Abstract
Allergy and asthma can reduce HRQOL as a result of profound physical and psychosocial complications. Most patients with asthma also suffer from rhinitis, which also impairs quality of life. However, the impact of allergic rhinitis on asthmatic patients has not been investigated.
Objective
To assess Quality of life (QOL) in asthmatic patients and assess relative burden of allergic rhinitis on asthmatics’ QOL.
Patients and Methods
we analysed HRQOL questionnaire (SF-36) answers of 219 patients (118 allergic rhinitis, 79 asthma and 22 asthma with allergic rhinitis) and controls (30 healthy individuals), in addition to analysis of questionnaire scores according to patients’ characteristic including gender, BMI and duration of symptoms. Moreover, pulmonary function test were done for all patients and control.
Results
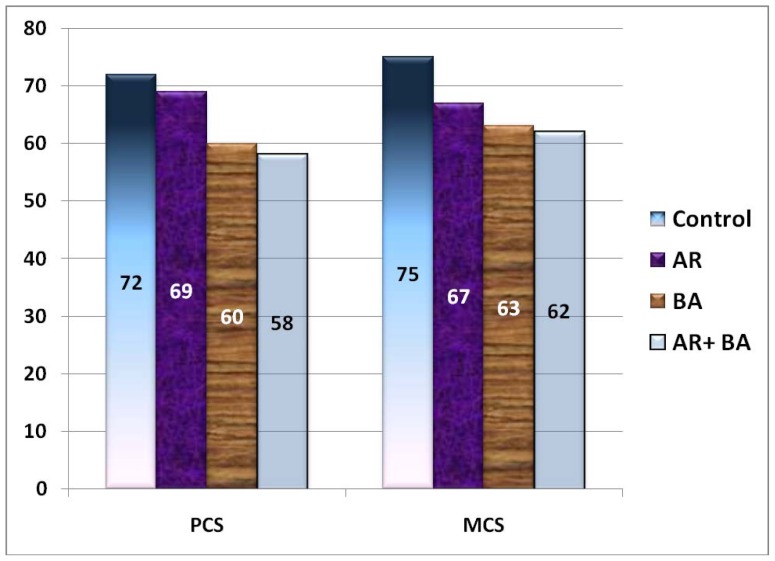
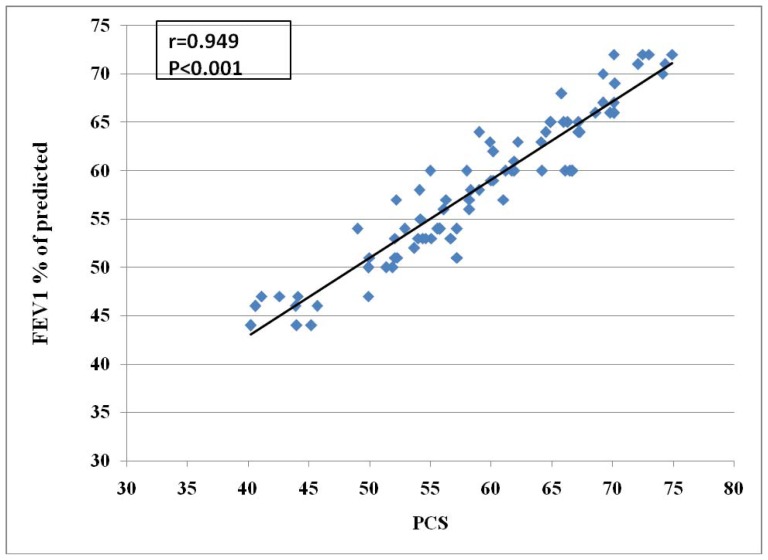
HRQOL parameters were significantly lower in females more than males and in patients with BMI>25 if compared with those with BMI<25. Moreover, HRQOL was significantly lower in all 3 patients’ groups if compared with control group (P<0.001) in all parameters except mental health and role emotional. Significantly higher scores (SF-36 sub-scales for physical functioning, role-physical, bodily pain) were found among allergic rhinitis patients compared with asthmatics with or without allergic rhinitis. Although, quality of life was worse in asthmatic patients compared to patients with rhinitis alone, no significant difference was found between asthmatics and those with both diseases. Both PCS and MCS scores are significantly lower in patients’ groups compared with the control (p<0.05). Asthmatic patients with or without rhinitis tended to have lower PCS and MCS scores than subjects with isolated allergic rhinitis, the difference between the groups was statistically significant only for PCS scores. Moreover, highly significant positive correlation between PCS score and FEV1 in asthmatics with or without allergic rhinitis was detected denoting that PCS score is markedly affected by severity of asthma. (r=0.949, P<0.001).
