Abstract
Introduction: Treatment of complex fracture patterns of the proximal humerus continues to be a challenging and controversial clinical scenario. The aim of this study was to report on the outcomes of complex displaced 3- and 4-part fractures of the proximal humerus treated with locked plating and compare the functional results of patients on the basis of age at time of injury. Methods: A retrospective review was completed to identify patients whom had sustained a 3- or 4-part fracture of the proximal humerus (Neer classification), treated surgically with locked compression plating. Patients were recruited for a final follow-up, with clinical (Constant and Disabilities of the Arm, Shoulder, Hand [DASH] scores) and radiographic outcome analysis. Results were compared (t test and Wilcoxon test) with fracture type (3- vs 4-part) and patient age at time of fracture (<65 years vs >65years) as the primary outcome measure. The presence or absence of a complication and presence or absence of a concomitant osseous injury at the time of presentation were evaluated as secondary outcome measures, in regard to overall functional results of the treatment in question. Complications were defined as posttraumatic osteoarthritis, avascular necrosis of the humeral head, and screw cutout with chondrolysis. The null hypothesis being that age of the patient at the time of injury would not greatly affect functional outcome measurements. Results: Forty-five fractures were identified in 45 patients, with 31 three-part fractures and 14 four-part fractures, and 17 patients were available for final follow-up (9 three-part and 8 four-part). Twelve patients were identified as under the age of 65 years and were compared with 5 patients who were identified as older than 65 years of age. The relative Constant score, at final follow-up, for those under the age of 65 was 88.58, while the score for those above the age of 65 was 82.5. In a similar fashion, the DASH score for those younger than 65 was 11.67, while the score for those older than 65 was 12.5. Neither the Constant score nor the DASH score differed in a statistically significant manner, when comparing patients who were younger than 65 to those older than 65 years of age. Conclusion: The current series of fractures was able to demonstrate similar and satisfactory outcomes following locked plating treatment of complex 3- and 4-part proximal humerus fractures in younger patients and patients older than the age of 65, while still accepting the null hypothesis.
Keywords: proximal humerus, locking plates, shoulder girdle trauma, geriatric fractures, osteosynthesis
Introduction
Fractures of the proximal humerus account for 5% of all fractures1 and are the third most common fracture pattern occurring in individuals over the age of 65.2 The vast majority of these fractures are relatively nondisplaced and can be successfully managed with nonoperative means.3,4 With the advent of locking plate technology and the development of proximal humerus locking plates, open reduction and internal fixation (ORIF), for the treatment of displaced and unstable proximal humerus fractures, has garnered a great deal of recent clinical attention.5–8 Treatment of complex fracture patterns, especially in the elderly individuals, continues to be a challenging and controversial clinical scenario, and there still remains no consensus for the optimal treatment algorithm for these types of fractures.9
More current data, concerning the use of locking plates in the treatment of proximal humerus fractures, has been very encouraging.5,7 However, these larger series have included less complex fracture patterns (2-part Neer classification and type A AO/OTA [Arbeitsgemeinschaft für Osteosynthesefragen/Orthopaedic Trauma Association] classification) as part of their overall appraisal of outcomes following ORIF of proximal humerus fractures with locked plating. In addition, other studies have focused their attention on postoperative complications,6 with relatively short follow-up, patient populations affected by osteoporosis,10 or the effect of reduction on functional outcome.11 A recent meta-analysis concluded that there was insufficient evidence to determine the optimal treatment for patients with displaced fractures of the proximal humerus.12
The aim of this study was to report on the mid-term outcomes of complex displaced 3- and 4-part fractures of the proximal humerus treated with locked plating and compare the results of osteosynthesis between patients that were younger the age of 65 at the time of injury to those patients who were older than 65 at the time of initial injury. The hypothesis being that these more complex fracture patterns would still offer favorable and similar results, between treatment groups, with ORIF, using locking plate technology.
