent sections (Figure 2a). The number of Iba-1+ cells was much greater than GFP+ cells, implying that full repopulation of the niche by incoming donor cells does not occur under these conditions. A significant increase in the overall number, and number of ramified Iba-1+ cells, was detected in irradiated compared with the busulfan-conditioned brain in the short term (P < 0.01; Figure 2a). However, this short-term increase in irradiated brains dropped to a similar level to busulfan-conditioned brain in the long term, with no significant differences detected between groups (Figure 2a), suggesting that homeostasis is re-established. GFP+ cells in both transplant groups were also Iba-1+ at both timepoints demonstrating that the incoming cells had differentiated into microglia (Figure 2b).
Figure 2.
Quantification of total, resting, and activated Iba-1+ microglia in the brains of busulfan- and irradiation-conditioned transplant recipients. (a) The number of Iba-1+ cells were counted in the adjacent set of six brain sections, also according to their morphology, either ramified or amoeboid (n = 6/group). A significant difference in the overall number and number of ramified Iba-1+ cells was detected in the brains of irradiated (Ir) recipients in the short-term period after BMT (P < 0.01) compared with the busulfan-conditioned (Bu) recipients. No significant differences in Iba-1+ cells were detected in recipients long term after BMT. (b) Colocalization of GFP (green) and Iba-1 (red; nuclei, blue) in recipients in both the short and long term after BMT at high magnification (bar = 20 µm) visualized using confocal microscopy. Error bars represent the SEM and P values are from Student's t-test. BMT, bone marrow transplantation; GFP, green fluorescent protein.
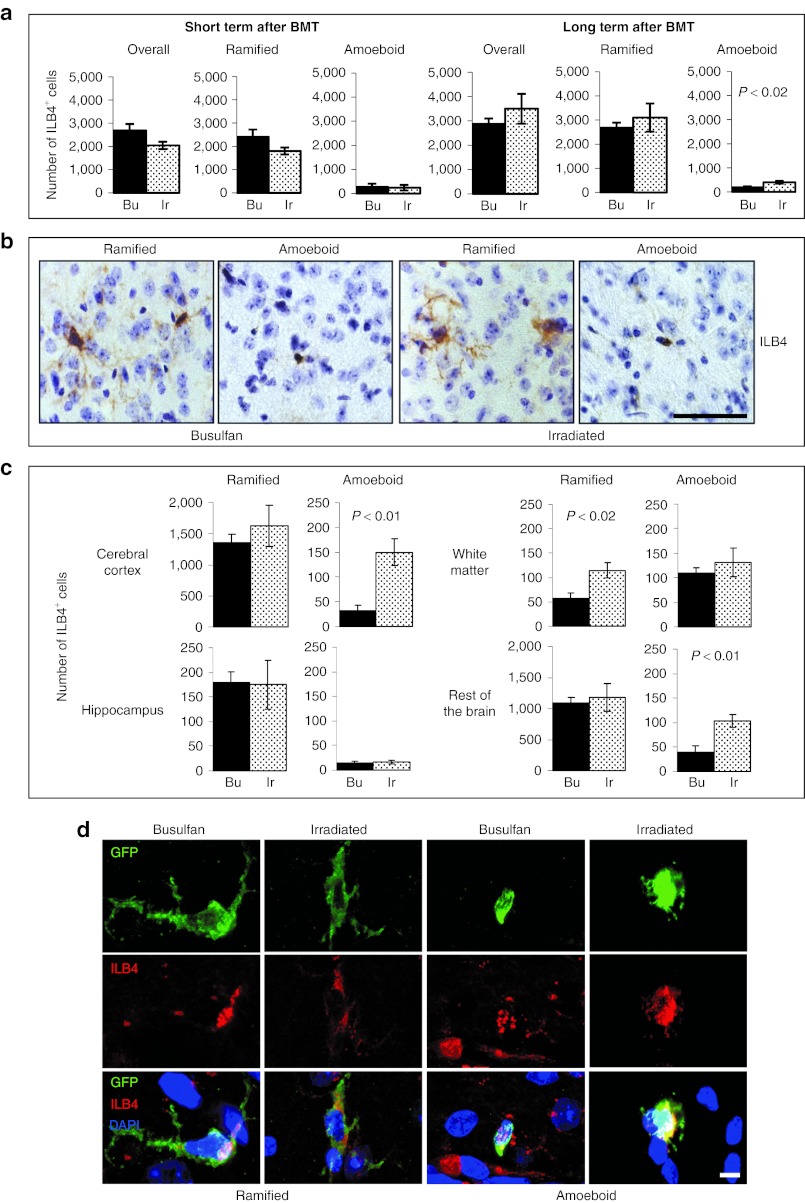
Brain microglia exhibit a more activated phenotype in irradiated than busulfan-conditioned mice in the long term after transplant
To measure the level of activated microglia in BMT recipient brain, we counted the number of ILB4+ cells24 in the adjacent set of GFP stained sections (Figure 3a–c). No significant differences in ILB4+ cell numbers were detected at either timepoint, except that more amoeboid microglia were detected in irradiated brain in the long term after BMT (P < 0.02; Figure 3a). In the long term after BMT, more ramified ILB4+ cells were detected in the white matter tracts of irradiated brains (P < 0.02; Figure 3c) and no difference was detected in amoeboid cell number, but again, it was difficult to distinguish between phenotypes in this area. GFP and ILB4 colocalized in both ramified and amoeboid microglia (Figure 3d) showing that the incoming cells are activated at least to some degree.
Figure 3.
