Abstract
Objectives. We compared childbirth-related outcomes for Medicaid recipients who received prenatal education and childbirth support from trained doulas with outcomes from a national sample of similar women and estimated potential cost savings.
Methods. We calculated descriptive statistics for Medicaid-funded births nationally (from the 2009 Nationwide Inpatient Sample; n = 279 008) and births supported by doula care (n = 1079) in Minneapolis, Minnesota, in 2010 to 2012; used multivariate regression to estimate impacts of doula care; and modeled potential cost savings associated with reductions in cesarean delivery for doula-supported births.
Results. The cesarean rate was 22.3% among doula-supported births and 31.5% among Medicaid beneficiaries nationally. The corresponding preterm birth rates were 6.1% and 7.3%, respectively. After control for clinical and sociodemographic factors, odds of cesarean delivery were 40.9% lower for doula-supported births (adjusted odds ratio = 0.59; P < .001). Potential cost savings to Medicaid programs associated with such cesarean rate reductions are substantial but depend on states’ reimbursement rates, birth volume, and current cesarean rates.
Conclusions. State Medicaid programs should consider offering coverage for birth doulas to realize potential cost savings associated with reduced cesarean rates.
In 2009, 4.1 million babies were born in US hospitals.1 Childbirth is the most frequent reason for hospitalization in the United States, and charges for maternity and newborn care exceed those for any other category of hospital expense for both public and private payers.2 Hospital costs for childbirth totaled $27.6 billion in 2009,3 and state Medicaid programs paid for 45% of all US births that year, indicating an extraordinary public-sector investment in hospital-based childbirth care.3,4
Costs are higher for cesarean deliveries and for births with clinical complications.5,6 Delivery-related complications are increasingly common and occur with highest frequency among women of color and low-income women.7,8 Racial/ethnic minorities have higher rates of cesarean delivery and worse birth outcomes than their White counterparts.9,10 Medicaid beneficiaries have a higher risk of preterm birth (< 37 weeks gestation) and low birth weight (< 2500 g) than do privately insured women.11,12 The strong link between income, race/ethnicity, and adverse birth outcomes has been well documented,13–15 but effective means of reducing this disparity are lacking.16 In a time of increasing fiscal pressures on health care systems and state Medicaid budgets, the need to stem the rising cost of maternity care is urgent.4,17
The sizeable public health and financial stake in childbirth care has engendered a growing interest in potential clinical models and policy tools that payers, hospitals, and health care providers can employ to achieve the triple aim of improved patient outcomes and better population health at lower cost.17,18 The midwifery model of maternity care and freestanding birth centers have shown great promise,19 as have home-visiting programs.20,21 Provisions of the Affordable Care Act are designed to increase access to these services via Medicaid coverage, among other policy tools.22,23 Another type of low-intervention care is continuous labor support from a birth doula, a type of care that is not typically reimbursed by health insurance.24
Unlike physicians, midwives, and obstetrical nurses, who provide medical care, doulas provide support in the nonmedical aspects of labor and delivery.25,26 The Doula Organization of North America (DONA), the largest organization of certified doulas, defines a birth doula as a “person trained and experienced in childbirth who provides continuous physical, emotional and informational support to the mother before, during and just after birth.”27 Randomized controlled trials provide strong evidence for the clinical benefits of continuous labor support.28,29 A recent Cochrane systematic review of the effects of continuous labor support revealed higher rates of spontaneous vaginal birth and lower odds of cesarean delivery, lower rates of regional anesthesia (e.g., epidural), lower rates of instrument-assisted delivery (i.e., forceps and vacuum), shorter labors, and higher levels of satisfaction among women who received labor support.28 The review indicated that labor support was most effective when provided by an individual such as a doula, who was not on the hospital’s staff and was not a family member or close friend without specialized training.28
In the United States, most doulas are middle-aged, married, and well-educated White women from upper-middle-class households.24 Although limited information is available about the characteristics of women who use doula care, it is likely that lack of insurance coverage for these services restricts financial access for low-income women, and limited racial/ethnic diversity of doulas (84% are White) may also influence the diversity of potential clients.24,30 In the US context, observational associations between doula care and positive birth outcomes may reflect a population of women with greater resources, better health status, and specific birth experience intentions or higher-risk women with access to doula care through a specific program or intervention.31,32
Although the clinical benefits of doula services have been well documented, few studies have examined doula care in a policy context, where legislators debate statutory changes, administrators implement programs, regulators oversee enforcement, and payers make coverage and benefits decisions and negotiate reimbursement rates with providers. Limited research explores doula care among the low-income and racially/ethnically diverse women who compose approximately half of the US childbearing population and are at elevated risk for adverse birth outcomes and poor obstetric care quality.10 We compared childbirth-related outcomes for racially/ethnically diverse Medicaid recipients who received prenatal education and childbirth support from trained doulas with those for a national population of similar women and estimated potential cost savings associated with offering coverage for birth doula care as a Medicaid benefit.
METHODS
Everyday Miracles is a group of doulas operating as a nonprofit organization with the goal of improving birth outcomes, parent–infant attachment, and breastfeeding skills. Everyday Miracles clients are referred through a Medicaid managed care plan and receive childbirth and breastfeeding education, continuous labor support, and prenatal and postpartum care from trained doulas at no out-of-pocket expense. From 2010 to 2012, Everyday Miracles employed 22 active doulas, all of whom completed DONA training requirements and were either DONA certified or working toward certification. DONA training requires completing a minimum of 28 hours of structured classroom instruction (≥ 16 hours in a DONA International–approved training workshop and ≥ 12 hours in an accredited childbirth education series), reading at least 5 books from the DONA International Birth Doula Required Reading List, and completing coursework in breastfeeding support or becoming a certified lactation consultant. Certification requires that the doula pass a written exam and apprentice for at least 3 births (≥ 2 of which must be vaginal deliveries), and develop an extensive referral network and listing of local support resources. This comprehensive training and certification process is described in detail on DONA’s training Web site (http://www.dona.org/develop/certification.php).
Everyday Miracles makes a concerted effort to match doulas with clients on race/ethnicity and language and to recruit, train, and hire doulas with this goal in mind. The doulas were therefore distinctive in their diversity. As of 2012, 12 were White, 4 Latino, 3 Somali, 2 Hmong, and 1 Black, with limited turnover during the study period.
DATA AND STUDY POPULATION
The study population comprised 2 groups: women who had Medicaid-funded singleton births nationwide (n = 279 008) and Medicaid beneficiaries whose labor and delivery were supported by doula care provided by Everyday Miracles (n = 1079).