Methods
A retrospective chart review was undertaken to identify patients whom had sustained a fracture of the proximal portion of the humerus between the years 2003 and 2006 and subsequently underwent ORIF with a locking compression plate. All patients were treated at a level I trauma center, and all operating surgeons were fellowship trained orthopedic trauma surgeons. Furthermore, displaced 3- and 4-part fracture patterns were distinguished for patient recruitment for final follow-up visit and outcomes analysis. Fracture pattern grading was accomplished, radiographically, through the Neer classification system,13,14 a part being considered displaced if it had been separated from its neighboring segment by more than 1 cm or angulated by greater than 45 degrees.14 Inclusion criteria for the study consisted of (1) displaced 3- or 4-part fractures of the proximal humerus, (2) skeletal maturity and 18 years of age or older, and (3) fixation of a fracture no more than 3 weeks old. Patients with 2-part displaced fractures, those younger than 18 years of age and those treated after the acute period of 3 weeks were excluded from analysis. The study was performed at a level I trauma center and approved by the Institutional Review Board prior to its commencement.
All patients with a minimum of 12 months of follow-up were recruited for outcome analysis data using plain radiographs (anteroposterior [AP], lateral, and axillary), Constant scores (CS)15,16 of both the affected and unaffected shoulder, and Disabilities of the Arm, Shoulder, Hand (DASH) score.17,25 Demographic data including age at the time of injury, sex, and concomitant injury patterns were also collected at the time of final follow-up. Constant scores were also measured as the percentage of the contralateral side because often scores represent little value in expressing functional outcome in those who were previously frail prior to their injury. Therefore, the CS is often more relevant when considered in relation to the healthy contralateral side.7This “relative” CS is especially valuable when assessing the outcomes in an elderly population. The CS was graded as poor (0-55 points), moderate (56-70 points), good (71-85 points), or excellent (86-100 points).8,9 Final fracture classification, adequacy of reduction, presence of union, osteonecrosis, and postoperative radiographic complications (failure of hardware, screw cutout, and chondrolysis) were determined by the senior authors (T.L. and J.W.). A consensus was reached when there was a discrepancy regarding any of the above outcome measures.
All patients underwent operative fixation of their proximal humerus fracture with standard Synthes proximal humerus locking plate (Synthes, Paoli, Pennsylvania). Surgical decision making was determined after a review of injury radiographs and a thorough preoperative discussion with the patient was undertaken. The decision to treat the proximal humerus fracture operatively with ORIF versus hemiarthroplasty or nonoperatively was based on fracture pattern and patient preference. In general, fracture osteosynthesis is performed regardless of patient age, this decision is based upon the amenability of the fracture to plate fixation and the overall viability of the humeral head based on injury pattern. Surgery was performed in the beach chair position, on a radiolucent table, with the aid of intraoperative fluoroscopy to allow visualization of the fracture fragments in 2 planes. An anterior deltopectoral approach was chosen for exposure of all fractures. Reduction was achieved with direct visualization of all fracture fragments, transosseous sutures were occasionally used for assistance with the reduction of tuberosity fragments. Provisional reduction and fixation, with K-wires, allowed for fluoroscopic confirmation of fracture reduction. A 3- or 5-hole plate was chosen for final fixation based on the level of extension of the fracture into the diaphysis of the humerus. The plate was positioned with the aid of an aiming device 5 to 8 mm distal to the upper end of the tuberosity and 2 to 4 mm posterior to the bicipital groove. Five to six locking, angularly stable, screws were placed into the humeral head and a standard 3 to 4 cortical screws were placed in the shaft. Final intraoperative images were taken to verify correct screw placement, and range-of-motion was assessed to minimize the risk of any postoperative impingement (Figure1).
Figure 1.