Quantification of activated ILB4+ microglia in the brains of busulfan- and irradiation-conditioned transplant recipients. (a) The number of ILB4+ cells (brown; nuclei, blue) were counted in the adjacent set of 6 brain sections to the GFP stained sections, also according to their morphology, either ramified or amoeboid (b; bar = 50 µm; n = 6 mice/group). No significant differences in the overall number and number of ramified ILB4+ cells were detected in the brains of irradiated (Ir) and busulfan-conditioned (Bu) recipients at either timepoint. Irradiated recipients contained significantly more amoeboid ILB4+ cells compared with the busulfan-conditioned recipients (P < 0.02) in the long-term period after BMT. (c) No significant differences were detected in the number of ramified ILB4+ cells in different regions of the brain in transplant recipients in the long-term period after BMT, except in the white matter where significantly more were detected in irradiated brain (P < 0.02). The number of amoeboid ILB4+ cells was significantly higher in all regions (P < 0.01) of irradiated brain except the white matter and hippocampus in the long term after BMT (n = 6 mice/group). (d) Colocalization of GFP (green) and ILB4 (red; nuclei, blue) in transplant recipients at high magnification (bar = 5 µm) visualized using confocal microscopy. Error bars represent the SEM and P values are from Student's t-test. BMT, bone marrow transplantation; GFP, green fluorescent protein.
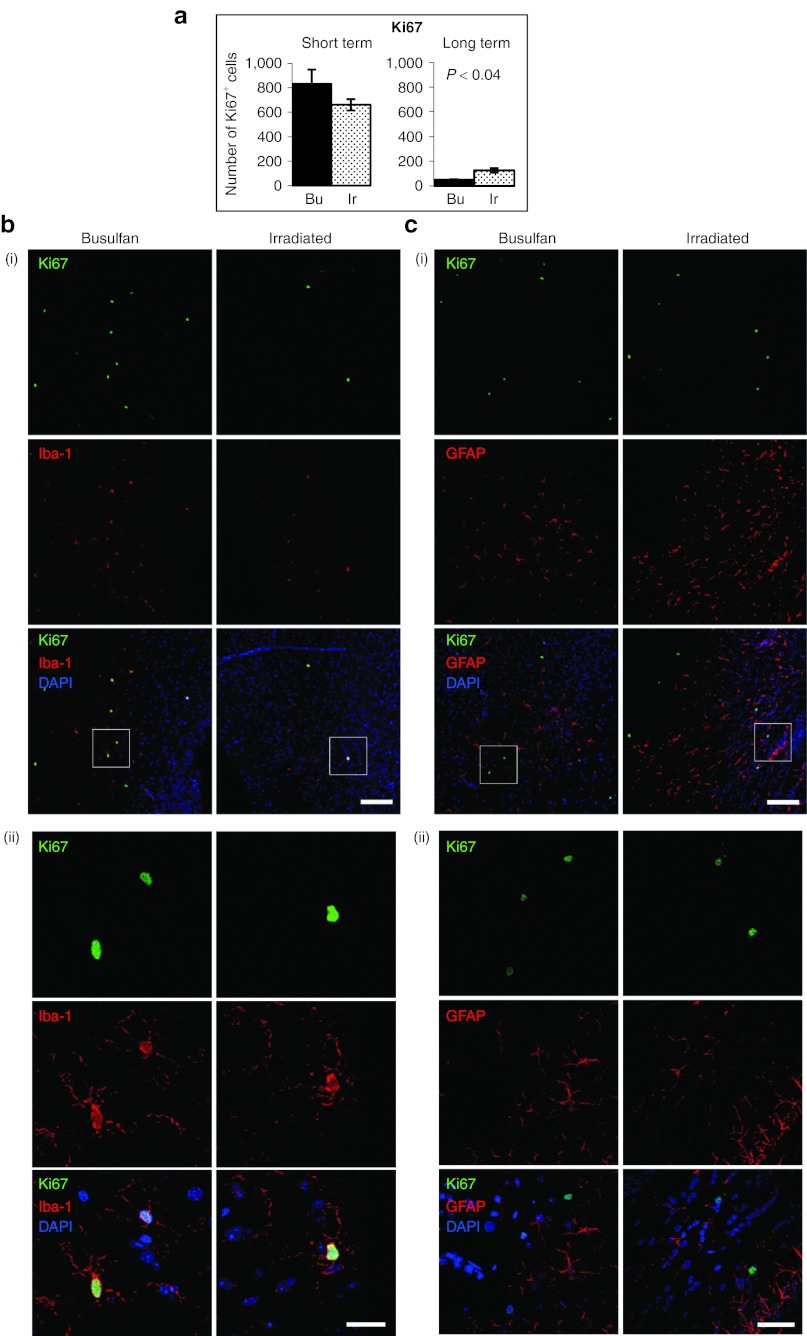
Long-term proliferation of microglia is increased in irradiated brains compared with the busulfan-conditioned brain
The observed increase in the number of Iba-1+ microglia in irradiated compared with the busulfan-conditioned brain in the short term after BMT indicates that there may be a relative increase in proliferation. We therefore compared the level of proliferation by counting parenchymal Ki67+ cells in the brain. Ki67+ cells were significantly increased over baseline (P < 0.01; data not shown) in the short term after BMT in both groups with no significant difference detected between transplant groups (Figure 4a). In the long term after BMT, Ki67+ cell numbers reduced, but irradiated brains retained significantly more Ki67+ cells than busulfan-conditioned brain (P < 0.04; Figure 4a). Ki67+ cells were characterized as Iba-1+/GFAP− (Figure 4b,c) and were predominantly GFP− demonstrating that the proliferating cells are not astrocytes but are mainly resident microglia.
Figure 4.
