Abstract
Purpose
To report the first case of acute endophthalmitis caused by Alloiococcus otitidis after a dexamethasone intravitreal implant.
Methods
A 74-year-old female was treated with intravitreal Ozurdex® in her left eye for central retinal vein occlusion (CRVO). Best-corrected visual acuity (BCVA) in the eye was 4/20. Intravitreal injection was uneventful. At 48 h after injection, she developed ocular pain and visual acuity had dropped to light perception. Endophthalmitis associated with intravitreal injection was suspected.
Results
The patient did not show a favorable clinical response following systemic, intravitreal, and topical fortified antibiotics. We then performed a vitreous biopsy and removed the Ozurdex implant by pars plana vitrectomy. A vitreous culture was positive for A. otitidis. At the 2-month follow up, no inflammation was observed, but due to CRVO and probably aggravated by endophthalmitis, the fundus showed macular fibrosis. The final BCVA was finger counting at 30 cm in her left eye.
Conclusions
In cases of an intravitreal implant associated with endophthalmitis, we recommend removal of the device because it may act as a permanent reservoir of organisms if it remains in the vitreous cavity.
Key words: Alloiococcus otitidis, Dexamethasone implant, Endophthalmitis, Ozurdex
Introduction
Intravitreal therapy using anti-vascular endothelial growth factor agents, triamcinolone, and Ozurdex® implants has increased consistently in recent years to treat macular edema due to central or branch retinal vein occlusion (CRVO or BRVO). Although endophthalmitis is uncommon following these procedures, the incidence is increasing in parallel with the number of intravitreal interventions and it is becoming a clinical concern with potentially devastating visual outcomes [1].
The bacterial etiology of endophthalmitis usually involves Gram-positive bacteria, particularly staphylococci and streptococci [2]. Alloiococcus otitidis is a Gram-positive bacterium that previously has not been reported as a causative organism of endophthalmitis after intravitreal injection.
Case Presentation
A 74-year-old female patient was referred to our hospital for CRVO in her left eye. The right eye was normal and she had no underlying illness. Best-corrected visual acuity (BCVA) was 18/20 and 10/20 in the right and left eye, respectively. Intraocular pressure was 14 mm Hg in both eyes, and the anterior segment was unremarkable.
The fundus showed a clinical picture of a CRVO with a macular thickness of 432 µm measured by OCT. At the 1-month follow-up, the patient had a decreased visual acuity of 4/20 with an increase in central retinal thickness (466 µm).
To increase the chance of an improvement in visual acuity in her left eye, the patient was given an intravitreal Ozurdex injection after obtaining a written informed consent. The injection was performed in a minor procedure room with topical and subconjunctival anesthesia under aseptic conditions including sterile drape, sterile eyelid speculum, calipers, cotton buds, and with the surgeon using sterile gloves and a face mask. Topical lidocaine 2% gel was administered to the eye, followed by the application of povidone-iodine solution to the eyelids, lashes, and fornix. Drops of ofloxacin were instilled at the end of the procedure. Azithromycin eye drops were prescribed twice daily for 3 days.
