Abstract
Background
Work-related injuries and illness are prevalent and costly. Firefighting is especially hazardous and many firefighters sustain work-related injuries. Workplace health promotion programmes have shown positive return on investment (ROI). Little is known about how similar programmes would impact injury and cost among firefighters.
Aims
To evaluate the impact of a workplace health promotion intervention on workers’ compensation (WC) claims and medical costs among Oregon fire departments participating in the PHLAME (Promoting Healthy Lifestyles: Alternative Models’ Effects) health promotion programme compared with Oregon fire departments not participating in PHLAME.
Methods
Data from firefighters from four large urban fire departments in Oregon were evaluated using a retrospective quasi-experimental study design. Outcomes were (i) total annual firefighter WC claims, (ii) total annual incurred medical costs prior to and after implementation of the PHLAME firefighter worksite health promotion programme (iii) and an ROI analysis.
Results
Data were obtained from 1369 firefighters (mean age of 42 years, 91% white, 93% male). WC claims (P < 0.001) and medical costs (P < 0.01) were significantly lower among PHLAME fire departments compared with Oregon fire departments not participating in the programme. Fire departments participating in the PHLAME TEAM programme demonstrated a positive ROI of 4.61–1.00 (TEAM is used to indicate the 12-session peer-led health promotion programme).
Conclusions
Fire department WC claims and medical costs were reduced after implementation of the PHLAME workplace health promotion programme. This is a low cost, team-based, peer-led, wellness programme that may provide a feasible, cost-effective means to reduce firefighter injury and illness rates.
Key words: Firefighter, health promotion, occupational health, occupational injury
Introduction
The overall economic impact of work-related injuries and illness is high [1]. In the USA in 2010 there were over 3 million non-fatal workplace injuries and illnesses [2], and the total direct and indirect costs associated with work-related injuries and illnesses are estimated at more than $250 billion, almost a 71% increase since 1992 [3]. Injuries are responsible for over 90% of these costs, with illness accounting for <10% [2].
The fire service is one of the most hazardous occupations [4–7]. Occupational injuries are the leading cause of disability and/or early retirement, and cardiovascular disease is the most common cause of firefighters’ work-related death [7–12]. The incidence of work-related injury is 5 to 10 times that of private industries. Based on survey data reported by fire departments, the National Fire Protection Agency (NFPA) estimated that >80 000 firefighter injuries occurred in the line of duty between 2005 and 2009 [12,13]. Every year, approximately one-third of the more than 1 million US firefighters sustain a work-related injury. In 2005 the National Institute of Standards and Technology (NIST) released a study conducted by the TriData Division of System Planning Corporation estimating that the costs of fire service-related injuries were from $2.8 billion to $7.8 billion per year [14].
One strategy to control health care costs is workplace health promotion [15–17]. While workplace wellness programmes have achieved success, showing a beneficial and positive return on investment (ROI) [17–20], there is little information about fire service health promotion and the impact on firefighter illness and injury. Fire service proponents argue the benefit of enhanced well-being and physical fitness will result in less firefighter disability, saving money while providing greater community safety and protection [21–23]. Despite this limited evidence, only 20% of US fire departments have an established wellness programme in place [14]. Understanding how a firefighter workplace wellness programme impacts upon occupational injury and costs will enable fire service organizations to make informed decisions regarding the cost-benefit of firefighter health promotion programmes.
The National Institutes of Health funded the PHLAME study to examine new methods of health promotion [24–26]. The PHLAME study compared comprehensive medical testing, individualized counselling, and a team-based, health promotion programme utilizing an outcome questionnaire and physical measures focusing on nutrition, physical activity, quality of life, stress, sleep and physical testing. Physical measures included 12h fasting blood test for cholesterol and lipids, ECG stress test with maximal oxygen uptake, anthropometric indices and strength and flexibility testing consisting of timed sit-ups, grip strength and sit-and-reach test.
The TEAM programme was a peer-led health promotion programme consisting of twelve 45min self-administered sessions conducted by firefighters at the fire station during a shift, focusing on healthy eating, exercise, injury reduction and stress management. In addition to being well-received and easy to implement, the TEAM intervention significantly increased healthy dietary behaviour, fruit and vegetable intake and fitness parameters, with less weight gain and a significant increase in an index of general well-being compared with the testing-only condition (see Table 1).
Table 1.
