Abstract
Background
The median orthopedic surgery wait time in Canada is 33.7 weeks, thus alternative treatments for pathologies such as lumbar disc herniations (LDH) are needed. We sought to determine whether transforaminal epidural steroid injections (TFESIs) alleviate or merely delay the need for surgery.
Methods
We retrospectively reviewed the charts of patients with LDH who received TFESIs between September 2006 and July 2008. Patient demographics, level and side of pathology, workers’ compensation status, levels injected, treatment outcome and time from referral to treatment were evaluated. The primary outcome measure was the need for versus the avoidance of surgery.
Results
We included 91 patients in our analysis. Time from family physician referral to injection was 123 (standard deviation [SD] 88) days; no significant differences in wait times were found between TFESI patients and those requiring surgery. In all, 51 patients (22 women, 29 men) with a mean age of 45.8 (SD 10.2) years avoided surgery following TFESI, whereas 40 patients (16 women, 24 mean) with a mean age of 43.1 (SD 12.0) years proceeded to surgery within 189 (SD 125) days postinjection. In all, 15 patients received multiple injections, and of these, 9 did not require surgical intervention. Age, sex and level/side of pathology did not influence the treatment outcome. Workers’ compensation status influenced outcome significantly; these patients demonstrated less benefit from TFESI.
Conclusion
Transforaminal epidural steroid injections are an important treatment tool, preventing the need for surgery in 56% of patients with LDH.
Abstract
Contexte
Le temps d’attente médian pour une chirurgie orthopédique au Canada est de 33,7 semaines. Il faut donc trouver des traitements de rechange pour certaines pathologies, telles que les hernies lombaires. Nous avons voulu déterminer si les infiltrations épidurales de corticostéroïdes par voie transforaminale (IECTF) procurent un soulagement ou ne font que retarder le recours à la chirurgie.
Méthodes
Nous avons analysé rétrospectivement les dossiers de patients souffrant d’hernie lombaire qui ont été soumis à des IECTF entre septembre 2006 et juillet 2008. Nous avons tenu compte des caractéristiques démographiques des patients, de l’ampleur et de la latéralité de la pathologie, du statut à l’égard des indemnités pour accidents du travail, des doses injectées, des résultats du traitement et du délai entre la consultation et le traitement. Le paramètre principal était le recours ou non à la chirurgie.
Résultats
Nous avons inclus 91 patients dans notre analyse. Le délai entre la demande de consultation par le médecin de famille et l’administration de l’infiltration a été de 123 (écart-type [ET] 88) jours; aucune différence significative quant au temps d’attente n’a été observée entre les patients soumis à l’IECTF et les patients soumis à la chirurgie. En tout, 51 patients (22 femmes, 29 hommes) âgés en moyenne de 45,8 (ET 10,2) ans ont évité la chirurgie après l’IECTF, tandis que 40 patients (16 femmes, 24 hommes) âgés en moyenne de 43,1 (ET 12,0) ans ont subi une chirurgie dans les 189 (ET 125) jours suivant l’injection. En tout, 15 patients ont reçu plusieurs infiltrations; parmi eux, 9 n’ont pas eu besoin d’une intervention chirurgicale. L’âge, le sexe, l’ampleur et la latéralité de la pathologie n’ont exercé aucune influence sur les résultats du traitement. Le statut à l’égard des indemnités pour accidents du travail a eu une influence significative sur les résultats. Ces patients semblent avoir moins bénéficié des IECTF.
Conclusion
Les infiltrations épidurales de corticostéroïdes par voie transforaminale sont un outil thérapeutique important et préviennent le recours à la chirurgie chez 56 % des patients qui souffrent d’hernie lombaire.
Lumbar disc herniation (LDH) is a common spinal pathology. Fortunately, most patients with lower extremity radiculitis and/or radiculopathy will note symptom resolution without surgical intervention(s), whereas each year 1%–3% of patients will require surgical intervention.1 In the United States, 287 122 patients underwent a discectomy procedure in 2002.2 Over time, surgical rates have remained remarkably stable and have been proven comparable across developed nations, including Canada, depending on physician population ratios.2–5
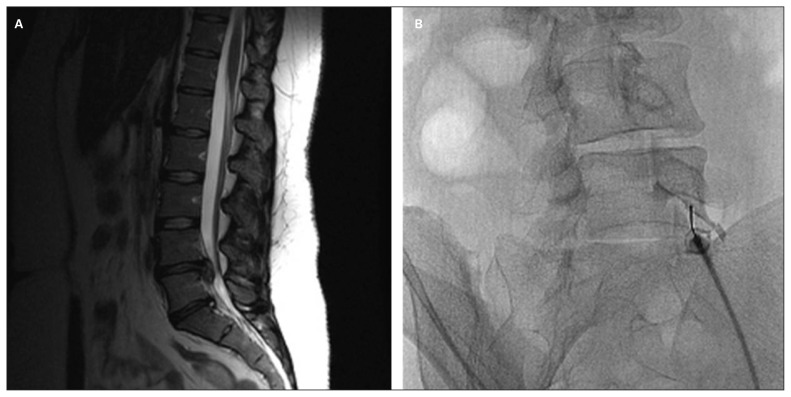
An often used adjunct to nonsurgical treatment is transforaminal epidural steroid injection (TFESI) or selective nerve root injection (Fig. 1). Focused placement of steroid medication at the injured nerve root addresses the specific pathophysiologic changes incurred owing to the disc herniation.6,7 Several studies have demonstrated the benefit of TFESI in treating radicular symptoms secondary to LDH.8–10 The success of TFESI compared with other injection techniques has also been demonstrated.11–13
Fig. 1.