We used data from 279 008 childbirth hospitalizations for singleton births in 44 states, where the primary payer was Medicaid, from the 2009 Nationwide Inpatient Sample (NIS), Healthcare Cost and Utilization Project (HCUP) Agency for Healthcare Research and Quality. The NIS is an all-payer inpatient claims database designed to approximate a 20% stratified sample of US hospitals.33 We also obtained state-level HCUP data on all Medicaid-funded deliveries, including hospital charges for Medicaid-funded births associated with relevant diagnosis-related groups, from HCUPNet,34 which generates estimates from the Statewide Inpatient Databases, a census of inpatient claims for participating states. To enable the conversion of hospital charges into costs of providing care, we used regional estimates of cost-to-charge ratios5 and applied the appropriate regional conversion factor to each of the 35 states for which data on charges were available in 2009.
Data on doula-supported births came from de-identified reports of routinely collected client services utilization information for women served by Everyday Miracles doulas. Doulas filled out standardized enrollment and childbirth data forms, and trained interns entered data for our study into an Excel spreadsheet (Microsoft, Redmond, WA); Everyday Miracles management and study investigators verified accuracy prior to data analysis. We used information for the 1079 women served by Everyday Miracles who delivered singleton babies between January 1, 2010, and April 30, 2012, all of whom were Medicaid recipients.
We used all available data from both sources for analysis: every singleton US birth in 2009 found in the HCUP NIS (for outcomes) or HCUPNet (for costs) for which Medicaid was the primary payer and every singleton birth attended by Everyday Miracles doulas from January 2010 through April 2012.
Variables
We derived variables from administrative data collected by Everyday Miracles or by hospitals (and compiled by HCUP). Primary outcomes of interest were cesarean delivery and preterm birth, extracted from the Everyday Miracles childbirth data form. In HCUP NIS data, we used International Classification of Diseases, Ninth Revision procedure codes to identify cesarean delivery (740X, 741X, 742X, 744X, 7499) and preterm delivery (6442, 64420, 64421).35 For cesarean delivery we also used diagnosis-related groups payment codes (370, 371).36 These methods have been validated and are consistent with previous research with HCUP data.37,38
We also measured maternal age, race/ethnicity, and 2 major pregnancy-related complications, hypertension and diabetes. Maternal age and race/ethnicity were self-reported. Everyday Miracles distinguishes US-born and African-born Black women, because this distinction is relevant in the local context. We presented information for each of these groups, as well as combined results for all Black women for comparability with national estimates. Hypertension and diabetes were identified by patient report for doula data and by Clinical Classification System code 183 (hypertension) and 196 (diabetes) in HCUP NIS data.39
We handled missing data within the HCUP NIS according to established procedures defined in the HCUP Agency for Healthcare Research and Quality protocols and descriptions of data elements.33 We identified study outcomes and clinical variables from payment, diagnosis, and procedure codes, which were validated and complete. For sociodemographic factors, only race/ethnicity was missing in significant quantity (> 5%) in NIS data. When no race/ethnicity information was available, we classified race/ethnicity as missing for that individual. We conducted a sensitivity analysis that controlled separately for missing values in race/ethnicity variables (results remained consistent). No data were missing among doula-supported births because the administrative procedures used by Everyday Miracles required that doulas report information for each of the variables in our analysis.
Analysis
We calculated means and 95% confidence intervals (CIs) for maternal characteristics, delivery mode, and birth outcomes for women whose singleton births were funded by Medicaid and supported by doula care (n = 1079) and for a national sample of women with Medicaid-funded singleton births (n = 279 008). We used the t test to evaluate rate differences. We used multivariate logistic regression models to estimate the impact of doula support on delivery mode and preterm birth, with adjustment for maternal age, race/ethnicity, and clinical complications among Medicaid recipients. All women in our samples had health insurance through Medicaid for their childbirth, and thus all met income eligibility thresholds, ensuring some consistency of socioeconomic status and health care access across the populations.
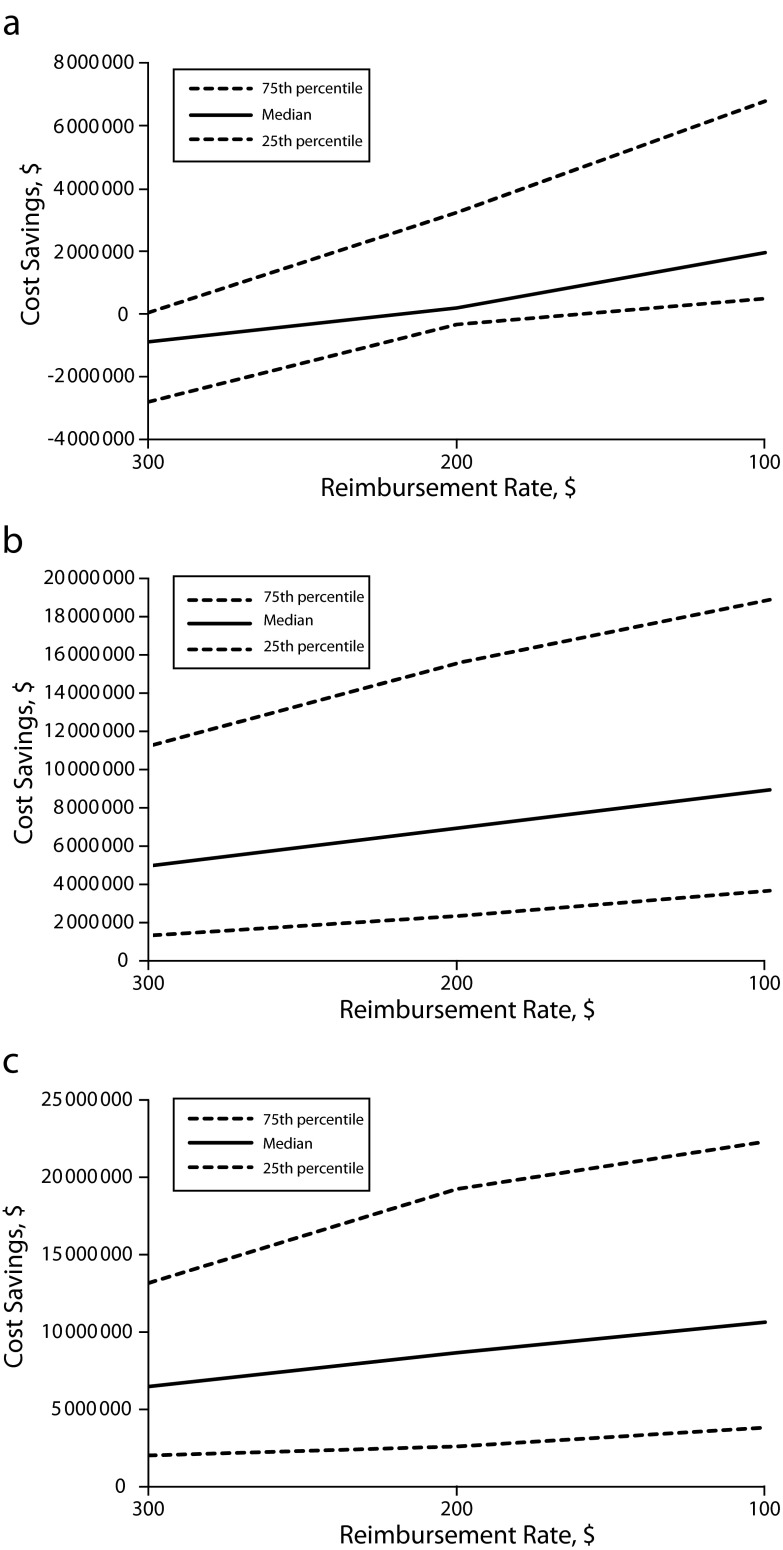
To assess the potential cost impacts of changes in delivery mode that may be associated with Medicaid reimbursement for continuous labor support from a trained doula, we used state-level data on Medicaid-funded births and associated costs and cesarean rates to model 3 different policy scenarios across a range of birth doula reimbursement rates ($100–$300; this range would reimburse for providing intrapartum support at the time of childbirth; other aspects of doula care, such as prenatal education and postpartum breastfeeding support, are separately reimbursed). The policy scenarios focused on intrapartum labor support and delivery mode (cesarean vs vaginal) and the potential costs and savings for a childbirth hospitalization from a payer perspective.