Conclusions
Allergic rhinitis has a limited role in reduction of HRQOL. HRQOL is markedly reduced in patients with asthma with or without rhinitis than in those with allergic rhinitis only; this could be related to the severity of asthma more than the presence of associated allergic rhinitis. These findings indicated that allergic rhinitis does not seem to further impair quality of life in subjects with asthma. We recommend that patients with bronchial asthma with or without allergic rhinitis in need of great help from physicians and social workers to improve their physical and mental health. Moreover, further studies with larger populations and longer duration are needed in order to determine the extent to which asthma and rhinitis comorbidities are associated in HRQOL.
Keywords: asthma, allergic rhinitis, HRQOL, SF-36 questionnaire
Introduction
Interest in research into the quality of life has been increasing over the last 20 yr but this field is still disregarded by some. However, it is now widely acknowledged that the personal burden of illness, as perceived by the patient, cannot be fully assessed by objective measures of disease severity, because for diseases such as asthma and allergic rhinitis, traditional clinical indices only moderately correlate with how patients feel and are able to function on a daily basis. (1)
Health-related quality of Life (HRQOL) has been considered an important variable to be managed in airway diseases. Allergy and asthma can reduce HRQOL as a result of profound physical and psychosocial complications. Most patients with asthma also suffer from rhinitis, which also impairs quality of life. However, the impact of allergic rhinitis on asthmatic patients has not been investigated. (2) Allergy and asthma are very common conditions that are recognized as causes of reduced quality of life. It was not until the early 1990s, however, that HRQOL questionnaires were introduced into the study and management of asthma and rhinitis. (3, 4) Both diseases share key elements of pathogenesis and are usually considered different manifestations of the same underlying atopic state. (5) Asthmatic symptoms lead to impairment in the physical, emotional, and social aspects of a patient’s life. Likewise, in allergic rhinitis, allergic and non nasal symptoms from allergen exposure result in difficulties. Both physical and mental health measures have been found to be adversely affected in patients with allergic rhinitis, in a population-based study. (6) Although clinical and experimental studies suggest that upper respiratory tract dysfunction may affect the lower airways, rhinitis has not been explored thoroughly as a potential risk factor for HRQOL impairment in asthma.
To date we have available specific instruments assessing health-related quality of life (HRQL) in rhinoconjunctivitis or in asthma, but not instruments evaluating rhinitis and asthma together, although they often coexist. (2, 7)
Asthma-specific quality-of-life questionnaires have been developed to quantify, the effects of asthma on the patient’s daily life and well being, and the extent to which a given treatment reduces these effects. (8)Disease-specific quality-of-life questionnaires have also been developed for allergic rhinitis. (9)Allergic rhinitis and asthma very often coexist in the same patients and both diseases impair quality of life. However, very few studies have assessed the health-related quality of life of individuals with asthma or allergic rhinitis at the population level, and the relative burden of these two diseases has not been investigated.
The interest in this point could be helpful to correct the drawbacks of these diseases on quality of life. This could lead to improvement in compliance with therapy to help in disease control and in turn improvement of the quality of life.
Objective
To assess Quality of life (QOL) in asthmatic patients and assess relative burden of allergic rhinitis on asthmatics’ QOL.
Patients and methods
This was a prospective study of 219 patients enrolled from among 290 initially attended outpatient clinic of Qassim University; eligible patients were diagnosed with either disease (allergic rhinitis/asthma) or both, In addition to 30 healthy individuals as control group. The protocol for this study was approved by the university ethics committee, and all patients gave their informed consent.
We excluded any cases suffered from any other illness which could affect the quality of life (e.g: neurological diseases, psychiatric disorders, renal failure etc).