Quantification of numbers of proliferating Ki67+ cells in the brains of busulfan- and irradiation-conditioned transplant recipients. (a) To examine the level of proliferation after BMT, Ki67+ cells were counted in brain sections taken from Bregma 0.26, −0.46, −1.18, and −1.94 mm (2 to 5; Figure 1a; (iii)) both in the short (n = 4/group) and long term after BMT (n = 3–4/group; one value was excluded as it was >10 SDs outside of the mean). Proliferation was significantly higher in irradiated (Ir) brain in the long-term group compared with the busulfan-conditioned (Bu) brain. (b) (i and ii) Ki67+ proliferating cells were identified as Iba-1+ and (c) (i and ii) GFAP− using colocalization immunohistochemistry. Brain sections were visualized using confocal microscopy at low (b (i) and c (i); bar = 100 µm) and higher power (b (ii) bar = 20 µm and c (ii) bar = 40 µm). The boxed areas in b (i) and c (i) are magnified in b (ii) and c (ii) respectively. Error bars represent the SEM and P values are from Student's t-test. BMT, bone marrow transplantation.
Busulfan exerts a MCP-1-driven promigratory effect whereas irradiation stimulates an IL-1α-driven neuroinflammatory environment
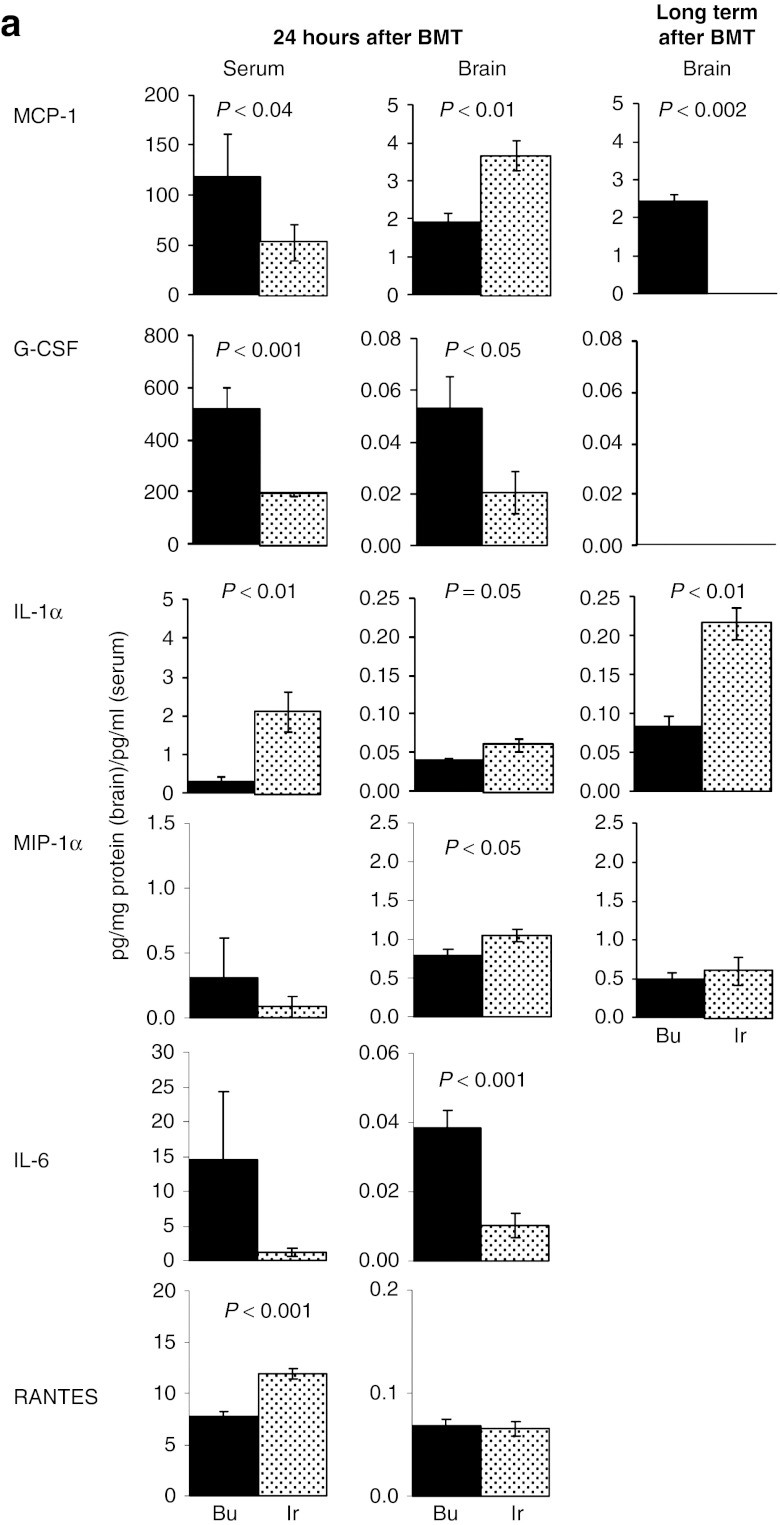
To investigate the mechanisms behind transmigration and activation of microglia, a panel of cytokines and chemokines were analyzed (Figure 5a). MCP-1, MIP-1α and IL-1α were upregulated in busulfan-conditioned and irradiated brain compared with the WT controls (P < 0.04; data not shown). MCP-1 was elevated in serum and brain of both groups at 24 hours, remaining elevated in busulfan-conditioned brain (P < 0.002) long term after BMT. G-CSF was elevated over irradiated groups in busulfan-conditioned serum (P < 0.001) and brain (P < 0.05) after 24 hours but was not detectable in either group over the long term.