Scenario 1 modeled the potential annual cost savings to a state of reducing the cesarean rate to the rate experienced in doula-supported Medicaid births in our analysis (22.3%). Alternatively, we modeled scenarios in which birth doula reimbursement was associated with a certain percentage reduction in cesarean rates, derived from results from multivariate regression models. Scenario 2 calculated the state-level annual cost savings of reducing the cesarean rate for Medicaid-funded births by the percentage indicated by the adjusted odds ratios (AORs) produced via regression models, and scenario 3 calculated cost reductions associated with the percentage drop in cesarean rates indicated by the upper bound of the 95% CIs around the estimate used for scenario 2 (a more conservative estimate of the difference between the doula-supported births and all Medicaid births in this study). To facilitate interpretation, we divided states into quartiles, according to potential cost impacts under each of the 3 scenarios, and estimated the median annual state cost savings, as well as the 25th and 75th percentile for birth doula reimbursement rates from $100 to $300. We conducted all analyses with SAS version 9.3 (SAS Institute Inc, Cary, NC).
RESULTS
The characteristics of pregnant Medicaid beneficiaries who received doula care were broadly similar to the general population of women whose births were covered by Medicaid (Table 1). However, women supported by doulas were more racially/ethnically diverse, were slightly older (27 vs 25 years), and had lower reported rates of gestational hypertension (3.8% vs 7.8%). Medicaid-funded births to women with doula support had a cesarean rate of 22.3% (95% CI = 19.8, 24.8), significantly lower than the cesarean rate in the general Medicaid population of 31.5% (95% CI = 31.3, 31.6). The average preterm birth rate was lower for women who received doula support than for Medicaid beneficiaries generally (6.1% vs 7.3%), but this difference was not statistically significant in uncontrolled comparisons.
TABLE 1—
Characteristics of Hospital-Based, Medicaid-Funded Singleton Births, Nationally in 2009 and With Doula Support Among a Cohort in Minneapolis, MN, 2010–2012
| Characteristic | Medicaid-Funded Deliveries (n = 279 008), Mean (95% CI) | Medicaid-Funded Deliveries With Doula Support (n = 1079), Mean (95% CI) | Difference |
| Maternal | |||
| Age, y | 25.1 (25.1, 25.2) | 27.3 (26.9, 27.6) | 2.1* |
| Pregnancy-related complications, % | |||
| Hypertension | 7.8 (7.7, 7.9) | 3.8 (2.7, 5.0) | −4.0* |
| Diabetes | 6.1 (6.0, 6.2) | 5.8 (4.4, 7.2) | −0.3 |
| Race/ethnicity, % | |||
| Asian | 3.0 (2.9, 3.0) | 5.6 (4.2, 7.0) | 2.6* |
| Black (total) | 20.2 (20.1, 20.4) | 46.3 (43.3, 49.3) | 26.1* |
| US-born Black | NA | 10.3 (8.5, 12.2) | NA |
| African-born Black | NA | 35.9 (33.1, 38.8) | NA |
| White | 38.8 (38.6, 39.0) | 10.2 (8.4, 12.1) | −28.6* |
| Hispanic | 38.0 (37.8, 38.2) | 36.2 (33.3, 39.1) | −1.8 |
| Labor and delivery | |||
| Cesarean delivery, % | 31.5 (31.3, 31.6) | 22.3 (19.8, 24.8) | −9.2* |
| Medication use, % | |||
| Epidural | NA | 27.9 (25.2, 30.6) | NA |
| Other pain medicine | NA | 19.9 (17.5, 22.3) | NA |
| Birth outcomes, % | |||
| Low birth weight | NA | 4.2 (3.0, 5.4) | NA |
| Preterm birth | 7.3 (7.2, 7.4) | 6.1 (4.7, 7.6) | −1.2 |
Note. CI = confidence interval; NA = not available in data set.
*P < .05.
We also calculated AORs for the association between doula care and study outcomes, with control for maternal race/ethnicity and age and for clinical complications (Table 2). Average cesarean rates were significantly lower in doula-supported Medicaid births than in Medicaid-funded births generally; doula care was associated with a 40.9% decreased odds of cesarean delivery (AOR = 0.59; 95% CI = 0.51, 0.68; P < .001). Preterm birth rates were also lower among doula-supported than among all Medicaid-funded births, but this difference was not statistically significant (AOR = 0.81; 95% CI = 0.63, 1.04). Other factors associated with higher preterm and cesarean delivery rates were Black race, older maternal age, maternal hypertension, and maternal diabetes. Hispanic and Asian women had lower preterm birth and cesarean delivery rates than did White women.
