Abstract
Background
The observational evidence of the impacts of climate conditions on human health is accumulating. A variety of direct, indirect, and systemically mediated health effects have been identified. Excessive daily heat exposures create direct effects, such as heat stroke (and possibly death), reduce work productivity, and interfere with daily household activities. Extreme weather events, including storms, floods, and droughts, create direct injury risks and follow-on outbreaks of infectious diseases, lack of nutrition, and mental stress. Climate change will increase these direct health effects. Indirect effects include malnutrition and under-nutrition due to failing local agriculture, spread of vector-borne diseases and other infectious diseases, and mental health and other problems caused by forced migration from affected homes and workplaces. Examples of systemically mediated impacts on population health include famine, conflicts, and the consequences of large-scale adverse economic effects due to reduced human and environmental productivity. This article highlights links between climate change and non-communicable health problems, a major concern for global health beyond 2015.
Discussion
Detailed regional analysis of climate conditions clearly shows increasing temperatures in many parts of the world. Climate modelling indicates that by the year 2100 the global average temperature may have increased by 3-4°C unless fundamental reductions in current global trends for greenhouse gas emissions are achieved. Given other unforeseeable environmental, social, demographic, and geopolitical changes that may occur in a plus-4-degree world, that scenario may comprise a largely uninhabitable world for millions of people and great social and military tensions.
Conclusion
It is imperative that we identify actions and strategies that are effective in reducing these increasingly likely threats to health and well-being. The fundamental preventive strategy is, of course, climate change mitigation by significantly reducing global greenhouse gas emissions, especially long-acting carbon dioxide (CO2), and by increasing the uptake of CO2 at the earth's surface. This involves urgent shifts in energy production from fossil fuels to renewable energy sources, energy conservation in building design and urban planning, and reduced waste of energy for transport, building heating/cooling, and agriculture. It would also involve shifts in agricultural production and food systems to reduce energy and water use particularly in meat production. There is also potential for prevention via mitigation, adaptation, or resilience building actions, but for the large populations in tropical countries, mitigation of climate change is required to achieve health protection solutions that will last.
Keywords: climate change, health, well-being, adaptation, mitigation
The best-understood of the impacts of climate change on human health can already be estimated statistically, in some cases even documented, where significant change has occurred (1). Future impacts of projected climates on many such health outcomes can be modelled, using information from empirical studies of the relationship of variations in climate conditions to specific health outcomes (2). A variety of direct, indirect, and systemically mediated health effects have been identified (3–5). The improved quantitative evidence of climate-health linkages is the basis for improved modelling methods and projections of the health and well-being impacts that on-going climate change will bring. An important aspect of these impacts is the economic costs involved. A recent analysis in the Climate Vulnerability Monitor 2012 (6), which looked in detail at the costs of different climate change impacts on the environment, and on human health and well-being, reported annual costs at the level of trillions of US$ by 2030. As the models and underlying data improve, such estimates will become more accurate.
Much of the research and analysis on the health impacts of climate change focuses on the actual impacts of change that is currently under way. If temperatures rise in mountainous areas and malaria cases start occurring at higher altitudes, this may be a sign of climate change impacts on health, but other factors need to be taken into account (7). When records show that extreme weather events have increased in frequency and intensity (8), the estimated additional health impact could also be considered a measure of climate change impact.
Based on studies of the actual health risks associated with differing climate conditions, epidemiological and health impact assessment methods can then be used to estimate the impacts of on-going and future climate change on these health risks. These can be direct, indirect, and systemically mediated (5) or with other terms, primary, secondary, and tertiary (9). The most obvious example is the impact of extreme heat on human physiology and clinical health (10). This area has been studied for more than a century, and quantitative relationships between heat and health risks exist, but will need confirmation in different settings (10).
