Abstract
Background
Research is limited on how the social environment of the home is related to childhood obesity.
Purpose
The purpose of this research was to examine the relationships between positive family meal practices, family stressors, and the weight of youth and to examine parental weight status as a moderator of these relationships.
Methods
The study enrolled 368 parent/child dyads from a Minnesota sample. We used mediation analysis to examine the associations
Results
Families represented by an overweight parent reported fewer positive family meal practices (p<0.001), higher levels of depression (p=0.01), and fewer family rules (p=0.02) as compared to families represented by a healthy weight parent. For overweight parents, positive family meal practices mediated the relationship between some family stressors and child weight.
Conclusions
This research suggests that the home environment may affect the weight of children in the family, and the effect is more pronounced in families with at least one overweight parent.
Keywords: Family meal practices, Family stressors, Youth weight
Introduction
A potential contributor to the epidemic of childhood obesity is the changing face of families. In the past 30 years, the proportion of dual-income households has increased from 17% to 39% as parents strive to provide for their families and as women’s role in the workplace has evolved [1]. This societal shift has meant that aspects of the home environment that may affect eating behaviors and weight outcomes of family members have changed including the frequency and quality of family meal time, foods made available at meals, the frequency of eating out, role modeling behaviors of parents and amounts of family stressors to which families are exposed. The role of the home social environment is an area of research that is understudied.
Much has been written about the relationship between family meal practices and the eating behaviors of youth in the family. In general, eating meals together as a family, having parents role model healthy eating habits and having healthful foods available in the home have been shown to be positively related to the eating habits and health outcomes of youth [2–7]. In addition, parents who have an involved and caring parenting style rather than a controlling style have children who eat healthier diets [8–10]. Several studies have examined the association of family meal frequency and obesity; findings have been inconsistent. Modest inverse associations have been found between family dinner frequency and children’s body mass index (BMI) and overweight [11–13], with fewer significant associations among adolescents [13, 14], particularly in longitudinal analyses.
Beyond family meal practices, parental role modeling and parenting style, it is reasonable to expect that other elements of home life may affect family health behaviors and outcomes. The socioeconomic status of the family has a profound impact on all health related issues including foods that are consumed and the weights of family members [15]. In addition, family level stress, strain and lack of resiliency has been examined with regard to impact on the mental and social health of families [16–18]. Family stress may stem from general causes of stress such as economic pressures in the family, strain from juggling work and family responsibilities, time demands and pressures, or the mental health status of the adults in the house including levels of depression. Stress may also be specific to health and eating activities with parents feeling stressed about having time to prepare and provide healthy foods, family satisfaction with meals, or making and enforcing family rules about meal time [14, 19].
One family stressor that has been inadequately studied is perceived and real time demands. Balancing the responsibilities of work, school and adult and youth activities is a significant challenge for most families. These time demands may reduce a parent’s real or imagined ability to support their child in practicing healthy eating and activity behaviors and their ability to engage in those behaviors themselves as good role models. Time demands may cause a parent to believe that they disappoint their child as they need to miss school or other family social events. Feeling out of balance may be a stressor for adults in the family that challenges their ability to be an intentional parent [20].
Another stressor may be parents’ perceptions of their ability to enforce rules with their child. As parents’ lives become busier fighting the battles with their child about what to eat or time spent watching television may slip as a priority; family peace and relaxation may be more important than standing one’s ground with regard to eating and television conflict. It is also possible that parents that fear they are disappointing their child may be more willing to give into their requests for treats or more screen time.
Parents may also be stressed by their internal expectation that there should be family rules about what and when children eat and how much television that they watch; stress comes from an expectation that, as adults, they should be in control and is heightened when actual control is elusive [21]. It may well be that stress comes from a disconnect between past family history (i.e., “When I was a kid…”) and the options that contemporary families have with regard to family meal practices, time demands, and the ability to have and enforce rules.
To our knowledge, there is no examination of these potential family stressors and how they may affect the eating, activity and weight-related outcomes of children in the home. It is reasonable to expect that higher levels of stressors makes it more difficult to practice healthy family meal practices and that both are related to weight-related outcomes of family members.