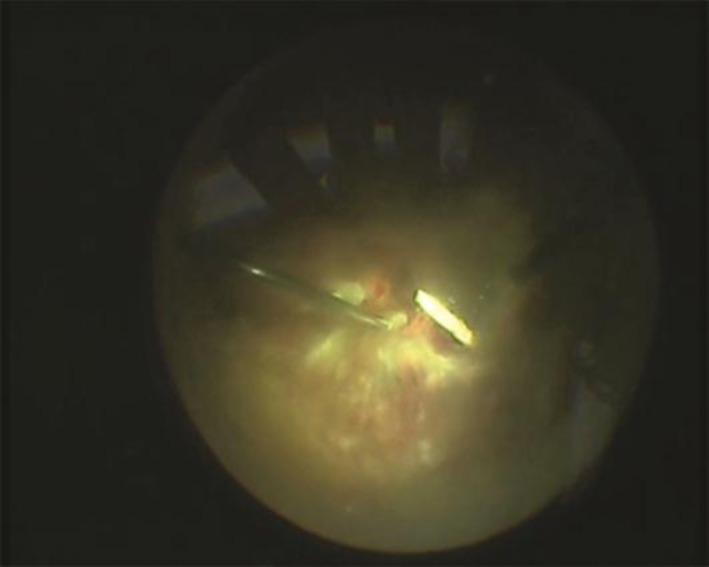
Forty-eight hours after injection, the patient developed a painful red eye, and left visual acuity had decreased to light perception. Ophthalmological examination showed conjunctival injection, hypopyon, 4+ cells, and inflammatory membrane in the anterior chamber. The lens showed moderate cataract formation as noted before injection. Fundus examination revealed a grade 4 vitreous opacity with no view of the retina. B-scan echography showed increased intravitreal echoes due to a severe inflammatory reaction without retinal detachment. Aqueous sampling for microbiological analysis was taken. As the patient was allergic to penicillin, she was treated with intravitreal vancomycin 1 mg/0.1 ml and tobramycin 0.4 mg/0.1 ml. Intravenous antibiotics (1 g vancomycin twice daily and 400 mg ciprofloxacin twice daily) and fortified vancomycin and tobramycin eye drops (every 30 min) were also administered. The aqueous culture result was negative. One week later, ophthalmological examination showed 2+ cells and a decreased inflammatory reaction without hypopyon in the anterior chamber. The dexamethasone intravitreal implant was visible and surrounded by grade III vitreous opacity. BCVA was hand movements. Pars plana vitrectomy, vitreous biopsy, and re-injection of vancomycin and tobramycin were performed 3 days later. The implant was surgically removed from the vitreous cavity by the vitreotome tip (fig. 1). One week after removal, we observed 1+ cells in the anterior chamber and grade I vitreous opacity. A vitreous specimen was cultured on conventional media (blood agar, chocolate agar, and sabouraud dextrose agar), and 2 days later, A. otitidis was isolated from blood and chocolate agar. The bacterium was sensitive to vancomycin and tobramycin. After vitrectomy, tobramycin, cycloplegic, and dexamethasone, eye drops were administered for 2 weeks.
Fig. 1.
Fundus appearance during vitrectomy. Vitreous fibrosis secondary to bacterial endophthalmitis is shown. The intravitreal implant is surrounded by grade III vitreous opacity. The implant was easily removed by the vitreotome tip.
Results
Endophthalmitis improved and no further inflammation was observed. Two months later, no cells in the anterior chamber or vitreous opacity were detected, but the retina showed macular fibrosis. BCVA in the left eye was finger counting at 30 cm.
Discussion
The dexamethasone drug delivery system (Ozurdex; Allergan, Inc., Irvine, Calif., USA) is an intravitreal device that contains 0.7 mg dexamethasone. It also contains a polymer matrix (d,l-lactide-co-glycolide) that dissolves and releases the corticosteroid into its target tissues, the retina, and vitreous over the following months. The device is inserted into the vitreous cavity through the pars plana using a 22-gauge applicator via a bi-planar injection. In 2009, the dexamethasone drug delivery system was approved by the United States Food and Drug Administration for the treatment of macular edema secondary to CRVO and BRVO. It has since become a first-line therapy [3].
Fortunately, the incidence of acute endophthalmitis following anti-vascular endothelial growth factor intravitreal injection is low, ranging from 0.02–0.05% [2]. In the recent clinical trial of the Ozurdex GENEVA Study Group [4], the main adverse ocular events after the intravitreal implant were eye pain, ocular hypertension, anterior chamber cells, cataracts, vitreous hemorrhage, and retinal detachment. No mention was made of endophthalmitis.
The most common causative organisms of infectious endophthalmitis are coagulase-negative staphylococcus (65.4%) and streptococcus species (30.8%) [2]. Irigoyen et al. [1] recently reported that streptococcal species are at least 3 times more frequent in endophthalmitis after intravitreal injections than after intraocular surgery.
The most common suspected source of post-injection endophthalmitis is normal conjunctival flora [5]. However, there is evidence that aerosolized droplet contamination from the oropharyngeal tract may be partly responsible for the relatively high rate of streptococcal endophthalmitis. Aerosol transmission may increase by talking or coughing, and an upper-respiratory viral infection can contaminate intravitreal injection. Wearing a face mask or avoiding talking during intravitreal injection procedures may help to reduce the risk of aerosol transmission [1, 2].