PHLAME TEAM programme results (mean [SEM])
| TEAM | Testing | |||
|---|---|---|---|---|
| Baseline | One year | Baseline | One year | |
| Daily servings fruits/vegetables | 5.8 (0.2) | 7.4 (0.3)** | 5.7 (0.3) | 5.8 (0.3) |
| Healthy dietary behaviour | 4.1 (0.1) | 4.6 (0.1)** | 4.0 (0.1) | 4.1 (0.1) |
| Body weight (lbs) | 195.7 (2.2) | 196.6 (2.2)* | 196.6 (2.6) | 200.0 (2.8) |
| Overall well being | 3.6 (0.1) | 3.7 (0.1)* | 3.6 (0.1) | 3.5 (0.1) |
*P < 0.05, **P < 0.01.
Complete descriptions of the programme and its findings have been published [24–27]. The positive impact of the PHLAME programme in improving physical activity and dietary behaviours of firefighters was the compelling rationale to examine the impact of this programme on fire service–related injury and illness rates [27]. Therefore the purpose of this study was to assess firefighter workers’ compensation (WC) claims and medical costs among Oregon fire departments that participated in the PHLAME programme compared with urban fire departments of similar size and demographics that did not participate.
Methods
This was a quasi-experimental before-after intervention-comparison study among four Oregon fire departments. Ethical approval for this study was obtained through the Institutional Review Board at Oregon Health & Science University. PHLAME was a 2 year multi-component health promotion programme conducted from 1999 to 2001. This current study retrospectively analysed firefighter WC claims and medical costs among fire departments over a 7 year period (1998–2004) including prior to, during and after the PHLAME programme was implemented. Retrospective information included computerized occupational medical injury/illness summary databases from each fire department, which tracked monthly and annual WC claims and medical costs.
In 2005, the human resources and risk management departments of Oregon’s largest fire bureaux (fire jurisdictions with a service population >50 000 persons) were contacted to acquire data on WC claims and medical costs between 1998 and 2004. Two large urban fire departments from the PHLAME intervention and two similar comparison urban fire departments that did not participate in the PHLAME programme were included in this study. Inclusion criteria were based on similar size, demographics, number of firefighters and having a comprehensive monthly and annual tracking of claims and costs during this period. Data from 1369 firefighters with a mean age of 42 years, 91% white, 93% male were collected. The PHLAME programme sites included Salem and Portland, Oregon fire departments with a total of 745 firefighters. The comparison sites not participating in the programme included Eugene and Tualatin Valley, Oregon fire departments totalling 624 firefighters. There were no statistically significant differences in the number of personnel or number of calls in the PHLAME and comparison fire departments (see Table 2).
Table 2.
Participating fire department sites
| Fire department | Participation | Personnel | Number of calls | ||
|---|---|---|---|---|---|
| 1998 | 2004 | 1998 | 2004 | ||
| Eugene, Oregon | Control | 203 | 221 | 12 010 | 18 209 |
| Tualatin, Oregon | Control | 306 | 403 | 21 675 | 30 227 |
| Portland, Oregon | PHLAME | 532 | 587 | 60 672 | 57 483 |
| Salem, Oregon | PHLAME | 135 | 158 | 14 102 | 16 175 |
Primary outcomes for this study were total annual WC claims, annual WC claims per firefighter and total annual medical costs incurred for the years between 1998 and 2004 inclusive. All study sites tracked monthly fire service-related WC claims and medical costs. The total number of claims and medical costs from monthly summary reports were aggregated for the two PHLAME and two comparison fire departments and then averaged to represent the mean total annual number of claims and costs for each department. In addition to total incurred medical cost, the data documented the cause and nature of the WC claim, age, gender and year of claim. For Oregon fire service-related injury or illness occurring on duty that required at least 1 day of restricted activity, a claim was filed and a State Accident Insurance Fund (SAIF) Corporation WC report filled out (SAIF is the state of Oregon’s not-for-profit, state-chartered workers’ compensation insurance company.). All claims were numerically identified without an individual’s name associated with the injury for confidentiality; therefore, a specific firefighter could not be identified. Confidentiality policies and standards were followed according to the Health Insurance Portability and Accountability Act of 1996 medical standards with no ability to identify an individual firefighter claim. Total incurred medical costs for all these claims were calculated from the perspective of the payer (government agency fire bureau) and converted to 2004 dollars using the medical consumer price index.