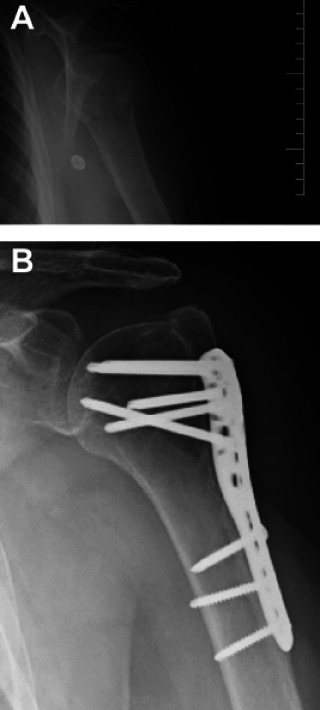
A, Preoperative radiographs of a patient who sustained a 3-part head splitting fracture. B, X-rays of the patient 43.5 months postoperative.
Postoperatively the patients were immobilized in a sling and passive range-of-motion exercises were initiated within 1 to 2 weeks. Controlled active mobilization was started 4 to 6 weeks into the postoperative course and focused on abduction and forward flexion greater than 90 degrees. Initiation of these exercises depends upon bone quality and stability of fixation achieved through osteosynthesis. Follow-up appointments, at regularly scheduled intervals, were arranged to assess position of the plate and adequacy of fracture healing.
After final follow-up, review of postoperative radiographs and tabulation of the outcome scores, a post hoc statistical analysis, was preformed primarily comparing results of the above-mentioned outcome scores with fracture type (3- vs 4-part) and age of the patient at the time of injury (<65 vs >65years). Secondary outcome measures were also compared with fracture type, presence or absence of a complication and presence or absence of a concomitant significant osseous injury (long bone injury that either required immobilization or surgical stabilization) at the time of initial presentation. Outcome measurements were performed by a trained research assistant who was blinded to the treating surgeon and initial injury pattern. Results were analyzed with variable-comparison test methods, the t test, and the Wilcoxon test, after a normality assessment of each outcome variable was first determined to ascertain whether results fell within normal or non-normal distributions. Constant scores of the affected and unaffected side were normally distributed and were analyzed with the t test. Both DASH scores and the CS as a percentage of the contralateral side followed a non-normal distribution and were analyzed using the Wilcoxon test. Statistical significance was set at P < .05.
Results
Forty-five fractures were identified in 45 patients who met the above inclusion criteria. In total, 31 three-part fractures and 14 four-part fractures were identified. Seventeen patients were available for final clinical and radiographic follow-up and outcome analysis. Of the 17 patients who were available for final follow-up, 9 had sustained a 3-part fracture and 8 had sustained a 4-part fracture. Average age at the time of injury was 57 years (range 32-76 years), and average final follow-up time was 37 months (range 12-65.5 months). Twelve patients were under the age of 65 years, while 5 patients were greater than 65 years old at the time of their proximal humerus fracture. In total, 5 patients sustained a total of 12 concomitant significant osseous injuries at the time of their proximal humerus fracture. Five of 17 patients sustained a total of 9 complications. A total of 4 patients had posttraumatic osteoarthrosis of the glenohumeral joint (2 of which had preexisting radiographic evidence of glenohumeral arthritis), while 2 patients had radiographic evidence of varus malreduction at final follow-up. Three of 17 patients had screw cutout of at least one locking screw into the humeral head, and one of these 3 patients sustained significant screw cutout and chondrolysis; necessitating revision to a hemiarthroplasty implant (Figure 2). It is of the authors’ opinion that the patient most likely had an initial varus malreduction of the fracture; however, osteoporotic collapse of the fractures should not be excluded as a possible cause of this complication.
Figure 2.