The evidence base
On-going and future climate change
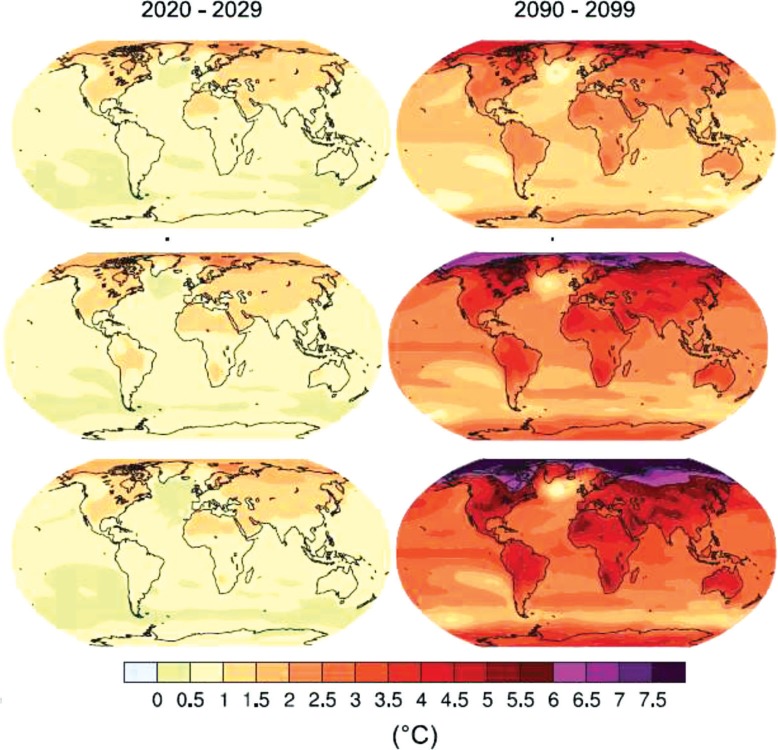
Detailed regional analysis of on-going trends of climate conditions and their modelled future trends shows clearly the observed and anticipated increases in temperatures in most parts of the world as shown in Fig. 1 (11). In some places, the coldest months are actually getting cooler creating more extreme seasonal differences and difficulties when interpreting human climate exposure issues from annual averages. Extreme recent winters in parts of the Northern hemisphere may be a sign of the changing climate. While temperature is a central concern, climate change entails shifts in temporal and spatial patterns of precipitation – less easy to model than temperature – and in winds, ocean currents, and overall short-term variability. All of these, acting separately or together, have great implications for human health and survival, affecting different regions in different ways.
Fig. 1.
Current and projected temperature changes globally (11). The top maps show the estimated climate change for a 2°C global average change; the middle figure for a 3°C change and the bottom figure for a 4°C change. The new unpublished maps for RCP8.5 are very similar to the bottom maps. Baseline=1961–1990.
The latest climate modelling outputs, using Representative Concentration Pathways (RCP) (12) greenhouse gas trajectories as inputs, indicate that by the year 2100 the global average temperature may have gained 3–4°C (highest likely estimate 6°C) unless fundamental reductions in the global trends for greenhouse gas emissions are achieved (IPCC report, 2013, forthcoming). The new maps and trends using RCP-based models do not differ substantially from the estimates derived from using previous models (13). Our article does not focus on such modelling, but it can be said with confidence that a thriving global civilization in a plus-6-degree world is inconceivable.
These estimated changes in climate of 3–4°C and above will shift rainfall patterns so that certain areas become drier and other areas become wetter (11). The frequency of extreme weather events (storms, hurricanes, rain-related floods, droughts, etc) is expected to increase as the climate system acquires more energy from higher average air temperatures and the latent heat of increased water vapour (14). Exposure to heat extremes will also change markedly.
Extremes of temperature have relatively direct and understandable impacts on human biology and health, and temperature increases in tropical areas (within 23 degrees of the Equator) and sub-tropical areas (up to 40 degrees from the Equator) are of particular concern. Strong and extreme heat stress outdoors at noon occurred for 3–8 months of each year in the 1970s (15), and such periods, currently increasing, will extend by at least one more month by the 2050s (15). A rapid rate of change contributes to the health risks.
Individuals living and working in rapidly growing urban areas around the world will be at particular risk due to the well-established urban heat-island effect (16). Warmer temperatures in colder temperate and arctic areas may reduce risks due to cold exposure (10). However, from a global viewpoint, the very much greater population numbers in hot areas, and the rapid urbanization in those areas, makes them vulnerable to heat-related climate change health impacts.
Impact of climate conditions on human health and well-being
Climate change acts at many levels and with differing relative influence in its impacts on health outcomes. In general, it plays a multiplier role, typically amplifying or extending a population's pre-existing health risks or problems.
The observational evidence of the human health impacts of variations in climate conditions is now very substantial, particularly in relation to heat and cold exposure (10, 17). The health impacts of heat have been a concern since the 19th century – particularly among European colonial staff, military personnel, and other working people (18) – and mechanistic physiological research has elucidated the ill effects of excess heat (17). Thermal physiology, environmental ergonomics, biometeorology, and other scientific disciplines continue to accumulate evidence of heat and cold impacts on human health and work productivity. Excessive daily heat exposures causes heat stroke, which may lead to deaths (19), heat exhaustion that reduces work productivity (20, 21), and heat stress that interferes with daily household activities (10, 22).
Other extreme weather events including storms, floods, and droughts create direct injury risks and follow-on outbreaks of infectious diseases, lack of nutrition, and mental stress (8, 23). Any heat, cold, or weather-related reduction of capacity to carry out daily activities should be considered a ‘health effect’, given WHO's standing definition of health (‘Health is a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity’). Further, if actions taken to prevent adverse effects of extreme weather conditions inadvertently impair health or well-being, that too should be considered a climate-related ‘health impact’.
