Abstract
Purpose:
To assess patient preference for diabetic retinopathy (DR) screening with teleophthalmology or face-to-face ophthalmologist evaluation in Nairobi, Kenya.
Materials and Methods:
Fifty seven diabetic patients from a one-stop multidisciplinary diabetic clinic (consisting of a diabetologist, nurse educator, foot specialist, nutritionist, ophthalmologist, and neurologist) in Nairobi, Kenya were included if they had undergone both a teleophthalmology (stereoscopic digital retinal photographs graded by an ophthalmologist remotely) and a traditional clinical screening exam (face to face examination). A structured questionnaire with a 5-point Likert scale was developed in both English and Swahili. The questionnaire was administered over the telephone. Ten questions were used to compare patient experience and preferences between teleophthalmology and a traditional clinical examination for DR. A mean score >3.25 on the Likert scale was considered favourable.
Results:
Successfully telephone contact was possible for 26 (58% male, 42% females) of the 57 patients. The mean ages of the male and female patients were 52.4 and 46.5 years respectively. Patients were satisfied with their teleophthalmology examination (mean 4.15 ± 0.97). Patients preferred the teleophthalmology option for future screenings (mean 3.42 ± 1.52). This preference was driven primarily by convenience, reduced examination time, and being able to visualize their own retina.
Conclusion:
In this study, diabetic patients preferred a teleophthalmology based screening over a traditional ophthalmologist-based screening. The use of teleophthalmology in Africa warrants further study and has the potential to become the screening model of choice. Cost effectiveness in comparison to an ophthalmologist-based screening also requires evaluation.
Keywords: Africa, Diabetes, Retinopathy, Teleophtalmology
INTRODUCTION
Diabetes mellitus (DM) represents one of the most common metabolic diseases worldwide.1 diabetic retinopathy (DR) is a common complication of DM that is observed in many long standing diabetics.2 In some cases, DR can lead to debilitating vision loss. Approximately 30% of the global population of diabetics have DR.2 By 2025 the prevalence of DM is expected to increase to 75% in Africa.2 Approximately 3.2% of the African population has DM and DM is expected to double by 2030. Currently, health care expenditure on DM in Africa accounts for USD 1.4 billion, and is anticipated to increase by 43% by 2030.1 From the public health perspective, there is a concern that DR presents earlier in the African population, as compared to other ethnic groups, due to the higher frequency of poorly controlled DM, hyperlipidemia, and a potential genetic predilection.2
Diabetic retinopathy is asymptomatic until advanced, hence patients with diabetes should undergo regular dilated fundus examinations. Regular screenings reduce the rate of vision loss by approximately 50%.3 The American Academy of Ophthalmology’s (AAO) preferred practice pattern for DR recommends primary eye examinations for type 1 diabetics within 5 years after diagnosis, while type 2 diabetics should be screened at the time of diagnosis.4 The AAO also recommends that follow-up examinations be performed yearly or sooner, based on the severity of DR at the initial visit.4
Telemedicine is described as “medicine at a distance,” utilizing a combination of computer equipment and innovative online communication to deliver health care to many areas of the world.5 Teleophthalmology, a form of telemedicine, allows for high quality fundus images to be uploaded to a secure server and transmitted to ophthalmologists who read the images and formulate reports used to provide ophthalmic care.6 It has been utilized globally with great success,6–11 facilitating care in underserviced, remote and rural areas.
One of the major challenges facing the developing world is the delivery of quality health care given the financial constraints and lack of trained personnel. As a solution, teleophthalmology has been implemented in various parts of the African continent.9,12 While still in its infancy, refinement of the current African teleophthalmology screening program for diabetics is needed. Patient feedback regarding their satisfaction with the current model is required to help guide the future practice of teleophthalmology in Africa. There is a relative paucity of studies evaluating patient satisfaction with teleophthalmology.6,13,14
The objective of this study was to assess diabetic patient satisfaction with teleophthalmology screening for DR and to compare it to standard face-to-face ophthalmologist screening in Nairobi, Kenya. Data from this study may help improve future ophthalmic care in the region.