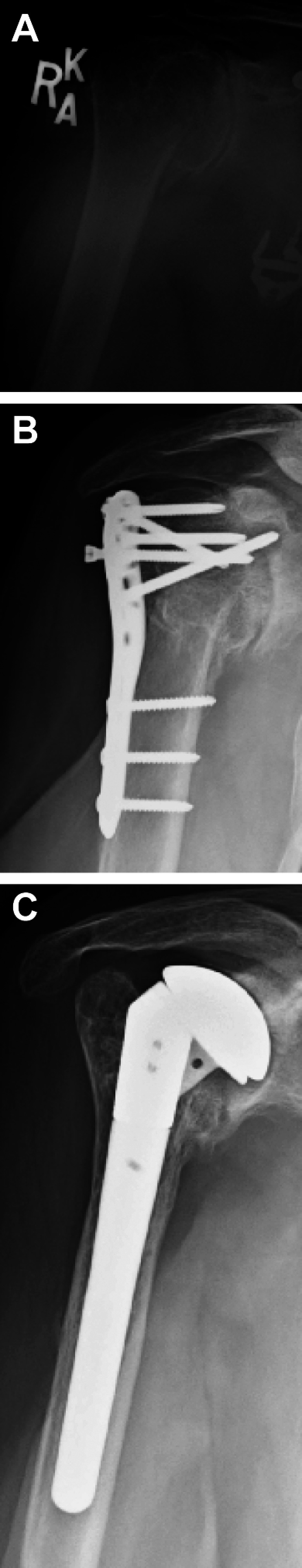
A, Initial injury films of a 76-year-old female who sustained a 4-part proximal humerus fractures. B, The 10-month postoperative x-rays of the patient; the screw cutout and failure of hardware is evident. C, Revision to a hemiarthroplasty implant in the patient.
Mean CS of the affected shoulder at final follow-up was 71 points (range 34-98). While mean CS as a percentage of the contralateral shoulder (relative score) was 84% (range 44%-126%). At final analysis, the difference between raw CS and relative CS was not significantly affected by incidence of fracture pattern (3- vs 4-part), or age of the patient at the time of injury to the proximal humerus (<65 vs >65 years; Table 1). The raw CS for those younger than 65 was 75.67 points, and the relative CS was 88.58 points. The raw CS for those older than 65 was 58 points and the relative CS was 82.5 points. Neither the raw CS nor the relative CS differed in a statistically significant manner for those above the age of 65 compared to those patients below the age of 65 (P values .07 and .19). Furthermore, presence of a postoperative complication or presence of a concomitant osseous injury at the time of fracture, possibly affecting the patient’s postoperative rehabilitation course, did not alter score results. Of the 17 patients evaluated at final follow-up, 11 of 17 achieved a good or excellent result on the basis of their CS, while 6 of 17 achieved a poor or moderate result (Table 1).
Table 1.
Patient Demographics by Age
| N | Average age | ASA score | Charlson index | |
|---|---|---|---|---|
| Group I | 12 | 51 years (32-61) | 1.4 (1-2) | 0.8 (0-2) |
| Group II | 5 | 72 years (69-76) | 2 (2) | 3.6 (3-5) |
Abbreviation: ASA, American Society of Anesthesiologists.
The mean DASH score of the affected upper extremity was 18 points (range 0-68). For individuals who were younger than 65, the mean DASH score was 11.67 points compared to a DASH score of 12.5 points for those individuals older than 65 years of age. This difference was not deemed to be statistically significant (P value = .46). Interestingly, median DASH scores of those patients who sustained a 3-part fracture were 15.83 points, while those who sustained a 4-part fracture was 8.75 points. This difference was determined to be statistically significant based on Wilcoxon analysis with a P value = .03. For all other parameters, the result of the DASH score was not significantly affected by fracture type (presence of postoperative complication or concomitant osseous injury; Table 2).
Table 2.
