Abstract
Recent studies have suggested a favorable effect of cardiac rehabilitation (CR) on patients with cardiovascular disease. This study aimed to evaluate the impact of home-based exercise training with wireless monitoring on acute coronary syndrome (ACS) patients undergoing percutaneous coronary intervention (PCI). A total of 55 ACS patients undergoing PCI were randomly divided into home based exercise training with wireless monitoring cardiac rehabilitation (CR, n = 26) and usual care (UC, n = 29). Exercise capacity and quality of life (QOL) were evaluated at baseline and after 12 weeks. Change of metabolic equivalent of the tasks, maximal exercise time and QOL were significantly increased (+2.47 vs +1.43, P = 0.021; +169.68 vs +88.31 sec, P = 0.012; and +4.81 vs +0.89, P = 0.022, respectively), and the change of submaximal rate pressure product, and of submaximal rate of perceived exertion were significantly decreased (-28.24 vs -16.21, P = 0.013; and -1.92 vs -1.62, P = 0.018, respectively) in the CR group compared to the UC group after 12 weeks. CR using home-based exercise training with wireless monitoring led to improvement of exercise capacity and QOL relative to conventional care in ACS patients undergoing PCI. Our findings suggest that early scheduled CR may be considered in ACS patients undergoing PCI.
Keywords: Acute Coronary Syndrome, Cardiac Rehabilitation, Exercise Capacity, Quality of Life
INTRODUCTION
The importance of cardiac rehabilitation (CR) recently has been stressed among the approaches for proper cardiac disease management including diet control, medications, percutaneous coronary intervention (PCI) or coronary artery bypass graft (1, 2). Although home-based, as is the case for in-hospital, CR has been shown to improve exercise capacity and quality of life (QOL) of patients with ischemic heart disease (IHD), those participating in CR programs have difficulties with compliance (3-6). Also, objective monitoring and exercise standardization is difficult for home-based training because of individual exercise prescription, self measurement of heart rates, heterogeneity among patients, and lack of previous research on effects of home-based exercise training for acute coronary syndrome (ACS) patients.
Therefore, the purpose of this study was to examine the effects on exercise capacity and QOL of home-based exercise training with wireless monitoring for exercise standardization in ACS patients undergoing PCI.
MATERIALS AND METHODS
Study population
The study participants comprised 60 ACS patients who underwent successful PCI at our hospital from October 2010 to May 2011. Patients were randomly allocated to either the CR group or the usual care (UC) group. Twenty six patients in the CR group and 29 patients in the UC group completed follow-up and were available for endpoint analysis (Table 1). The reasons for drop out of patients in the CR group were: inability to exercise due to general weakness (n = 2), dizziness (n = 1) and patient refusal (n = 1); one patient in the UC group was not able to exercise due to general weakness. Patients between 18 and 80 years old with a diagnosis of ACS and having undergone PCI were included in the study. Exclusion criteria were: chronic stable angina pectoris or New York Heart Association (NYHA) class III-IV; left ventricular ejection fraction less than 30%; chronic renal failure; and inability to exercise.
Table 1.