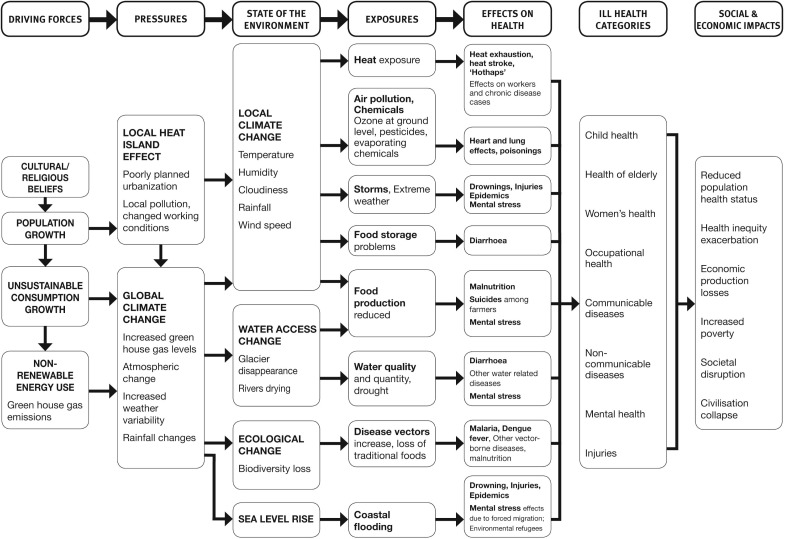
The indirect effects of changes in climatic conditions are many and diverse. Changes in access to clean drinking water, particularly in conditions of crowding and poverty, can cause diarrhoeal diseases and other water-related diseases, including cholera (2). Other major examples include malnutrition and under-nutrition and impaired childhood development due to declines in local agriculture (24), altered ranges and rates of various vector-borne diseases and other infectious diseases (25–27), and mental health disorders and conflict-prone tensions caused by forced migration from affected homes and workplaces (28). Of course, a variety of other factors influence these health problems and may have much greater impact than climate change. Examples of systemic impacts include food crises (sometimes causing famine), conflicts/wars over access to water, and large-scale adverse economic effects due to reduced human and environmental productivity (5, 9). Figure 2 summarises the relationships between driving forces for local climate change, pressures on the environment, changes in the environment, human exposures to hazards, and the health impacts using the DPSEEA framework developed at WHO (29).
Fig. 2.
DPSEEA framework for climate change and Global Public Health.
As highlighted in Fig. 2, the local climate conditions where people live and work create most of the direct human health hazards, such as those due to the urban heat-island effect (especially in a rapidly urbanizing world) (16), while the more indirect health effects are often associated with global or large-scale regional climate change. Changes in water access may relate to climate-environmental conditions far from the affected people, and sea-level rise is a global phenomenon. Changes in climate may create positive impacts in cold temperate areas (10). However, one detailed analysis (30) concluded that no overall reduction of winter mortality is likely in USA and Europe (differences occur within these regions). Improved agricultural productivity is another potential beneficial impact in these temperate areas (4), although this may contribute to increased inequity between high- and low-income countries.
Climate conditions have an important role to play in all of the health issues described in Fig. 2. However, the impacts of changes in climate on population health and well-being in many parts of the world, particularly tropical countries, have not yet been well established. A partial attempt to quantify the impacts attributable to the extent of climate change that had occurred by 2000 entailed an analysis of mortality for five key areas of health impacts (1). Somewhere in the order of 150,000 deaths could be assigned as climate change impacts on malnutrition, diarrhoea, malaria, floods, and cardiovascular diseases (heat stroke deaths) as early as 2000. However, a number of potential climate change impacts on health were not included. That deficit is now being addressed.
A second-generation project initiated by WHO in 2009 (coordinated by S. Kovats and S. Hales) is still developing an updated analysis of these impacts and their projected future levels, including a more comprehensive list of health effects (see Box 1). The project aims to incorporate future social and economic trends into the analysis, which creates additional complexity in the analysis. Some publications on specific impacts are available (e.g. 27, 31), but the overall impact analysis requires further work. A valid comparison of the global, regional, and national disease-specific impact estimates can therefore not yet be made.
Box 1. The WHO project on ‘burden of disease’ due to climate change.
This list includes health risks and specific disease topics included. Each topic is using the same future estimates of climate and population change. Modelling of health impacts is specific for each topic.
Malaria
Dengue
Schistosomiasis
Coastal flooding
Burden of disease from changes in effectiveness of water and sanitation infrastructure
Diarrhoeal disease (temperature driven)
Direct impacts of temperature on work ability
The direct impacts of heat on mortality
Malnutrition
Health effects of economic damages from climate change
The following impacts were also identified as important and may be added to the project:
Impacts on outdoor air pollution
Health co-benefits and harms from mitigation and adaptation policies
Links to non-communicable diseases, social determinants, and health equity
Much attention has been given to the vector-borne and infectious disease risks related to climate change (4). However, there will also be various impacts on non-communicable diseases (NCDs) (32).
Recent publications (33, 34) have shown the increases, during heat-waves, in admission rates and emergency presentation rates for NCDs at health service institutions in Australia and the USA. Along with exacerbations of cardiovascular disease, the greatest relative heat-related increase of hospital admissions in these reports was for kidney diseases. This could signal the physiological link between high heat exposure, sweat function, dehydration, and kidney function (35). A related issue is the apparent increase of kidney stone incidence in relation to a hotter climate (36). Another relationship to NCDs is the higher risk of heat illness among overweight people (37).