It is also reasonable to expect that the weight status of an adult in the family may affect family meal practices and stressors. With over 60% of adults in the United States being overweight or obese [22], examining the potential impact of adults’ weight status on how they manage meal times and family stressors is warranted. Adults’ own struggles with food choices, portion size, and mindless eating are likely to be evident in their own eating patterns and the food choices available at home. A “do what I say and not what I do” approach to health behaviors is not likely to be successful. However, very little has been written about how the weight status of adult family members affects the family meal environment and what has been examined has had a very narrow focus [23].
The purpose of this research was to examine the relationships between positive family meal practices, family stressors and the weight of youth and adult family members and to examine parental weight status as a moderator of these relationships. To that end, this paper (1) describes a set of newly developed measures to assess family meal practices and stressors hypothesized to be related to the weight of children in the family, (2) examines the extent to which variables representing family meal practices and family stressors differ by the weight status of the participating adult, (3) evaluates whether family meal practices mediate the relationship between family stressors and child’s BMI, and (4) examines parental weight as a moderator of the relationships. We hypothesize that positive family meal practices will mediate the relationship between family stressors and child BMI status and that the relationships will differ in families where at least one parent is overweight.
Methods
This research is from the Etiology of Childhood Obesity study, a longitudinal cohort study examining factors at multiple levels of influence that may affect obesity risk in youth. The conceptual model used in the Etiology Of Childhood Obesity research is described elsewhere [24]. In brief, the etiologic research from which this study is drawn examines correlates and predictors of factors believed to be associated with unhealthy weight gain in youth including individual-level attitudes and behaviors of youth and one adult in their family, the home and school environment and the physical environment of neighborhoods surrounding the child’s school and home using Geographical Information Systems. The University of Minnesota’s Institutional Review Board approved the study. Data specific to this research are drawn from the youth and parent data.
Sample and Recruitment
From June 2007 through March 2008, 374 parent/child dyads were recruited from the membership of Health Partners health plan within the seven-county metropolitan area of Minneapolis and St. Paul, Minnesota. In order to recruit a sample representing both healthy and overweight youth and adults, recruitment was targeted to fill a 2×2 table crossing child weight status (<85th% for sex/age vs. ≥85th% for sex/age) with parent weight status (BMI<25 vs. BMI≥25). Additional goals were to recruit a sample including at least 20% racial and ethnicity minorities, and to obtain a sample with a moderate amount of clustering by school (e.g., multiple students per school).
To be eligible for enrollment, youth were required to be current Health Partners members, in grades 6 through 11 in the fall of 2007, residing in one of the randomly selected middle or high-school districts included in the sample, have a parent willing to participate and be willing to allow their names and contact information to be sent from Health Partners to the study team at University of Minnesota for further eligibility screening, consent and measurement. Parent/child dyads were ineligible if they planned to move from the area in the next 3 years, had a medical condition that affected their growth, were non-English speaking or otherwise had difficulty comprehending English, or had any other physical or emotional condition that would affect their diet/activity levels or make it difficult to complete measurements. Recruitment was initiated at Health Partners through invitation letters mailed to the participants’ homes. These letters invited parents to contact the study team at the University of Minnesota if potentially interested for further eligibility screening.
Measures
Child and parent height, weight and body composition were taken at a clinic visit by trained staff using a Shorr height board and a Tanita bioelectrical impedance device that assesses body weight and composition. For the youth, BMI z scores were derived from data from the Centers for Disease Control and Prevention Growth Charts [25]. Underweight students (<5th percentile for BMI) were dropped from this analysis (n=6). For the parents, healthy weight was defined as BMI≤25 kg/m2 and overweight/ obese defined as BMI >25 kg/m2.
Parents also completed a self-report survey that included parent sex, age and race and elicited information on socioeconomic status including parental education level and if the family qualified for free and reduced meals at the child’s school. Child’s age and sex was taken from the student survey.