Clinical characteristics of study participants
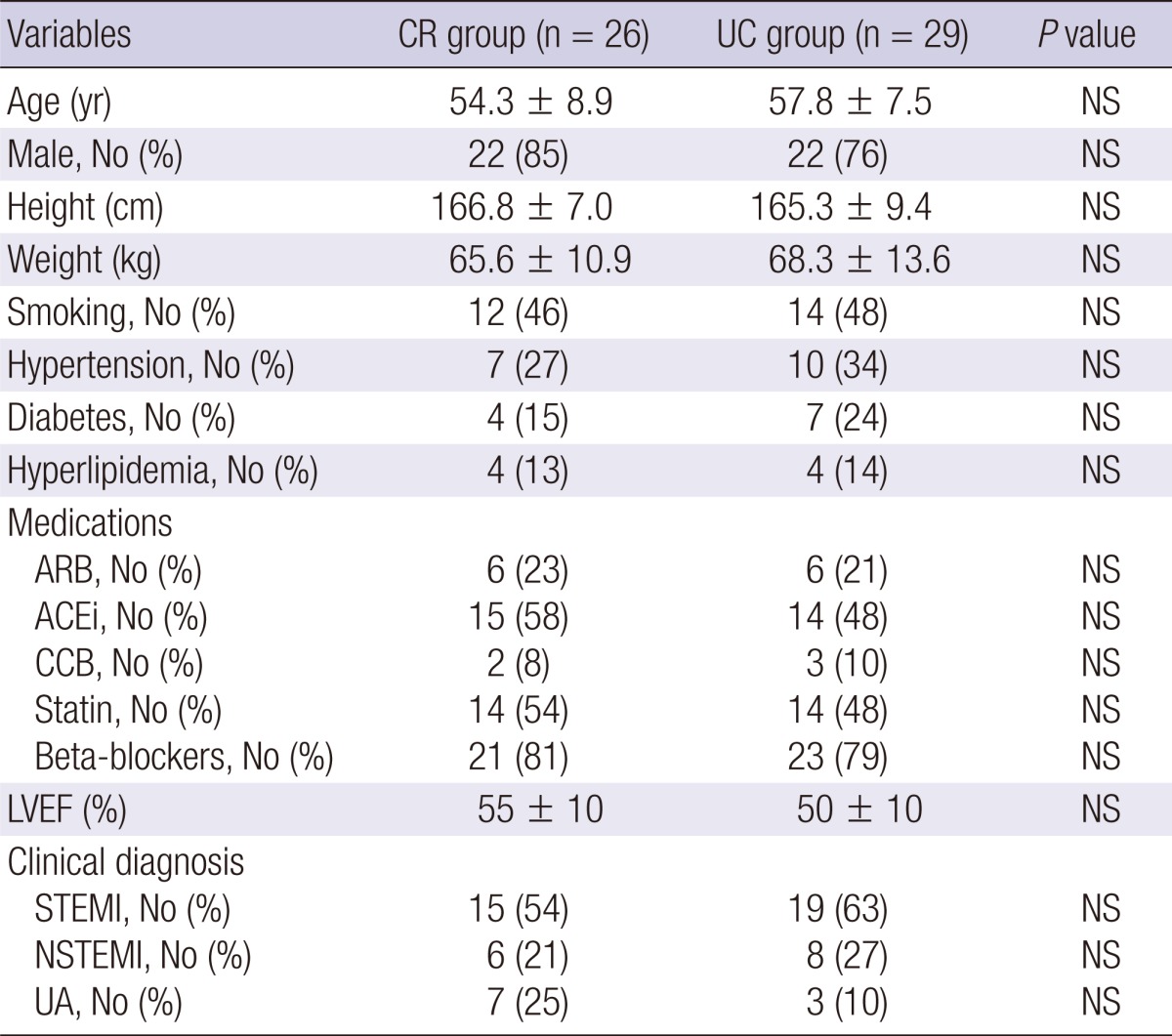
Values are presented as mean ± SD or No (%). CR, cardiac rehabilitation; UC, usual care; ARB, angiotensin II receptor blocker; ACEi, angiotensin converting enzyme inhibitor; CCB, calcium channel blocker; NS: not significant; LVEF, left ventricular ejection fraction; STEMI, ST-segment elevation myocardial infarction; NSTEMI, non-ST elevation myocardial infarction; UA, unstable angina.
Intervention protocol
The CR group received standard medical therapy and a CR program, which consisted of educational rehabilitation and exercise training. For educational rehabilitation, the researcher educated the subjects in person prior to their hospital discharge on risk factors for heart disease, diet control, and how to institute exercise training.
From the second to the twelfth weeks after hospital discharge, exercise training consisted of scheduled gait exercise at home four to five times weekly 50 min each including flexibility exercise for 20 min (warm-up exercise for 10 min and cool-down exercise for 10 min) and main exercise of gait for 30 min. Study participants also conducted treadmill exercise once to twice while in hospital during the study period. They were instructed to perform for 2 weeks after hospital discharge the main exercise at home while wearing the wireless monitoring equipment provided (HeartCall™, U-HEART, Korea) to check their heart rates through electrocardiography. A phone call was made to them once weekly for counseling, and to minimize risk factors and establish exercise intensity in stages (Fig. 1).
Fig. 1.