Figure 5.
Quantification of chemokine/cytokines in the brains of busulfan- and irradiation-conditioned transplant recipients. Cytometric Bead Array analysis demonstrated upregulation of MCP-1, MIP-1α, and IL-1α in busulfan-conditioned (Bu) and irradiated (Ir) brain compared with the wild-type controls (P < 0.04; data not shown). 24 hours posttreatment, MCP-1 was significantly elevated in the serum of busulfan-conditioned recipients (P < 0.04) and in irradiated brain (P < 0.01); G-CSF was significantly elevated in busulfan-conditioned serum and brain (P < 0.05); IL-1α was significantly elevated in irradiated serum and brain and MIP-1α was significantly elevated in irradiated brain (P < 0.05; n = 7–8/group). At 6–9 months (long term), MCP-1 was significantly increased in busulfan-conditioned brain compared with the irradiated (P < 0.002) and IL-1α was significantly higher in irradiated brain (P < 0.01; n = 2–4/group). Cytometric Bead Array analysis demonstrated upregulation of IL-6 in busulfan-conditioned brain (P < 0.001) and RANTES and irradiated serum (P < 0.001). KC, IL-1β, IL-9, IL-13, IFN-γ, and GM-CSF were below the level of detection at both timepoints. Error bars represent the SEM and P values are from Student's t-test.
In contrast, IL-1α was significantly increased in serum (P < 0.01) and brain (P = 0.05) 24 hours after BMT, and brain in the long term after BMT (P < 0.01) of irradiated compared with the busulfan-conditioned recipients. MIP-1α was elevated in irradiated brain (P < 0.05) and RANTES was increased in irradiated serum (P < 0.001) 24 hours after BMT with IL-6 elevated in busulfan-conditioned brain (P < 0.001; Figure 5a).
Discussion
This is the first clear demonstration that transmigration and hematopoietic donor-derived brain engraftment of microglia is increased in busulfan-conditioned transplant recipients compared with the irradiated recipients in both the short and long-term period after BMT.
Busulfan-conditioned mice were slower to reach full blood chimerism compared with the irradiated recipients. Previous work has shown that irradiation exerts an apoptotic effect on hematopoietic cells; whereas, busulfan suppresses cells by inducing senescence, allowing donor cells a selective advantage.17 This could explain the differences in chimerism at 2 weeks after BMT, with full chimerism achieved in both groups by 7 weeks. In addition, the use of busulfan in the absence of an immune suppressant may result in the retention of T cells, unlike irradiation where they are ablated, and may contribute to this difference in repopulation kinetics 2 weeks after transplant. We have shown that the percentage contribution of T cells in peripheral blood 2 weeks after transplant was much lower in irradiated recipients compared with the busulfan but after 4 weeks, T cell levels were equivalent and were maintained over time (Supplementary Figure S2). Furthermore, it has been shown that the immune function recovers more quickly in busulfan-conditioned mice compared with the irradiated.25,26
Significantly increased donor-derived GFP+ cell engraftment was detected in busulfan-conditioned brain compared with the irradiated at both timepoints and was double that observed in irradiated mice in the long term after BMT. Almost all GFP+ cells detected were also Iba-1+, suggesting that engrafting donor cells at least share some characteristics of resident microglial cells. MCP-1 is a key mediator of transmigration to the brain5,6 and was increased in both busulfan and irradiated brain. Although irradiated brain contained higher levels of MCP-1 compared with the busulfan-conditioned brain initially, the levels were maintained and were significantly higher in busulfan-conditioned brain in the long term, suggesting that busulfan continues to exert a long-term transmigratory effect. Furthermore, G-CSF, implicated in proliferation and mobilization of hematopoietic cells,27 may also contribute to enhanced brain engraftment after busulfan conditioning.
These data conflict with the observations made by Lampron et al., where no brain engraftment was observed in busulfan-conditioned mice after transplant.19 This difference may be due to the lower dose of busulfan conditioning used; 80 mg/kg compared with a fully myeloablative dose of 125 mg/kg28 used in our study. We were able to confirm that 125 mg/kg of busulfan, in this formulation at least, was comparable with 10 Gy of irradiation, whereas at the same time, demonstrating that 75–100 mg/kg busulfan was nonmyeloablative in C57BL/6 recipients (Supplementary Figure S1). This could lead to the limited elevation of MCP-1 Lampron et al. observed after transplant, thus compromising migration. Clinically, high doses of busulfan are often combined with cyclophosphamide or fludarabine to generate a fully myeloablative regimen. Typically, this leads to >95% recipient engraftment.29 However, although this makes sense in an allogeneic setting, cyclophosphamide is not required as an immunosuppressive in syngeneic murine transplants with full intensity busulfan myeloablation, as there is no requirement for immunosuppression. The combination of low dose nonmyeloablative busulfan and cyclophosphamide in this setting19 obscures the outcome, due to insufficient myeloablation and potential interactions between the two drugs.
Capotondo et al., observed an increase in brain engraftment in busulfan-conditioned recipients compared with the irradiated at 45 days and 3 months posttransplant but showed no differences at 5 days, 2 weeks or 6 months. Their regimen was almost fully myeloablative at 100 mg/kg busulfan,20 and this may have contributed to the variability observed. In our hands and using our formulation of busulfan this dose is borderline myeloablative, with mixed responses (Supplementary Figure S1). In addition, a mixture of metachromatic leukodystrophy and WT recipients was used, despite a significant increase in brain engraftment observed in metachromatic leukodystrophy recipients compared with the WT recipients at 3 months posttransplant (genotype differences from other timepoints were not presented). It is possible that the storage material or more likely, the established neuroinflammatory events observed in metachromatic leukodystrophy14,30 could have perturbed chemokine/cytokine levels resulting in elevated transmigration.