The parent survey also included items to assess (1) positive family meal practices based on practices identified in the literature as related to eating behaviors or health outcomes including; family meals eaten together, meals eaten in the car, purchasing foods from fast food, eating with the television on, phone use during meal time and serving fruits, vegetables, milk and soft drinks at dinner time; (2) questions written to tap family stressors that potentially challenge positive family meal practices including: perceived time demands, the existence of family rules around meal time, and perceived difficulty enforcing rules; (3) depression [26]; and (4) stress [27]. We combined the positive family meal practices into an index, giving each family a point for each positive practice. For example, respondents scored a “1” if they answered that fruit was served at dinner or if they did not allow their child to watch television during a meal. Throughout the paper, we use the term “family stressors” to describe the items tapping stressors specific to meal time as well as the more general measures of depression and stress. Face validity of the newly created questions was established through consultation with experts in the field and internal consistency of the scales was evaluated using Cronbach’s alpha. Table 1 shows the questions representing the positive family meal practices index and the family stressors. All of the scales show moderate to good internal consistency including: time demands (α=0.81), family rules (α=0.62), rule enforcement (α=0.82), the depression scale [26] (α=0.82), and the stress scales [27] (α=0.78). In addition, construct validity was assessed by examining the bivariate relationships between the constructs and health-related outcomes, including child and parent BMI. As expected, the positive family meal practice index was inversely related to child BMI (r=−0.29; p<0.0001) and parent BMI (r=−0.30; p< 0.0001). Likewise, perception of more time demands was positively related to child BMI (r=0.15; p=0.003) and adult BMI (r=0.17; p=0.001).
Table 1.
Item descriptions, response options, and internal consistency reliability of major variables and constructs. (n=368)
| Construct, source, Cronbach alpha | Question |
|---|---|
| Positive family meal patterns index | During the past 7 days how many times…(response categories: never, 1–2 times, 3–4 times, 5–6 times, 7 times) |
| Source: Original | Did all, or most, of your family living in your home eat dinner or supper (i.e., the evening meal) together? |
| Cronbach α not applicable; index | Did all, or most of your family living in your home eat breakfast together? |
| Was at least one parent present when your child ate his/her evening meal? | |
| Was a family evening meal purchased from a fast food restaurant and eaten either at the fast food restaurant or at home? | |
| During the past month, how often…(response categories: never or rarely, once or twice/month, about once/week, several times/week, almost every day) | |
| Was at least one type of vegetable (other than potatoes) served at dinner in your home? | |
| Was fruit served at dinner in your home? | |
| Was milk served at dinner in your home? | |
| Were soft drinks (soda, pop) served at dinner in your home? | |
| Agree or disagree with the following statements (response categories: strongly disagree, disagree, agree, strongly agree) | |
| I allow my child to watch TV during a family meal | |
| I allow my child to answer the phone during a family meal | |
| My child often eats meals in the car (do not include snacks) | |
| Time demands | Agree or disagree with the following statements about you and your family (response categories: strongly disagree, disagree, agree, strongly agree) |
| Source: Original | I feel too busy with work or other demands |
| Cronbach α=0.81 | I often disappoint my children because I am too busy with work or other demands (for, example, miss attending your child’s sport/school events) |
| I have a healthy balance between work, other demands on my time, and quality time for my family and myself | |
| If I was less busy, I would be able to help my child make healthier food choices | |
| If I was less busy, I would be able to help my child be more physically active | |
| If I was less busy, I would be happier | |
| I am confident that I can find a healthy balance between work, other demands on my time and quality time for my family and myself | |
| If I was less busy, I would be able to eat a healthier diet | |
| If I was less busy, I would be able to be more physically active | |
| Family rules | Agree or disagree with the following statements (response categories: strongly disagree, disagree, agree, strongly agree) |
| Source: Original | We have family rules about what/when children eat |
| Cronbach α=0.62 | We have family rules about time spent on TV/video games |
| When I was a child, my parents enforced rules about what/when I ate | |
| When I was a child, my parents enforced rules about TV watching | |