Mean differences in WC claims per firefighter and medical costs per firefighter over the intervention and follow-up period among the PHLAME and comparison fire departments were analysed using analysis of variance. Post hoc comparisons of the four fire departments (two PHLAME, two comparison) were carried out using paired t-tests where appropriate. An ROI analysis was performed by measuring the cost of the PHLAME interventions in addition to the cost savings incurred from the programme. The testing plus counselling group cost $1500 per firefighter ($500 testing + $1000 counselling). The testing plus TEAM programme cost a total of $600 per firefighter ($500 testing + $100 TEAM programme).
Results
Table 3 shows the mean total annual number of firefighters, total WC claims and claims rate (total claims per total number of firefighters) among the PHLAME and comparison fire bureaux in Oregon between 1998 and 2004. At baseline there was no statistically significant difference in total WC claims or claims rate.
Table 3.
Total number of firefighters, total WC claims and claims rate among PHLAME and comparison fire departments
| Claim years | PHLAME fire departments | Comparison fire departments | ||||
|---|---|---|---|---|---|---|
| Number of firefighters | Total WC claims | Claims rate (%) | Number of firefighters | Total WC claims | Claims rate (%) | |
| Mean (1998–1999) | 675 | 202 | 30 | 522 | 149 | 29 |
| Mean (2000–2004) | 727 | 200 | 28*** | 594 | 194 | 32*** |
| Percentage change | +8 | −1 | −8 | ++14 | +30 | +13 |
***P < 0.001.
For the period of time during and after the PHLAME programme (2000–2004), there was a statistically significant reduction in claims rates among firefighters in PLAME fire departments compared with comparison fire departments. The mean claims rate of 28 among the PHLAME fire departments was significantly lower (P < 0.001) than the mean claims rate of 32 amongst comparison fire departments over the same time period.
Results show that the PHLAME fire departments had an 8% increase in the number of firefighters from 1998 to 2004. The comparison fire departments had a 14% increase in the number of firefighters in the same period. Results demonstrate a 1% decrease in the mean total annual number of WC claims among the PHLAME fire departments up to 2 years after the PHLAME programme. This was in contrast to a 30% increase during the same time period among the comparison departments that did not get the PHLAME programme. When these WC claims were adjusted for the change in the number of firefighters (claims rate), there was an 8% reduction in the number of claims per total firefighter number among the PHLAME fire departments compared with a 13% increase among the comparison fire departments.
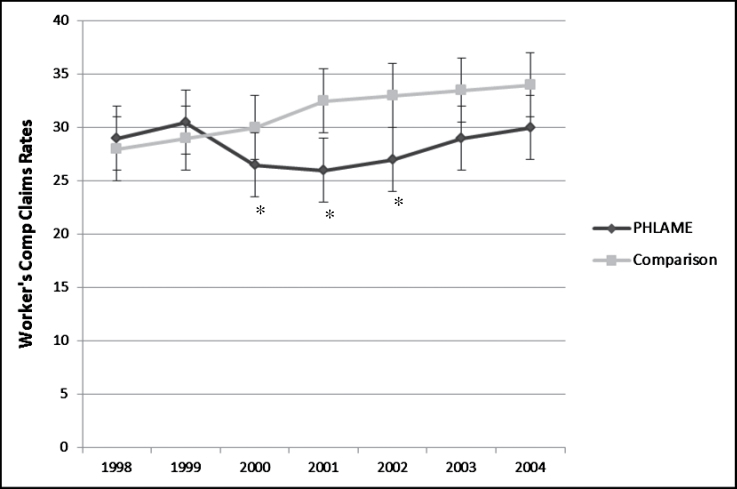
When the total number of WC claims was adjusted for the total number of firefighters (claims rate) for the PHLAME and comparison fire departments and graphed with a slope of change, there was a statistically significant difference (P < 0.01) in the slope of these lines (Figure 1). Figure 1 shows that the slope of change line actually crosses over after the first year of PHLAME and persists after the second year of the PHLAME programme after the study was completed. This graph shows that the PHLAME fire departments decreased claim rates while the comparison fire departments increased the number of claim rates during the same period of time.
Figure 1.
WC claims rate between PHLAME and comparison fire bureaux. *P < 0.01.
Table 4 shows the mean total incurred medical costs and adjusted costs per firefighter for the PHLAME and comparison fire departments. The PHLAME departments had lower mean medical costs per firefighter (P < 0.01). Post hoc analysis revealed that the PHLAME departments spent significantly less per firefighter than both comparison fire department sites (P < 0.01). The PHLAME departments had a 15% increase in total incurred medical costs compared with a 41% increase in medical costs for the comparison departments.