(A) Sagittal view magnetic resonance imaging scan demonstrating L4/5 disc herniation. (B) Perineural injection of iohexol confirming L5 nerve root location.
To date, the literature on the use of TFESI to treat radicular symptoms has focused on early intervention.14 Outcomes with early intervention have been favourable, with improvement or resolution of pain and/or neurologic abnormality.6,15,16 The early timing prevents chronicity of nerve root injury, but will include some patients who would have realized symptom relief despite the TFESI if given additional time. Furthermore, the number of patients who require surgery even after treatment with TFESI is rarely reported.8
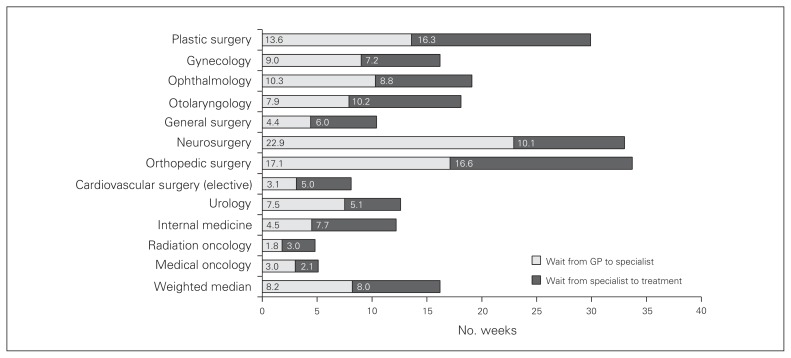
In Canada, a publicly funded care model ensures that all citizens receive high-quality health care.2,17 Unfortunately, resource allocation issues create wait times that have become formidable. The median wait time from referral is 33.7 weeks for orthopedic surgery and 33.0 weeks for neurosurgery.18 Both are concerningly long, even in comparison to other Canadian surgical specialties (Fig. 2). Relatively less severe pathologies, such as disc herniations, are further delayed to ensure timely management of more serious or emergent conditions. This delay in treatment can introduce harm to the patient, as symptoms become chronic and more resistant to manage; chronicity affects mood, fatigue, employability and social functioning.19–24 This environment demands an effort to find alternate treatment techniques to alleviate the need for surgery. Successful nonsurgical treatment should reduce surgical wait times and costs to an overburdened health care system. Transforaminal epidural steroid injection has proven to be an effective early intervention for lower extremity radiculitis and/or radiculopathy secondary to LDH, but its effectiveness is unproven in patients demonstrating more longstanding symptoms.
Fig. 2.
Median wait times (2009) from referral by a general practitioner (GP) to treatment grouped by specialty. Provided by The Fraser Institute’s National Waiting List Survey, 2009 (www.fraserinstitute.org/).
Our objective was to assess the effectiveness of TFESI in alleviating the need for surgical intervention in patients with lower extremity radiculitis and/or radiculopathy secondary to LDH and to determine which patient characteristics influence the injection outcome.
Methods
An audit of procedural referrals and scheduling within the Department of Diagnostic Imaging was cross-referenced to a prospective databank within the office of the principal investigator (N.A.M.) to identify patients who received a TFESI for an LDH and those who received surgical intervention. We retrospectively assessed the demographic and clinical characteristics and the outcomes of patients treated for an LDH between September 2006 and July 2008. Our institution’s research ethics board approved the study protocol.
To be included in the study, patients must have received a diagnosis of LDH causing lower extremity radiculitis and/or radiculopathy confirmed by clinical and radiologic evaluation, must have failed nonoperative measures and must have been surgical candidates. The patients’ clinical history confirmed radiculitis (subjective pain severity or dysesthesia) and functional compromise. Clinical examination confirmed radiculopathy (signs of neurologic dysfunction, including abnormalities of sensation, reflex, motor or gait, with associated nerve tension signs). Magnetic resonance imaging confirmed corroborating anatomic pathology. We considered nonoperative measures to have failed in patients who reported persistent and intolerable symptoms after a minimum of 6 weeks of treatment with a combination of medications, activity modification, physical therapy or other ancillary care. Patients who had failed nonoperative measures and had requested to proceed with surgical intervention owing to persistence of symptoms were considered to be surgical candidates if they were psychologically and physiologically able to tolerate surgery.