MATERIALS AND METHODS
A prospective observational study was conducted to compare patient satisfaction with DR screening using teleophthalmology versus traditional ophthalmologist face-to-face screening. Research ethics board approval was granted by Aga Khan University Ethics Board. Patients were selected from a database at a one-stop multidisciplinary diabetes clinic. To be included, patients must have undergone both an ophthalmologist-based and teleophthalmology screening examination from July 2005 to July 2010. For teleophthalmology assessment at the diabetic clinic, dilated stereoscopic digital fundus images were acquired by trained nurses using the Topcon fundus camera TRC/NW100 (Topcon Corp., Tokyo, Japan). These digital images were uploaded onto the SDI (Secure Diagnostic Imaging Inc., Edmonton, Alberta, Canada) system and were reviewed and graded utilizing the modified Early Treatment Diabetic Retinopathy Study (ETDRS) criteria,15 by a local Nairobi based and trained ophthalmologist. Electronic reports were generated and included data regarding diagnosis, treatment, and follow-up recommendations, including referral for an in-person consultation. Once the reports were completed, patients were notified to return to the office, and a trained nurse reviewed the results and follow-up recommendations.
The traditional ophthalmologist based clinical examinations were performed at the multidisciplinary diabetes clinic. At this clinic, patients were evaluated by a team of health professionals for their diabetic care and complications on the same day: A diabetologist, nurse educator, foot specialist, nutritionist, ophthalmologist, and neurologist. The ophthalmologist performed a dilated eye examination and explained the findings and recommendations to the patient.
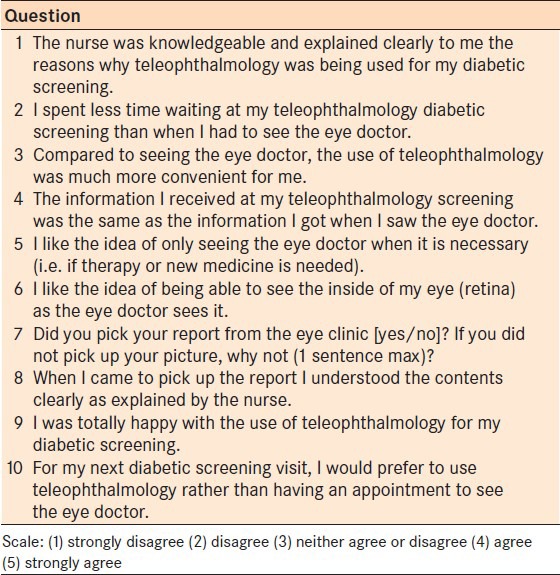
A structured patient satisfaction questionnaire with a five-point Likert scale (1. strongly disagree; 2. disagree; 3. neutral; 4. agree; 5. strongly agree), was developed in both English and Swahili. All patients who were successfully contacted agreed to participate in the study. Informed consent was obtained from all participants. A total of ten questions were utilized to assess the experience and preferences of diabetic patients between the teleophthalmology and traditional clinical consultations. An initial trial of the questionnaire was performed and validated by ensuring that questions with similar inferences had reliable answers.6 The questionnaire was then administered over the telephone by a trained nurse or medical student, and responses were recorded on individual data sheets.
Each question from the questionnaire was analyzed independently from the other. Only question 7 was not based on the Likert scale. Question 7 was used to assess issues surrounding patient compliance to our screening program. An excel (Microsoft Corp., Redmond, WA, USA) spreadsheet was used to compile the data and SAS (version 9.2, SAS Institute Inc., Cary, NC, USA) was used for all analyses. For each question, a mean score >3.25 on the Likert scale was considered favourable. Satisfaction was defined as being completely happy with their experience. In order to calculate percentages, individuals who responded favorably to a question with a 4 or higher on the Likert scale were grouped together for analyses. Conversely, individuals who responded unfavorably to a question with a 2 or lower on the Likert scale were grouped together for analyses.