TABLE 2—
Odds of Adverse Birth Outcomes for Hospital-Based, Medicaid-Funded, Singleton Births Nationally in 2009 and Supported by Doulas Among a Cohort in Minneapolis, MN, 2010–2012, With Control for Demographic and Clinical Factors
| Preterm Birth, AOR (95% CI) | Cesarean Delivery, AOR (95% CI) | |
| Doula support | 0.81 (0.63, 1.04) | 0.59 (0.51, 0.68) |
| Race/ethnicity | ||
| Asian | 0.84 (0.77, 0.93) | 0.78 (0.74, 0.82) |
| Black | 1.42 (1.37, 1.47) | 1.07 (1.04, 1.09) |
| Hispanic | 0.85 (0.82, 0.88) | 0.96 (0.94, 0.97) |
| White (Ref) | 1.00 | 1.00 |
| Age, y | ||
| < 20 | 1.06 (1.02, 1.11) | 0.68 (0.67, 0.70) |
| 21–25 | 1.01 (0.97, 1.04) | 0.95 (0.93, 0.97) |
| 26–30 (Ref) | 1.00 | 1.00 |
| 31–35 | 1.08 (1.03, 1.13) | 1.28 (1.25, 1.31) |
| ≥ 36 | 1.22 (1.15, 1.30) | 1.54 (1.49, 1.59) |
| Pregnancy-related complications | ||
| Hypertension | 2.32 (2.23, 2.42) | 1.89 (1.83, 1.94) |
| Diabetes | 1.50 (1.42, 1.58) | 1.75 (1.69, 1.81) |
Note. AOR = Adjusted odds ratio; CI = confidence interval. Sample size = 280 087.
With 3 scenarios generated by empirically driven assumptions, we simulated annual cost impacts to state Medicaid programs that might result from a reduction in cesarean delivery rates associated with reimbursement of birth doula services. Table 3 provides detailed state-level information on these calculations, with the number of Medicaid-funded births, the cesarean rate for Medicaid-funded births, the total annual Medicaid payments to hospitals for childbirth, and the potential cost impacts associated with the scenarios. We used this information to calculate the cost impacts shown in Figure 1.
TABLE 3—
Estimated Annual Savings to State Medicaid Programs Resulting From Reduction in Cesarean Delivery Rates Associated With Doula Services Among a Cohort in Minneapolis, MN, 2010–2012, by Reimbursement Rate
| State | Medicaid Births in 2009, No. | Cesarean Deliveries in 2009 Medicaid Births, % | Estimated 2009 Medicaid Payments to Hospitals for Childbirth, $ | Scenario 1: Savings With 22.3% Cesarean Rate, by Birth Doula Reimbursement Amounta |
Scenario 2: Savings With Cesarean Rate Reduced by 40.8%, Birth Doula by Reimbursement Amountb |
Scenario 3: Savings With Cesarean Rate Reduced by 31.6%, by Birth Doula Reimbursement Amountc |
||||||
| $300, $ | $200, $ | $100, $ | $300, $ | $200, $ | $100, $ | $300, $ | $200, $ | $100, $ | ||||
| Arkansas | 21 602 | 34.14 | 159 693 579 | −483 963 | 1 676 237 | 3 836 437 | 573 980 | 2 734 180 | 4 894 380 | −1 016 759 | 1 143 441 | 3 303 641 |
| Arizona | 44 884 | 26.61 | 282 710 234 | −6 249 819 | −1 761 419 | 2 726 981 | 12 925 801 | 17 414 201 | 21 902 601 | 17 027 105 | 21 515 505 | 26 003 905 |
| California | 246 439 | 32.27 | 2 277 662,653 | 50 386 316 | 75 030 216 | 99 674 116 | 164 350 905 | 188 994 805 | 213 638 705 | 201 381 310 | 226 025 210 | 250 669 110 |
| Colorado | 24 068 | 23.64 | 147 560 306 | −5 975 935 | −3 569 135 | −1 162 335 | 5 764 379 | 8 171 179 | 10 577 979 | 7 782 284 | 10 189 084 | 12 595 884 |
| Florida | 110 864 | 36.75 | 1 400 051,280 | 14 438 204 | 25 524 604 | 36 611 004 | 38 552 970 | 49 639 370 | 60 725 770 | 49 712 969 | 60 799 369 | 71 885 769 |
| Hawaii | 6140 | 25.73 | 29 066 661 | −1 297 455 | −683 455 | −69 455 | 574 480 | 1 188 480 | 1 802 480 | 950 014 | 1 564 014 | 2 178 014 |
| Illinois | 74 646 | 28.86 | 526 716 590 | −892 110 | 6 572 490 | 14 037 090 | 33 595 754 | 41 060 354 | 48 524 954 | −11 420 838 | 49 761 433 | 57 226 033 |
| Iowa | 13 824 | 28.76 | 65 393 014 | −1 194 848 | 187 552 | 1 569 952 | 3 632 524 | 5 014 924 | 6 397 324 | 4 841 536 | 6 223 936 | 7 606 336 |
| Kansas | 12 141 | 30.04 | 75 733 972 | −698 119 | 515 981 | 1 730 081 | 3 123 183 | 4 337 283 | 5 551 383 | 4 174 576 | 5 388 676 | 6 602 776 |
| Kentucky | 25 160 | 35.72 | 117 429 199 | 383 699 | 2 899 699 | 5 415 699 | 4 948 224 | 7 464 224 | 9 980 224 | 6 890 205 | 9 406 205 | 11 922 205 |
| Maine | 6012 | 28.59 | 24 158 540 | −575 940 | 25 260 | 626 460 | 1 498 663 | 2 099 863 | 2 701 063 | 2 011 853 | 2 613 053 | 3 214 253 |
| Maryland | 27 654 | 30.52 | 95 050 379 | −5 777 767 | −3 012 367 | −246 967 | −2 760 597 | 4803 | 2 770 203 | −1 900 334 | 865 066 | 3 630 466 |
| Massachusetts | 23 570 | 29.64 | 117 520 821 | −2 763 357 | −406 357 | 1 950 643 | 3 227 441 | 5 584 441 | 7 941 441 | 4 827 875 | 7 184 875 | 9 541 875 |
| Michigan | 48 311 | 30.12 | 262 689 941 | −2 711 439 | 2 119 661 | 6 950 761 | 12 362 426 | 17 193 526 | 22 024 626 | 16 535 951 | 21 367 051 | 26 198 151 |
| Minnesota | 8591 | 26.49 | 53 775 975 | −972 856 | −113 756 | 745 344 | 3 424 292 | 4 283 392 | 5 142 492 | 4 356 972 | 5 216 072 | 6 075 172 |