| Rule enforcement | Agree or disagree with the following statements (response categories: strongly disagree, disagree, agree, strongly agree) |
| Source: Original | It is difficult for me to enforce rules about what/when my child eats |
| Cronbach α=0.82 | It is difficult for me to enforce rules about time spent on TV or video games |
| When I feel like I’ve disappointed my child, I’m more likely to give into requests for treats | |
| When I feel like I’ve disappointed my child, I’m more likely to give into requests for fast food | |
| When I feel like I’ve disappointed my child I’m more likely to give into requests to play video games or watch TV or videos | |
| Depression | During the past 12 months, how often have you been bothered or troubled by…(response categories: not at all, somewhat, very much) |
| Source: Kandel Davies [21] | Feeling too tired to do things? |
| Cronbach α=0.82 | Having trouble going to sleep or staying asleep? |
| Feeling unhappy, sad, or depressed? | |
| Feeling hopeless about the future? | |
| Feeling nervous or tense? | |
| Worrying too much about things? | |
| Changes in your appetite? | |
| Stress | In the last month, how often have you felt that…(response categories: never, almost never, sometimes, fairly often, very often) |
| Source: Cohen et al. [22] | You were unable to control the important things in your life? |
| Cronbach α=0.78] | Confident about your ability to handle your personal problems? |
| Things were going your way? | |
| Difficulties were piling up so high that you could not overcome them? |
Analyses
Descriptive characteristics of the total sample and the sample stratified by parent weight status were calculated and tested for differences by weight status using chi square and t test statistics. Mediation analyses to assess the positive family meal practice index as a potential mediator between family stressors and child BMI-z scores were conducted following the procedures suggested by MacKinnon [28]. Separate models were run for each of the family stressor variables. Unadjusted and adjusted models were run for each of the following steps: We first estimated the association for the family stressors and the outcome (BMI z score) which MacKinnon labels C. Next, we estimated the association between each family stressor variable and the mediator (positive family meal practices), which MacKinnon labels A. We estimated the association of the mediator (positive family meal practices) and the outcome (BMI z score), adjusted for the effects of the family stressor variables, which MacKinnon labels B. Finally, we assessed the effect of the family stressor on the outcome, adjusted for the mediator, which MacKinnon labels C′. The mediated effect was calculated using the product of coefficients method, as A*B [29]. The standard error was calculated using the Sobel method [30]. A statistical test of the mediated effect AB/σAB was evaluated using the z-distribution. Finally, the percentage of the association mediated by the positive family meal practice index was calculated as the estimate of the mediated effect (AB) divided by the total effect of the intervention, or (AB/AB+C).
All statistical models used generalized estimating equations to account for school level clustering. We used PROC GENMOD to perform the GEE analysis, identifying the school as the cluster in the REPEATED statement. We used robust standard errors, an independent working correlation matrix, an identify link and a normal variance function. We have data from 368 youth who were enrolled in 149 schools. With this number of schools, we are confident that the asymptotic assumption for the use of an independent working correlation is safe. As parent weight status was identified a priori as a possible effect modifier, interactions were tested on unadjusted multivariate models by parent weight status. Significant models (p<0.05) were subsequently stratified by healthy weight and overweight status of parents, with the same steps conducted for assessing mediation, in fully adjusted models. All analyses were conducted using SAS v.9.1 of the SAS System for Windows [SAS Institute, SAS/STAT, SAS Institute, Editor. 2002–2003: Cary, NC.]
Results
Univariate Results
Table 2 shows the characteristics of the total sample and stratified by the weight status of the participating parent. The total sample of responding adults was made up of 82% female respondents, was primarily Caucasian, well educated and 16% of the sample qualified for free and reduced lunch for their children at school. Across the total sample, the mean age of children represented was 14 years of age and there were slightly more females. About 1/3 of the children were classified as overweight or obese. The mean BMI z score for the children was 0.56 (sd=1.03) and the mean BMI for the participating adult was 28.04 (sd=6.58). All the items for the positive family meal practice index and family stressor variables for the total sample were near mid-range and showed good variance.
Table 2.
