Abstract
Purpose
The goal of this survey was to obtain detailed information on the faculty currently responsible for teaching radiation biology courses to radiation oncology residents in the U.S. and Canada.
Methods and Materials
In March-December 2007 a survey questionnaire was sent to faculty having primary responsibility for teaching radiation biology to residents in 93 radiation oncology residency programs in the U.S. and Canada.
Results
The responses to this survey document the aging of the faculty who have primary responsibility for teaching radiation biology to radiation oncology residents. The survey found a dramatic decline with time in the percentage of educators whose graduate training was in radiation biology. A significant number of the educators responsible for teaching radiation biology were not fully acquainted with the radiation sciences, either through training or practical application. In addition, many were unfamiliar with some of the organizations setting policies and requirements for resident education. Freely available tools, such as the ASTRO Radiation & Cancer Biology Practice Exam used by residents and educators. Consoination and Study Guides, were widely lidation of resident courses or use of a national radiation biology review course, were viewed as unlikely to be employed by most programs.
Conclusions
A high priority should be given to the development of comprehensive teaching tools to assist those individuals who have responsibility for teaching radiation biology courses, but who do not have an extensive background in critical areas of radiobiology related to radiation oncology. These findings also suggest a need for new graduate programs in radiobiology.
Keywords: radiation biology, teaching, radiation oncology residents
INTRODUCTION
A foundation in the biological principles underlying radiotherapy and familiarity with the major research areas in contemporary radiation biology are essential components of residency training for radiation oncologists. Knowledge of relevant areas of radiobiology is also critical to allow radiation oncologists to deliver state-of-the-art clinical care to their patients and to undertake translational and clinical research related to cancer therapy. On a more pragmatic level, radiation biology is one of the three major content areas in which radiation oncology residents must demonstrate proficiency, through successful completion of the written examination in radiation biology, to receive certification from the American Board of Radiology (ABR) (1). This exam also includes a significant number of questions on basic molecular biology and cancer biology; in this report, it is therefore assumed that “didactic courses in radiation biology” include lectures in these areas.
For continuing accreditation of radiation oncology residency programs, the Accreditation Council for Graduate Medical Education (ACGME) requires that a comprehensive course in radiation biology be provided as part of the training program and that “The faculty must include at least one full-time radiation biologist or cancer biologist (Ph.D. level or equivalent) who is on site to provide a scholarly environment of research, and to participate in the teaching of radiation and cancer biology” (2). However, based upon the widely perceived decline in the number of pre- and post-doctoral radiation biology trainees, concern has arisen that there may be a shortage of educators with backgrounds appropriate to teach a comprehensive course in radiation biology that includes all the topics listed in the ABR syllabus for radiation and cancer biology.
Several previous publications have addressed issues related to radiation biology education in radiation oncology (3-8). A survey of radiation biology instructors and radiation biology courses performed in 2001 (9, 10) provided the first documentation of the aging of the cohort of radiation biology educators with backgrounds in the radiation sciences. The purposes of the current survey were to update the demographic data for individuals with responsibility for teaching radiation biology, to obtain information not addressed in the previous survey and to formulate recommendati Rons that could help maintain the quality of radiation biology instruction in radiation oncology residency programs.
METHODS AND MATERIALS
A survey was developed by the members of the Radiation and Cancer Biology Teaching and Curriculum Subcommittee of the ASTRO Radiation and Cancer Biology Committee. The authors comprise this subcommittee. The survey consisted of 26 questions in 6 categories: 6 questions on teacher educational background, 3 on research interests and resident participation, 7 on effort and departmental support for teaching and mentoring residents, 2 on familiarity with responsible for formulating educational guidelines in radiation oncology, 6 on certification and self-assessment examinations and 2 on potential use of new educational materials.
Information concerning radiation oncology residency programs in the U.S. was obtained from the Directory of Radiation Oncology Residency Programs, which is updated annually by the Association of Residents in Radiation Oncology (ARRO). Radiation oncology residency programs in Canada were identified using information from the Canadian Association of Radiation Oncology (CARO). A telephone call was placed to the individual listed as the program director for each radiation oncology residency program to request the name and contact information for the faculty member with primary responsibility for teaching radiatio biology in that program. An e-mail was then sent to this individual asking for confirmation that he/she had primary responsibility for teaching radiation biology in that program. If that individual responded negatively, he/she was asked to provide the name and contact information for the correct individual. If that person confirmed his/her role as the primary radiation biology instructor in the program, a request was made to complete and return the Radiation Biology Educators Survey. Assurance was given that all survey responses would remain anonymous and that statistical analyses and publication of study results would include only grouped data, thereby eliminating potential linkage of information to specific participants or programs.