Study Design
We evaluated HRQOL in patients with allergic rhinitis (118 patients), with asthma only (79 patients), and those with rhinitis and concomitant asthma (22 patients). Demographic data of the study groups were collected. A diagnosis of asthma was made according to GINA guidelines update 2009. (10) Rhinitis was diagnosed if any symptoms of rhinorrhea, nasal obstruction or itching, or sneezing were documented. (6). Independent variables examined were age, gender, body mass index (BMI), and duration of symptoms.
The BMI was calculated by dividing the weight in kilograms by the square of the height in meters.
All cases were subjected to the following
full history including history suggestive of allergic rhinitis(nasal congestion, rhinorrhea, sneezing, pruritis, and post nasal discharge), history suggestive of bronchial asthma (paroxysmal dyspnea, wheezes, cough, triggering factors etc)
Thorough clinical examination
Pulmonary function test (spirometric study) to assess the severity of airway obstruction.
Including:
Forced expiratory volume in 1st second FEV1
Forced vital capacity FVC
FEV1/FVC
Forced expiratory flow: FEF25-75
All patients completed short form questionnaire 36 (SF-36). The SF-36 questionnaire is based on the Medical Outcome Study survey. It comprises 36 items which are combined to measure eight concepts:
Physical functioning.
Limitations due to physical problem.
Bodily pain
General health
Vitality
Social functioning
Limitations due to emotional problem
Mental health
In addition to the 8 separate scales, 2 general domain measures were used to provide summary scores: the physical component summary (PCS) and the mental component summary (MCS). Higher scores represent better health status. The general health perceptions scale of the SF-36 questionnaire is multidimensional and represents multiple aspects of health perceptions.
We used the three-step scoring system to calculate the values for the concepts from the questionnaire items as described in the SF-36 manual and interpretation guide.
Statistical analysis
Statistical analysis was performed using SPSS statistical software, version 10.0 (SPSS Inc, Chicago, Illinois, USA). Differences between qualitative variables were studied by means of the χ2 test. For the normally distributed quantitative variables one-way analysis of variance (ANOVA) was used to compare results. Continuous variables were described as means (SD). Multivariate ANOVA was performed with the post-hoc Bonferroni correction for multiple comparisons of age, duration of symptom(s), PCS, and MCS as well as scores on the 8 SF-36 domains.
Statistical significance was set at P <0.05.
Results
Characteristics of the 219 patients are summarized in (Table 1). Females predominated and ages ranged from 14 to 59 years. Most of the patients were diagnosed with allergic rhinitis, followed by asthma alone then both diseases together with female predominance in all groups.
Table (1).
Characteristics of the study groups
| Allergic rhinitis | Asthma | Allergic rhinitis+ asthma | Control | P wave | |
|---|---|---|---|---|---|
| n=118 | n=79 | n=22 | n=30 | ||
|
| |||||
| Age M±SD | 26±12.1 | 32±15.2 | 37±9.1 | 34±8.6 | <0.001♦ |
|
| |||||
| Sex n (%) | |||||
| Male | 31(26.3%) | 23(29.1%) | 8(36.4%) | 10(33.3%) | |
| Female | 87(73.7%) | 56(70.9%) | 14(63.6%) | 20(66.7%) | |
|
| |||||
| Duration of symptoms SD,y | 6.2±3.5 | 7.2±6.2 | 8.3±7.1 | ------------- | NS |
|
| |||||
| BMI Kg/m2 | 23.4(4) | 26.1(5.1) | 26.7(4.3) | 23.1(2.3) | <0.001* |
| <25 n (%) | 70(59.3%) | 41(51.9%) | 9(40.9%) | 8(26.7%) | |
| >25 n (%) | 48(40.7% | 38(48.1%) | 13(59.1%) | 22(73.3%) | |
significant p<0.05 allergic rhinitis vs other patients groups and control
significant p<0.05 allergic rhinitis and control on one hand vs other asthmatic patients with or without allergic rhinitis
Patients with allergic rhinitis alone were significantly younger (p<0.001).
Duration of symptoms was significantly lower in allergic rhinitis group if compared to those with both allergic rhinitis and asthma (p=0.03). Asthmatic patients with or without allergic rhinitis tended to be overweight (BMI ≥ 25 kg/m2) especially if compared with patients with allergic rhinitis only (P < 0.001).