| Missouri | 34 177 | 30.21 | 209 320 982 | −1 499 651 | 1 918 049 | 5 335 749 | 9 542 950 | 12 960 650 | 16 378 350 | 12 619 363 | 16 037 063 | 19 454 763 |
| Nebraska | 7944 | 29.66 | 40 180 116 | −98 398 | 696 002 | 1 490 402 | 3 068 977 | 3 863 377 | 4 657 777 | 3 916 275 | 4 710 675 | 5 505 075 |
| Nevada | 11 087 | 31.50 | 67 596 255 | 858 921 | 1 967 621 | 3 076 321 | 5 159 140 | 6 267 840 | 7 376 540 | 6 477 792 | 7 586 492 | 8 695 192 |
| New Hampshire | 3990 | 28.05 | 17 844 658 | −669 029 | −270 029 | 128 971 | 328 775 | 727 775 | 1 126 775 | 565 889 | 964 889 | 1 363 889 |
| New Mexico | 14 454 | 21.88 | 62 430 527 | −4 513 493 | −3 068 093 | −1 622 693 | 1 174 588 | 2 619 988 | 4 065 388 | 2 030 995 | 3 476 395 | 4 921 795 |
| New Jersey | 23 598 | 32.41 | 270 147 800 | 4 694 952 | 7 054 752 | 9 414 552 | 15 260 199 | 17 619 999 | 19 979 799 | 18 731 894 | 21 091 694 | 23 451 494 |
| New York | 97 092 | 31.45 | 507 671 529 | −6 152 894 | 3 556 306 | 13 265 506 | 17 611 710 | 27 320 910 | 37 030 110 | 24 875 251 | 34 584 451 | 44 293 651 |
| North Carolina | 59 127 | 28.60 | 282 968 323 | −6 553 980 | −641 280 | 5 271 420 | 12 302 297 | 18 214 997 | 24 127 697 | 16 970 737 | 22 883 437 | 28 796 137 |
| Oklahoma | 28 670 | 33.71 | 168 520 929 | 868 831 | 3 735 831 | 6 602 831 | 7 960 776 | 10 827 776 | 13 694 776 | 10 534 566 | 13 401 566 | 16 268 566 |
| Oregon | 19 779 | 28.31 | 98 998 489 | −2 016 382 | −38 482 | 1 939 418 | 4 986 067 | 6 963 967 | 8 941 867 | 6 683 058 | 8 660 958 | 10 638 858 |
| Rhode Island | 5144 | 28.34 | 40 126 480 | −415 515 | 98 885 | 613 285 | 1 587 656 | 2 102 056 | 2 616 456 | 2 074 208 | 2 588 608 | 3 103 008 |
| South Carolina | 23 166 | 33.24 | 151 860 595 | 2 503 200 | 4 819 800 | 7 136 400 | 10 050 775 | 12 367 375 | 14 683 975 | 12 692 757 | 15 009 357 | 17 325 957 |
| Tennessee | 37 556 | 32.52 | 206 897 080 | 173 281 | 3 928 881 | 7 684 481 | 10 280 321 | 14 035 921 | 17 791 521 | 13 628 860 | 17 384 460 | 21 140 060 |
| Texas | 194 157 | 34.42 | 1 203 431,561 | 12 708 575 | 32 124 275 | 51 539 975 | 61 019 692 | 80 435 392 | 99 851 092 | 79 554 396 | 98 970 096 | 118 385 796 |
| Utah | 15 622 | 23.97 | 56 171 062 | −4 117 148 | −2 554 948 | −992 748 | 145 110 | 1 707 310 | 3 269 510 | 895 984 | 2 458 184 | 4 020 384 |
| Vermont | 2432 | 27.47 | 9 771 389 | −388 163 | −144 963 | 98 237 | 344 878 | 588 078 | 831 278 | 511 857 | 755 057 | 998 257 |
| Washington | 31 274 | 28.35 | 174 656 160 | −2 840 958 | 286 442 | 3 413 842 | 8 772 645 | 11 900 045 | 15 027 445 | 11 594 006 | 14 721 406 | 17 848 806 |
| West Virginia | 10 714 | 35.12 | 41 670 222 | −1 126 293 | −54 893 | 1 016 507 | 171 516 | 1 242 916 | 2 314 316 | 3 911 874 | 1 769 074 | 2 840 474 |
| Wisconsin | 25 058 | 23.11 | 132 079 135 | −6 729 124 | −4 223 324 | −1 717 524 | 5 727 781 | 8 233 581 | 10 739 381 | 7 786 153 | 10 291 953 | 12 797 753 |
| Wyoming | 2634 | 27.79 | 13 823 634 | −165 651 | 97 749 | 361 149 | 1 081 246 | 1 344 646 | 1 608 046 | 1 372 078 | 1 635 478 | 1 898 878 |
| State savings | ||||||||||||
| Maximum | 50 386 316 | 75 030 216 | 99 674 116 | 164 350 905 | 188 994 805 | 213 638 705 | 201 381 310 | 226 025 210 | 250 669 110 | |||
| 75th Percentile | 37 441 | 3 228 003 | 6 776 796 | 11 291 309 | 15 614 723 | 18 885 660 | 13 160 808 | 19 238 077 | 22 295 777 | |||
| Median | −892 110 | 187 552 | 1 950 643 | 4 986 067 | 6 963 967 | 8 941 867 | 6 477 792 | 8 660 958 | 10 638 858 | |||
| 25th Percentile | −2 802 158 | −338 193 | 487 217 | 1 336 626 | 2 361 022 | 3 667 449 | 2 021 424 | 2 600 830 | 3 825 425 | |||
| Minimum | −6 729 124 | −4 223 324 | −1 717 524 | −2 760 597 | 4803 | 831 278 | −11 420 838 | 755 057 | 998 257 | |||
Average rate for doula-supported births.
Derived from adjusted odds ratio of 0.592 for risk of cesarean delivery in doula-supported births, calculated from multivariate analysis of odds of cesarean delivery for doula-supported, Medicaid-funded births (n = 1079) compared with a national sample of Medicaid-funded births (n = 279 008).
Derived from upper-bound 95% confidence interval for adjusted odds ratio of 0.592 for risk of cesarean delivery in doula-supported births, calculated from multivariate analysis of odds of cesarean delivery for doula-supported, Medicaid-funded births (n = 1079) compared with a national sample of Medicaid-funded births (n = 279 008).
FIGURE 1—
State-level estimated annual savings for all states from lower cesarean rates associated with birth doula coverage in Medicaid-funded deliveries, across a range of reimbursement rates, for (a) scenario 1 (rate reduced to 22.3%), (b) scenario 2 (rate reduced by 40.8%), and (c) scenario 3 (rate reduced by 31.6%).