Table 4.
Total incurred medical costs and costs per firefighter among PHLAME and comparison fire departments
| Claim years | PHLAME fire departments | Comparison fire departments | ||
|---|---|---|---|---|
| Total costs ($) | Cost/firefighter ($) | Total costs ($) | Cost/firefighter ($) | |
| Mean (1998–1999) | 3 032 836 | 4493 | 2 261 328 | 4332 |
| Mean (2000–2004) | 3 493 263 | 4805±433** | 3 197 170 | 5358±316** |
| Percentage change | +15 | +7 | +41 | +24 |
**P < 0.01.
Additionally, when adjusted per the number of firefighters, there was a 7% increase in medical costs per firefighter over a 5 year period among the PHLAME departments as compared with a 24% increase among the comparison departments. In dollar amounts, this represents an increase of $312 per firefighter among the PHLAME departments and an increase of $1026 per firefighter among the comparison departments over this 5 year period. Thus, the medical costs per firefighter after the PHLAME programme were less than a third of those in comparison Oregon fire departments during this time.
Cost savings per firefighter were calculated using the difference in the mean medical cost per firefighter for period of time during and after the PHLAME programme (2000–2004). This difference ($553) was multiplied by five to represent the total cost savings of the PHLAME programme for the period 2000–2004 ($2765).
Comprehensive medical testing alone did not result in a statistically significant reduction in self-reported injury rates, so the ROI was performed on the TEAM and counselling groups only. Using the calculated cost savings of $2765, the PHLAME fire departments participating in the counselling intervention demonstrated a positive ROI of 1.8–1, and the TEAM intervention demonstrated a positive ROI of 4.6–1 (see Table 5).
Table 5.
Return on investment for counselling and TEAM PHLAME interventions.
| Intervention | Cost ($) | Cost savings per firefighter (2000–4) ($) | Return on investment |
|---|---|---|---|
| Testing + counselling | 1500 | 2765 | 1.8–1 |
| Testing + TEAM | 600 | 2765 | 4.6–1 |
Discussion
Our results demonstrate that in comparison with other fire departments in Oregon WC claims were reduced after the PHLAME health promotion intervention. Despite WC claims increasing to a similar degree in urban Oregon fire departments over the same time period, the reduction seen among PHLAME departments decreases the chance that this observation was a statewide or universal effect. The results also show that the PHLAME fire departments had less of an increase in medical costs associated with claims compared with the comparison sites. National annual fire department health care cost increases range from 5–8% per year [13,14]. The PHLAME fire departments had an average annual increase in incurred medical costs of 1% compared with an average annual 5% increase in such costs for the comparison fire departments.
The economic benefit from decreased WC claims and medical costs observed among the PHLAME fire departments is supported by research outside the fire service, which demonstrates that for every dollar spent on health promotion, between 2.00 and 6.00 dollars are saved [15–21]. Typical health promotion benefits may, however, take a while to return the initial investment, and for this reason funders are sceptical of long-term investment in wellness.
Injury is the leading cause of disability and early retirement in US firefighters. In 2009 the NFPA reported 84 550 firefighter injuries that required medical treatment or resulted in at least 1 day of restricted activity [12]. A large-scale study examining the relationships between the cause, nature and costs of firefighters’ injur ies found that over-exertion accounted for a significant proportion of injuries (one-third) at a cost of $9715 per claim [5]. That study calculated that eliminating injuries caused by over-exertion saved, on average, $545 000 per year for a large city fire bureau [5]. Another study of a firefighter health promotion programme emphasizing physical fitness found a reduction in injuries and injury costs during and post intervention [28]. Most recently, two studies have shown that a high proportion of US and UK firefighters are obese, with one showing a relationship between WC claims and obesity [29,30].
Despite the economic benefit of worksite wellness programmes in other industries [15–20] and the increased awareness of the importance of fire service-related job performance and the overall health and safety of firefighters, only 20% of US fire departments have an established wellness programme in place [14]. The PHLAME TEAM programme is a low cost, team-based, peer-led firefighter health promotion programme designed to be implemented at the fire station while on shift. The PHLAME programme improved nutrition and exercise habits [24–27] but equally importantly reduced WC claims and medical costs. Despite the positive ROI and economic benefit of PHLAME, this cost saving underestimates the true cost savings incurred as we did not assess total incurred costs associated with lost work days, overtime losses and backfill.