RESULTS
Demographics
All 93 radiation oncology residency programs in the U.S. and Canada were contacted. Nine program directors responded that there was no faculty member assigned to teach a course in radiation biology at the time of the survey. In the remaining 84 programs, 73 educators were identified as having primary responsibility for teaching radiation biology to radiation oncology residents; some educat taught in more than one program (two to five residency programs). Of these 73 educators, 66 submitted completed surveys, yielding an overall response rate of 90%. Responses were not obtained for every question from each participant. Thus, the number of responses to certain questions was less than 66.
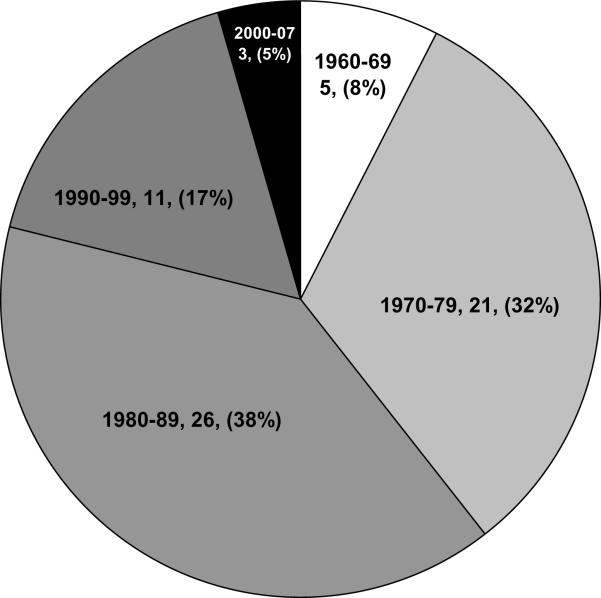
Of the radiation biology educators responding to the survey, 78% (Fig. 1) obtained their highest degree before 1990. The average age of faculty having principal responsibility for teaching radiation biology in the residency programs was estimated to be approximately 52 years. This estimation was made by assuming that for each time interval on the survey, the average year in which the decade and that the aver age at the time of completion of the degree was 27 years. Of greatest significance is the relative lack of lead radiobiology teachers who completed their training since 1990. This reflects in part the fact that in some residency programs responsibility for organizing the course is given to a senior member of a group of radiobiologists. However, in many programs, the lead educator teaches most or all of the course. Under such circumstances, which are probably more typical of small and medium sized residency programs, a critical problem could develop in 10-15 years, when a substantial cohort of educators who received their degrees during the 1970s and 1980s retire.
Figure 1.
Decade during which the highest degree was awarded. The number and percentage of respondents for each decade are indicated.
Training Backgrounds
Of the respondents to this survey, 83%, 8% and 9% hold Ph.D., M.D. and M.D./Ph.D. degrees, respectively. The average age of 45 years for the educators with M.D. or M.D./Ph.D. degrees was lower than that of 54 years for those with a Ph.D. This finding supports the perceived decline in radiobiology-trained Ph.D.s in radiation oncology programs and also suggests an emerging trend of assigning responsibility for organizing radiation biology courses to faculty holding M.D. or M.D/Ph.D. degrees. For those educators possessing M.D. degrees, 9/11 were either board certified or board eligible in radiation oncology.
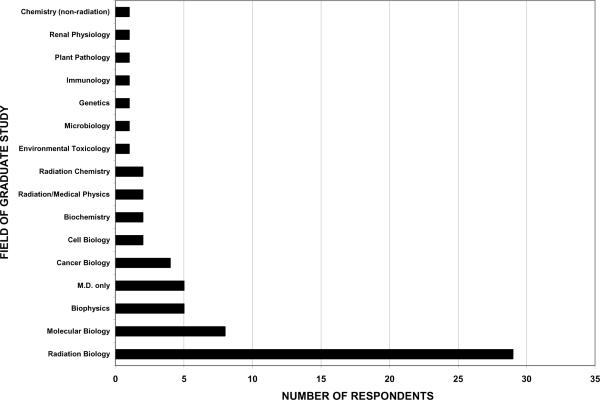
There was an almost equal division between educators holding Ph.D. degrees in either radiation biology or biophysics (52%) and those whose highest degree was either an M.D. or a Ph.D in a field other than radiobiology/biophysics (48%). (It is appropriate to group individuals with Ph.D.s in biophysics with those holding Ph.D.s in radiation biology since, historically, several major institutions that trained radiobiologists granted doctorates in biophysics, rather than in radiation biology per se. These programs included substantial radiobiology course work, particularly during the 1970s and 1980s when many of the current educators were trained.) The average ages for educators whose degrees are in radiobiology and biophysics were 58 years and 56 years, respectively. Those who received degrees in areas outside of radiation biology or biophysics held degrees in a wide variety of fields (Fig. 2). The average age for radiation biology educators with Ph.D.s in fields other than radiobiology/biophysics was 47 years. This again suggests that faculty whose degrees are in fields outside radiobiology/biophysics may be increasingly responsible for teaching radiation biology courses.