Under the assumption that a state could reduce its cesarean rate for Medicaid births to 22.3% by offering birth doula services to beneficiaries (the rate experienced by Medicaid recipients served by Everyday Miracles doulas), approximately half of states would experience cost savings at a $200 birth doula reimbursement rate. Annual savings might exceed $2.5 million for up to a quarter of all states (Figure 1a). At a $100 reimbursement rate, three quarters of states would likely see cost savings. Figure 1b shows estimated annual cost impacts for a 40.9% reduction in the cesarean rate among Medicaid-funded births, indicating likely savings for nearly all states, even at a birth doula reimbursement rate of $300. In this scenario nearly all states would save at least $2 million per year for a $200 rate, and for a $100 reimbursement, savings might exceed $9 million annually for at least half of states. The final scenario (Figure 1c) is a more conservative estimate of the potential reduction in cesarean rates (showing a 31.6% reduction) and also indicates broad and substantial potential cost savings across a range of reimbursement rates, in nearly all state settings.
DISCUSSION
Consistent with the results of randomized controlled trials of the clinical benefits of continuous labor support from trained doulas,28,29 our analysis indicated that low-income, ethnically diverse women could experience reduced rates of cesarean delivery. The odds of cesarean delivery were 40.9% lower for Medicaid-funded births with doula support than for Medicaid-funded births generally. Among vulnerable subgroups, such as Black women, lower cesarean and preterm rates for doula-supported births are indicative of the role doulas could play in reducing persistent racial/ethnic disparities in these outcomes if high-quality doula services were made financially and culturally accessible to women at highest risk of poor outcomes.7,10
Increasing financial access by offering coverage of birth doula care would be costly to state Medicaid programs, but these costs might be offset by reductions in payments to hospitals and clinicians (fees for cesarean deliveries being substantially higher than for vaginal deliveries), should cesarean rates decrease sufficiently without adverse health consequences. Our findings indicate that cost savings would depend on many state-level factors, such as the number of Medicaid-funded births, the cesarean delivery rate, and reimbursement rates for childbirth services.
The policy scenarios presented here used a payer perspective and calculated costs (of reimbursing doulas for intrapartum support) and savings (associated with lower cesarean rates) in the context of a childbirth hospitalization. It is possible that achieving the outcomes suggested by our analysis would require reimbursement of comprehensive doula services, beyond intrapartum support, in which case the policy scenarios might have overestimated potential savings. On the other hand, doula support might affect childbirth costs via changes in obstetric care beyond delivery mode. Although we examined the cost impacts of changes in cesarean delivery rates associated with doula care, previous research indicates that continuous labor support is also associated with reductions in instrument-assisted delivery, epidural anesthesia, and other obstetric care interventions, without adverse quality impacts.28 Indeed, infants born to mothers who received continuous labor support have significantly higher 5-minute Apgar scores.28,40 In addition, the cost impacts presented in Figure 1 solely relate to childbirth hospitalization and not to long-term health and social benefits or intergenerational transfers of health that may accrue from improving the quality of maternity care.13 From this perspective, our potential cost savings may be a conservative estimate.
Financial and Cultural Access
Although some doulas offer sliding-scale fees according to income, charges for comprehensive doula services range from $300 to more than $1800, depending on geographic location and the doula’s level of experience.40,41 Most Medicaid maternity care benefit packages do not include birth doula care. Oregon’s Medicaid program recently received a federal waiver, making it the first state to include birth doulas in its Medicaid program.42 Some doulas, including those who provided care to our study population, are reimbursed by Medicaid programs for childbirth-related education (e.g., car seat demonstrations and breastfeeding support), but are not reimbursed for support during labor and delivery, a core function of their training and profession. The vast majority of certified doulas recognize a need for health insurance coverage of doula services,24 and DONA and the International Childbirth Education Association have established training and certification programs and payment code information.43,44
Our analysis was intended to inform policy discussions at state public health agencies and Medicaid programs regarding benefits and potential cost savings associated with inclusion of doula care as a Medicaid benefit. Although conditions vary across states, we demonstrated that a state Medicaid program that offers coverage for birth doula care might improve outcomes and reduce costs. To consider this potential coverage policy change, policymakers must assess available evidence in the context of whether and how the proposed intervention could be effectively implemented in their particular setting. They need to evaluate the logistics of implementation, absorptive capacity, training and human capital, measurement, evaluation, enforcement, and sociocultural obstacles.
Studies suggest that doulas can serve diverse populations,32,40,45,46 but the majority of women who receive doula care are women with resources, support, and in-depth education about birth options.24 The women who stand to benefit the most from doula care have the least access to it—both financially and culturally. Most doulas are White middle-class women serving White middle-class women.24 Racial/ethnic concordance between patient and provider is an important facilitator of access to health care services and may also be relevant in the context of doula care.47–50 Recruiting a diverse population of trained doulas, however, may be difficult in the current environment. It is likely that doula work will not become more lucrative or appealing unless more people are willing to pay for these services or third-party reimbursement becomes more common.24 Doulas themselves report that their work is emotionally satisfying but not financially rewarding.24 Broadening the payer base will likely enhance the feasibility of a doula care business model for a wider range of women and facilitate recruitment of doulas from low-income communities, communities of color, and immigrant communities.
Limitations
Our doula data came from 1 practice in 1 state; however, our results were consistent with Cochrane review findings.28 Our 2 data sources were not from the same period; doula data were collected in 2010 to 2012, and the most recent data available through HCUP at the time of the analysis were from 2009. Because little change was observed in preterm birth and cesarean rates in 2009 to 2011,1,9 this difference likely had minimal effects on interpretation of our findings. Information on maternal complications came from hospital discharge reports in HCUP data and patient self-reports in doula data. Any underreporting of maternal complications among doula-supported births would have a downward bias on results, lending credence to our findings.
We did not have information on educational attainment, marital status, prenatal care, and other risk markers or whether Medicaid beneficiaries in HCUP data received doula care. Selection bias could have arisen from Medicaid beneficiaries’ choice to use doula services in lieu of traditional childbirth education. Differences in reporting conventions precluded comparisons for certain racial/ethnic subgroups. Finally, we estimated cost data from charges, converted with a regional cost-to-charge ratio, because we were unable to identify a source of accurate state-level cost data for childbirth-related hospitalizations. Improved data collection and reporting as doula payment codes are adopted are vital to improving these estimates.