We observed incomplete repopulation of the brain by donor cells, with much fewer donor-derived GFP+ cells in busulfan-conditioned and irradiated brain compared with the total number of Iba-1+ microglia. We estimate that 22% of GFP+ donor cells repopulated the microglial niche after busulfan conditioning and 10% GFP+ donor cells repopulated the microglial niche in irradiated recipients, in agreement with the published data.4,31 In contrast, Capotondo et al. detected a higher proportion of donor-derived cells;20 however, these data may be skewed by the use of CD45 and CD11b cell surface markers and flow cytometry to distinguish GFP+ donor microglia. These markers are also expressed by a number of other cell types such as macrophages, neutrophils, T, and B cells, and we have also found a higher donor cell contributions to CD45+/CD11b+ brain cells (25–30%) when using this method (data not shown).
We detected a significant increase in total Iba-1+ microglial numbers in irradiated brain 2 weeks after BMT. These were predominantly GFP−/Iba-1+ microglia, suggesting in situ proliferation of resident microglial cells. However, although proliferation was very high in both treatment groups, no significant difference in the number of Ki67+ positive cells was detected between treatment groups at this timepoint, although there was a trend towards an increase in busulfan-conditioned brain. We hypothesize that in irradiated mice, microglia probably starts proliferating before those of busulfan-conditioned mice. This leads to an overall increase in total Iba-1+ cells in irradiated mice at 2 weeks, but proliferating cell numbers at this timepoint are approximately equal. It is well known that busulfan treatment leads to delayed engraftment over irradiation17 as previously discussed, and is the reason for delayed BM engraftment at 2 weeks (Figure 1a; (ii)). In the long term, the number of Iba-1+ cells in irradiated brains has returned to short term after BMT levels—which probably reflects homeostatic regulation of microglial numbers in the brain. However, irradiated microglia continue to exhibit significantly increased Ki67+ cell numbers compared with the busulfan in the long term. This observation, along with reduced donor-derived brain engraftment compared with the busulfan, strongly suggests that irradiation preferentially stimulates in situ proliferation over migration. In situ proliferation of microglia in response to irradiation has been described previously.2
In addition, irradiated brain exhibited significantly more amoeboid GFP+ and ILB4+ cells compared with the busulfan-conditioned recipients, suggesting that irradiation preferentially induces microglial activation. Irradiated brain exhibited significantly higher levels of IL-1α, a key mediator of inflammation,32 both initially and long term compared with the busulfan-conditioned brain, pointing towards an IL-1α driven proinflammatory environment. Furthermore, irradiation stimulated increased short-term levels of brain MIP-1α and serum RANTES both downstream of IL-1α whereas, busulfan conditioning led to higher short-term levels of IL-6, which is associated with pro- and anti-inflammatory properties.33
In summary, both irradiation and busulfan induce a neuroinflammatory environment but with different downstream effects. The prominent and sustained levels of IL-1α and reduced long-term MCP-1 in irradiated recipients, appears to drive an IL-1α neuroinflammatory response and in situ proliferative amoeboid phenotype in resident microglia, with less effective transmigration of donor cells to the brain. Around 20% of busulfan delivered intravenously can cross the BBB,34 exerting a long-term chemokine response in the brain via MCP-1, and driving a more promigratory inflammatory response, increasing transmigration of donor-derived microglia with ramified, surveillant morphology, and a reduced overall inflammatory profile over irradiation.
The different outcomes observed suggest that busulfan and irradiation stimulate neuroinflammation via different pathways. Irradiation has a potent apoptotic effect on cells and usually signals through the p53 pathway,35 but has also been shown to signal though acid sphingomyelinase in mouse BBB endothelial cells.36 In contrast, busulfan has been shown to induce senescence in cultured fibroblasts through Erk and p38 MAPK pathways in a p53 independent manner.18
We have demonstrated the significance of the different mechanisms of action of busulfan and irradiation by defining their role in transmigration and brain engraftment of donor-derived cells after BMT. Our findings have significant implications for the methodology used to test hematopoietic stem cells-based gene therapies in mouse models of neuropathic lysosomal storage disorders to achieve maximum delivery to the brain. Furthermore, myeloablative busulfan is more clinically applicable than irradiation and therefore, questions the use of irradiation in these mouse models. Future studies to investigate reduced intensity conditioning regimens, using low dose busulfan, in combination with infusion of gene-modified autologous cells, could expand the applicability of this therapeutic route to other severe neurodegenerative diseases such as Alzheimer's disease.
Methods
Mouse maintenance and BMT. Mice were housed in a 12/12-hour light/dark cycle with food and water provided ad libitum in accordance with the Animal (Scientific Procedures) Act, 1986 (UK), project license PPL40/3117. Recipients of 8–10 weeks old (C57BL/6J; Harlan, Bicester, UK) received full myeloablation; irradiation (2 × 5 Gy, 4 hours apart)37,38 or intraperitoneal busulfan (125 mg/kg) (Busilvex; Pierre Fabre, Boulogne, France) (25 mg/kg/day for 5 days).15
This dose of busulfan was selected based on the literature that showed that 125 mg/kg of busulfan was equivalent to a fully myeloablative dose of irradiation (10 Gy)28 and confirmed using a busulfan dose optimization study. C57BL/6 mice received busulfan (25–125 mg/kg) or 2 × 5 Gy irradiation ± anti-CD4/CD8 Abs (1 mg/mouse) followed by whole BM (2–10 × 106 cells/200 µl phosphate-buffered saline/mouse) transplant from CBA mice (Harlan Laboratories, Bicester, UK).37,39 All mice rejected transplants and were culled if they became anemic and had lost more than 20% of their body weight and the survival time was recorded.