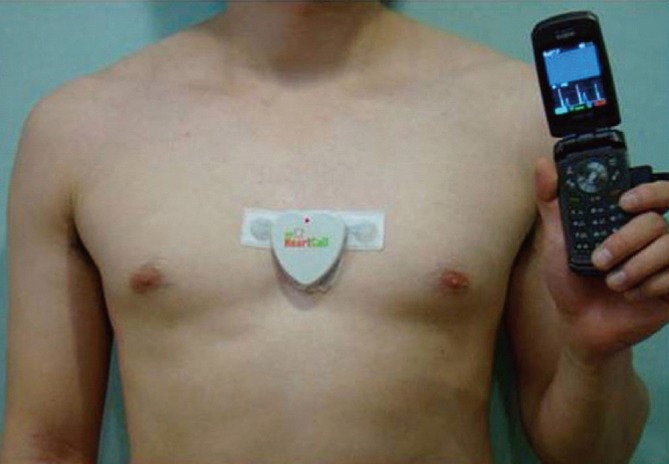
Wireless monitoring (HeartCall™). The HeartCall device was attached to the chest, and the ECG data was sent to the server via mobile phone.
Exercise intensity was increased in stages from 40% to 80% based on heart rate reserve calculated by the difference between maximum heart rate and resting heart rate, which was measured by a gradual symptom-limited exercise stress test. Target heart rate was derived from the Karvonen formula: Target heart rate = (maximum heart rate - resting heart rate) × percentage + resting heart rate. Exercise intensity was 40% weeks 2 to 4, 50% weeks 5 to 6, 60% weeks 7 to 8, 70% weeks 9 to 10, and 80% weeks 11 to 12. The UC group received ordinary medical therapy, diet control, and conducted exercise at home on their own and without participating in a CR program.
Gradual symptom-limited exercise stress test
Both groups twice underwent gradual symptom-limited exercise stress testing, at baseline and after week 12. The gradual symptom-limited exercise stress test was conducted using the modified Bruce protocol with a treadmill to examine exercise load (Marquette, GE, Fairfield, CT, USA). Heart rate and blood pressure were measured for two minutes during each exercise stage using a 12-channel real-time electrocardiogram monitoring system and an ambulatory blood pressure monitor (ABPM, GE), respectively. Exercise capacity was assessed by submaximal rate pressure product (RPPsubmax), submaximal rate of perceived exertion (RPEsubmax), metabolic equivalent of the tasks (METs), and maximal exercise time (ETmax). RPPsubmax and RPEsubmax were measured at stage 3, and the 6-20 Borg scale was used for the measurement of RPEsubmax.
Quality of life questionnaire
QOL of both groups was measured at baseline and after week 12 using a 20-item questionnaire by adding the scores corresponding to each answer. The QOL questionnaire, which was independently filled out by all patients based on a previous study (7) and with a Cronbach's alpha reliability of 0.766, included: sleep, fatigue, anxiety, chest pain, nutrition, and social psychological status.
Statistical analysis
All statistical analyses were performed with the Statistical Package for the Social Sciences (version 15.0 for Windows; SPSS Inc, Chicago, IL, USA). The sample size was determined using a statistical power of 80% and a type 1 error of 0.05. The Levene-test for equal variances was used to verify homogeneity between the two groups in terms of gender, age, height, weight, medications and risk factors such as smoking, hypertension, diabetes mellitus, and hyperlipidemia.
Paired t-tests were used to compare the changes in exercise capacity, and QOL between baseline and after week 12 in each group. Independent t-test was used to test the significance of the difference between groups. The statistical significance level, P, was set at 0.05.
Ethics statement
The study protocol was approved by the institutional medical review board of Keimyung University Dongsan Medical Center (IRB approval No. 10-1019), and written informed consent was obtained from all patients.
RESULTS
The median age of the CR group was 54 yr with 85% male, while the median age of the UC group was 57 yr with 76% male. There were no significant differences between the two groups in height, weight, and in distribution of medications and risk factors such as smoking, hypertension, diabetes mellitus, and hyperlipidemia (P = NS). Baseline exercise capacity assessed by RPPsubmax, RPEsubmax, METs, and ETmax, and QOL were not significantly different between groups (P = NS).