Conclusions
Policy action to increase access to doula care has been slow to develop, in spite of well-established clinical benefits. We modeled potential cost impacts to state Medicaid programs of offering coverage for birth doula services under various scenarios; our results suggest that cost savings are feasible for the majority of states across a range of reimbursement rates. Although our estimates can serve as a guide for states to better understand the cost of cesarean delivery and the role of birth doulas in mitigating cost and improving outcomes, states should consider internal analyses to investigate whether reimbursing birth doulas may result in improved birth outcomes and possibly cost savings for their Medicaid programs.
Payers, including state Medicaid programs that facilitate access to doula services via coverage policies, could capture cost savings associated with reduced cesarean delivery rates. Doula care may also hold promise for addressing persistent racial/ethnic disparities in birth outcomes.
Acknowledgments
This work was supported by a Building Interdisciplinary Research Careers in Women’s Health Grant (K12HD055887) from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, the Office of Research on Women’s Health, and the National Institute on Aging, administered by the University of Minnesota Deborah E. Powell Center for Women’s Health.
The authors gratefully acknowledge helpful input, guidance, and collaboration from Debby L. Prudhomme, CD (DONA) and Mary R. Williams, LPN, CD (DONA), cofounders of Everyday Miracles Inc. We sincerely appreciate data entry support from Lauren Hindt. This research would not have been possible without the extraordinary work of the doulas employed by Everyday Miracles. K. B. Kozhimannil extends particular thanks to Teresa Stewart and Maria Rader.
Human Participant Protection
The University of Minnesota institutional review board exempted this study from approval because it used de-indentified administrative data.
References
- 1.Martin JA, Hamilton BE, Sutton Pet al. Births: Final Data for 2009. Natl Vital Stat Rep. 2011;60(1):1–70 [PubMed] [Google Scholar]
- 2.Sakala C, Corry MP, Fund MM. Evidence-Based Maternity Care: What It Is and What It Can Achieve. New York, NY: Milbank Memorial Fund; 2008 [Google Scholar]
- 3.Corry M, Thompson J, Dilweg AC, Mazza F. Caesar’s Ghost: The Effect of the Rising Rate of C-Sections on Health Care Costs and Quality. Washington, DC: National Health Policy Forum; 2012 [Google Scholar]
- 4.Markus AR, Rosenbaum S. The role of Medicaid in promoting access to high-quality, high-value maternity care. Womens Health Issues. 2010;20(1 suppl):S67–S78 [DOI] [PubMed] [Google Scholar]
- 5.The Healthcare Costs of Having a Baby. Santa Barbara, CA: Thomson Healthcare; 2007. Available at: http://www.kff.org/womenshealth/upload/whp061207othc.pdf. Accessed January 15, 2013 [Google Scholar]
- 6.Podulka J, Stranges E, Steiner C. Hospitalizations Related to Childbirth, 2008. Rockville, MD: Agency for Healthcare Research and Quality; 2011. Statistical brief 110 [PubMed] [Google Scholar]
- 7.Berns SD, Kott A, eds. Toward Improving the Outcome of Pregnancy III: Enhancing Perinatal Health Through Quality, Safety and Performance Initiatives. White Plains, NY: March of Dimes National Foundation; 2010 [Google Scholar]
- 8.Elixhauser A, Wier LM. Complicating Conditions of Pregnancy and Childbirth, 2008. Rockville, MD: Agency for Healthcare Research and Quality; 2008. HCUP statistical brief 113. Available at: http://www.hcup-us.ahrq.gov/reports/statbriefs/sb113.pdf. Accessed January 15, 2013 [PubMed] [Google Scholar]
- 9.Martin JA, Hamilton BE, Sutton PD, Ventura SJ, Mathews T, Osterman MJ. Births: final data for 2008. Natl Vital Stat Rep. 2010;59(1):1–72 [PubMed] [Google Scholar]
- 10.Bryant AS, Worjoloh A, Caughey AB, Washington AE. Racial/ethnic disparities in obstetric outcomes and care: prevalence and determinants. Am J Obstet Gynecol. 2010;202(4):335–343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Krieger JW, Connell FA, LoGerfo JP. Medicaid prenatal care: a comparison of use and outcomes in fee-for-service and managed care. Am J Public Health. 1992;82(2):185–190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schwethelm B, Margolis LH, Miller C, Smith S. Risk status and pregnancy outcome among medicaid recipients. Am J Prev Med. 1989;5(3):157–163 [PubMed] [Google Scholar]
- 13.Lu MC, Halfon N. Racial and ethnic disparities in birth outcomes: a life-course perspective. Matern Child Health J. 2003;7(1):13–30 [DOI] [PubMed] [Google Scholar]
- 14.Collins JW, Jr, Herman AA, David RJ. Very-low-birthweight infants and income incongruity among African American and White parents in Chicago. Am J Public Health. 1997;87(3):414–417 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lu MC, Kotelchuck M, Hogan VK, Johnson K, Reyes C. Innovative strategies to reduce disparities in the quality of prenatal care in underresourced settings. Med Care Res Rev. 2010;67(5 suppl):198S–230S [DOI] [PubMed] [Google Scholar]
- 16.Preterm Birth: Causes, Consequences, and Prevention. Institute of MedicineWashington, DC: National Academies Press; 2006. IOM report brief [PubMed] [Google Scholar]
- 17.Transforming Maternity Care Symposium Steering Committee, Angood PB, Armstrong EMet al. Blueprint for action: steps toward a high-quality, high-value maternity care system. Womens Health Issues. 2010;20(1 suppl):S18–S49 [DOI] [PubMed] [Google Scholar]
- 18.Chassin MR, Loeb JM, Schmaltz SP, Wachter RM. Accountability measures—using measurement to promote quality improvement. N Engl J Med. 2010;363(7):683–688 [DOI] [PubMed] [Google Scholar]
- 19.Jackson DJ, Lang JM, Swartz WHet al. Outcomes, safety, and resource utilization in a collaborative care birth center program compared with traditional physician-based perinatal care. Am J Public Health. 2003;93(6):999–1006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Olds DL, Kitzman HJ, Cole REet al. Enduring effects of prenatal and infancy home visiting by nurses on maternal life course and government spending: follow-up of a randomized trial among children at age 12 years. Arch Pediatr Adolesc Med. 2010;164(5):419–424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kitzman H, Olds DL, Henderson CR, Jret al. Effect of prenatal and infancy home visitation by nurses on pregnancy outcomes, childhood injuries, and repeated childbearing. JAMA. 1997;278(8):644–652 [PubMed] [Google Scholar]