In this study, half of the HRQOL parameters (physical functioning, role physical, bodily pain, social functioning) were significantly lower in patients with BMI>25 if compared with those with BMI<25. Moreover, most of HRQOL parameters were highly significantly lower in females than in males (P<0.001) except mental health which is only significantly lower (<0.05) and no difference in role emotional.
HRQOL was significantly lower in all 3 patients’ groups if compared with control group (P<0.001) in all parameters except mental health and role emotional.
As regard the 3 patients’ groups HRQOL was significantly different between the 3 groups, except for the role-emotional SF-36 domain. Significantly higher scores (SF-36 sub-scales for physical functioning, role-physical, bodily pain) were found among allergic rhinitis patients compared with asthmatic with or without allergic rhinitis. Although, quality of life was worse in asthmatic patients compared to patients with rhinitis alone, no significant difference was found between asthmatics and those with both diseases. Mean scores on the SF-36 sub-scales for physical functioning, role-physical, bodily pain and role-emotional were slightly lower for patients with both diseases than for asthmatic patients, but the difference was not significant (Table 2).
Table (2).
Mean SF36 scores±SD according to the subjects’ characteristics
| Physical functioning | Role physical | Bodily pain | General health | Vitality | Social functioning | Mental health | Role emotional | |
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Allergic rhinitis | 83±18 | 64±37 | 70±23 | 56±20 | 56±22 | 75±27 | 64±23 | 70±37 |
|
| ||||||||
| Asthma | 71±20 | 49±42 | 61±21 | 53±22 | 51±21 | 69±23 | 62±22 | 72±38 |
|
| ||||||||
| Allergic rhinitis +asthma | 70±23 | 39±41 | 59±27 | 52±23 | 50±21 | 69±22 | 60±21 | 60±43 |
|
| ||||||||
| Control | 94±10 | 92±20 | 85±21 | 82±17 | 70±18 | 92±11 | 70±28 | 72±14 |
|
| ||||||||
| P value | <0.001• | <0.001• | <0.01• | NS | NS | NS | NS | NS |
|
| ||||||||
| Sex | ||||||||
| Male | 85±12 | 72±23 | 75±21 | 59±32 | 61±26 | 77±20 | 65±23 | 71±35 |
| Female | 72±11 | 51±26 | 60±23 | 51±25 | 49±24 | 69±22 | 58±24 | 60±30 |
| P value | <0.001 | <0.001 | <0.001 | 0.036 | <0.001 | 0.008 | 0.035 | 0.07 |
|
| ||||||||
| BMI | ||||||||
| <25 | 84±21 | 66±38 | 70±25 | 58±16 | 57±20 | 76±21 | 65±18 | 72±31 |
| >25 | 70±22 | 52±40 | 63±24 | 54±13 | 53±22 | 66±23 | 60±20 | 64±33 |
| P value | <0.001 | 0.009 | 0.04 | 0.052 | 0.16 | 0.001 | 0.55 | 0.069 |
significant p<0.05 allergic rhinitis Vs asthmatic patients with or without allergic rhinitis
Both PCS and MCS scores are significantly lower in patients’ groups compared with the control (p<0.05). Asthmatic patients with or without rhinitis tended to have lower PCS and MCS scores than subjects with isolated allergic rhinitis, the difference between the groups was statistically significant only for PCS scores (Fig 1).
Fig. (1).