Figure 2.
Field in which respondents received their doctorates.
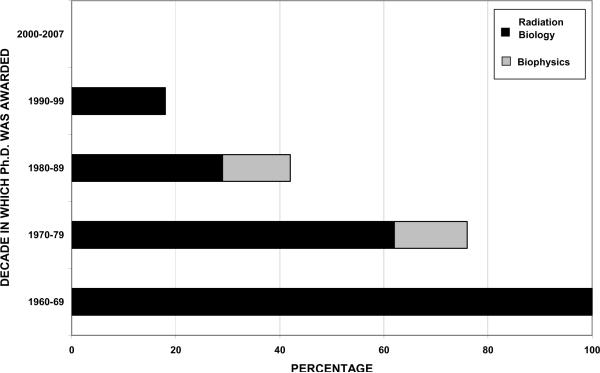
The percentage of radiobiology educators whose graduate training was reported as being in radiation biology/biophysics changed dramatically as a function of the year in which the Ph.D. degree was received (Fig. 3). Younger educators were much less likely to have degrees in radiobiology/biophysics. Of those educators who either do not possess a Ph.D. in a “radiation science” (i.e., radiation biology, biophysics, radiation chemistry and medical physics) or are not board certified/eligible in radiation oncology, 42% reported both taking courses and performing research in the radiation sciences as graduate students. However, 25% responded that they only conducted research in this area, 8% reported only taking courses in the radiation sciences and 25% indicated that they had neither taken courses nor performed research in radiation biology during their graduate training.
Figure 3.
Percentage of respondents holding a Ph.D. in either radiation biology or biophysics as a function of the decade during which they obtained their degrees. There were no respondents who received a Ph.D. in radiation biology or biophysics during the period 2000-2007.
Of the respondents, 89% held academic appointments in radiation oncology departments, 3% held adjunct appointments, and 8% did not hold a position as a faculty member in a radiation oncology department.
Research Areas
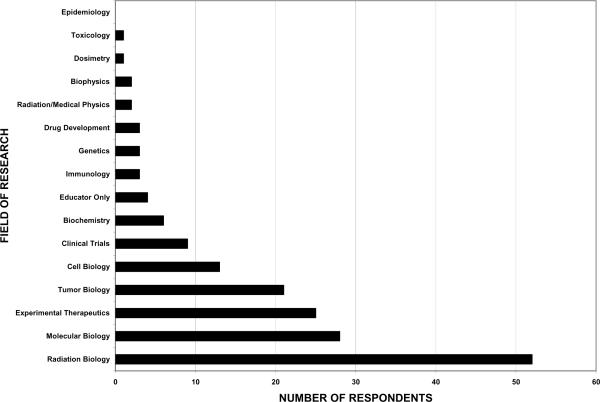
Respondents were asked to select up to three choices indicating their research areas of interest. Radiation biology was the most common area and was selected by 79% (52/66) as a research focus (Fig. 4). Experimental therapeutics, tumor biology and molecular biology were identified frequently as areas of research. This suggests that, independent of the field of their graduate training, a majority of the educators perform research in or related to radiation biology, cancer biology or cancer therapy.
Figure 4.
Fields in which respondents were performing research. Respondents were asked to identify up to three areas of research; 21 of the 66 respondents identified one or two areas of focus while the remaining 45 respondents listed three areas. The data reflect the number of responses, rather than the number of educators.