The clinical condition of patients with chronic diseases (e.g. hypertension, heart disease, diabetes, etc.) will often deteriorate if the patient is exposed to excessive heat levels (32). This has been studied and known for several decades, and is easily overlooked in current research and reviews. For example, a vivid example of the negative impact of heat on cardiovascular disease patients comes from Texas in the 1950s (38). One particular hospital had some wards with air conditioning and some without. Clinical progress of acute heart disease was much worse in patients in wards without air conditioning. In 2013, it is likely that air conditioning is standard infrastructure in all hospitals in high-income countries with very hot seasons, but in low-income countries, this is probably not true and excessive heat exposure at home or in those health service institutions is likely to have a negative impact on clinical status and progress in treatment (39).
The direct effects of heat are of course ‘non-communicable’ (heat stroke depends on individual environmental exposure). The greatest health and well-being impacts of climate change in large parts of the highly populated hot world are likely to be due to heat stress and heat exhaustion, which are often ignored by the health sector, as the victims seldom approach health services for help. High heat exposure also increases injury risk (40), which is not classified as NCD, but the underlying mechanism is fundamentally related to the heat effects on non-communicable health variables.
This leads into the issue of social determinants of health and well-being, and the differential impacts that climate change may have. The additional risks for poor people in low-and middle-income countries include most items in Fig. 2.
Human capacity and resource constraints
Strengthening resilience to climate change
Many of the health impacts of climate change referred to above are a particular threat to poor people in low- and middle-income countries. An important method to reduce impacts of climate change is to improve general public health status of populations at risk (4). Since climate change acts primarily as an amplifier of existing health risks, the lower the background rate of any health disorder or disease, the less the absolute change due to climate change is likely to be. This strategy improves resilience to climate change impacts, but it cannot fully protect against the undermining of human living and working conditions that excessive heat stress, droughts, floods, storms, sea-level rise, etc. will bring. It should be pointed out that the climate change impacts on communities also interact with several other global concerns, such as population growth rates, availability of education and primary health services, and other infrastructure, as well as corruption that undermines efficient reductions in inequalities (5). Strategies to reduce impacts of climate change need a multi-dimensional approach. The economic costs and benefits of these preventive strategies are also key issues linked to the possibilities to make them effective and durable. Valid detailed estimates are still not easily available.
Another way to strengthen resilience is to reduce the urban heat-island effect by using known urban design methods to lessen the local heat load. This also includes considerations of architectural design that reduce need for air conditioning of indoor spaces. Air conditioning in dense urban areas is also a factor increasing the local heat levels, as the heat from indoors is transferred outdoors. In Taiwan, it was shown that the air conditioning can add 0.7°C to the outdoor heat load (41).
Potential for human adaptation to new climate conditions
Adaptation is the term applied to preventive strategies that reduce the immediate effects of direct or indirect exposures to the changing climate variables. By forecasting health problems that may occur, such as the health and well-being impacts of tropical storm Sandy in the USA recently, government agencies and communities can prepare for the worst and, if needed, evacuate from the most affected geographic areas. Long-term planning with adaptation impacts includes the analysis of future coastal flooding risks and banning of new buildings in risk areas. In areas where vector-borne diseases, such as malaria and dengue fever, will spread due to changing climate conditions, application of known malaria control methods can be an important adaptation (27). Providing air conditioning in old-age homes was a broadly applied adaptation in France to the severe mortality impacts of the extreme heat wave in 2003 (42). However, such strategies contribute to electricity use, and this contributes to greenhouse gas emissions.
Resource implications for adaptation
Effective improvement of climate resilience and adaptation to on-going and future climate change will require expertise at national and local level, a resource issue. Scientific/professional analysis should include the full life-cycle impact of urban development, transport, food production and distribution systems, and housing and workplace design. The up-front and continuing cost of air conditioning and other adaptation methods will create another resource limitation issue. Currently, power cuts (blackouts and brownouts) are common in some developing economies, and adaptation methods requiring electricity may not be reliable.
An issue for the health sector is of course the costs for treatment of people who become ill due to climate change. The health sector also needs to develop knowledge and skills in local prevention/adaptation programmes, in order to reduce the cost of treatments.
Action strategies that work
Limits of adaptation
It is sometimes assumed that human populations can adapt to whatever climatic changes will occur during this century and beyond. Historically, when the climate has changed over the last thousands of years, affected populations have sometimes been able to migrate to other regions and re-establish their communities. Mostly, however, this has not been so since the advent of settled agrarian communities and villages (43). However, with current high population densities, particularly in hot tropical areas, the possibilities for large populations to migrate to new living space has become very difficult, and is not a convenient adaptation solution.