In patients meeting the inclusion criteria, TFESI was offered as a nonoperative option before surgery.25
All TFESIs were completed by 1 of 4 interventional radiologists. All were subspecialty-trained interventionists and used standard injection techniques. Perineural placement of triamcinalone (40 mg) and 0.25% bupivicaine (1 mL) was performed after identification of the target nerve root using fluoroscopic guidance with a preliminary injection of 1–2 mL of iohexol, accompanied by reproduction of radicular pain. An intervention involved TFESI at the offending root(s) discerned by imaging, physical findings and symptoms. If symptoms returned after successful resolution following the first intervention, patients were offered a second intervention; a second intervention was not provided if patients reported no change in symptoms after the first one.26
Patients were instructed to start a physical therapy program 48 hours after receiving the TFESI. Physical therapy encompassed patient education, methods to control pain, core strengthening, lumbopelvic stabilization and a home exercise program. Therapy was not standardized across patients. Reassessment occurred 6 weeks after the TFESI.
No formal scoring or criteria confirmed or graded TFESI success, the need for repeat TFESI or the need for surgery. Success was subjectively reported by the patient and was graded via threshold: satisfied patients chose not to proceed with their surgical request, whereas dissatisfied patients proceeded to surgery (microdiscectomy). Initially satisfied patients whose conditions then worsened were offered a second TFESI.
A statistical power calculation with α = 0.05 confirmed that the avoidance of surgery in 30% of the patient population (an effect size of 0.30) would validate the efficacy of the TFESI intervention for a sample size of 90 patients. The primary outcome measure was the avoidance of surgical intervention. Secondary measures were patient demographic characteristics (age, sex), workers’ compensation status, side and level of pathology, location of TFESI and time from symptom onset to treatment. We assessed these secondary measures to determine if any patient characteristics influenced the injection outcome.
Statistical analysis
We calculated means and standard deviations (SD) for age, time from symptom onset to referral, time from referral to diagnosis, time from diagnosis to injection, time from injection to surgery and time from referral to alleviation of symptoms. A 1-way analysis of variance (ANOVA) was used to compare surgical and nonsurgical groups for all continuous variables. A Pearson χ2 test was used to examine the following variables for the primary surgical outcome: sex, side of pathology, injecting physician and workers’ compensation status. We considered results to be significant at p < 0.05. All data were analyzed using Minitab version 15 (Minitab Inc.).
Results
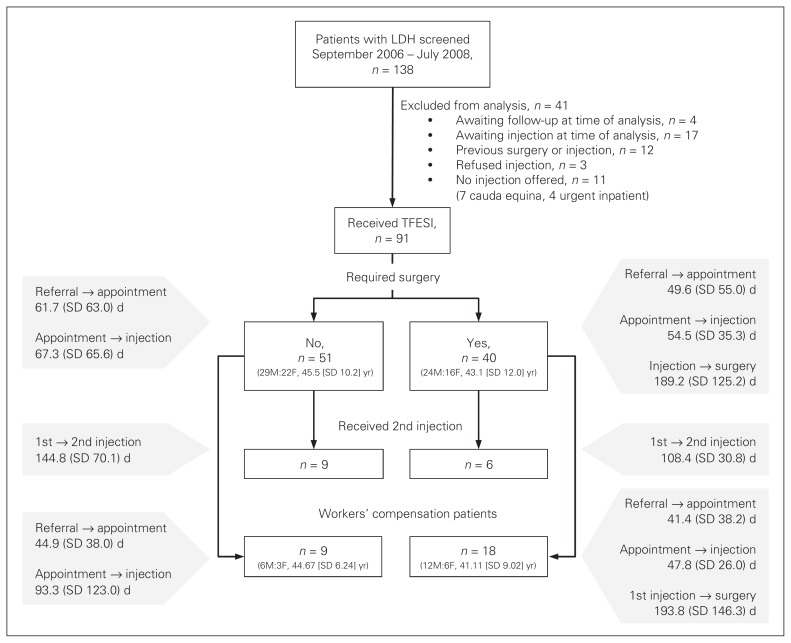
Between September 2006 and July 2008, 138 consecutive patients received the diagnosis of LDH causing lower extremity radiculitis and/or radiculopathy. Of these, 41 patients were excluded from analysis for the following reasons: awaiting injection or awaiting follow-up at the time of analysis (n = 21), previous surgery or injection (n = 12), or patient refused injection (n = 3). Eleven patients were not offered the option of TFESI owing to cauda equina (n = 7) or urgent inpatient admission (n = 4; Fig. 3).
Fig. 3.
Summary of variables and their association with primary (surgical requirement) and secondary (workers’ compensation status, demographic characteristics) outcomes. LDH = lumbar disc herniation; SD = standard deviation;TFESI = transforaminal steroid injection.
The remaining 91 patients (38 women and 53 men with a mean age of 44.6 [SD 11.0] yr) all received TFESI. Disc herniation predominated at the L4–5 or L5–S1 vertebrae; the herniations of 85 (93%) patients were identified at these 2 levels. Table 1 summarizes patient demographic and clinical characteristics.