Results Regarding Functional Outcomes of Fractures in Relation to Fracture Pattern and Age of the Patient
| N | Constant score | P value | Relative constant score | P value | DASH score | P value | |
|---|---|---|---|---|---|---|---|
| Neer classification | |||||||
| 3 part | 9 | 68.44 | .65 | 86.21 | .48 | 15.83 | .03 |
| 4 part | 8 | 72.75 | 90.38 | 8.75 | |||
| Patient age | |||||||
| <65 years | 12 | 75.67 | .07 | 88.58 | .19 | 11.67 | .46 |
| ≥65 years | 5 | 58 | 82.5 | 12.5 | |||
Discussion
Complex 3- and 4-part fractures of the proximal humerus have notoriously behaved as a clinical dilemma. While Neer’s original work suggests that operative intervention in these fracture patterns will produce improved results, in light of the inferior results of nonoperative treatment,13 the precise method of surgical intervention remains controversial.15 Furthermore, the appropriate type of intervention, operative (ORIF or hemiarthroplasty) or nonoperative in the elderly, low-demand patient, also remains contentious.9 With the advent of locked plating techniques, there is a clear trend toward ORIF with all displaced fractures of the proximal humerus5–7,9; however, even a recent meta-analysis of the literature was unable to discern a benefit from internal fixation or arthroplasty for treatment of these complex fracture patterns.12 The importance of this clinical question becomes more apparent since revision arthroplasty for failed ORIF has historically poor results.18,19The current series of 17 fractures was able to demonstrate satisfactory outcomes following locked plating treatment of complex proximal humerus fractures, while accepting the null hypothesis that no single objective finding of fracture pattern, age, presence or postoperative complications, or concomitant injury would greatly affect functional outcomes. Importantly, age of the patient (<65 vs >65 years) did not have a statistically significant impact on the results of operative intervention. Thus, pointing to the fact that even elderly patients should be considered suitable candidates for operative osteosynthesis with locked plating, in the face of a complex proximal humerus fracture.
The average relative CS was 84% of the unaffected side, with the majority of our patients having good to excellent results. The mean DASH score of all patients was 18 points. These results are in line with larger prospective studies that have reviewed functional results for ORIF of displaced proximal humeral fractures. Brunner et al reviewed 158 fractures 12 months after surgery and discovered a mean CS of 72 points (87% of the contralateral) and mean DASH score of 16 points.7 However, their final analysis of functional shoulder scores did not distinguish between the less complicated type A fracture (AO/OTA classification) and the more complex type C fracture.
Our results also compare favorably with the published functional results following hemiarthroplasty for proximal humerus fractures. Kontakis et al was able to “systemically” review hemiarthroplasty for acute intervention of proximal humerus fractures and identified a total of 808 patients among 16 different studies. Most fractures were complex, and the mean CS was only 56.63 points at final follow-up. They concluded that while hemiarthroplasty provided excellent pain relief, functional outcomes may be variable and unpredictable.20Hemiarthroplasty has been advocated for displaced 3- and 4-part fractures because of the association with osteonecrosis and the higher risk of complication.21No patients in our series experienced radiographic findings of avascular necrosis (AVN); thus, its incidence did not correlate with final outcome. However, it must be noted that AVN can often occur many years after the initial trauma and subsequent surgery. Thus, with an average follow-up time of 3 years, the true rate of AVN maybe under estimated. This finding is more consistent with recent reports that AVN is difficult to predict and may have limited correlation with pain and function.22 In our series, patient age at the time of injury did not significantly affect functional outcome. The DASH scores, CS, or relative CS were not significantly different for patients greater than 65 years of age, in comparison with patients younger than 65 years of age. This finding is in contrast to previously reported data that has found a correlation between patient age and outcome. Owsley et al reported a significant increase of complication rate in their elderly patients.23 In addition, a multicenter trial found a relative risk increase of 3.3 of implant-related complications in the their elderly population, and the number of postoperative complication was directly corollary with functional outcome.7
Our study does contain a number of limitations, most notably its small sample size and retrospective nature. We were able to identify 45 fractures that fit our criteria and only achieved a 38% final follow-up for radiographic and clinical assessment. We were still able to perform a post hoc statistical analysis and variable-comparisons tests to analyze our functional outcomes with a number of objective variables. It is also worth noting that due to our study’s retrospective nature, we were unable to successfully perform any osteoporosis assessment of our patients and thus does not allow us to determine whether any of our patients had subsequent fragility fractures. Our data should be taken in concert with the growing body of literature concerning fixation of proximal humerus fractures and demonstrate the need for a prospective study comparing outcomes of complex fractures treated, in elderly patients, with either locked plating or hemiarthroplasty. A finding that merits further consideration is the significantly higher DASH score of patients with 4-part fractures. The authors believe this result occurred for 2 reasons. The first being that in our series 4-part fractures were more likely to be in association with initial valgus impaction, a deformity that traditionally dictates favorable surgical results. The second reason being that the patient with the highest DASH score of 68.3 points (23 points higher than the next highest score) did sustain a 3-part fracture, thus another limitation that may have been avoided with a larger sample size. A final limitation in our study maybe in the bias of treatment modality, in so far as our institution’s preferred treatment for displaced proximal humerus fractures is with plate osteosynthesis and not hemiarthroplasty. We feel that fracture pattern and not age should determine the treatment modality of choice for a displaced proximal humerus fracture. However, our preliminary results are relatively encouraging, when comparing treatment outcomes with the age of the patient at the time of injury.