Physical component summary (PCS) and mental component summary (MCS) health related quality of life scores in patients and control
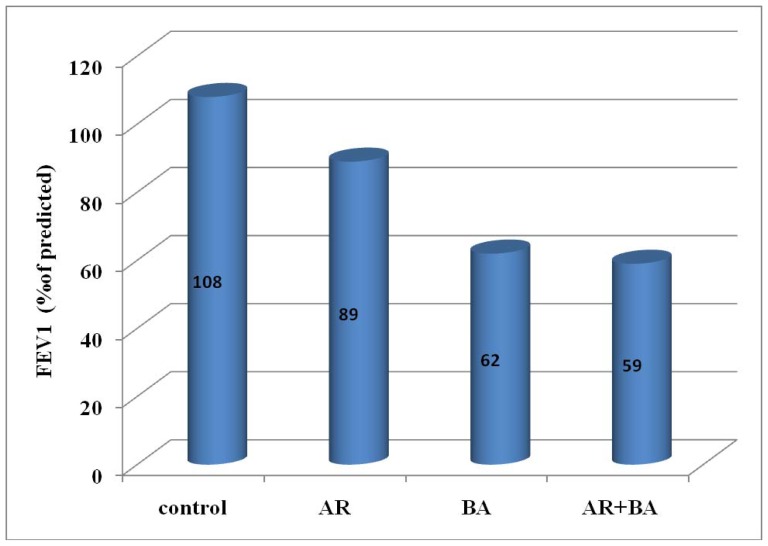
Pulmonary function tests revealed obstructive pulmonary dysfunction in asthmatics with or without allergic rhinitis, mean while, in allergic rhinitis alone no significant difference was found between them and controls. In allergic rhinitis we found lower FEF25-27 than those of controls (p=0.59). Mean values of FEV1 were significantly lower in asthmatic patients with or without allergic rhinitis compared with those in controls and in patients with allergic rhinitis (fig 2). Moreover, highly significant positive correlation between PCS score and FEV1 in asthmatics with or without allergic rhinitis was detected denoting that PCS score is markedly affected by severity of asthma. (r=0.949, (P<0.001) (fig 3).
Fig. (2).
Mean values of FEV1 in all groups
Fig. (3).
Correlation between PCS values and FEV1 (% of predicted) in asthmatic patients with or without allergic rhinitis
Discussion
Over the last decade, the united airway concept has indicated significant similarities between rhinitis and asthma and influenced ideas about their pathophysiology. This concept is based on the following observations: 1- Allergic rhinitis and comorbid asthma exhibit similar four-stage allergic responses (sensitization, acute-phase mast-cell activation, acute-phase neuronal response, late-phase response) that correlate with clinical signs/symptoms. (11) Some patients present with allergic rhinitis and subclinical asthma; other patients manifest both conditions, with rhinorrhea, nasal congestion, sneezing, tightness in the chest and coughing, and spirometric evidence of reversible bronchospasm. 2-Allergic rhinitis and asthma share common mechanisms for the airway inflammatory process. The mediators and triggers involved produce mucosal edema, inflammation, excessive mucus production, and airway constriction.(12, 13) In patients with both allergic rhinitis and allergic asthma, clinical data suggest that the effective treatment of allergic rhinitis can reduce the severity or frequency of flare-ups of allergic asthma. (13, 14, 15) Therefore, the united airways concept calls for a special approach to the management of these diseases. (16, 17)
HRQOL is a major outcome in both asthma and rhinitis. (18, 19) Asthma represents a global health problem because it interferes with psychological well-being and activities of daily living and affects social as well as economic outcomes. (20) There is a growing awareness of how allergy and asthma can affect patients’ quality of life, work or school performance, and emotional well-being. Besides physical symptoms, patients may exhibit fatigue, psychomotor sluggishness, irritability, and mood and cognitive disturbances. This combination of physical, emotional, and functional problems may diminish HRQOL. However, the impact of rhinitis on HRQOL in asthma has rarely been investigated, (21) a situation that led to the design of our study.
In agreement with Leynaert et al. (2000), (1) we found that patient with allergic rhinitis suffer from signicantly lower quality of life if compared with control. Further impairment was noticed in asthmatic patients with or without allergic rhinitis.
In this work, we found significant difference between the three groups of patients in most of SF-36 questionnaire domains, except for the role-emotional SF-36 domain. Significantly higher scores were found among allergic rhinitis patients. Although, quality of life was impaired in allergic rhinitis patients and it was worse in asthmatic patients compared to patients with rhinitis alone, no significant difference was found between asthmatics and those with both diseases. These results indicate that allergic rhinitis does not seem to further impair quality of life in subjects with asthma.