For the brain engraftment study, whole BM37,39 from C57BL/6-TgN(ACTbEGFP)1Osb mice,40 (6–8 weeks old) expressing eGFP (Jackson Laboratories, Bar Harbor, ME), was delivered via tail vein (2 × 107 cells/200 µl phosphate-buffered saline/mouse). Peripheral blood chimerism (GFP) was measured using a BD FACS Canto II flow cytometer (BD Biociences, Oxford, UK) with ToPro3 iodide (Life Technologies, Paisley, UK) live/dead stain.
Mice (n = 6/group) were terminally anesthetized at either 2 weeks (short term) or 6–9 months (long term) after BMT and transcardially perfused with Tyrode's buffer to remove peripheral blood as previously described.15 One brain hemisphere was frozen for biochemistry, the other was fixed for immunohistochemistry.41
Immunohistochemistry. Free-floating immunohistochemistry was performed on brain sections (30 µm) (Figure 1a; (iii))42 using standard protocols.41 Rabbit anti-GFP antibody (1:750; Abcam, Cambridge, UK), rabbit anti-Iba-1 (1:1000; Wako Chemicals GmbH, Neuss, Germany) and isolectin B4 (ILB4; Sigma, Poole, UK)43 staining was visualized using DAB substrate (Vector, Peterborough, UK) and Mayer's hematoxylin. Sections were imaged using the Panoramic SCAN with Zeiss Plan-apochromat 20×/0.8 objective, (3D Histotech/Laser2000, Ringstead, UK). GFP+, ILB4+, and Iba-1+ cells were counted from six sections of mouse brain as shown (Figure 1a; (i)).
Fluorescent labeling used Alexa-594-ILB4 (1:200; Life Technologies) and primary antibodies; chicken anti-GFP (1:500; Abcam), rabbit anti-Ki67 antibody (1:500; Abcam), goat anti-Iba-1 (1:600; Abcam), and chicken anti-GFAP (1:1500; Abcam). Primary antibodies were labeled with the appropriate secondary antibodies; Alexa-488 or Alexa-594 goat anti-chicken IgG, or Alexa-488 goat anti-rabbit IgG (1:1000; Life Technologies) and 300 nmol/l DAPI (Life Technologies) to stain nuclei as previously described.44 Sections were mounted using ProLong Gold Antifade medium (Life Technologies) and examined using a Nikon C1 confocal microscope on an upright 90i microscope with a ×20 or 60×/1.40 Plan Apo objective (Nikon UK, Kingston upon Thames, UK). At least three sections per mouse and three mice per group were visualized.
Brain cytokine/chemokine levels. IL-1α, IL-1β, IL-6, IL-9, IL-13, IFN-γ, MCP-1 (CCL2), MIP-1α (CCL3), G-CSF, GM-CSF, KC (CXCL1), and RANTES (CXCL5) were measured in brain extracts using BD Cytometric Bead Array (CBA) Flex Set kits (BD Biosciences, Oxford, UK) as previously described.44
Statistical analysis. The data were analyzed using a Student's t-test (cell counting and biochemistry) or one-way analysis of variance with Tukey's multicomparison test (chimerism) and significance assumed at P ≤ 0.05.
SUPPLEMENTARY MATERIAL Figure S1. Selection of a myeloablative busulfan dose comparable with the 10 Gy of irradiation. Figure S2. Determining the percentage contribution of donor and recipient T cells, B cells, and monocytes in peripheral blood over time after syngeneic transplant.
Acknowledgments
The authors gratefully acknowledge the MPS Society (UK) and the Lady Shauna Gosling Trust for funding, the NIHR Manchester Biomedical Research Centre, and the staff from the BSU and the Bioimaging Facility (FLS) at the University of Manchester. The authors declared no conflict of interest.