Demographic, weight, positive family meal practice index, and stressor scale characteristics for the total sample and stratified by parent weight status
| Total sample (n=368) | Healthy weight parent (n=151) | Overweight/obese parent (n=217) | Chi-Sqr./T-Stat | p valuea | |
|---|---|---|---|---|---|
| Variable | |||||
| Demographics and weight status: adult | |||||
| Female (%) | 82.0 | 89.4 | 78.3 | 7.68 | 0.006 |
| Parent reporting “White” race (%) | 86.4 | 95.4 | 80.2 | 17.48 | <0.001 |
| Parent with college education (%) | 64.0 | 71.3 | 59.0 | 5.87 | 0.02 |
| Family qualifies for free or reduced lunch (%) | 16.0 | 9.3 | 20.7 | 8.70 | 0.003 |
| BMI (mean, SD) | 28.04 (6.58) | 22.39 (1.91) | 31.98 (5.77) | t=−19.70 | <0.001 |
| Demographics and weight status: child | |||||
| Child age (mean, SD) | 14.0 (1.7) | 14.0 (1.7) | 14.0 (1.7) | t=0.22 | 0.82 |
| Child female (%) | 51.9 | 45.7 | 49.8 | 0.59 | 0.44 |
| Child weight status: | |||||
| Healthy weight (%) | 68.5 | 79.5 | 60.8 | 24.47 | <0.001 |
| Overweight (%) | 13.9 | 14.6 | 13.4 | ||
| Obese (%) | 17.7 | 6.0 | 25.8 | ||
| BMI z score (mean, SD) | 0.56 (1.03) | 0.19 (0.91) | 0.82 (1.03) | t=−6.02 | <0.001 |
| Parent survey data (mean, SD) | |||||
| Positive family meal practicesb (range=0–11) | 6.07 (2.39) | 6.8 (2.06) | 5.55 (2.47) | 5.10 | <0.001 |
| Depression (range=10–30) | 15.79 (4.45) | 15.10 (4.01) | 16.27 (4.69) | −2.49 | 0.01 |
| Stress (range=4–19) | 8.06 (2.91) | 7.70 (2.74) | 8.32 (2.99) | −2.03 | 0.04 |
| Time demands (range=9–32) | 20.88 (3.81) | 20.38 (3.27) | 21.22 (4.12) | −2.08 | 0.04 |
| Lack of family rules (range=4–16) | 9.61 (2.09) | 9.31 (1.96) | 9.81 (2.16) | −2.27 | 0.02 |
| Difficulty with rule enforcement (range=6–22) | 12.54 (2.90) | 12.33 (2.72) | 12.69 (3.02) | −1.18 | 0.24 |
Testing the difference between healthy weight/overweight parents
Positive family meal practices is an index comprised of 11 behaviors such as serving milk at dinner, not watching TV during dinner, and serving fruits and vegetables
As shown in Table 2, there were demographic differences between healthy weight and overweight parents and overweight parents were nearly twice as likely as healthy weight parents to have an overweight child. In relation to the positive family meal practice index and family stressor variables, compared to families represented by a healthy weight parent, the families represented by an overweight parent reported significantly fewer positive family meal practices and had higher scores on depression, stress, experienced more time demands and reported fewer family rules as compared to healthy weight parents.
Mediation Results
Table 3 shows the parameter estimates for the mediation models examining the relationship between the family stressors and child’s BMI in the total sample and also stratified by the weight status of the parent; testing for interactions suggested a stratified analysis. Column C represents the direct effect between each stressor and child BMI z score and shows a positive and statistically significant relationship for depression in all of the samples and, in the total sample and the overweight sample, a positive and statistically significant relationship between child BMI z score and stress and time demands. In the total sample and healthy weight parent sample, a positive and statistically significant relationship was also seen between child BMI z score and difficulty enforcing rules.
Table 3.