Table 1.
Demographic and clinical characteristics of patients receiving transforaminal epidural steroid injections
| Characteristic | Group, mean (SD)* | p value | |
|---|---|---|---|
| No surgery | Surgery | ||
| Age, yr | 45.8 (10.2) | 43.1 (12.0) | 0.25 |
| Sex | 0.76 | ||
| Male | 29 | 24 | |
| Female | 22 | 16 | |
| Side of pathology/injection | 0.68 | ||
| Right | 22 | 19 | |
| Left | 24 | 19 | |
| Bilateral | 5 | 2 | |
| Patients receiving second injections, no. | 9 | 6 | |
| WCB patients, no. | 9 | 18 | 0.005 |
| Days from symptom onset to referral | 64.0 (64.4) | 47.5 (53.6) | 0.22 |
| Days from referral to appointment | 61.7 (63.0) | 49.6 (55.0) | 0.36 |
| Days from appointment to injection | 67.3 (65.6) | 54.5 (35.3) | 0.27 |
SD = standard deviation; WCB = Workers’ Compensation Board.
Unless otherwise indicated.
In all, 51 (56%) patients (22 women and 29 men with a mean age of 45.8 [SD 10.2] yr) reported positive results following TFESI for a follow-up period of 418.9 (SD 164.7, median 396.0, range 103–747) days. Positive results constituted improvement or resolution of pain and/or neurologic abnormality, such that the primary outcome measure — surgical intervention — was not required. These 51 patients, who had initially requested microdiscectomy surgery, voluntarily declined surgery owing to symptom improvement or resolution following TFESI. Forty (44%) patients (16 women and 24 men with a mean age of 43.1 [SD 12.0] yr) failed to demonstrate benefit following TFESI and thus proceeded to surgery. These results demonstrated a 56% reduction in patients requiring surgical intervention.
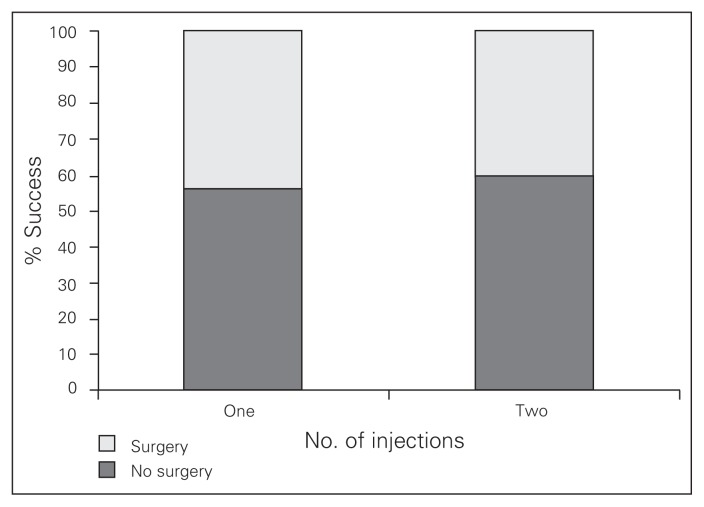
Of the 91 study patients, 76 (84%) received a single TFESI intervention. Of these 42 (55%) did not require surgical intervention. Fifteen (16%) patients received a second TFESI owing to symptom recurrence despite initial resolution. Of the 15 patients who received a second TFESI intervention, 9 (60%) did not require surgical intervention. Equal success was noted despite the number of injections required. The need for a second injection did not indicate a greater likelihood of failure or progression to surgery (Fig. 4).
Fig. 4.
The percentage of patients who did and did not require surgical intervention after the first and second injections.
The Pearson χ2 tests revealed no significant difference in treatment outcome for sex (χ2 = 0.091), side of pathology (χ2 = 0.768) and injecting physician (χ2 = 2.073; all p > 0.05). Our ANOVA showed no significant differences in age (45.8 v. 43.1 yr) between the surgical and nonsurgical groups. Therefore, these factors had no influence on treatment outcome.
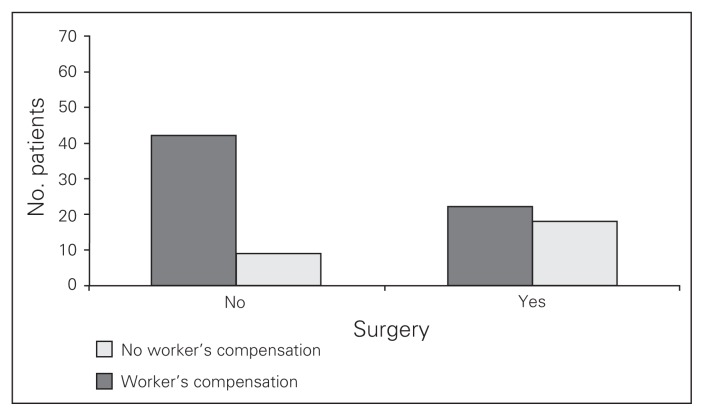
Workers’ compensation status had a significant negative influence on treatment outcome (χ2 = 8.038, p = 0.005). Of 91 patients, 27 were on workers’ compensation and 18 of these 27 patients (67%) required surgery (Fig. 5). There were no significant differences in demographic characteristics between patients receiving workers’ compensation and those not receiving it.