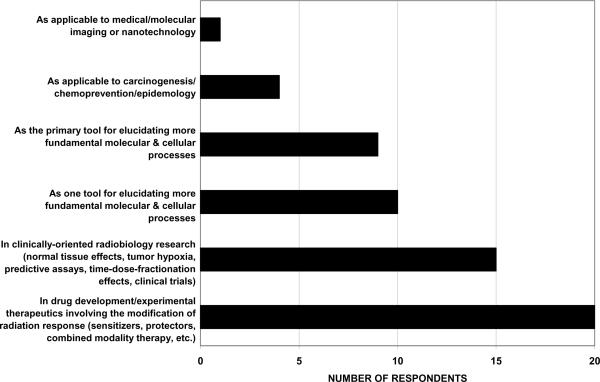
When asked what percentage of their research involved the use of ionizing radiation, 60% of the respondents indicated that radiation was used in more than half of their research (Table 1). Of those who used ionizing radiation in their research, 56% used radiation for research directly related to cancer therapy, while another 29% used radiation as a tool for elucidating fundamental molecular and cellular processes (Fig. 5).
Table 1.
Research using radiation, time devoted to teaching & salary support for teaching
| 0% | 0-5% | 5-10% | 10-25% | 25-50% | 50-75% | 75-100% | |
|---|---|---|---|---|---|---|---|
| Percentage of research involving ionizing radiation | 5* (8)† | 11 (18) | 9 (15) | 13 (21) | 24 (39) | ||
| Percentage of time & effort devoted to teaching radiation biology | 0* (0) | 2 (3) | 40 (61) | 18 (27) | 6 (9) | 0 (0) | 0 (0) |
| Percentage of time & effort devoted to training residents in research | 6 (9) | 21 (31) | 28 (42) | 11 (16) | 1 (1) | 0 (0) | 0 (0) |
| Percentage of salary designated to teaching & mentoring residents | 18 (27) | 9 (14) | 11 (17) | 17 (26) | 6 (9) | 3 (4) | 2 (3) |
= number of respondents
Percentage of respondents
Figure 5.
Research uses of ionizing radiation by survey respondents.
Proportion of time teaching and guiding research
On average, the educators devoted 13% of their time to teaching radiobiology and 8% of their time to mentoring residents in research (Table 1). The mean percentage of salary paid to support their efforts in teaching residents was 15%, somewhat lower than the 21% effort that the faculty indicated they spent in this capacity.
Priority placed on resident education
While 71% and 65% of the radiation biology educators indicated that they and their departments, respectively, placed either a high priority or the highest priority on teaching residents (Table 2), a small number of respondents indicated that either they or their departments placed a medium or low priority on teaching residents.
Table 2.
Priority placed on teaching
| Lowest | Low | Medium | High | Highest | |
|---|---|---|---|---|---|
| Personal Teaching/Mentoring Priority | 0* (0)† | 1 (2) | 18 (27) | 35 (53) | 12 (18) |
| Department Teaching/Mentoring Priority | 1 (2) | 5 (8) | 17 (25) | 34 (51) | 9 (14) |
Number of respondents
Percentage of respondents
In terms of support from their departments, only 35% of the respondents indicated they had secretarial/administrative assistance in preparing teaching materials. Another 57% said they had no secretarial/administrative assistance and 8% indicated that in principle they had such support, but in practice it was insufficient. Fifty-six percent said that they had funds available from their department to purchase books, pay professional society dues, attend meetings, etc., in order to maintain or improve their teaching effectiveness. However, 20% indicated that they did not receive this type of support from their departments, while 24% responded that while they were given funds for these purposes, the amount provided was insufficient.
Familiarity with organizations that set educational guidelines
Most radiation biology educators were familiar with ASTRO and the Radiation Research Society (RRS) (Table 3). In contrast, 31%, 59% and 47% of the respondents reported that they were either unfamiliar with or had little familiarity with the ABR, ACGME and the American College of Radiology (ACR), respectively. Although 72% of the respondents stated that they were familiar with the ABR guidelines, 28% indicated that they had little or no familiarity with these guidelines. Just a small percentage of educators were moderately to very familiar with the American College of Radiation Oncology (ACRO).
Table 3.