Supplementary Material
References
- Krause DS, Theise ND, Collector MI, Henegariu O, Hwang S, Gardner R.et al. (2001Multi-organ, multi-lineage engraftment by a single bone marrow-derived stem cell Cell 105369–377. [DOI] [PubMed] [Google Scholar]
- Ajami B, Bennett JL, Krieger C, Tetzlaff W., and, Rossi FM. Local self-renewal can sustain CNS microglia maintenance and function throughout adult life. Nat Neurosci. 2007;10:1538–1543. doi: 10.1038/nn2014. [DOI] [PubMed] [Google Scholar]
- Mildner A, Schmidt H, Nitsche M, Merkler D, Hanisch UK, Mack M.et al. (2007Microglia in the adult brain arise from Ly-6ChiCCR2+ monocytes only under defined host conditions Nat Neurosci 101544–1553. [DOI] [PubMed] [Google Scholar]
- Priller J, Flügel A, Wehner T, Boentert M, Haas CA, Prinz M.et al. (2001Targeting gene-modified hematopoietic cells to the central nervous system: use of green fluorescent protein uncovers microglial engraftment Nat Med 71356–1361. [DOI] [PubMed] [Google Scholar]
- Chen Y, Hallenbeck JM, Ruetzler C, Bol D, Thomas K, Berman NE.et al. (2003Overexpression of monocyte chemoattractant protein 1 in the brain exacerbates ischemic brain injury and is associated with recruitment of inflammatory cells J Cereb Blood Flow Metab 23748–755. [DOI] [PubMed] [Google Scholar]
- Kuziel WA, Morgan SJ, Dawson TC, Griffin S, Smithies O, Ley K.et al. (1997Severe reduction in leukocyte adhesion and monocyte extravasation in mice deficient in CC chemokine receptor 2 Proc Natl Acad Sci USA 9412053–12058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu K, Waskow C, Liu X, Yao K, Hoh J., and, Nussenzweig M. Origin of dendritic cells in peripheral lymphoid organs of mice. Nat Immunol. 2007;8:578–583. doi: 10.1038/ni1462. [DOI] [PubMed] [Google Scholar]
- Soulet D., and, Rivest S. Bone-marrow-derived microglia: myth or reality. Curr Opin Pharmacol. 2008;8:508–518. doi: 10.1016/j.coph.2008.04.002. [DOI] [PubMed] [Google Scholar]
- Ransohoff RM. Microgliosis: the questions shape the answers. Nat Neurosci. 2007;10:1507–1509. doi: 10.1038/nn1207-1507. [DOI] [PubMed] [Google Scholar]
- Diserbo M, Agin A, Lamproglou I, Mauris J, Staali F, Multon E.et al. (2002Blood-brain barrier permeability after gamma whole-body irradiation: an in vivo microdialysis study Can J Physiol Pharmacol 80670–678. [DOI] [PubMed] [Google Scholar]
- Li YQ, Chen P, Jain V, Reilly RM., and, Wong CS. Early radiation-induced endothelial cell loss and blood-spinal cord barrier breakdown in the rat spinal cord. Radiat Res. 2004;161:143–152. doi: 10.1667/rr3117. [DOI] [PubMed] [Google Scholar]
- Kyrkanides S, Moore AH, Olschowka JA, Daeschner JC, Williams JP, Hansen JT.et al. (2002Cyclooxygenase-2 modulates brain inflammation-related gene expression in central nervous system radiation injury Brain Res Mol Brain Res 104159–169. [DOI] [PubMed] [Google Scholar]
- Linard C, Marquette C, Mathieu J, Pennequin A, Clarençon D., and, Mathé D. Acute induction of inflammatory cytokine expression after gamma-irradiation in the rat: effect of an NF-kappaB inhibitor. Int J Radiat Oncol Biol Phys. 2004;58:427–434. doi: 10.1016/j.ijrobp.2003.09.039. [DOI] [PubMed] [Google Scholar]
- Biffi A, De Palma M, Quattrini A, Del Carro U, Amadio S, Visigalli I.et al. (2004Correction of metachromatic leukodystrophy in the mouse model by transplantation of genetically modified hematopoietic stem cells J Clin Invest 1131118–1129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Langford-Smith A, Wilkinson FL, Langford-Smith KJ, Holley RJ, Sergijenko A, Howe SJ.et al. (2012Hematopoietic stem cell and gene therapy corrects primary neuropathology and behavior in mucopolysaccharidosis IIIA mice Mol Ther 201610–1621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Visigalli I, Delai S, Politi LS, Di Domenico C, Cerri F, Mrak E.et al. (2010Gene therapy augments the efficacy of hematopoietic cell transplantation and fully corrects mucopolysaccharidosis type I phenotype in the mouse model Blood 1165130–5139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meng A, Wang Y, Brown SA, Van Zant G., and, Zhou D. Ionizing radiation and busulfan inhibit murine bone marrow cell hematopoietic function via apoptosis-dependent and -independent mechanisms. Exp Hematol. 2003;31:1348–1356. doi: 10.1016/j.exphem.2003.08.014. [DOI] [PubMed] [Google Scholar]
- Probin V, Wang Y, Bai A., and, Zhou D. Busulfan selectively induces cellular senescence but not apoptosis in WI38 fibroblasts via a p53-independent but extracellular signal-regulated kinase-p38 mitogen-activated protein kinase-dependent mechanism. J Pharmacol Exp Ther. 2006;319:551–560. doi: 10.1124/jpet.106.107771. [DOI] [PubMed] [Google Scholar]
- Lampron A, Lessard M., and, Rivest S. Effects of myeloablation, peripheral chimerism, and whole-body irradiation on the entry of bone marrow-derived cells into the brain. Cell Transplant. 2012;21:1149–1159. doi: 10.3727/096368911X593154. [DOI] [PubMed] [Google Scholar]
- Capotondo A, Milazzo R, Politi LS, Quattrini A, Palini A, Plati T.et al. (2012Brain conditioning is instrumental for successful microglia reconstitution following hematopoietic stem cell transplantation Proc Natl Acad Sci USA 10915018–15023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ransohoff RM., and, Cardona AE. The myeloid cells of the central nervous system parenchyma. Nature. 2010;468:253–262. doi: 10.1038/nature09615. [DOI] [PubMed] [Google Scholar]