- 22.Johnson KA. Women’s health and health reform: implications of the Patient Protection and Affordable Care Act. Curr Opin Obstet Gynecol. 2010;22(6):492–497 [DOI] [PubMed] [Google Scholar]
- 23.Sakala C. Health care reform legislation offers major new gains to childbearing women and newborns. Birth. 2010;37(4):337–340 [DOI] [PubMed] [Google Scholar]
- 24.Lantz PM, Low LK, Varkey S, Watson RL. Doulas as childbirth paraprofessionals: results from a national survey. Womens Health Issues. 2005;15(3):109–116 [DOI] [PubMed] [Google Scholar]
- 25.Klaus MH, Kennell JH. The doula: an essential ingredient of childbirth rediscovered. Acta Paediatr. 1997;86(10):1034–1036 [DOI] [PubMed] [Google Scholar]
- 26.Klaus MH, Kennell JH, Klaus PH. Mothering the Mother: How a Doula Can Help You Have a Shorter, Easier, and Healthier Birth. Cambridge, MA: Da Capo Press, Addison-Wesley Reading; 1993 [Google Scholar]
- 27.Birth doula FAQs The Doula Organization of North America (DONA). Available at: http://www.dona.org/mothers/faqs_birth.php. Accessed January 15, 2013
- 28.Hodnett ED, Gates S, Hofmeyr GJ, Sakala C, Weston J. Continuous support for women during childbirth. Cochrane Database Syst Rev. 2011;16(2):CD003766 [DOI] [PubMed] [Google Scholar]
- 29.Zhang J, Bernasko JW, Leybovich E, Fahs M, Hatch MC. Continuous labor support from labor attendant for primiparous women: a meta-analysis. Obstet Gynecol. 1996;88(4 pt 2):739–744 [DOI] [PubMed] [Google Scholar]
- 30.McGrath SK, Kennell JH. A randomized controlled trial of continuous labor support for middle-class couples: effect on cesarean delivery rates. Birth. 2008;35(2):92–97 [DOI] [PubMed] [Google Scholar]
- 31.Mottl-Santiago J, Walker C, Ewan J, Vragovic O, Winder S, Stubblefield P. A hospital-based doula program and childbirth outcomes in an urban, multicultural setting. Matern Child Health J. 2008;12(3):372–377 [DOI] [PubMed] [Google Scholar]
- 32.Dundek LH. Establishment of a Somali doula program at a large metropolitan hospital. J Perinat Neonatal Nurs. 2006;20(2):128–137 [DOI] [PubMed] [Google Scholar]
- 33. Overview of the Nationwide Inpatient Sample (NIS). Health Care Cost and Utilization Project (HCUP), Agency for Healthcare Research and Quality. 2013. Available at: http://www.hcup-us.ahrq.gov/nisoverview.jsp. Accessed January 14, 2013.
- 34.Miller DC, Gust C, Dimick JB, Birkmeyer N, Skinner J, Birkmeyer JD. Large variations In Medicare payments for surgery highlight savings potential from bundled payment programs. Health Aff (Millwood). 2011;30(11):2107–2115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.International Classification of Diseases, Ninth Revision. Geneva, Switzerland: World Health Organization; 1980 [Google Scholar]
- 36.Averill RF, Goldfield N, Hughs JS All patient refined diagnosis related groups (APR-DRGs): methodology overview. Version 20.0. 2013. Available at: http://www.hcup-us.ahrq.gov/db/nation/nis/APR-DRGsV20MethodologyOverviewandBibliography.pdf. Accessed January 14, 2013.
- 37.Kuklina EV, Whiteman MK, Hillis SDet al. An enhanced method for identifying obstetric deliveries: implications for estimating maternal morbidity. Matern Child Health J. 2008;12(4):469–477 [DOI] [PubMed] [Google Scholar]
- 38.Kuklina E, Callaghan W. Chronic heart disease and severe obstetric morbidity among hospitalisations for pregnancy in the USA: 1995–2006. BJOG. 2011;118(3):345–352 [DOI] [PubMed] [Google Scholar]
- 39.Clinical classification software (CCS) for ICD-9-CM. Washington, DC: Agency for Healthcare Research and Quality; 2013. Available at: http://www.hcup-us.ahrq.gov/toolssoftware/ccs/ccs.jsp. Accessed January 14, 2013 [Google Scholar]
- 40.Campbell DA, Lake MF, Falk M, Backstrand JR. A randomized control trial of continuous support in labor by a lay doula. J Obstet Gynecol Neonatal Nurs. 2006;35(4):456–464 [DOI] [PubMed] [Google Scholar]
- 41. The cost of a doula. Doula.com Web site. Western Belt Buckles; 2006. Available at: http://www.doula.com. Accessed January 15, 2013.
- 42.Tillman T, Gilmer R, Foster A. Utilizing doulas to improve birth outcomes among underserved women in Oregon. Salem: Oregon Health Authority; 2012. Available at: http://www.oregon.gov/oha/legactivity/2012/hb3311report-doulas.pdf. Accessed January 15, 2013 [Google Scholar]
- 43.Wennberg JE. Practice variations and health care reform: connecting the dots. Health Aff (Millwood). 2004;suppl variation:VAR140–VAR141 [DOI] [PubMed] [Google Scholar]
- 44.Newhouse JP, Garber A. Geographic Variation in Health Care Spending and Promotion of High-Value Care. Washington, DC: National Academies Press; 2010 [PubMed] [Google Scholar]
- 45.Breedlove G. Perceptions of social support from pregnant and parenting teens using community-based doulas. J Perinat Educ. 2005;14(3):15–22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Small R, Gagnon A, Gissler Met al. Somali women and their pregnancy outcomes postmigration: data from six receiving countries. BJOG. 2008;115(13):1630–1640 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Strumpf EC. Racial/ethnic disparities in primary care: the role of physician-patient concordance. Med Care. 2011;49(5):496–503 [DOI] [PubMed] [Google Scholar]
- 48.Cooper LA, Roter DL, Johnson RL, Ford DE, Steinwachs DM, Powe NR. Patient-centered communication, ratings of care, and concordance of patient and physician race. Ann Intern Med. 2003;139(11):907–915 [DOI] [PubMed] [Google Scholar]
- 49.Saha S, Komaromy M, Koepsell TD, Bindman AB. Patient-physician racial concordance and the perceived quality and use of health care. Arch Intern Med. 1999;159(9):997–1004 [DOI] [PubMed] [Google Scholar]
- 50.LaVeist TA, Carroll T. Race of physician and satisfaction with care among African-American patients. J Natl Med Assoc. 2002;94(11):937–943 [PMC free article] [PubMed] [Google Scholar]