Familiarity with radiation oncology organizations
| Unfamiliar | Little familiarity | Moderately familiar | Quite familiar | Very familiar | |
|---|---|---|---|---|---|
| American Society for Radiation Oncology, ASTRO | 0* (0)† | 1 (2) | 12 (18) | 24 (36) | 29 (44) |
| Radiation Research Society, RRS | 3 (5) | 2 (3) | 5 (8) | 10 (15) | 46 (69) |
| American Board of Radiology, ABR | 5 (8) | 15 (23) | 19 (28) | 14 (21) | 13 (20) |
| Accreditation Council for Graduate Medical Education, ACGME | 17 (26) | 22 (33) | 13 (20) | 6 (9) | 8 (12) |
| American College of Radiology, ACR | 10 (15) | 21 (32) | 18 (27) | 9 (14) | 8 (12) |
| American College of Radiation Oncology, ACRO | 23 (25) | 27 (40) | 7 (11) | 8 (12) | 1 (2) |
| ABR Guidelines for Teaching Radiation & Cancer Biology | 4 (6) | 14 (22) | 46 (72) | 0 (0) | 0 (0) |
Number of respondents
Percentage of respondents
Only 38% of the educators reported that they were routinely provided with resident scores on either the biology section of the annual In-Training examination of the ACR or the comparable section of the ABR Written Board exam in radiation oncology. This information was sometimes provided to 42% of the respondents, while 20% indicated that they were never given these results. Thus, slightly more than half of the educators were not routinely offered this information on the performance of their students, even though it could have been of help in determining how their residents were performing relative to residents in other programs and in identifying areas of weakness in their courses. For the educators who indicated that they were given the scores, 58% reported that they received this information from the residency program director, whereas 10%, 22% and 10% indicated that they had to ask other people to obtain the scores, were given the results by residents or were informed of the scores at faculty meetings, respectively.
ASTRO Radiation and Cancer Biology Practice Examination and Study Guide
In recognition of the critical need to develop new ways to promote education in the biologic basis of radiotherapy, the ASTRO Radiation and Cancer Biology Committee appointed a subcommittee several years ago to develop a dynamic, web-based educational tool for radiation oncologists to further their study of radiation and cancer biology. The annual ASTRO Radiation and Cancer Biology Practice Examination and Study Guides (RCB Study Guides), which can be downloaded from the ARRO web site (http://www.arro.org/residents/physics_rad_bio/index.htm), are the product of these efforts. The topics included in the RCB Study Guides are based on those listed by the ABR for the written examination in radiation biology. The number of questions in each section roughly reflects the relative weight given by the ABR to each topic on the written board certification examination. The RCB Study Guides provide guidance and review both to residents preparing for the biology portion of their radiation oncology certification examination and to radiation oncologists taking the examination required for maintenance of certification. References are included in the RCB Guides with hypertext links to review articles on topics that are not addressed in depth in the most widely used radiation biology textbooks.
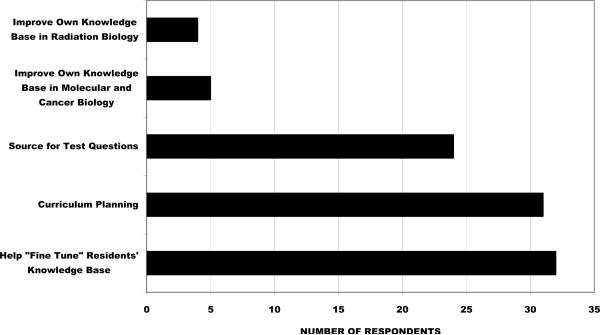
83% of the radiation biology instructors were familiar with and used the RCB Study Guides, 11% had heard of the Guides, but did not use them and 6% had not heard of this educational tool. The educators reported that a high percentage of their residents use the RCB Study Guides: 85% of the respondents reported that 75-100% of the residents in their program used the Guides, while 8% and 7% indicated that 50-75% and 25-50% of their residents used these materials, respectively. The teachers primarily used the RCB Study Guides for curriculum planning, as a source of test questions and to help “fine tune” their residents' knowledge base (Fig. 6).
Figure 6.
Use of the ASTRO Radiation & Cancer Biology Practice Examination and Study Guides by survey respondents.
An annual evaluation of the RCB Study Guides is performed by ARRO. The combined results of the surveys for the 2006-2008 versions of the Study Guides (Table 4), which tabulated the responses of 166 residents who completed surveys, indicated that more than 90% of the respondents either “strongly agreed” or “agreed” with positive statements characterizing the RCB Study Guides. These results were provided by Mr. Steven Smith, the ASTRO liaison to ARRO, and are quoted with the permission of ARRO.
Table 4.