RESULTS
Of the total fifty seven patients that fit the selection criteria, 26 [15 male (58%), 11 females (42%)] were successfully contacted by telephone. Such a small number may be due to the numerous landscape of issues facing East Africans (i.e. low number and maldistribution of medical specialist, low literacy level for the population, low medical insurance coverage, challenges in transport communication, low availability of diagnostic and treatment equipment, and medications). The mean ages of male and female patients were 52.4 and 46.5 years respectively.
In the entire study cohort, 62% believed that the trained nurse clearly explained the rationale for undergoing the teleophthalmology screening. Another 42% of patients felt that the information they received at the teleophthalmology screening was similar to the information they received at their in-person ophthalmology exam. In terms of preference for an in-person examination for every visit, 65% of patients preferred to only see the ophthalmologist when necessary. In all, 15 patients (58%) returned to the clinic to pick up a copy of their teleophthalmology report [Table 1; Question 7], of which 87% (n = 13) believed that their results and corresponding recommendations were clearly explained by the nurse.
Table 1.
Patient satisfaction/preferences questionnaire
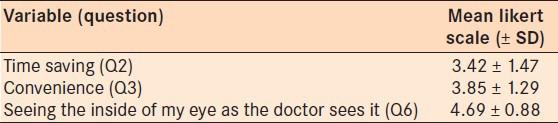
In terms of their overall experience, patients were quite satisfied with the teleophthalmology screen [Table 2; Question 9]. Specifically, patients were satisfied with the information that they received from the teleophthalmology nurse [Table 2; Questions 1 and 8] and with the consistency of the information received at either type of consultation [Table 2; Question 4]. Furthermore, patients preferred to use teleophthalmology as their method of choice for diabetic eye screening in the future. Patients cited the saved time, convenience and the ability to view the inside of their eye as the ophthalmologist sees it as reasons that they favoured the use of teleophthalmology [Table 3].
Table 2.
Patient satisfaction and preferences for the use of teleophthalmology-based screening
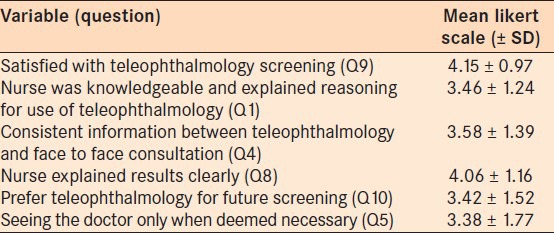
Table 3.
Patient responses regarding the benefits of teleophthalmology-based screening
DISCUSSION
One of the emerging tools in the current healthcare system is the advent of telemedicine, which affords physicians the ability to provide high quality care to patients worldwide. Teleophthalmology has been utilized effectively to provide ophthalmic screening, diagnosis, ongoing monitoring and management of various eye conditions including glaucoma, age-related macular degeneration and DR.6 The use of teleophthalmology allows ophthalmologists to provide eye care to patients who may not necessarily be located in the same geographical area. This allows ophthalmic services to be delivered to remote, rural underserviced areas.13,14 While, teleophthalmology offers several advantages there are several challenges in East Africa. One challenge is whether or not teleophthalmology is actually cost effective in the region, and whether the benefits of improving access to eye services actually outweighs the cost of establishing such sustainable programs. Teleophthalmology offers some obvious efficiency and cost saving implications including: (1) The stereoscopic photos can be taken quickly and on time rather than have the patient wait for the ophthalmologist to become available, (2) The ophthalmologist does not have to be present to do the exam and can be free to do other activities and report on the stereoscopic pictures at appropriate time, (3) The actual cost of the photography session is lower than if ophthalmologist had to be present. We hope to perform large scale studies in the near future to assess the cost-effectiveness of our current teleophthalmology practice in the region in comparison to the standard in person-based screening examination.
Patient preferences and satisfaction are important for implementing a new examination technique such as teleophthalmology, as these opinions will help shape and improve the model. Currently there are a handful of studies comparing patient satisfaction between face-to-face consultations and telemedicine.6,16 In 2006, Kumari Rani and colleagues,6 noted that 99% of their patients were satisfied with their teleophthalmology screening. Another study showed similar levels of satisfaction (94%) with teleophthalmology screening.13 The outcomes of the current study concur, as we observed 88% of our patients were completely satisfied with teleophthalmology.