The possibilities for adaptation are also influenced by the duration of time that climate condition persists. Excessive heat, rainfall, or wind exposures may be a short-term feature of each day or it may continue during the whole day. The global analysis by Sherwood and Huber (44) and more detailed analysis for Perth, Australia, (45) indicated that some parts of the planet will get to these heat limits during this century. The growing threat for natural disasters (8) is another challenge for adaptation.
Air conditioning is often thought of as the solution to the indoor heat problems, but it requires electrical power, which in many locations is produced by fossil fuel energy contributing to greenhouse gas emissions. New approaches using renewable energy for air conditioning will be essential as a way to ensure more sustainable cooling methods. Living in an air-conditioned environment also reduces heat acclimatization and increases health risks during power cuts.
Mitigation of climate change: a crucial approach to health protection
The human species primarily settled where the ecosystem was safe and, with appropriate cultural adaptation, healthy for humans. Such a habitat provides resources for food production and drinking water access, and has other features essential for human survival. The exact threshold for a ‘liveable climate’ for human society has not yet been analysed, but the papers by Sherwood and Huber (44) and Mahoney and Forbes (45) allude to this major problem. If climate change in tropical areas threatens to make the climate so hot or dry or wet during long periods of the year that people really cannot live and carry out daily activities in particular locations, then the only way to protect health and well-being is via climate change mitigation.
This would involve urgent shifts in energy production from fossil fuels to renewable energy sources, energy conservation in building design and urban planning, and reduced waste of energy for transport, building cooling, and agriculture. It would also involve shifts in agricultural production and food systems to reduce energy and water use, particularly in meat production. A key issue is the reduction of greenhouse gas emissions, especially long-acting carbon dioxide (CO2), and increased uptake of CO2 at the earth's surface. Mitigation strategies are impeded by the short-term perspective of many political debates and decision-making processes, and by the profitability criteria that drive large-scale corporate investment in dominant sectors of our economies. Meanwhile, the threats remain and are growing.
In order to achieve greater support for the type of strategies needed for mitigation it is essential to promote the importance of creating a better future for our children, grandchildren, and the subsequent generations. The concerns about climate change impacts are ignored by some as ‘issues of the future’ while we can actually see the future as the present via the eyes of our young people. Children born since 2000 will mostly still be alive in 2070, or even in 2080 or 2100, as life expectancy continues to increase. If we consider ‘child health and well-being’ an important concern, a life-time perspective on these lives brings climate change into the picture in a new way. Preventive strategies have to be developed and implemented in the next decade. However, most decision-makers of today will not be alive when climate change impacts become very prominent.
Strategies for mitigation can have combined adaptation impacts, which may make them easier to choose and implement. Building design that reduces energy demand yet maintains a healthy indoor environment and reduces exposures to temperature extremes, is such an approach. Indeed, architectural and urban design methods that minimise energy consumption via thermal insulation, solar heat management, and shade provision are available. This is of particular importance to the elderly and other vulnerable citizens, as well as for workplaces where both health and productivity are affected by heat extremes (20). Climate change may reduce heating needs in global areas with a very cold winter climate, but the proportion of the global population living in such areas is relatively small. Most people live and work in the hot tropical and sub-tropical areas, and there climate change will increase energy demand for cooling.
Health co-benefits of climate change mitigation
Many mitigation strategies have important health co-benefits of a mostly localized kind, which can reduce the political reluctance to take action (46). Improved quality household energy sources and more efficient use of such energy will reduce local and indoor air pollution and protect population health (47). A shift to cook stoves that produce less indoor air pollution is a priority for the protection of health in poor communities (47).
Shifting transport from private motor vehicles towards public transport and ‘active transport’ for short daily trips (walking and cycling) will create increased daily physical activity in otherwise sedentary groups, and this has a number of population health benefits (48). Energy efficient public transport is an important approach to reduce urban air pollution and its impacts on heart and lung diseases (48). The development of renewable energy sources can also promote health by reducing the very high occupational injury and disease risk among coal miners and other fossil energy workers, while new jobs in other energy production create health benefits (49, 50). Another example is the reduction of weekly consumption of meat and saturated fats from animals, particularly red fatty meat, which will reduce health risks associated with such a diet (24, 51). This includes certain cancers, obesity, and heart diseases. To the extent that climate change mitigation reduces on-going biodiversity loss, a health co-benefit will also be the protection of natural species that will be of importance for our understanding of disease prevention and treatment.
Economic costs of impacts on human health and well-being and benefits from prevention
The economic costs and benefits of these preventive strategies are also a key issue concerning the possibility make them effective and durable. Valid detailed estimates are still not easily available, but the estimates in the recent Climate Vulnerability Monitor 2012 (6) give an approximate indication of the implications (Table 1).
Table 1.
Economic impacts of climate change
| Total global net cost, (% of total climate cost) | Net cost in 2030 by specific country type | ||||
|---|---|---|---|---|---|
|
|
|
||||
| Impact component | 2010 | 2030 | Developing, low GHG emitters | Developing, high GHG emitters | Developed |
| Total climate change | 609 (100) | 4,345 (100) | 1,730 (100) | 2,292 (100) | 179 (100) |
| Labour productivity loss due to workplace heat | 311 (51) | 2,436 (56) | 1,035 (60) | 1,364 (60) | 48 (27) |
| Clinical health impacts | 23 (3.7) | 106 (2.4) | 84 (4.9) | 21 (0.9) | 0.002 (0.001) |
Source: DARA 2012 (6).