Exercise capacity and quality of life
The CR group showed significantly decreased RPPsubmax and RPEsubmax (159.72 ± 41.11 vs 131.48 ± 22.06 bpm·mmHg, P = 0.002, and 10.56 ± 1.98 vs 8.64 ± 1.75, P < 0.001, respectively) and significantly increased METs, ETmax and QOL score (7.14 ± 1.86 vs 9.61 ± 1.80, P < 0.001, 670.16 ± 153.42 vs 839.84 ± 106.65 sec, P < 0.001, and 56.31 ± 5.67 vs 61.12 ± 5.91, P < 0.001, respectively) between baseline and after 12 weeks. The UC group showed significantly decreased RPEsubmax (11.38 ± 2.32 vs 9.76 ± 2.01, P < 0.001) and significantly increased METs and ETmax (7.07 ± 2.07 vs 8.50 ± 2.05, P = 0.001, and 676.66 ± 145.87 vs 764.97 ± 125.95 sec, P = 0.001, respectively) between baseline and after 12 weeks.
Furthermore, the CR group showed significant improvements in the change of RPPsubmax (-28.24 vs -16.21 bpm·mmHg, P = 0.013), RPEsubmax (-1.92 vs -1.62, P = 0.018), METs (+2.47 vs +1.43, P = 0.021), ETmax (+169.68 vs +88.31 sec, P = 0.012), and QOL (+4.81 vs +0.89, P = 0.022) compared to the UC group (Table 2).
Table 2.
Exercise capacity data for cardiac rehabilitation (CR) and usual care (UC) groups
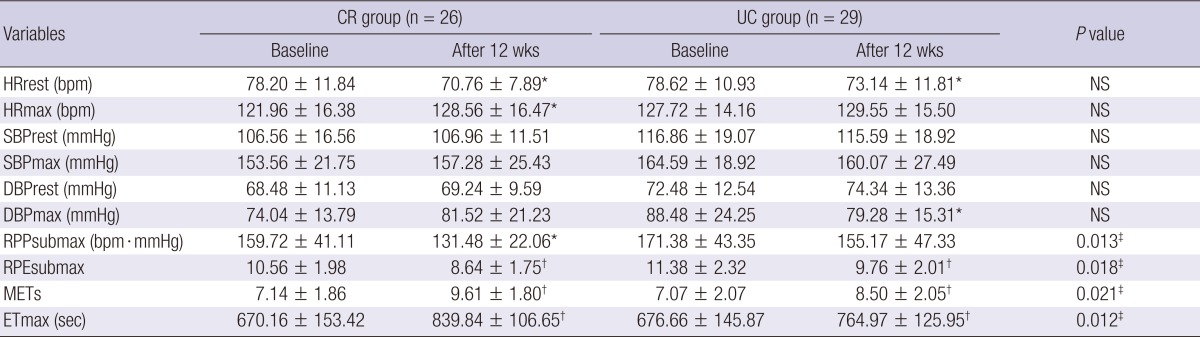
Values are presented as mean ± SD or No (%). *P < 0.05: versus baseline, †P < 0.001: versus baseline, ‡P < 0.05: CR group versus UC group. HR, heart rate; SBP, systolic blood pressure; DBP, diastolic blood pressure; RPPsubmax, rate pressure product at stage III by modified Bruce protocol; RPEsubmax, rate of perceived exertion at stage III by modified Bruce protocol; METs, metabolic equivalent of the tasks; ETmax, maximal exercise time; NS, not significant.
DISCUSSION
Intervention programs including exercise and medical therapy may prevent coronary artery disease and sudden cardiac death. Regular exercise training is in most individually recommended to patients as intervention for coronary artery disease (8) aiming to induce various physiological adaptations, increase oxygen levels in the arteries (9), and decrease rate of perceived exertion during physical activities or exercise, thereby improving cardiac exercise capacity. In the present study, the CR group showed significantly decreased RPPsubmax and RPEsubmax (-18.7% and -18.2%, respectively) and significantly increased METs and ETmax (+34.6% and +25.3%, respectively).
In line with the present study, in-hospital cardiac rehabilitation for IHD patients had been associated with significantly improved exercise capacity (10-12). Previous studies, however, were based on heterogeneous populations including ACS and stable angina patients (6, 13), while the present study included ACS patients only. In addition, in previous studies home-based exercise training was performed through individual exercise prescription, and heart rates were measured by the patients themselves, whereas in the present study they were instructed to use wireless monitoring equipment. Therefore, patients in the CR group were able to reduce the anxiety they felt over exercise during the early period after discharge, and their heart rates measured through monitoring verified whether their exercise intensity was adequate, which in turn enabled prescription of exercise intensity in stages.