The events of 11 September 2001 increased concern for safety and health among firefighters across the USA. The study authors maintain that any ensuing health promotion activities would have affected both PHLAME and non-PHLAME departments equally. This assumption is supported by the normal increase in WC claims observed in non-PHLAME departments. None of the study sites reported implementing additional wellness programmes during this time.
This study indicates that a firefighter health promotion programme designed to improve physical activity, fitness and nutrition habits was associated with reduced WC claims and medical costs among large urban fire departments in Oregon. Caution is needed in interpreting the results of this study due to the retrospective nature of the methodology and data collection. WC claims data contain total medical payments only for the specific work-related injury or illness and do not include time loss payments, lost or sick days and overtime payments. The data only represent occupational injury/illness claims and do not include non-occupational claims and costs due to difficulty with tracking this information through private insurance and individual medical providers. Thus, this dataset may actually underestimate the impact of the intervention as up to one-third of firefighter injury/illness is non-occupational and not accounted for in this sample.
Further health promotion research is needed in this area, with the ideal study design being a prospective randomized controlled trial to include a cost-benefit analysis.
Key points
Firefighting is a dangerous occupation with injury rates five to eight times higher than other workers.
Promoting Healthy Lifestyles: Alternative Models’ Effects is an evidence-based fire service wellness programme proven to improve health behaviours.
In this study the Promoting Healthy Lifestyles: Alternative Models’ Effects worksite wellness programme was associated with reduced injury rates and costs with a beneficial return on investment.
Funding
National Institute on Arthritis and Musculoskeletal and Skin Diseases (R01 45901); National Cancer Institute (R01 CA105774); and in part by US Public Health Service grant (M01 RR00334).
Conflicts of interest
The PHLAME programme is listed on the Cancer Control P.L.A.N.E.T. website of evidence-based programmes, and the PHLAME TEAM programme is distributed through the Center for Health Promotion Research at Oregon Health & Science University (OHSU). OHSU and Drs Kuehl, Goldberg, Elliot, and Moe have a financial interest from the commercial sale of technologies used in this research. This potential conflict of interest has been reviewed and managed by the OHSU Conflict of Interest in Research Committee.
References
- 1. Karter MJ, Jr, Molis JL. U.S. firefighter injuries—2011. NFPA Fire Anal Res 2012;FF110:1–27 [Google Scholar]
- 2. Bureau of Labor Statistics Workplace Injury and Illness Summary in 2010. Washington, DC: US Department of Labor, 2010 [Google Scholar]
- 3. Leigh JP. Economic burden of occupational injury and illness in the United States. Milbank Q 2011;89:728–772 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Leigh JP, Markowitz SB, Fahs M, Shin C, Landrigan PJ. Occupational injury and illness in the United States. Estimates of costs, morbidity, and mortality. Arch Intern Med 1997;157:1557–1568 [PubMed] [Google Scholar]
- 5. Walton SM, Conrad KM, Furner SE, Samo DG. Cause, type, and workers’ compensation costs of injury to fire fighters. Am J Ind Med 2003;43:454–458 [DOI] [PubMed] [Google Scholar]
- 6. Reichard AA, Jackson LL. Occupational injuries among emergency responders. Am J Ind Med 2010;53:1–11 [DOI] [PubMed] [Google Scholar]
- 7. Moore-Merrell L, Zhou A, McDonald-Valentine S, Goldstein R, Slocum C. Contributing factors to firefighter line-of-duty injury in metropolitan fire departments in the United States. Int Assoc Fire Fighters Paper 2008; 1–28 [Google Scholar]
- 8. Kales SN, Soteriades ES, Christoudias SG, Christiani DC. Firefighters and on-duty deaths from coronary heart disease: a case control study. Environ Health 2003;2:14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Kales SN, Soteriades ES, Christophi CA, Christiani DC. Emergency duties and deaths from heart disease among firefighters in the United States. N Engl J Med 2007;356:1207–1215 [DOI] [PubMed] [Google Scholar]