Currency=millions of USD PPP; GHG=greenhouse gases.
The estimated clinical health impacts produce substantial economic costs: US$23 billion in 2010 and US$106 billion in 2030. The worst impacts in relation to the local economy are in developing countries with low greenhouse gas emissions. The high-emitting countries have much lower percentages of the costs in the form of health effects, and developed countries even less so.
Interestingly, the table indicates that more than 50% of the economic costs at global level and in developing countries would arise from labour productivity loss due to workplace heat. These are the first calculations of this type to have been published. They entail a range of assumptions and need assessment and confirmation by further research and analysis.
Another recent analysis (52) highlights the links between population-based incomes and climatic conditions. When it gets hotter in hot countries, the economic output goes down.
Conclusions
There is a great variety of potential health impacts of climate change in different settings around the world. At any one time, the prevailing climate conditions and the background population health status are of great importance in influencing the risk to health. It is most likely that countries in the hot tropical and sub-tropical countries will be greatly affected, and a low general level of population health increases local vulnerability to the health effects of climate conditions and climate change.
The expected climate change will create both communicable and non-communicable health challenges depending on the underlying health determinants panorama. Resources for analysing the challenges and finding solutions will be limited in low- and middle-income countries for many years to come.
There are prevention strategies based on adaptation that will work but the cost may be significant. A number of actions for climate change mitigation have important health co-benefits, meaning that reduced greenhouse gas emissions are achieved with actions that promote and facilitate improved population health. For the most fundamental health threats, only climate change mitigation will achieve the necessary protection of good population health for current and future generations.
Conflict of interest and funding
The authors have not received any funding or benefits from industry to conduct this analysis and has no conflicts of interest. Funding was provided from research funds at Umeå University and Australian National University.
References
- 1.McMichael AJ, Campbell-Lendrum D, Kovats S, Edwards S, Wilkinson P, Wilson T, et al. Global climate change. In: Ezzati M, Lopez A, Rodgers A, Murray CJL, editors. Comparative quantification of health risks, global and regional burden of disease attributable to selected major risk factors. vol. 2. Geneva: World Health Organization; 2004. pp. 1543–650. [Google Scholar]
- 2.McMichael A, Campbell-Lendrum D, Ebi K, Githeko A, Scheraga J, Woodward A. Climate change and human health: risks and responses. Geneva: World Health Organization; 2003. [Google Scholar]
- 3.McMichael AJ, Haines A, Sloof R, Kovats S. Climate change and human health. Geneva: World Health Organization; 1996. [Google Scholar]
- 4.Costello A, Abbas M, Allen A, Ball S, Bell S, Bellamy R, et al. Managing the health effects of climate change: Lancet-University College London Institute for Global Health Commission. Lancet. 2009;373:1693–733. doi: 10.1016/S0140-6736(09)60935-1. [DOI] [PubMed] [Google Scholar]
- 5.Butler CD, Corvalan CF, Koren HS. Human health, well-being and global ecological scenarios. Ecosystems. 2005;8:153–62. doi: 10.1007/s10021-004-0076-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.DARA (2012) A guide to the cold calculus of a hot planet. Barcelona: Fundacion DARA International; 2012. Climate vulnerability monitor 2012; p. 320. http://daraint.org/climate-vulnerability-monitor/climate-vulnerability-monitor-2012/ [Google Scholar]
- 7.Pascual M, Ahumada JA, Chaves LF, Rodo X, Bouma M. Malaria resurgence in East African highlands: temperature trends revisited. PNAS. 2006;103:5829–34. doi: 10.1073/pnas.0508929103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sauerborn R, Ebi K. Climate change and natural disasters – integrating science and practice to protect health. Glob Health Action. 2012;5:19295. doi: 10.3402/gha.v5i0.19295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Butler CD, Harley D. Primary, secondary and tertiary effects of eco-climate change: the medical response. Postgrad Med J. 2010;86:230–4. doi: 10.1136/pgmj.2009.082727. [DOI] [PubMed] [Google Scholar]
- 10.Parsons K. The effects of hot, moderate and cold temperatures on human health, comfort and performance. 2nd ed. London: Taylor & Francis; 2003. Human thermal environments. [Google Scholar]
- 11.IPCC. Climate change 2007: the physical science basis. Summary for policymakers; Contribution of working group 1 to the fourth assessment report; Geneva: The Intergovernmental Panel on Climate Change; 2007. [Google Scholar]
- 12.IPCC. Towards new scenarios for analysis of emissions, climate change, impacts and response strategies. IPCC expert meeting report. 2007. Available from: http://www.ipcc.ch/pdf/supporting-material/expert-meeting-ts-scenarios.pdf.