Recent studies showed that QOL of IHD patients is improved by a CR program even in patients with acute myocardial infarction (4, 14, 15). Similarly, in the present study, the CR group showed a significant increase in QOL score (+8.5%). In most IHD patients, anxiety over exercise, social participation, and return to their job during an early period after hospital discharge may play a major factor that reduced their QOL. Possible explanations of improvement of QOL in the CR program are that the invention program may ameliorate participant's risk factors by education and increase exercise capacity by gradual exercise loading, resulting in improvement of their job performance and a better QOL.
The timing and safety of exercise performance are an important aspect in ACS patients after hospital discharge. Previous investigations have reported that the exercise program was launched at least 4 to 6 weeks after discharge (14, 15), whereas the present study started the CR program in all patients 1 week after discharge without any cardiac complications. Furthermore, most patients in the present study safely completed our CR program without cardiac symptoms and only two patients in the CR group complained of atypical chest discomfort. These observations suggest that an individually tailored CR program can safely be used in the acute phase (1 week later) after hospital discharge in ACS patients who underwent PCI.
Similar to the current study, Ades et al. (16) demonstrated the favorable effect of cardiac rehabilitation exercise at home on QOL using transtelephonic monitoring. The possible benefits of wireless monitoring include the ability to reduce the anxiety felt by patients over exercise during an early period after discharge, to verify the adequacy of exercise intensity by measuring their heart rates through wireless monitoring, and to prescribe exercise intensity in stages. These findings encourage further research on wireless monitoring to allow safer physical activity and exercise and popularization of wireless monitoring.
Similar to the current study, Ades et al. (16) demonstrated the favorable effect of cardiac rehabilitation exercise at home on QOL using transtelephonic monitoring. The possible benefits of wireless monitoring include the ability to reduce the anxiety felt by patients over exercise during an early period after discharge, to verify the adequacy of exercise intensity by measuring their heart rates through wireless monitoring, and to prescribe exercise intensity in stages. These findings encourage further research on wireless monitoring to allow safer physical activity and exercise and popularization of wireless monitoring.
The present study has several limitations. First, due to the short study period, comparison with previous studies on a long-term basis was difficult. Second, because the subjects were ACS patients, who are relatively poorly represented in numbers among heart disease patients, the number of study participants was too small to generalize its results. Third, although the patients performed exercise on wireless monitoring equipment and were counseled and managed through phone calls, quantification of exercise was difficult. Fourth, because of the diverse patient job characteristics, standardization of individual job load was difficult. Fifth, although used in a previous study (7), the QOL questionnaire used in the present study may need further validation.
The present study assessed the effects of home-based exercise training by scheduled walking started at an early period after hospital discharge in ACS patients undergoing PCI. Compared to the UC control group, CR using home-based exercise training with wireless monitoring can improve not only exercise capacity but also QOL in this patient subset. Therefore, our findings suggest that scheduled early CR may be considered in ACS patients undergoing PCI. In particular, the finding that patients were able to reduce their anxiety by using the wireless monitoring equipment during exercise at home is considered clinically meaningful and more studies on its clinical application are warranted to complement the present study.
ACKNOWLEDGMENTS
This study was supported by a grant from Daewong Pharm. Co., Ltd., Seoul, Korea and the Regional Technology Innovation Program (2012, RTI 04-01-01) of the Ministry of Knowledge Economy (MKE) of Korea. All authors had no conflicts of interest pertinent to the contents of this paper to disclose. The sponsor in this study did not participate in the selection and management of patients and analysis of the data.