Fig. 5.
Number of patients receiving workers’ compensation who did and did not require surgery.
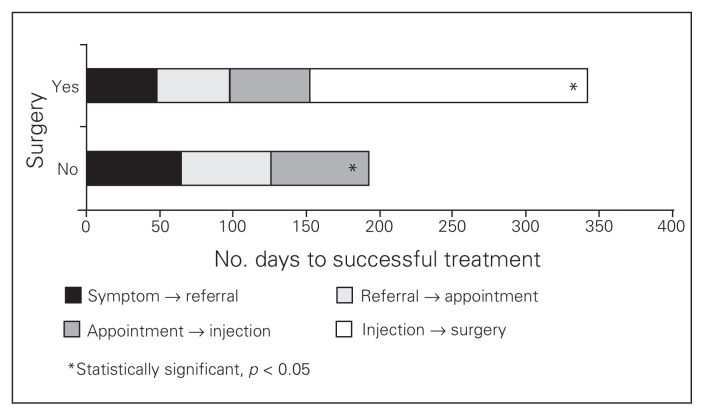
Among patients who had a recorded time from symptom onset to primary assessment (n = 86), that time varied greatly (median 197.5, range 33–1768 d). The mean wait time from family physician referral for surgical assessment to the TFESI injection for all 91 patients was 123.8 (SD 88.9) days. The time from TFESI to surgical intervention (n = 40) was 189.2 (SD 125.2) days. The 1-way ANOVA revealed no significant differences for any of the 3 time periods in relation to TFESI success and surgical avoidance: symptom onset to referral (228.33 v. 229.3 d), referral to appointment (61.7 v. 49.6 d) and appointment to injection (67.3 v. 54.5 d). Patients whose injections were successful and thus did not require surgery had a significantly shorter management course (p < 0.001; Fig. 6).
Fig. 6.
Means and standard deviations for appointment time-lines. Time to effective treatment was statistically different.
Adverse events were recorded during immediate post-injection observation, before discharge, and at 6-week orthopedic re-evaluation. We noted no significant complications secondary to TFESI. Two patients suffered vasovagal events (feeling flushed, lightheaded) that were transient in nature and that did not alter postinjection care or outcome. No further complications were noted in any patients at final evaluation.
Discussion
The efficacy of TFESI to relieve radicular symptoms secondary to lumbar disc pathology has been well documented.8–13 The complication profile is limited,27,28 and the alleviation of surgical need has also been demonstrated.8–10 Recently, 2 independent systematic reviews15,16 evaluated the evidence of TFESI effectiveness, scoring it at level II: evidence obtained from well-designed, controlled cohort or case–control studies.
In these previous studies, 6-week symptom duration qualified for study intervention. To our knowledge, ours is the first study to address the role of TFESI in the management of longstanding radicular symptoms secondary to LDH.
Treatment delay has been reported to affect clinical outcomes. Surgical delay not only diminishes function and quality of life while paitents wait for surgery, but also negatively impacts their surgical outcomes.9,11,19,29 Parameters most affected by extended spine surgery wait times were physical function and pain severity.19 Optimizing management pathways to decrease time to treatment, improve outcomes and control costs are essential. The possibility of shortening the treatment course via elimination of the wait to surgical intervention is therefore very attractive. Furthermore, surgical avoidance frees critical resources and permits other patients to access these resources.
The present study quantified the wait times for 3 distinct periods of the management course. Each period is lengthy owing to resource limitations creating barriers to care. Despite these extended times, TFESI proved successful in most patients. Furthermore, variations in individual patients’ wait times were not a factor influencing TFESI effectiveness. They continued to be an effective treatment tool regardless of the severity of chronicity observed in our study. Likewise, Peul and colleagues29 acknowledged the equivalent success of early versus delayed (up to 23 wk after specialist assessment) surgery for LDH. To our knowledge, no data existed until now regarding the outcome of delayed TFESI.
Our study demonstrated a 56% reduction in surgical cases in a patient population with chronic symptoms and dysfunction who wished to proceed to surgery. Although this cohort study cannot establish causation, we believe TFESI can be attributed to this reduction in the number of surgeries performed. Weinstein and colleagues2 demonstrated a dropout rate of only 4% over 2 years in patients requesting surgery. At our own institution during the same time period, an audit of all orthopedic and neurosurgery patients not receiving TFESI before consenting to discectomy surgery demonstrated a dropout rate of only 10% (23 of 231). Thus an association between TFESI and the avoidance of discectomy surgery is suggested.
The 51 (56%) patients who avoided surgery avoided surgical risk and postoperative recovery. They also realized a significantly more rapid treatment course than those awaiting surgery (Fig. 6). This protraction of time to symptom and functional improvement would be expected to provide additional benefit to the patient.