The Endophthalmitis Vitrectomy Study Group [6] states that immediate surgery has substantial benefit compared to antibiotic intravitreal injection in cases of endophthalmitis with light perception or less vision at presentation. However, in this case, we preferred performing vitrectomy when lack of improvement was demonstrated.
We hypothesize that in bacterial endophthalmitis associated with an intravitreal slow-release device, the infectious agent may be stationed inside the device and that this could explain the partial response to antibiotic and corticosteroid treatment in our patient. It would therefore be reasonable to remove the intravitreal implant by vitrectomy when endophthalmitis is diagnosed.
In our patient, the causative organism of endophthalmitis was A. otitidis. A. otitidis is a Gram-positive, aerobic bacterium. In 1989 [7], it was recovered for the first time from the middle ear of children with otitis media with effusion. Tano et al. [8] found a high prevalence (29%) of this bacterium in the outer ear canals of healthy people, which strongly suggests that A. otitidis is part of the normal bacterial flora of the outer ear canal and also of the nasopharynx. In our patient, we were not able to identify the source of the infection.
To our knowledge, this is the first case report of A. otitidis endophthalmitis after a dexamethasone intravitreal implant. An evidence-based guideline for the treatment of endophthalmitis associated with an intravitreal device is lacking. Further investigations are needed to establish the optimal treatment for endophthalmitis related to an intravitreal slow-release device. However, based on the evolution of our patient, removal of the implant through pars plana vitrectomy could be a good therapeutic option.
Disclosure Statement
None of the authors has conflicts of interest relevant for this paper.
Acknowledgements
The authors thank C. Newey and J. Martí for their important contribution to the development of this paper.
References
- 1.Irigoyen C, Ziahosseini K, Morphis G, Stappler T, Heimann H. Endophthalmitis following intravitreal injections. Graefes Arch Clin Exp Ophthalmol. 2012;250:499–505. doi: 10.1007/s00417-011-1851-1. [DOI] [PubMed] [Google Scholar]
- 2.McCannel CA. Meta-analysis of endophthalmitis after intravitreal injection of anti-vascular endothelial growth factor agents: causative organisms and possible prevention strategies. Retina. 2011;31:654–661. doi: 10.1097/IAE.0b013e31820a67e4. [DOI] [PubMed] [Google Scholar]
- 3.Chan A, Leung LS, Blumenkranz MS. Critical appraisal of the clinical utility of the dexamethasone intravitreal implant (Ozurdex) for the treatment of macular edema related to branch retinal vein occlusion or central retinal vein occlusion. Clin Ophthalmol. 2011;5:1043–1049. doi: 10.2147/OPTH.S13775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Haller JA, Bandello F, Belfort R, Jr, Blumenkranz MS, Gillies M, Heier J, Loewenstein A, Yoon YH, Jiao J, Li XY, Whitcup SM, Ozurdex GENEVA Study Group. Li J. Dexamethasone intravitreal implant in patients with macular edema related to branch or central retinal vein occlusion twelve-month study results. Ophthalmology. 2011;118:2453–2460. doi: 10.1016/j.ophtha.2011.05.014. [DOI] [PubMed] [Google Scholar]
- 5.Speaker MG, Milch FA, Shah MK, Eisner W, Kreiswirth BN. Role of external bacterial flora in the pathogenesis of acute postoperative endophthalmitis. Ophthalmology. 1991;98:639–649. doi: 10.1016/s0161-6420(91)32239-5. [DOI] [PubMed] [Google Scholar]
- 6.Endophthalmitis Vitrectomy Study Group Results of the endophthalmitis vitrectomy study. A randomized trial of immediate vitrectomy and of intravenous antibiotics for the treatment of postoperative bacterial endophthalmitis. Arch Ophthalmol. 1995;113:1479–1496. [PubMed] [Google Scholar]
- 7.Harimaya A, Takada R, Hendolin PH, Fujii N, Ylikoski J, Himi T. High incidence of Alloiococcus otitidis in children with otitis media, despite treatment with antibiotics. J Clin Microbiol. 2006;44:946–949. doi: 10.1128/JCM.44.3.946-949.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tano K, von Essen R, Eriksson PO, Sjöstedt A. Alloiococcus otitidis–otitis media pathogen or normal bacterial flora? APMIS. 2008;116:785–790. doi: 10.1111/j.1600-0463.2008.01003.x. [DOI] [PubMed] [Google Scholar]