Asthmatic subjects (with or without allergic rhinitis) had significantly greater impairment in physical measures whereas mental health scores in patients with isolated allergic rhinitis were nearly similar to those of asthmatic subjects. Previous studies (2, 22) results were in consistent with our results as regard the PCS results whereas mental health scores in patients with isolated allergic rhinitis were lower than those of asthmatic subjects in their studies. Moreover, we found that reduced PCS is significantly correlated with the severity of asthma as assessed by FEV1 level as previously stated. (1, 23, 24)
In concordance with Leynaert and co workers, (1) individual analysis revealed that older age and longer duration of symptoms considered as risk factors for reduced HRQOL, particularly in patients with both asthma and allergic Rhinitis, as they were the oldest group with the longest duration of symptoms. Moreover, Patients with a BMI less than 25 kg/m2 were shown to have better SF-36 scores in all domains that also add another risk factor for reduction in HRQOL in asthmatics as they had higher BMI if compared with other groups. (25, 26)
In conclusion, Allergic rhinitis has a limited role in reduction of HRQOL. HRQOL is markedly reduced in patients with asthma with or without rhinitis than in those with allergic rhinitis only; this could be related to the severity of asthma more than the presence of associated allergic rhinitis. These findings indicated that allergic rhinitis does not seem to further impair quality of life in subjects with asthma. We recommend that patients with bronchial asthma with or without allergic rhinitis in need of great help from physicians and social workers to improve their physical and mental health. Moreover, further studies with larger populations and longer duration are needed in order to determine the extent to which asthma and rhinitis comorbidities are associated in HRQOL.
Acknowledgement
We acknowledge deanship of scientific research for sponsoring this research. Also, we acknowledge students Reem Al-Salamah, Najla Al-Sowayan, Taghreed Al-Mutairi for their great help.
References
- 1.Leynaert B, Neukirch C, Liard R, et al. Quality of life in allergic rhinitis and asthma. Am J Respir Crit Care Med. 2000;162(4):1392–1396. doi: 10.1164/ajrccm.162.4.9912033. [DOI] [PubMed] [Google Scholar]
- 2.Kalpaklioğlu AF, Baççioğlu A. Evaluation of quality of life: impact of allergic rhinitis on asthma. J Investig Allergol Clin Immunol. 2008;18(3):168–73. [PubMed] [Google Scholar]
- 3.van Wijk RG. Quality of life, should we bother? Allergy. 2003;58:284–6. doi: 10.1034/j.1398-9995.2003.00108.x. [DOI] [PubMed] [Google Scholar]
- 4.Fokkens W, van Drunen CM. Nose and lung, two of a kind? Allergy. 2006;61:653–5. doi: 10.1111/j.1398-9995.2006.01169.x. [DOI] [PubMed] [Google Scholar]
- 5.Leynaert B, Bousquet J, Neukirch C, Liard R, Neukirch F. Perennial rhinitis: an independent risk factor for asthma in nonatopic subjects: results from the European Community Respiratory Health Survey. J Allergy Clin Immunol. 1999;104:301–4. doi: 10.1016/s0091-6749(99)70370-2. [DOI] [PubMed] [Google Scholar]
- 6.Bousquet J, Van Cauwenberge P, Khaltaev N the ARIAWorkshop Group. Allergic rhinitis and its impact on asthma. J Allergy Clin Immunol. 2001;108(5 Suppl):S147–334. doi: 10.1067/mai.2001.118891. [DOI] [PubMed] [Google Scholar]
- 7.Baiardini I, Pasquali M, Giardini A, et al. Rhinasthma: a new specific QoL questionnaire for patients with rhinitis and asthma. Allergy. 2003;58(4):289–94. doi: 10.1034/j.1398-9995.2003.00079.x. [DOI] [PubMed] [Google Scholar]
- 8.The Allergy report. The American Academy of Allergy. Asthma&Immunology. 2000 [Google Scholar]
- 9.Flemons W, Tsai W. Quality of life consequences of sleep- disordered breathing. J Allergy Clin Immunol. 1997;99:S750–756. doi: 10.1016/s0091-6749(97)70123-4. [DOI] [PubMed] [Google Scholar]
- 10.Global strategy for asthma management and prevention (updated 2005) Global Initiative for Asthma (GINA); 2009. URL: http://www.ginasthma.org. [Google Scholar]
- 11.Bousquet J, van Cauwenberge P, Khaltaev N for the ARIA Workshop/World Health Organization. Allergic rhinitis and its impact on asthma. J Allergy Clin Immunol. 2001;108:S147–336. doi: 10.1067/mai.2001.118891. [DOI] [PubMed] [Google Scholar]
- 12.American Academy of Allergy Asthma and Immunology (AAAAI) Allergic Disorders: Promoting Best Practices-The Allergy Report. 2000. [Accessed Mar 30, 2001]. [online]. Available from http://theallergyreport.com/, http://TheAllergyReport.com.