Both nonsurgical and surgical interventions have proven safe and effective in the treatment of LDHs.29–33 These findings were further confirmed via the SPORT trial34,35 focused on LDH. In both the randomized trial arm (owing to crossover) and the observational trial arm, patients actively selected the treatment course perceived to be most beneficial to them. These patients proved successful decision-makers, steering their treatment course to satisfactory symptom relief most of the time.34,35 In our present study, patient bias for treatment choice was minimized, as all nonurgent patients received TFESI. While it is possible that some patients may benefit most from bypassing this treatment and moving directly to surgery, predictive factors have not been delineated at present. Identifying these patients who should move directly to surgery should be the effort of future research.
Cost analysis included institutional costs provided by the hospital corporation for both TFESI and outpatient microdiscectomy, and physician costs (anesthesia, surgery, radiology) provided by the provincial fee schedule. The direct cost to our institution for an outpatient discectomy surgery is $2050. The direct cost for TFESI is $230, only 11% of the surgical cost. This represented a substantial direct cost saving for treatment to our institution during the study period. The indirect cost saving realized with improved work potential and return of quality of life in a shorter time course could prove important to the individual patient; however, this was not directly measured in our study.
To our knowledge, no study has included workers’ compensation patients in assessing the outcome of TFESI. Compensation status is often associated with poor outcomes after therapeutic intervention.5,36,37 However, these patients also demonstrate decreased surgical success.37 Specifically, patients receiving workers’ compensation who had lumbar discectomy and lumbar fusion had worse surgical outcomes than patients who were not receiving workers’ compensation.37,38 The ability to validate the success of TFESI as an additional nonoperative modality to improve outcomes in this group is important. To improve outcomes while also avoiding surgery is paramount.
Workers’ compensation patients did demonstrate benefit from TFESI. The significant difference in treatment outcome and surgical need as compared with patients not receiving workers’ compensation parallels that seen in other studies.37,39 The rationale for this difference is a source of ongoing study; clinical and nonclinical factors are presented as potential impediments to healing.39 Pain-related fear, avoidance of physical activity (kinesophobia), excessive focus on pain symptoms (catastrophizing), and depression may be amplified in the setting of work-related characteristics, expectations and preferences as well as features of the disability system itself.39,40
This study demonstrated the continued efficacy of TFESI in the treatment of LDH, even in patients with longstanding symptoms. Transforaminal epidural steroid injection is an additional nonoperative treatment option that alleviates symptoms and may alleviate the need for surgery for many patients. The delay in surgical treatment observed with the creation of the TFESI pathway is justifiable based on the number of successful treatments.
Limitations
Study limitations pertain to the study design and its retrospective nature. The primary outcome measure of surgery avoidance was valuable. However, it does not allow description of the posttreatment success of each patient. No specific measures were provided for relief of pain, use of medications, return to work and function, or patient satisfaction. Causation between TFESI success and surgical avoidance cannot be confirmed but appears to be correlated, as discussed previously.
Conclusion
Transforaminal epidural steroid injections continued to be effective despite delayed time to patient assessment and treatment and despite longstanding patient symptoms. They are an important treatment tool, preventing the need for surgery in 56% of patients with LDH and easing the surgical burden on a taxed health care system. Both 1-time and repeat injections were effective in surgery avoidance and did not simply delay the need for surgery. Patients receiving workers’ compensation continue to demonstrate lower rates of success, as can be observed throughout the literature. These patients may not be as effectively served with nerve root injections for reasons that are currently unknown.
Acknowledgement
We thank Jim Croll, EdD, of the University of New Brunswick, for assistance with the statistical methods.
Footnotes
This work was presented at the 24th Annual North American Spine Society Meeting in San Francisco, California, Nov. 10, 2009.
Competing interests: None declared.
Contributors: All authors participated in study design, data acquisition and analysis, article review, and each approved it for publication. N.A. Manson and M.D. McKeon wrote the article.