ARRO survey results for the 2006, 2007 and 2008 ASTRO Radiation & Cancer Biology Examination & Study Guides
| Strongly Agree | Agree | Disagree | Strongly Disagree | Not Applicable | |
|---|---|---|---|---|---|
| The Study Guide questions were well written and clear. | 50* | 44 | 1 | 0 | 5 |
| The explanations to the questions were clear and informative with appropriate justification for the correct and incorrect responses. | 48 | 44 | 3 | 0 | 5 |
| Provided references helped to further your study of the area tested. | 34 | 39 | 7 | 3 | 17 |
| The material was helpful in preparing for the boards. | 67 | 23 | 1 | 0 | 9 |
| The questions were a good representation of the information tested on the boards. | 36 | 36 | 8 | 3 | 17 |
| I would recommend the use of the Study Guide to other residents/my colleagues. | 71 | 21 | 2 | 1 | 5 |
Percentage of respondents in each category for every statement. The number of respondents for the 2006, 2007 and 2008 RCB Study Guides were 51, 67 and 48. respectively.
Educational Resources
In order to improve their teaching of radiation biology, nearly all (97%) of the educators responded that they might, probably or definitely would use a detailed core curriculum expanding on the ABR syllabus (Table 5). In addition, the majority might or would use free or low cost educational materials provided by ASTRO, ABR or ACR. One third of the respondents already used some guest lecturers with specific expertise to teach their residents and many others would consider this option. Only 23% said they would not use guest lecturers or were unlikely to do so. However, most educators said they would not or were unlikely to use third party, web-based distance learning courses (for which there would presumably be a charge). The majority of respondents said their programs were unlikely to employ a freelance educator to do most or all of the teaching.
Table 5.
Proposed Actions to Improve Teaching
| Wouldn't | Unlikely | Might | Probably | Definitely | Already | |
|---|---|---|---|---|---|---|
| Use a detailed core curriculum expanding on the ABR syllabus? | 2* (3)† | 0 (0) | 10 (15) | 24 (36) | 30 (46) | N/A |
| Use free or low cost ASTRO, ABR, or ACR web-based/distance learning courses | 3 (5) | 4 (6) | 11 (17) | 14 (21) | 32 (48) | 2 (3) |
| Use guest lecturers with expertise for some teaching | 4 (6) | 11 (17) | 5 (8) | 14 (21) | 10 (15) | 22 (33) |
| Use third party web-based/distance learning courses | 12 (18) | 25 (38) | 10 (15) | 14 (21) | 5 (8) | 0 (0) |
| Use freelance educator to do most teaching | 33 (22) | 22 (33) | 3 (5) | 5 (8) | 1 (2) | 2 (3) |
| Use local or regional consolidation of teaching by a single radiation biologist | 8 (12) | 12 (18) | 10 (15) | 19 (29) | 3 (5) | 14 (21) |
| Consolidate teaching efforts, but use acknowledged experts | 12 (18) | 17 (26) | 6 (9) | 21 (32) | 3 (5) | 7 (11) |
| Send residents to a national course | 23 (35) | 19 (29) | 10 (15) | 5 (8) | 2 (3) | 7 (10) |
Number of respondents
Percentage of respondents
Results provided by Mr. Steven Smith (ASTRO liaison to ARRO) and are quoted with the permission of ARRO.
Responses on consolidation of teaching were mixed. A significant number of educators reported that they already participated in consolidated teaching programs taught by either a single radiobiologist or a group of acknowledged experts. Other respondents replied that they would consider participation in regionally consolidated teaching efforts. However, a substantial number of educators responded that their programs were unlikely to participate in such regional efforts. Although 10% of the respondents reported that they now send their residents to a national review course, 64% said their programs were unlikely to do so.
DISCUSSION
This survey documents the aging of the faculty who have primary responsibility for teaching radiation biology to radiation oncology residents. In particular, the average age of the educators whose graduate training was in radiation biology is now estimated to be 58 years. Younger respondents tended to have Ph.D.s in areas only indirectly related to radiobiology, including molecular biology and cancer biology, or were M.D.s. If current trends continue, those directing radiobiology training in the future will likely be individuals with Ph.D. degrees in a variety of fields other than radiation biology and radiation oncologist physician-scientists.
The growing lack of educators with graduate training in radiation biology has implications beyond the training of radiation oncology residents. Radiology and nuclear medicine residents also require a background in the principles of radiation biology, as do radiographers, radiologic technologists, radiation therapists and medical dosimetrists. The ABR recently mandated that medical physicists in radiologic specialties complete a course in radiation biology to be eligible to sit for their written board certification exams. In addition, educators with expertise in radiobiology are needed in a variety of other venues ranging from radiation safety and regulatory affairs to emergency response and homeland security. The need for additional graduate programs providing training in radiation biology is therefore a issue that merits attention.