- 13.Rogelj J, Meinshausen M, Knutti R. Global warming under old and new scenarios using IPCC climate sensitivity range estimates. Nat Clim Change. 2012;2:248–53. [Google Scholar]
- 14.IPCC. Special report. Geneva: The Intergovernmental Panel on Climate Change; 2012. Managing the risks of extreme events and disasters to advance climate change adaptation. [DOI] [PubMed] [Google Scholar]
- 15.Jendritzky G, Tinz B. The thermal environment of the human being on the global scale. Glob Health Action. 2009;2:2005. doi: 10.3402/gha.v2i0.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Oke TR. City size and the urban heat island. Atmos Environ. 1973;7:769–79. [Google Scholar]
- 17.Bridger RS. Introduction to ergonomics. 2nd ed. London: Taylor & Francis; 2003. [Google Scholar]
- 18.Hollowell DR. Human perceptions and reactions to environmental heat – a brief note of issues of concern in relation to occupational health. Glob Health Action. 2010;3:5632. doi: 10.3402/gha.v3i0.5632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bouchama A, Knochel JP. Heat stroke. N Engl J Med. 2002;346:1978–88. doi: 10.1056/NEJMra011089. [DOI] [PubMed] [Google Scholar]
- 20.Kjellstrom T, Holmer I, Lemke B. Workplace heat stress, health and productivity – an increasing challenge for low and middle income countries during climate change. Glob Health Action. 2009;2:2047. doi: 10.3402/gha.v2i0.2047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dunne JP, Stouffer RJ, John JG. Nat Clim Change. 2013. Reductions in labour capacity from heat stress under climate warming; p. 3. [DOI] [Google Scholar]
- 22.Kovats RS, Hajat S. Heat stress and public health: a critical review. Ann Rev Public Health. 2007;29:41–55. doi: 10.1146/annurev.publhealth.29.020907.090843. [DOI] [PubMed] [Google Scholar]
- 23.Greenhough G, McGeehin M, Bernard SM, Trtanj J, Riad J, Engelberg D. The potential impacts of climate variability and change on health impacts of extreme weather events in the USA. Environ Health Perspect. 2001;109:191–8. doi: 10.1289/ehp.109-1240666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.McMichael AJ, Powles JP, Butler CD, Uauy R. Food, livestock production, energy, climate change and health. Lancet. 2007;370:1253–63. doi: 10.1016/S0140-6736(07)61256-2. [DOI] [PubMed] [Google Scholar]
- 25.Rogers DJ, Randolph SE. Climate change and vector-borne diseases. Adv Parasitol. 2006;62:345–81. doi: 10.1016/S0065-308X(05)62010-6. [DOI] [PubMed] [Google Scholar]
- 26.Banu S, Hu W, Hurst C, Tong S. Dengue transmission in the Asia-Pacific region: impact of climate change and socio-environmental factors. Trop Med Int Health. 2011;16:598–607. doi: 10.1111/j.1365-3156.2011.02734.x. [DOI] [PubMed] [Google Scholar]
- 27.Beguin A, Hales S, Rocklov J, Astrom C, Louis VR, Sauerborn R. The opposing effects of climate change and socio-economic development on the global distribution of malaria. Glob Environ Change. 2011;21:1209–14. [Google Scholar]
- 28.Berry HL, Bowen K, Kjellstrom T. Climate change and mental health: a causal pathways framework. Int J Public Health. 2010;55:123–32. doi: 10.1007/s00038-009-0112-0. [DOI] [PubMed] [Google Scholar]
- 29.Kjellstrom T, Corvalan C. Framework for the development of environmental health indicators. World Health Stat Q. 1995;48:144–54. [PubMed] [Google Scholar]
- 30.Kinney P, Pascal M, Vautard R, Laaidi K. Winter mortality in a changing climate: will it go down? BEH (Inst de Veille sanitaire) 2012;12:148–51. (in French) [Google Scholar]
- 31.Lloyd SJ, Kovats RS, Chalabi Z. Climate change, crop yields, and undernutrition: development of a model to quantify the impact of climate scenarios on child undernutrition. Environ Health Perspect. 2011;119:1817–23. doi: 10.1289/ehp.1003311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kjellstrom T, Butler A-J, Lucas R, Bonita R. Public health impact of global heating due to climate change – potential effects on chronic non-communicable diseases. Int J Public Health. 2010;55:97–103. doi: 10.1007/s00038-009-0090-2. [DOI] [PubMed] [Google Scholar]
- 33.Hansen A, Bi P, Ryan P, Nitschke M, Pisaniello D, Tucker G. The effect of heat waves on hospital admissions for renal disease in a temperate city of Australia. Int J Epidemiol. 2008;37:1359–65. doi: 10.1093/ije/dyn165. [DOI] [PubMed] [Google Scholar]