References
- 1.Awad JN, Moskovich R. Lumbar disc herniations: surgical versus nonsurgical treatment. Clin Orthop Relat Res. 2006;443:183–97. doi: 10.1097/01.blo.0000198724.54891.3a. [DOI] [PubMed] [Google Scholar]
- 2.Weinstein JN, Lurie J, Olson P, et al. United States’ trends and regional variations in lumbar spine surgery: 1992–2003. Spine. 2006;31:2707–14. doi: 10.1097/01.brs.0000248132.15231.fe. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Organisation for Economic Co-operation and Development (OECD) OECD Health Data 2012: How does Canada compare? Paris (France): OECD; 2012. [accessed 2012 Dec. 11]. Available: www.oecd.org/canada/BriefingNoteCANADA2012.pdf. [Google Scholar]
- 4.Cherkin DC, Deyo R, Loeser J, et al. An international comparison of back surgery rates. Spine. 1994;19:1201–6. doi: 10.1097/00007632-199405310-00001. [DOI] [PubMed] [Google Scholar]
- 5.McIntosh G, Hall H, Melles T. The incidence of spinal surgery in Canada. Can J Surg. 1998;41:59–66. [PMC free article] [PubMed] [Google Scholar]
- 6.Eckel TS, Bartynski WS. Epidural steroid injections and selective nerve root blocks. Tech Vasc Interv Radiol. 2009;12:11–21. doi: 10.1053/j.tvir.2009.06.004. [DOI] [PubMed] [Google Scholar]
- 7.Saal JS. The role of inflammation in lumbar pain. Spine. 1995;20:1821–7. doi: 10.1097/00007632-199508150-00013. [DOI] [PubMed] [Google Scholar]
- 8.Riew KD, Yin Y, Gilula L, et al. The effect of nerve root injections on the need for operative treatment of lumbar radicular pain: a prospective, randomized, controlled, double blind study. J Bone Joint Surg Am. 2000;82-A:1589–93. doi: 10.2106/00004623-200011000-00012. [DOI] [PubMed] [Google Scholar]
- 9.Karppinen J, Malmivaara A, Kurunlahti M, et al. Periradicular infiltration for sciatica: a randomized controlled trial. Spine (Phila Pa 1976) 2001;26:1059–67. doi: 10.1097/00007632-200105010-00015. [DOI] [PubMed] [Google Scholar]
- 10.Riew KD, Park JB, Cho YS, et al. Nerve root blocks in the treatment of lumbar radicular pain. A minimum five-year follow-up. J Bone Joint Surg Am. 2006;88:1722–5. doi: 10.2106/JBJS.E.00278. [DOI] [PubMed] [Google Scholar]
- 11.Vad VB, Bhat A, Lutz G, et al. Transforaminal epidural steroid injections in lumbosacral radiculopathy: a prospective randomized study. Spine. 2002;27:11–6. doi: 10.1097/00007632-200201010-00005. [DOI] [PubMed] [Google Scholar]
- 12.Thomas E, Cyteval C, Abiad L, et al. Efficacy of transforaminal versus interspinous corticosteroid injectionin discal radiculalgia — a prospective, randomised, double-blind study. Clin Rheumatol. 2003;22:299–304. doi: 10.1007/s10067-003-0736-z. [DOI] [PubMed] [Google Scholar]
- 13.Ackerman WE, Ahmad M. The efficacy of lumbar epidural steroid injections in patients with lumbar disc herniations. Anesth Analg. 2007;104:1217–22. doi: 10.1213/01.ane.0000260307.16555.7f. [DOI] [PubMed] [Google Scholar]
- 14.DePalma MJ, Bhargava A, Slipman CW. A critical appraisal of the evidence for selective nerve root injection in the treatment of lumbosacral radiculopathy. Arch Phys Med Rehabil. 2005;86:1477–83. doi: 10.1016/j.apmr.2005.01.006. [DOI] [PubMed] [Google Scholar]
- 15.Buenaventura RM, Datta S, Abdi S, et al. Systematic review of therapeutic lumbar transforaminal epidural steroid injections. Pain Physician. 2009;12:233–51. [PubMed] [Google Scholar]
- 16.Manchikanti L, Boswell MV, Datta S, et al. Comprehensive review of therapeutic interventions in managing chronic spinal pain. Pain Physician. 2009;12:E123–98. [PubMed] [Google Scholar]
- 17.World Health OrganizationThe world health report 2000 — Health systems: improving performanceGeneva (Switzerland)WHO; The Organization; 2000 [Google Scholar]
- 18.Esmail N. Waiting your turn: hospital waiting lists in Canada: 2009 report. Calgary (AB): The Fraser Institute; 2009. [Google Scholar]
- 19.Braybrooke J, Ahn H, Gallant A, et al. The impact of surgical wait time on patient-based outcomes in posterior lumbar spinal surgery. Eur Spine J. 2007;16:1832–9. doi: 10.1007/s00586-007-0452-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Okoro T, Sell P. The prediction of outcome in somatised patients undergoing elective lumbar surgery. J Bone Joint Surg Br. 2009;91:517–21. doi: 10.1302/0301-620X.91B4.21861. [DOI] [PubMed] [Google Scholar]
- 21.Trief PM, Grant W, Fredrickson B. A prospective study of psychological predictors of lumbar surgery outcome. Spine. 2000;25:2616–21. doi: 10.1097/00007632-200010150-00012. [DOI] [PubMed] [Google Scholar]