The North American radiation biology educators who responded to this survey generally placed a high priority on teaching and mentoring radiation oncology residents. Their responses to the survey suggest potential benefit from additional guidance in curriculum planning. One finding of concern was the lack of familiarity with several of the organizations that play major roles in setting policies for resident education and certification, including the ABR, ACGME and ACR. In particular, it is surprising that more than a quarter of the faculty with primary responsibility for teaching radiation biology to radiation oncology residents reported that they were not familiar with the guidelines provided by the ABR, since the topics outlined in that syllabus reflect the areas of radiobiology and cancer biology in which residents are expected to have received training and to be knowledgeable. (Inclusion of data from educators in Canadian programs, who might be less familiar with U.S. organizations, did not substantially affect the results of the survey; removal of their responses did not markedly change the overall pattern of response for any survey questions.) However, it should be recognized that the intent of the ABR syllabus and the accreditation process for residency training programs is not to homogenize teaching across all training programs. Educators can and should emphasize and expand upon subject matter that they view as particularly important or relevant.
Although an increasing number of people who have responsibility for teaching radiation biology to radiation oncology residents do not possess a degree in radiation biology or another radiation science, most of these individuals either performed coursework in radiation biology or participated in a radiobiology research project during their training. The majority use radiation in at least some of their research, even though they generally self-identified as, for example, molecular or cancer biologists, rather than as radiation biologists. Because fundamental concepts and the results of research in molecular and cancer biology have become increasingly relevant to the practice of clinical radiation oncology and represent an expanding portion of the material addressed on the board examinations, these individuals bring valuable expertise to resident education. However, their lack of formal training in many areas of radiation biology may present challenges as they organize and teach radiobiology courses.
Thus, a critical question for the radiation oncology community becomes: What teaching tools and/or other resources should be developed now to assist today's younger, predominantly non-radiobiologist educators, and the educators of the future, as the senior teaching faculty retire over the next 10-15 years?
One important educational tool that has already been developed is the RCB Study Guides. While geared mostly to the needs of radiation oncology residents preparing for the ABR written certification exam, this teaching resource has also proved useful for radiation biology educators. In the present survey, more than 80% of radiobiology instructors reported that they used this resource. A similar resource is the recently “repurposed” ACR annual In-Training exam that now serves as an educational aid as well as an instrument to evaluate resident educational progress (8, 11). This exam and an answer key (with answer justifications and pertinent references) are freely available from the ACR website 3-4 months after the exam is given.
Nearly all educators felt that it would be helpful to have a more detailed core curriculum that expanded on the outline provided by the current ABR syllabus. About 90% of the teachers would also be interested in having access to free or low cost educational materials provided by ASTRO, the ABR or ACR. Along those lines, consideration could be given to expanding tele-education resources, e.g., video-taped lectures from various experts available to accredited educators for their own education. If such materials are to be used directly by residents, however, on-site educators should ensure that residents are learning and understanding material appropriately. Three-quarters of the educators reported that they already used or would use guest lecturers with specific expertise to teach some topics in their courses. The majority of the respondents replied that they did or would consider participating in regional consolidated teaching efforts. It is unclear whether the programs that responded that they were unlikely to consider multi-institutional regionally consolidated courses were limited by geographical factors or whether this reflected institutional philosophy.
The options which garnered the least support among the respondents were those of hiring an outside educator to do most of the teaching and sending residents to a national review course. Several potential factors could account for this decision. First, outside educators are not on site continually, and therefore are not available to act as research mentors, participate routinely in journal clubs, seminars, conferences and other educational venues, or provide the important casual education and guidance that occurs outside the classroom. Also, the residency program must still meet the ACGME mandate of having a full-time radiation or cancer biologist on site. In addition, there are inherent limitations to the format of a national review course. Such a course would, of necessity, be condensed for presentation over at most a few days. This limits the depth of independent study that could be expected of students during the course. Moreover, for such a course to be cost-effective it would need to be given in a lecture format, with little time for questions or informal discussion. The design of such a course would therefore be non-optimal. Furthermore, refresher courses, didactic sessions and young investigator courses at or immediately preceding meetings of ASTRO, RRS, AACR and other scientific societies already provide some of the content that would comprise a national radiation biology course, providing alternative educational experiences that diminish the potential value of a national course in the eyes of many programs and program directors.
“Teach-the-teacher” short courses, whether stand alone, or associated with national meetings of radiation-related professional societies, have been proposed as a mechanism for training resident educators. However, given the inevitable time and financial constraints of the faculty, it seems likely that many educators would not be willing or able to justify attending such courses. This could be especially true for non-radiobiologists, as such courses would likely be associated with meetings of societies such as ASTRO or RRS, which may not be among the scientific meetings these researchers normally attend.