- 34.Knowlton K, Rotkin-Ellman M, King G, Margolis HG, Smith D, Solomon G, et al. The 2006 California heat wave: impacts on hospitalizations and emergency department visits. Environ Health Perspect. 2009;117:61–7. doi: 10.1289/ehp.11594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Schrier RW, Hano J, Keller HI, Finkel RM, Gilliland PF, Cirksena WJ, et al. Renal, metabolic, and circulatory responses to heat and exercise. Ann Intern Med. 1970;73:213–23. doi: 10.7326/0003-4819-73-2-213. [DOI] [PubMed] [Google Scholar]
- 36.Brikowski TH, Lotan Y, Pearle MS. Climate-related increase in the prevalence of urolithiasis in the United States. Proc Natl Acad Sci U S A. 2008;105:9841–6. doi: 10.1073/pnas.0709652105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bedno SA, Li Y, Han W, Cowan DN, Scott CT, Cavicchia MA, et al. Exertional heat illness among overweight US Army recruits in basic training. Aviat Space Environ Med. 2010;81:107–11. doi: 10.3357/asem.2623.2010. [DOI] [PubMed] [Google Scholar]
- 38.Burch GE, DePasquale NP. Hot climates, man and his heart. Springfield, IL: Charles C. Thomas; 1962. [Google Scholar]
- 39.Costrini AM, Pitt HA, Gustafson AB, Uddin DE. Cardiovascular and metabolic manifestations of heat stroke and severe heat exhaustion. Am J Med. 1979;66:296–302. doi: 10.1016/0002-9343(79)90548-5. [DOI] [PubMed] [Google Scholar]
- 40.Ramsey JD, Burford CL, Beshir MY, Jensen RL. Effects of workplace thermal conditions on safe working behavior. J Safety Res. 1983;14:105–14. [Google Scholar]
- 41.Liu J, Ma F, Li Y. The Effect of Anthropogenic Heat on Local Heat Island Intensity and the Performance of Air Conditioning Systems. Adv Mater Res. 2011;250:2975–8. [Google Scholar]
- 42.Fouillet A, Rey G, Wagner V, Laaidi K, Empereur-Bissonet P, Le Tertre A, et al. Has the impact of heat waves on mortality changed in Grane since the European heat wave of summer 2003? A study of the 2006 heat wave. Int J Epidemiol. 2008;37:309–17. doi: 10.1093/ije/dym253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.McMichael AJ. Insights from past millennia into climatic impacts on human health and survival. Proc Natl Acad Sci U S A. 2012;109:4730–7. doi: 10.1073/pnas.1120177109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sherwood SC, Huber M. An adaptability limit to climate change due to heat stress. Proc Natl Acad Sci U S A. 2010;107:9552–5. doi: 10.1073/pnas.0913352107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Maloney SK, Forbes CF. What effect will a few degrees of climate change have on human heat balance? Implications for human activity. Int J Biometeorol. 2011;55:147–60. doi: 10.1007/s00484-010-0320-6. [DOI] [PubMed] [Google Scholar]
- 46.Haines A, McMichael AJ, Smith KR, Roberts I, Woodcock J, Markandya A, et al. Public health benefits of strategies to reduce greenhouse gas emissions: overview and implications for policymakers. Lancet. 2009;374:2104–14. doi: 10.1016/S0140-6736(09)61759-1. [DOI] [PubMed] [Google Scholar]
- 47.Wilkinson P, Smith KR, Davies M, Adair H, Armstrong BG, Barrett M, et al. Public health benefits of strategies to reduce greenhouse gas emissions: household energy. Lancet. 2009;374:1917–29. doi: 10.1016/S0140-6736(09)61713-X. [DOI] [PubMed] [Google Scholar]
- 48.Woodcock J, Edwards P, Tonne C, Armstrong BG, Ashiro O, Banister D, et al. Public health benefits of strategies to reduce greenhouse gas emissions: urban land transport. Lancet. 2009;374:1930–43. doi: 10.1016/S0140-6736(09)61714-1. [DOI] [PubMed] [Google Scholar]
- 49.Markandya A, Armstrong BG, Hales S, Chiabai A, Criqui P, Mima S, et al. Public health benefits of strategies to reduce greenhouse gas emissions: low-carbon electricity generation. Lancet. 2009;374:2006–15. doi: 10.1016/S0140-6736(09)61715-3. [DOI] [PubMed] [Google Scholar]
- 50.Smith KR, Jerrett M, Ross Anderson H, Burentt RT, Stone V, Derwent R, et al. Public health benefits of strategies to reduce greenhouse gas emissions: health implications of short-lived greenhouse pollutants. Lancet. 2009;374:2091–103. doi: 10.1016/S0140-6736(09)61716-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Friel S, Dangour A, Garnett T, Lock K, Butler C, Butler A, et al. Public health benefits of strategies to reduce greenhouse gas emissions: food and agriculture. Lancet. 2009;374:2016–25. doi: 10.1016/S0140-6736(09)61753-0. [DOI] [PubMed] [Google Scholar]
- 52.Dell M, Jones BF, Olken BA. Temperature and income: reconciling new cross-sectional and panel estimates. Am Econ Rev. 2009;99:198–204. [Google Scholar]