References
- 1.Brubaker PH, Kaminsky LA, Whaley MH. Coronary artery disease: essentials of prevention and rehabilitation programs. Champaign: Human Kinetics; 2002. pp. 171–483. [Google Scholar]
- 2.Vonder Muhll I, Daub B, Black B, Warburton D, Haykowsky M. Benefits of cardiac rehabilitation in the ninth decade of life in patients with coronary heart disease. Am J Cardiol. 2002;90:645–648. doi: 10.1016/s0002-9149(02)02574-2. [DOI] [PubMed] [Google Scholar]
- 3.Ahn JK, Kim C, Bang IK, Kim YJ. Effectiveness of cardiac rehabilitation on exercise capacity and ventricular function in ischemic heart disease patients. Korean J Sports Med. 2006;24:229–236. [Google Scholar]
- 4.Choo J, Burke LE, Pyo Hong K. Improved quality of life with cardiac rehabilitation for post-myocardial infarction patients in Korea. Eur J Cardiovasc Nurs. 2007;6:166–171. doi: 10.1016/J.EJCNURSE.2006.07.004. [DOI] [PubMed] [Google Scholar]
- 5.Kim C, Lim HS, Ahn JK, Bang IK, Lee SM, Kim YJ. The reasons that cardiac patients did not participate in and drop out from the cardiac rehabilitation program. J Korean Acad Rehabil Med. 2002;26:790–796. [Google Scholar]
- 6.Tygesen H, Wettervik C, Wennerblom B. Intensive home-based exercise training in cardiac rehabilitation increases exercise capacity and heart rate variability. Int J Cardiol. 2001;79:175–182. doi: 10.1016/s0167-5273(01)00414-4. [DOI] [PubMed] [Google Scholar]
- 7.McGirr M, Rukholm E, Salmoni A, O'Sullivan P, Koren I. Perceived mood and exercise behaviors of cardiac rehabilitation program referrals. Can J Cardiovasc Nurs. 1990;1:14–19. [PubMed] [Google Scholar]
- 8.Joshi SB. Exercise training in the management of cardiac failure and ischaemic heart disease. Heart Lung Circ. 2007;16:S83–S87. doi: 10.1016/j.hlc.2007.03.013. [DOI] [PubMed] [Google Scholar]
- 9.Ades PA. Cardiac rehabilitation and secondary prevention of coronary heart disease. N Engl J Med. 2001;345:892–902. doi: 10.1056/NEJMra001529. [DOI] [PubMed] [Google Scholar]
- 10.Hao SC, Chai A, Kligfield P. Heart rate recovery response to symptom-limited treadmill exercise after cardiac rehabilitation in patients with coronary artery disease with and without recent events. Am J Cardiol. 2002;90:763–765. doi: 10.1016/s0002-9149(02)02607-3. [DOI] [PubMed] [Google Scholar]
- 11.Kalapura T, Lavie CJ, Jaffrani W, Chilakamarri V, Milani RV. Effects of cardiac rehabilitation and exercise training on indexes of dispersion of ventricular repolarization in patients after acute myocardial infarction. Am J Cardiol. 2003;92:292–294. doi: 10.1016/s0002-9149(03)00628-3. [DOI] [PubMed] [Google Scholar]
- 12.Kligfield P, McCormick A, Chai A, Jacobson A, Feuerstadt P, Hao SC. Effect of age and gender on heart rate recovery after submaximal exercise during cardiac rehabilitation in patients with angina pectoris, recent acute myocardial infarction, or coronary bypass surgery. Am J Cardiol. 2003;92:600–603. doi: 10.1016/s0002-9149(03)00733-1. [DOI] [PubMed] [Google Scholar]
- 13.Bäck M, Wennerblom B, Wittboldt S, Cider A. Effects of high frequency exercise in patients before and after elective percutaneous coronary intervention. Eur J Cardiovasc Nurs. 2008;7:307–313. doi: 10.1016/j.ejcnurse.2008.02.001. [DOI] [PubMed] [Google Scholar]
- 14.Izawa K, Hirano Y, Yamada S, Oka K, Omiya K, Iijima S. Improvement in physiological outcomes and health-related quality of life following cardiac rehabilitation in patients with acute myocardial infarction. Circ J. 2004;68:315–320. doi: 10.1253/circj.68.315. [DOI] [PubMed] [Google Scholar]
- 15.Maines TY, Lavie CJ, Milani RV, Cassidy MM, Gilliland YE, Murgo JP. Effects of cardiac rehabilitation and exercise programs on exercise capacity, coronary risk factors, behavior, and quality of life in patients with coronary artery disease. South Med J. 1997;90:43–49. doi: 10.1097/00007611-199701000-00010. [DOI] [PubMed] [Google Scholar]
- 16.Ades PA, Pashkow FJ, Fletcher G, Pina IL, Zohman LR, Nestor JR. A controlled trial of cardiac rehabilitation in the home setting using electrocardiographic and voice transtelephonic monitoring. Am Heart J. 2000;139:543–548. doi: 10.1016/s0002-8703(00)90100-5. [DOI] [PubMed] [Google Scholar]