Strengths of our study include the relatively sizeable mean final follow-up time of 37 months. Most series describing results after locked plating treatment of proximal humerus fractures report short-term outcomes from an average of 19 weeks to 12 months.5–7,9,24 Another inherent strength is the focus on complex fracture patterns which currently do not have a gold standard of care. Here, we are able to report on more mid-term results for treatment of more complex proximal humerus fractures.
In conclusion, ORIF with locked plating can offer consistent satisfactory clinical results for complex 3- and 4-part proximal humerus fractures, results that are compatible regardless of patient age. Expansion of its uses and indications for fracture patterns once thought suitable for humeral head replacement may be warranted. To fully elucidate appropriate treatment for the elderly patient with a complex proximal humerus fracture future, well-powered randomized trials need to be conducted comparing the outcomes of nonoperative treatment, ORIF, and proximal humeral head replacement.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Helmy N, Hinterman B. New trends in treatment of proximal humerus fractures. Clin Orthop Relat Res. 2006; 442: 100–108 [DOI] [PubMed] [Google Scholar]
- 2. Baron JA, Barrett JA, Karagas MR. The epidemiology of peripheral fractures. Bone. 1996; 18(3 suppl): 209S–213S [DOI] [PubMed] [Google Scholar]
- 3. Court-Brown CM, Caesar B. Epidemiology of adult fractures. Injury. 2006; 37(8): 691–697 [DOI] [PubMed] [Google Scholar]
- 4. Zyto K. Non-operative treatment of comminuted fractures of the proximal humerus in elderly patients. Injury. 1998; 29(5): 349–352 [DOI] [PubMed] [Google Scholar]
- 5. Sudkamp N, Bayer J, Hepp P, et al. Open reduction and internal fixation of proximal humerus fractures with the use of the locking proximal humerus plate. J Bone Joint Surg Am. 2009; 91(6): 1320–1328 [DOI] [PubMed] [Google Scholar]
- 6. Agudelo J, Schurman M, Stahel P, et al. Analysis of efficacy and failure in proximal humerus fractures treated with locking plates. J Orthop Trauma. 2007; 21(10): 676–681 [DOI] [PubMed] [Google Scholar]
- 7. Brunner F, Sommer C, Bahrs C, et al. Open reduction and internal fixation of proximal humerus fractures using proximal humeral locked plate: a prospective multicenter analysis. J Orthop Trauma. 2009; 23(3): 163–172 [DOI] [PubMed] [Google Scholar]
- 8. Wijgman AJ, Rookler W, Patt TW, et al. Open reduction and internal fixation of three and four-part fractures of the proximal humerus. J Bone and Joint Surg Am. 2002; 84(11): 1920–1925 [PubMed] [Google Scholar]
- 9. Bjorkenheim JM, Pajarinen J, Savolainen V. Internal fixation of proximal humeral fractures with a locking compression plate. Acta Orthop Scand. 2004; 75(6): 741–745 [DOI] [PubMed] [Google Scholar]
- 10. Bastian J, Hertel R. Osteosynthesis and hemiarthroplasty of fractures of the proximal humerus: outcomes in a consecutive case series. J Shoulder Elbow Surg. 2009; 18(2): 216–219 [DOI] [PubMed] [Google Scholar]