- 10. Aronson KJ, Tomlinson GA, Smith L. Mortality among fire fighters in metropolitan Toronto. Am J Ind Med 1994;26:89–101 [DOI] [PubMed] [Google Scholar]
- 11. Poston WS, Jitnarin N, Haddock CK, Jahnke SA, Tuley BC. Obesity and injury-related absenteeism in a population-based firefighter cohort. Obesity (Silver Spring) 2011;19:2076–2081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Karter MJ. U.S. Firefighter Injuries—2009. NFPA J 2010;9:1– 25 [Google Scholar]
- 13. Karter MJ, Molis N. United States firefighter injuries of 2005. NFPA J 2006;95:49–54 [Google Scholar]
- 14. TriData Corporation The economic consequences of firefighter injuries and their prevention. Final report. NIST GCR 05-874 2005
- 15. Chapman LS. ; American Journal of Health Promotion Inc Meta-evaluation of worksite health promotion economic return studies: 2005 update. Am J Health Promot 2005;19:1–11 [DOI] [PubMed] [Google Scholar]
- 16. Task Force on Community Preventive Services Recommendations for worksite-based interventions to improve workers’ health. A J Prev Med 38 (Suppl.2):S232–S236 [DOI] [PubMed] [Google Scholar]
- 17. Pelletier KR. A review of the clinical and cost-effectiveness studies of comprehensive health promotion and disease management programmes at the worksite: update VIII 2008 to 2010. J Occup Environ Med 2011;53:1310–1331 [DOI] [PubMed] [Google Scholar]
- 18. Pelletier K. A review and analysis of the clinical cost-effectiveness studies of comprehensive health promotion and disease management programmes at the worksite: Update VI 2000–2004. J Occup and Environ Med 2005;47:1051–1058 [DOI] [PubMed] [Google Scholar]
- 19. Pelletier K. A review and analysis of the clinical and cost-effectiveness studies of comprehensive health promotion and disease management programmes at the worksite. Am J Health Promo 2001;16:107–115 [DOI] [PubMed] [Google Scholar]
- 20. Pelletier B, Boles M, Lynch W. Change in health risks and work productivity over time. J Occup Environ Med 2004;46:746–754 [DOI] [PubMed] [Google Scholar]
- 21. International Association of Fire Fighters The Fire Service Joint Labor Management Wellness/fitness Initiative. 3rdedn. Washington, DC: International Association of Fire Fighters Department of Occupational Health and Safety, 2008 [Google Scholar]
- 22. Soteriades ES, Hauser R, Kawachi I, Christiani DC, Kales SN. Obesity and risk of job disability in male firefighters. Occup Med (Lond) 2008;58:245–250 [DOI] [PubMed] [Google Scholar]
- 23. Poston WS, Haddock CK, Jahnke SA, Jitnarin N, Tuley BC, Kales SN. The prevalence of overweight, obesity, and substandard fitness in a population-based firefighter cohort. J Occup Environ Med 2011;53:266–273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Elliot DL, Kuehl KS, Goldberg L, DeFrancesco CA, Moe EL. Worksite health promotion in six varied US sites: Beta testing as a needed translational step. J Environ Public Health 2011; 1–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Elliot DL, Goldberg L, Duncan TE, et al. The PHLAME firefighters’ study: feasibility and findings. Am J Health Behav 2004;28:13–23 [DOI] [PubMed] [Google Scholar]
- 26. Elliot DL, Goldberg L, Kuehl KS, Moe EL, Breger RK, Pickering MA. The PHLAME (Promoting Healthy Lifestyles: Alternative Models’ Effects) firefighter study: outcomes of two models of behavior change. J Occup Environ Med 2007;49:204–213 [DOI] [PubMed] [Google Scholar]
- 27. Kuehl K, Elliot D, Goldberg L, Kraemer D, McGinnis W, Breger R. The PHLAME study: Short-term economic impact of health promotion. J Investigative Medicine 2005;53:S127 [Google Scholar]
- 28. Leffer M, Grizzell T. Implementation of a physician-organized wellness regime (POWR) enforcing the 2007 NFPA standard 1582: injury rate reduction and associated cost savings. J Occup Environ Med 2010;52:336–339 [DOI] [PubMed] [Google Scholar]
- 29. Kuehl KS, Kisbu-Sakarya Y, Elliot DL, et al. Body mass index as a predictor of firefighter injury and workers’ compensation claims. J Occup Environ Med 2012;54:579–582 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Munir F, Clemes S, Houdmont J, Randall R. Overweight and obesity in UK firefighters. Occup Med (Lond) 2012;62:362–365 [DOI] [PubMed] [Google Scholar]