- Wake H, Moorhouse AJ, Jinno S, Kohsaka S., and, Nabekura J. Resting microglia directly monitor the functional state of synapses in vivo and determine the fate of ischemic terminals. J Neurosci. 2009;29:3974–3980. doi: 10.1523/JNEUROSCI.4363-08.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kanazawa H, Ohsawa K, Sasaki Y, Kohsaka S., and, Imai Y. Macrophage/microglia-specific protein Iba1 enhances membrane ruffling and Rac activation via phospholipase C-gamma -dependent pathway. J Biol Chem. 2002;277:20026–20032. doi: 10.1074/jbc.M109218200. [DOI] [PubMed] [Google Scholar]
- Streit WJ., and, Kreutzberg GW. Lectin binding by resting and reactive microglia. J Neurocytol. 1987;16:249–260. doi: 10.1007/BF01795308. [DOI] [PubMed] [Google Scholar]
- Samlowski WE, Araneo BA, Butler MO, Fung MC., and, Johnson HM. Peripheral lymph node helper T-cell recovery after syngeneic bone marrow transplantation in mice prepared with either gamma-irradiation or busulfan. Blood. 1989;74:1436–1445. [PubMed] [Google Scholar]
- Samlowski WE., and, Crump CL. Recovery of contact hypersensitivity responses following murine bone marrow transplantation: comparison of gamma-irradiation and busulfan as preparative marrow-ablative agents. Blood. 1987;70:1910–1920. [PubMed] [Google Scholar]
- Thomas J, Liu F., and, Link DC. Mechanisms of mobilization of hematopoietic progenitors with granulocyte colony-stimulating factor. Curr Opin Hematol. 2002;9:183–189. doi: 10.1097/00062752-200205000-00002. [DOI] [PubMed] [Google Scholar]
- Jopling C., and, Rosendaal M. A cautionary tale: how to delete mouse haemopoietic stem cells with busulphan. Br J Haematol. 2001;113:970–974. doi: 10.1046/j.1365-2141.2001.02825.x. [DOI] [PubMed] [Google Scholar]
- Bacigalupo A, Ballen K, Rizzo D, Giralt S, Lazarus H, Ho V.et al. (2009Defining the intensity of conditioning regimens: working definitions Biol Blood Marrow Transplant 151628–1633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hess B, Saftig P, Hartmann D, Coenen R, Lüllmann-Rauch R, Goebel HH.et al. (1996Phenotype of arylsulfatase A-deficient mice: relationship to human metachromatic leukodystrophy Proc Natl Acad Sci USA 9314821–14826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kennedy DW., and, Abkowitz JL. Kinetics of central nervous system microglial and macrophage engraftment: analysis using a transgenic bone marrow transplantation model. Blood. 1997;90:986–993. [PubMed] [Google Scholar]
- Allan SM, Tyrrell PJ., and, Rothwell NJ. Interleukin-1 and neuronal injury. Nat Rev Immunol. 2005;5:629–640. doi: 10.1038/nri1664. [DOI] [PubMed] [Google Scholar]
- Mihara M, Hashizume M, Yoshida H, Suzuki M., and, Shiina M. IL-6/IL-6 receptor system and its role in physiological and pathological conditions. Clin Sci. 2012;122:143–159. doi: 10.1042/CS20110340. [DOI] [PubMed] [Google Scholar]
- Hassan M, Oberg G, Ericson K, Ehrsson H, Eriksson L, Ingvar M.et al. (1992In vivo distribution of [11C]-busulfan in cynomolgus monkey and in the brain of a human patient Cancer Chemother Pharmacol 3081–85. [DOI] [PubMed] [Google Scholar]
- Lowe SW, Schmitt EM, Smith SW, Osborne BA., and, Jacks T. p53 is required for radiation-induced apoptosis in mouse thymocytes. Nature. 1993;362:847–849. doi: 10.1038/362847a0. [DOI] [PubMed] [Google Scholar]
- Soussain C, Ricard D, Fike JR, Mazeron JJ, Psimaras D., and, Delattre JY. CNS complications of radiotherapy and chemotherapy. Lancet. 2009;374:1639–1651. doi: 10.1016/S0140-6736(09)61299-X. [DOI] [PubMed] [Google Scholar]
- Bigger BW, Siapati EK, Mistry A, Waddington SN, Nivsarkar MS, Jacobs L.et al. (2006Permanent partial phenotypic correction and tolerance in a mouse model of hemophilia B by stem cell gene delivery of human factor IX Gene Ther 13117–126. [DOI] [PubMed] [Google Scholar]
- Siapati EK, Bigger BW, Kashofer K, Themis M, Thrasher AJ., and, Bonnet D. Murine leukemia following irradiation conditioning for transplantation of lentivirally-modified hematopoietic stem cells. Eur J Haematol. 2007;78:303–313. doi: 10.1111/j.1600-0609.2006.00813.x. [DOI] [PubMed] [Google Scholar]
- Siapati EK, Bigger BW, Miskin J, Chipchase D, Parsley KL, Mitrophanous K.et al. (2005Comparison of HIV- and EIAV-based vectors on their efficiency in transducing murine and human hematopoietic repopulating cells Mol Ther 12537–546. [DOI] [PubMed] [Google Scholar]
- Okabe M, Ikawa M, Kominami K, Nakanishi T., and, Nishimune Y. ‘Green mice' as a source of ubiquitous green cells. FEBS Lett. 1997;407:313–319. doi: 10.1016/s0014-5793(97)00313-x. [DOI] [PubMed] [Google Scholar]
- Malinowska M, Wilkinson FL, Langford-Smith KJ, Langford-Smith A, Brown JR, Crawford BE.et al. (2010Genistein improves neuropathology and corrects behaviour in a mouse model of neurodegenerative metabolic disease PLoS ONE 5e14192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paxinos F. Academic Press: New York; 2004. The Mouse Brain in Stereotaxic Coordinates. [Google Scholar]
- Canal MM, Wilkinson FL, Cooper JD, Wraith JE, Wynn R., and, Bigger BW. Circadian rhythm and suprachiasmatic nucleus alterations in the mouse model of mucopolysaccharidosis IIIB. Behav Brain Res. 2010;209:212–220. doi: 10.1016/j.bbr.2010.01.045. [DOI] [PubMed] [Google Scholar]
- Wilkinson FL, Holley RJ, Langford-Smith KJ, Badrinath S, Liao A, Langford-Smith A.et al. (2012Neuropathology in mouse models of mucopolysaccharidosis type I, IIIA and IIIB PLoS ONE 7e35787. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.