- 22.Jellema P, van der Horst H, Vlaeyen J, et al. Predictors of outcome in patients with sub-acute low back pain differ across treatment groups. Spine. 2006;31:1699–705. doi: 10.1097/01.brs.0000224179.04964.aa. [DOI] [PubMed] [Google Scholar]
- 23.Ostendorf M, Buskens E, van Stel H, et al. Waiting for total hip arthroplasty: avoidable loss in quality time and preventable deterioration. J Arthroplasty. 2004;19:302–9. doi: 10.1016/j.arth.2003.09.015. [DOI] [PubMed] [Google Scholar]
- 24.Fishbain DA, Cutler R, Rosomoff H, et al. Chronic pain-associated depression: Antecedent or consequence of chronic pain? A review. Clin J Pain. 1997;13:116–37. doi: 10.1097/00002508-199706000-00006. [DOI] [PubMed] [Google Scholar]
- 25.Chou R, Loeser J, Owens D, et al. Interventional therapies, surgery, and interdisciplinary rehabilitation for low back pain. Spine. 2009;34:1066–77. doi: 10.1097/BRS.0b013e3181a1390d. [DOI] [PubMed] [Google Scholar]
- 26.Arden NK, Price C, Reading I, et al. A multicentre randomized controlled trial of epidural corticosteroid injections for sciatica: the WEST study. Rheumatology. 2005;44:1399–406. doi: 10.1093/rheumatology/kei028. [DOI] [PubMed] [Google Scholar]
- 27.Huston CW, Slipman C, Garvin C. Complications and side effects of cervical and lumbosacral selective nerve root injections. Arch Phys Med Rehabil. 2005;86:277–83. doi: 10.1016/j.apmr.2004.02.018. [DOI] [PubMed] [Google Scholar]
- 28.Stalcup ST, Crall T, Gilula L, et al. Influence of needle-tip position on the incidence of immediate complications in 2,217 selective lumbar nerve root blocks. Spine J. 2006;6:170–6. doi: 10.1016/j.spinee.2005.08.009. [DOI] [PubMed] [Google Scholar]
- 29.Peul WC, van Houwelingen H, van den Hout W, et al. Surgery versus prolonged conservative treatment for sciatica. N Engl J Med. 2007;356:2245–56. doi: 10.1056/NEJMoa064039. [DOI] [PubMed] [Google Scholar]
- 30.Hoffman RM, Wheeler K, Deyo R. Surgery for herniated lumbar discs: a literature synthesis. J Gen Intern Med. 1993;8:487–96. doi: 10.1007/BF02600110. [DOI] [PubMed] [Google Scholar]
- 31.Atlas SJ, Keller R, Wu Y, et al. Long-term outcomes of surgical and nonsurgical management of sciatica secondary to a lumbar disc herniation: 10 year results from the maine lumbar spine study. Spine. 2005;30:927–35. doi: 10.1097/01.brs.0000158954.68522.2a. [DOI] [PubMed] [Google Scholar]
- 32.Thomas KC, Fisher C, Boyd M, et al. Outcome evaluation of surgical and nonsurgical management of lumbar disc protrusion causing radiculopathy. Spine. 2007;32:1414–22. doi: 10.1097/BRS.0b013e318060a5d1. [DOI] [PubMed] [Google Scholar]
- 33.Saal JA, Saal J. Nonoperative treatment of herniated lumbar intervertebral disc with radiculopathy. An outcome study. Spine. 1989;14:431–7. doi: 10.1097/00007632-198904000-00018. [DOI] [PubMed] [Google Scholar]
- 34.Weinstein JN, Lurie J, Tosteson T, et al. Surgical vs nonoperative treatment for lumbar disk herniation: the Spine Patient Outcomes Research Trial (SPORT) observational cohort. JAMA. 2006;296:2451–9. doi: 10.1001/jama.296.20.2451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Weinstein JN, Tosteson T, Lurie J, et al. Surgical vs nonoperative treatment for lumbar disk herniation: the Spine Patient Outcomes Research Trial (SPORT): a randomized trial. JAMA. 2006;296:2441–50. doi: 10.1001/jama.296.20.2441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hakelius A. Prognosis in sciatica. A clinical follow-up of surgical and non-surgical treatment. Acta Orthop Scand Suppl. 1970;129:1–76. doi: 10.3109/ort.1970.41.suppl-129.01. [DOI] [PubMed] [Google Scholar]
- 37.Harris I, Mulfordm J, Solomon M, et al. Association between compensation status and outcome after surgery: a meta-analysis. JAMA. 2005;293:1644–52. doi: 10.1001/jama.293.13.1644. [DOI] [PubMed] [Google Scholar]
- 38.Atlas SJ, Chang Y, Keller R, et al. The impact of disability compensation on long-term treatment outcomes of patients with sciatica due to a lumbar disc herniation. Spine. 2006;31:3061–9. doi: 10.1097/01.brs.0000250325.87083.8d. [DOI] [PubMed] [Google Scholar]
- 39.Atlas SJ, Tosteson T, Blood E, et al. The impact of workers’ compensation on outcomes of surgical and nonoperative therapy for patients with a lumbar disc herniation: SPORT. Spine. 2010;35:89–97. doi: 10.1097/BRS.0b013e3181c68047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Margison DA, French D. Predicting treatment failure in the subacute injury phase using the Orebro Musculoskeletal Pain Questionnaire: an observational prospective study in a workers’ compensation system. J Occup Environ Med. 2007;49:59–67. doi: 10.1097/JOM.0b013e31802db51e. [DOI] [PubMed] [Google Scholar]