- 11. Solberg BD, Moon CN, Franco DP, et al. Locked plating of 3- and 4- part proximal humerus fractures in older patients: the effect of initial fracture pattern on outcome. J Orthop Trauma. 2009; 23(2): 113–119 [DOI] [PubMed] [Google Scholar]
- 12. Bhandari M, Matthys G, McKee MD. Four part fractures of the proximal humerus. J Orthop Trauma. 2004; 18(2): 126–127 [DOI] [PubMed] [Google Scholar]
- 13. Neer CS II. Displaced proximal humeral fractures: part I. Classification and evaluation. J Bone and Joint Surg Am. 1970; 52(6): 1077–1089 [PubMed] [Google Scholar]
- 14. Neer CS II. Displaced proximal humeral fractures: part II. Treatment of three-part and four-part displacement. J Bone Joint Surg Am. 1970; 52(6): 1090–1103 [PubMed] [Google Scholar]
- 15. Naranja RJ, Iannotti JP. Displaced three- and four- part proximal humerus fractures: evaluation and management. JAAOS. 2000; 8(6): 373–382 [DOI] [PubMed] [Google Scholar]
- 16. Constant CR, Gerber C, Emery RJ, et al. A review of the constant score: modifications and guidelines for its use. J Shoulder Elbow Surg. 2008; 17(2): 355–361 [DOI] [PubMed] [Google Scholar]
- 17. Bankes MJ, Crossman JE, Emery RJ. A standard method of shoulder strength measurement for the constant score with a spring balance. J Shoulder Elbow Surg. 1998; 7(2): 116–121 [DOI] [PubMed] [Google Scholar]
- 18. Tanner MW, Cofield RH. Prosthetic arthroplasty for fractures and fracture-dislocations of the proximal humerus. Clin Orthop Relat Res. 1983; 179: 116–128 [PubMed] [Google Scholar]
- 19. Frich LH, Sojberg JO, Sneppen O. Shoulder arthroplasty in complex acute and chronic proximal humerus fractures. Orthopedics. 1991; 14(9): 949–954 [DOI] [PubMed] [Google Scholar]
- 20. Kontakis G, Koutras C, Tosounidis T, Giannoudis R. Early management of proximal humerus fractures with hemiarthroplasty: a systematic review. J Bone Joint Surg Br. 2008; 90(11): 1407–1413 [DOI] [PubMed] [Google Scholar]
- 21. Vallier HA. Treatment of proximal humerus fractures. J Orthop Trauma. 2007; 21(7): 469–476 [DOI] [PubMed] [Google Scholar]
- 22. Farmer KW, Wright TW. Three- and four-part proximal humerus fractures: open reduction and internal fixation versus arthroplasty. J Hand Surg. 2010; 35(11): 1881–1884 [DOI] [PubMed] [Google Scholar]
- 23. Owsley KC, Gorczyca JT. Fracture displacement and screw cutout after open reduction and locked plate fixation of proximal humeral fracture. J Bone Joint Surg. 2008; 90(2): 233–240 [DOI] [PubMed] [Google Scholar]
- 24. Koukakis A, Apostolou CD, Taneja T, et al. Fixation of proximal humerus fractures using the PHILOS plate. Clin Orthop Relat Res. 2006; 442: 115–120 [DOI] [PubMed] [Google Scholar]
- 25. Hudak PL, Amadio PC, Bombardier C. Development of an upper extremity outcome measure: the DASH(Disabilities of the Arm, Shoulder, and Hand). The Upper Extremity Collaborative Group (UECG). Am J Ind Med. 1996; 29(6): 602–608 [DOI] [PubMed] [Google Scholar]