When asked whether they would prefer teleophthalmology as their screening method of choice in the future, 58% of our patients preferred the use of teleophthalmology. Other studies have also shown similar preferences for the use of teleophthalmology for future ophthalmic screenings.6,13,14 In the current study, patient preference for teleophthalmology was driven primarily by convenience (73%) and decreased consultation time (58%). Previous studies evaluating patient satisfaction with teleophthalmology have reported similar reasons and the reduction in cost, travel time, time off work, and increased assess to clinical support.13,14,17
Interestingly, the most substantive benefit perceived by 85% of our patients was being able to visualize the inside of their eye exactly as the doctor sees it; i.e. a fundoscopic image. Visual aids improve comprehension of the disease process and increased adherence to treatment recommendations, specifically amongst the elderly population and those with limited literacy.18 Nevertheless, while most of the patients in this study expressed a preference to see the images of their eye, only 58% actually returned to pick up and discuss their reports with trained nurses. This outcome may seem adequate to some considering the plethora of issues facing East Africans including the low number and inadequate distribution of medical specialists, low literacy of the population, low medical insurance coverage, challenges in transport and communication, low availability of diagnostic and treatment equipment, and medications. However we believe this is not an acceptable outcome, as the entire emphasis of the teleophthalmology program is to improve the access and quality of patient eye care in the region. Some of the reasons offered by patients who did not pick up their reports included: “Did not know I had to pick it up,” “I thought I would just pick it up next time I came in,” “did not really care to go over it.” The utilization of more convenient avenues of communicating reports (i.e. registered mail, secure electronic mail), may improve patient adherence to our screening program.
The use of teleophthalmology needs greater exploration in Sub Saharan Africa and has the potential for becoming the screening model of choice, particularly in enhancing access to expert care, as well as improving efficiency of care for underserviced populations. While a low volume of participants were surveyed in our study, the feedback gathered from this study will help ophthalmologists in the region to shape and improve existing teleophthalmology services. As the program continues to expand and evolve, the number of patients accessing teleophthalmology services will continue to grow and in turn, response rates for future satisfaction studies will increase. The use of teleophthalmology in East Africa has undoubtedly vast implications and has the potential to be expanded to include services such as mobile screening vans, which would further allow patients all over East Africa increased access to high quality ophthalmic care.
ACKNOWLEDGEMENT
The authors are thankful to Ophthalmology nurses Beatrice Nyaga and Florence Mutisya and diabetic nurse Lillian Gachago for their time and help in gathering the data and translating the questionnaire into the local language. We are also thankful to the diabetologist Dr. Nancy Kunyiha for coordinating the collaboration for the diabetic eye care.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.IDF Diabetes Atlas. 4th ed. Brussels, Belgium: International Diabetes Federation; 2009. [Last accessed on July 1]. International Diabetes Federation. Available from: http://www.idf.org/diabetesatlas . [Google Scholar]
- 2.Guigui S, Lifshitz T, Levy J. Diabetic retinopathy in Africa: Advantages of screening. Postgrad Med. 2011;123:119–25. doi: 10.3810/pgm.2011.07.2311. [DOI] [PubMed] [Google Scholar]