- 13.Simons FER. Allergic rhinobronchitis: the asthma-allergic rhinitis link. J Allergy Clin Immunol. 1999;104:534–40. doi: 10.1016/s0091-6749(99)70320-9. [DOI] [PubMed] [Google Scholar]
- 14.Fireman P. Rhinitis and asthma connection: management of coexisting upper airway allergic diseases and asthma. Allergy Asthma Proc. 2000;21:45–54. doi: 10.2500/108854100778248935. [DOI] [PubMed] [Google Scholar]
- 15.Schoenwetter William F, Dupclay Leon, Jr, Appajosyula Sireesh, Botteman Marc F, Pashos Chris L. Economic Impact and Quality-of-Life Burden of Allergic Rhinitis. Curr Med Res Opin. 2004;20(3) doi: 10.1185/030079903125003053. [DOI] [PubMed] [Google Scholar]
- 16.Cruz AA. The ‘united airways’ require a holistic approach to management. Allergy. 2005;60:871–4. doi: 10.1111/j.1398-9995.2005.00858.x. [DOI] [PubMed] [Google Scholar]
- 17.Harmsen L, Nolte H, Backer V. The effect of generalist and specialist care on quality of life in asthma patients with and without allergic rhinitis. Int Arch Allergy Immunol. 2010;152(3):288–94. doi: 10.1159/000283041. [DOI] [PubMed] [Google Scholar]
- 18.Chen H, Katz PP, Eisner MD, Yelin EH, Blanc PD. Health-related quality of life in adult rhinitis: The role of perceived control of disease. J Allergy Clin Immunol. 2004;114:845–50. doi: 10.1016/j.jaci.2004.07.008. [DOI] [PubMed] [Google Scholar]
- 19.Blaiss MS. Outcome’s analysis in asthma. JAMA. 1997;278:1874–80. [PubMed] [Google Scholar]
- 20.Van Cauwenberg P. Advances in allergy management. Allergy. 2002;57:29–36. doi: 10.1034/j.1398-9995.57.s75.6.x. [DOI] [PubMed] [Google Scholar]
- 21.Laforest L, Bousquet J, Pietri G, Kocevar VS, Yin D, Pacheco Y, Ganse EV. Quality of life during pollen season in patients with seasonal allergic rhinitis with or without asthma. Int Arch Allergy Immunol. 2005;136:281–6. doi: 10.1159/000083955. [DOI] [PubMed] [Google Scholar]
- 22.European Academy of Allergology and Clinical Immunology. The impact of allergic rhinitis on quality of life and other airway diseases: summary of a European conference. Allergy. 1998;53:S1–31. [PubMed] [Google Scholar]
- 23.Bousquet J, Knani J, Dhivert H, Richard A, Chicoye A, Ware JE, Michel F-B. Quality of life in asthma: I. Internal consistency and validity of the SF-36 questionnaire. Am. J. Respir. Crit Care Med. 1994;149:371–375. doi: 10.1164/ajrccm.149.2.8306032. [DOI] [PubMed] [Google Scholar]
- 24.Bousquet J, Bullinger M, Fayol C, Marquis P, Valentin B, Burtin B. Assessment of quality of life in patients with perennial allergic rhinitis with the French version of the SF-36 Health Status Questionnaire. J. Allergy Clin Immunol. 1994;94:S182–188. doi: 10.1016/0091-6749(94)90038-8. [DOI] [PubMed] [Google Scholar]
- 25.Kalpaklioglu AF, Kara T, Kurtipek E, Saygun M. Effect of body mass index on quality of life in allergic/asthmatic patients. Allergy Asthma Proc. 2006;27:499–503. doi: 10.2500/aap.2006.27.2909. [DOI] [PubMed] [Google Scholar]
- 26.Ford ES, Mannino DM, Redd SC, Moriarty DG, Mokdad AH. Determinants of quality of life -among people with asthma: findings from the Behavioral Risk Factor Surveillance System. J Asthma. 2004;41:327–36. doi: 10.1081/jas-120026090. [DOI] [PubMed] [Google Scholar]