In conclusion, the declining numbers of radiobiologists has the potential to threaten the quality of the didactic radiation biology education that radiation oncology residents receive and could also affect research mentoring for residents. The RCB Study Guides, although principally geared to the needs of residents, appear to be beneficial to both residents and educators teaching radiobiology courses. Most current radiation biology educators agree however that additional resources directed specifically at educators, such as a more detailed description of the core curriculum expected of radiobiology/cancer biology courses for radiation oncology residents (that expands on the current outline in the ABR syllabus), would be of value. Consideration should also be given to the need for and utility of more comprehensive, albeit time-consuming and possibly expensive, educational resources such as downloadable, annotated slide presentations or other web based webinars and didactic materials. Finally, creation of new graduate programs in radiation biology should be seriously considered by medical schools and universities, with NIH providing funds to assist the endeavors. Such programs are needed to supply future educators for radiation oncology, radiology and nuclear medicine programs, as well as to supply the radiation biologists needed for many other areas including translational research related to radiation oncology and mitigation of radiation injuries, diagnostic imaging, regulatory affairs and homeland security.
Acknowledgement
This research was supported in part by an Education Core grant 5 U19 AI067733-03 from NIH/NIAID (JW)
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errorsmaybe discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of Interest Notification All authors teach in radiation and cancer biology courses for radiation oncology residents. All authors are editors of the ASTRO Radiation and Cancer Biology Practice Examination and Study Guides; they receive no financial compensation for their work on this examination or for their work related to the survey described in this report.
REFERENCES
- 1. http://www.theabr.org/RO_Study_Bio.htm.
- 2. http://www.acgme.org/acWebsite/downloads/RRC_progReq/430_radiation_oncology_01012009.pdf.
- 3.Hall EJ, Denekamp J. Residency training in radiation oncology; radiation biology and cancer biology. Int J Radiat Oncol Biol Phys. 1992;24:847–849. doi: 10.1016/0360-3016(92)90455-q. [DOI] [PubMed] [Google Scholar]
- 4.Coleman CN, Griffin TW, Prosnitz LR, et al. Training the radiation oncologist for the twenty-first century. Int J Radiat Oncol Biol Phys. 1996;35:821–826. doi: 10.1016/0360-3016(96)00208-8. [DOI] [PubMed] [Google Scholar]
- 5.Hussey DH, Sagerman RH, Halberg F, et al. Report of the 1997 SCAROP survey on resident training. Society of Chairmen of Academic Radiation Oncology Programs. Acad Radiol. 2000;7:176–183. doi: 10.1016/s1076-6332(00)80120-8. [DOI] [PubMed] [Google Scholar]
- 6.Radiation oncology training in the United States: Report from the Radiation Oncology Resident Training Working Group organized by the Society of Chairman of Academic Radiation Oncology Programs (SCAROP) Int J Radiat Oncol Biol Phys. 1999;45:153–161. doi: 10.1016/s0360-3016(99)00155-8. [DOI] [PubMed] [Google Scholar]
- 7.Coleman CN, Stone HB, Alexander GA, et al. Education and training for radiation scientists: radiation research program and American Society of Therapeutic Radiology and Oncology Workshop, Bethesda, Maryland, May 12-14, 2003. Radiat Res. 2003;160:729–737. doi: 10.1667/rr3096. [DOI] [PubMed] [Google Scholar]
- 8.Dynlacht JR, Zeman EM. Recent initiatives for radiation oncology resident education in radiation and cancer biology. Radiat Res. 2007;168:262–265. doi: 10.1667/rr0953.1. [DOI] [PubMed] [Google Scholar]
- 9.Zeman EM, Dynlacht JR, Rosenstein BS, et al. Toward a national consensus: Teaching radiobiology to radiation oncology residents. Int J Radiat Oncol Biol Phys. 2002;54:861–872. doi: 10.1016/s0360-3016(02)02968-1. [DOI] [PubMed] [Google Scholar]
- 10.Dynlacht JR, Dewhirst MW, Hall EJ, et al. Toward a consensus on radiobiology teaching to radiation oncology residents. Radiat Res. 2002;157:599–606. doi: 10.1667/0033-7587(2002)157[0599:tacort]2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 11.Paulino AC. Results and resident evaluation of the 2007 American College of Radiology in-training examination in radiation oncology. J Am Coll Radiol. 2008;5:1077–1079. doi: 10.1016/j.jacr.2008.04.006. [DOI] [PubMed] [Google Scholar]