- 3.Singer DE, Nathan DM, Fogel HA, Schachat AP. Screening for diabetic retinopathy. Ann Intern Med. 1992;116:660–71. doi: 10.7326/0003-4819-116-8-660. [DOI] [PubMed] [Google Scholar]
- 4.Diabetic Retinopathy. San Francisco, CA: American Academy of Ophthalmology; 2008. [Last accessed on July 3]. American Academy of Ophthalmology Retina Panel. Preferred Practice Pattern® Guidelines. Available from: http://www.aao.org/ppp . [Google Scholar]
- 5.Sibson L, Dunn R, Evans J, Jones R, Hayward M, Wallace S. The virtual mole clinic: Preliminary results from the Plymouth skin cancer screening study using telemedicine. Med Inform Internet Med. 1999;24:189–99. doi: 10.1080/146392399298393. [DOI] [PubMed] [Google Scholar]
- 6.Kumari Rani P, Raman R, Manikandan M, Mahajan S, Paul PG, Sharma T. Patient satisfaction with teleophthalmology versus ophthalmologist-based screening in diabetic retinopathy. J Telemed Telecare. 2006;12:159–60. doi: 10.1258/135763306776738639. [DOI] [PubMed] [Google Scholar]
- 7.Ng M, Nathoo N, Rudnisky CJ, Tennant MT. Improving access to eye care: Teleophthalmology in Alberta, Canada. J Diabetes Sci Technol. 2009;3:289–96. doi: 10.1177/193229680900300209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Boucher MC, Desroches G, Garcia-Salinas R, Kherani A, Maberley D, Olivier S, et al. Teleophthalmology screening for diabetic retinopathy through mobile imaging units within Canada. Can J Ophthalmol. 2008;43:658–68. doi: 10.3129/i08-120. [DOI] [PubMed] [Google Scholar]
- 9.Jivraj I, Ng M, Rudnisky CJ, Dimla B, Tambe E, Nathoo N, et al. Prevalence and severity of diabetic retinopathy in Northwest Cameroon as identified by teleophthalmology. Telemed J E Health. 2011;17:294–8. doi: 10.1089/tmj.2010.0155. [DOI] [PubMed] [Google Scholar]
- 10.Gonzalez F, Castro AF. Publication output in telemedicine in Spain. J Telemed Telecare. 2005;11:23–8. doi: 10.1177/1357633X0501100106. [DOI] [PubMed] [Google Scholar]
- 11.Finamor LP, Martins MC, Muccioli C, Singulem D, Lopes PR, Belfort R., Jr Teleophthalmology as an auxiliary approach for the diagnosis of infectious and inflammatory ocular diseases: Evaluation of an asynchronous method of consultation. Rev Assoc Med Bras. 2005;51:279–84. doi: 10.1590/s0104-42302005000500020. [DOI] [PubMed] [Google Scholar]
- 12.Johnston K, Kennedy C, Murdoch I, Taylor P, Cook C. The cost-effectiveness of technology transfer using telemedicine. Health Policy Plan. 2004;19:302–9. doi: 10.1093/heapol/czh035. [DOI] [PubMed] [Google Scholar]
- 13.Luzio S, Hatcher S, Zahlmann G, Mazik L, Morgan M, Liesenfeld B, et al. Feasibility of using the TOSCA telescreening procedures for diabetic retinopathy. Diabet Med. 2004;21:1121–8. doi: 10.1111/j.1464-5491.2004.01305.x. [DOI] [PubMed] [Google Scholar]
- 14.Tuulonen A, Ohinmaa T, Alanko HI, Hyytinen P, Juutinen A, Toppinen E, et al. The application of teleophthalmology in examining patients with glaucoma: A pilot study. J Glaucoma. 1999;8:367–73. [PubMed] [Google Scholar]
- 15.Rudnisky CJ, Tennant MT, Weis E, Ting A, Hinz BJ, Greve MD. Web-based grading of compressed stereoscopic digital photography versus standard slide film photography for the diagnosis of diabetic retinopathy. Ophthalmology. 2007;114:1748–54. doi: 10.1016/j.ophtha.2006.12.010. [DOI] [PubMed] [Google Scholar]
- 16.Williams TL, May CR, Esmail A. Limitations of patient satisfaction studies in telehealthcare: A systematic review of the literature. Telemed J E Health. 2001;7:293–316. doi: 10.1089/15305620152814700. [DOI] [PubMed] [Google Scholar]
- 17.Kumar S, Yogesan K, Hudson B, Tay-Kearney ML. Internetbased electronics eye care consultations: Patient perspective. In: Yogesan K, Kumar S, Goldschmidth L, Cuadros J, editors. Tele-ophthalmology. Springer: Verlag; 2008. pp. 133–38. [Google Scholar]
- 18.Katz MG, Kripalani S, Weiss BD. Use of pictorial aids in medication instructions: A review of the literature. Am J Health Syst Pharm. 2006;63:2391–7. doi: 10.2146/ajhp060162. [DOI] [PubMed] [Google Scholar]