Parameter estimates for the effect of the positive family meal practice index as a mediator of family stressors on child BMI z scores, stratified by parental weight status
| C | SE C | C′ | SE C′ | A | SE A | B | SE B | AB | SE AB | z | % Med | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total sample (n=368) | ||||||||||||
| Depressiona | 0.046* | 0.011 | 0.034* | 0.011 | −0.063* | 0.027 | −0.063* | 0.025 | 0.004 | 0.002 | 1.66 | 7.5 |
| Stressa | 0.039* | 0.017 | 0.023 | 0.016 | −0.08 | 0.042 | −0.065* | 0.025 | 0.005 | 0.003 | 1.55 | 11.9 |
| Time demandsa | 0.033* | 0.014 | 0.018 | 0.014 | −0.125* | 0.029 | −0.061* | 0.025 | 0.008 | 0.004 | 2.13* | 18.6 |
| Lack of family rulesa | 0.029 | 0.027 | 0 | 0.026 | −0.253* | 0.054 | −0.069* | 0.024 | 0.017 | 0.007 | 2.4* | 37.8 |
| Difficulty enforcing rulesa | 0.039* | 0.018 | 0.019 | 0.018 | −0.199* | 0.043 | −0.061* | 0.026 | 0.012 | 0.006 | 2.13* | 23.9 |
| Healthy weight parents (n=151) | ||||||||||||
| Depression | 0.044* | 0.017 | 0.037* | 0.017 | −0.076 | 0.052 | −0.048 | 0.036 | 0.004 | 0.004 | 0.99 | 7.6 |
| Stress | 0.027 | 0.027 | 0.023 | 0.025 | −0.110 | 0.073 | −0.055 | 0.040 | 0.006 | 0.006 | 1.02 | 18.3 |
| Time demands | 0.026 | 0.020 | 0.022 | 0.019 | −0.077 | 0.053 | −0.054 | 0.036 | 0.004 | 0.004 | 1.04 | 13.8 |
| Lack of family rules | 0.007 | 0.034 | −0.001 | 0.034 | −0.138* | 0.069 | −0.059 | 0.037 | 0.008 | 0.007 | 1.25 | 53.8 |
| Difficulty enforcing rules | 0.048* | 0.024 | 0.039 | 0.025 | −0.212* | 0.056 | −0.044 | 0.037 | 0.009 | 0.008 | 1.13 | 16.3 |
| Overweight parents (n=217) | ||||||||||||
| Depression | 0.048* | 0.014 | 0.043* | 0.013 | −0.066* | 0.030 | −0.087* | 0.030 | 0.006 | 0.003 | 1.75 | 10.7 |
| Stress | 0.045* | 0.022 | 0.024 | 0.021 | −0.076 | 0.049 | −0.080* | 0.028 | 0.005 | 0.004 | 1.11 | 9.5 |
| Time demands | 0.037* | 0.017 | 0.024 | 0.018 | −0.151* | 0.033 | −0.086* | 0.028 | 0.013 | 0.005 | 2.55* | 26.0 |
| Lack of family rules | 0.043 | 0.033 | 0.012 | 0.034 | −0.326* | 0.069 | −0.096* | 0.029 | 0.313 | 0.067 | 4.68* | 42.1 |
| Difficulty enforcing rules | 0.037 | 0.023 | 0.019 | 0.024 | −0.197* | 0.056 | −0.093* | 0.030 | 0.018 | 0.008 | 2.33* | 33.1 |
Adjusted for student age, student sex, parental race, free and reduced cost lunch and parental college education (Y/N). Positive family meal practices is an index comprised of 11 behaviors such as serving milk at dinner, not watching TV during dinner and serving fruits and vegetables. C main effect of family stress variable on child BMI z score, C′ effect of family stress variable on child BMI z score adjusting for mediator, A effect of family stress variable on positive family meal practices, B effect of positive family meal practices on child BMI z score adjusting for main effect; % mediation=[AB/((AB)+C)] *100
SE standard error
Statistically significant interaction with parent weight status in crude models, p<0.05
p<0.05
The values in the A column show the relationship between each family stressor examined and the positive family meal practice index, adjusting for student age, sex, parental race, if the family qualified for free and reduced lunch, and parental education. Across all three samples, statistically significant and negative associations were seen between positive family meal practices and lack of family rules and difficulty enforcing rules; fewer rules and more problems with rule enforcement were related to less positive family meal practices. For the total sample and the sample of overweight parents, depression and perceived time demands were also negatively related to positive family meal practices.
The values in column B represent the relationship between the positive family meal practice index and child BMI z score adjusted for each family stressor. In both the total sample and the sample of overweight parents, the relationships between positive family meal practices and child BMI z score were statistically significant and negative; the relationships were stronger in the overweight sample. There were no statistically significant relationships between positive family meal practices and child BMI z scores in the families represented by a healthy weight parent.
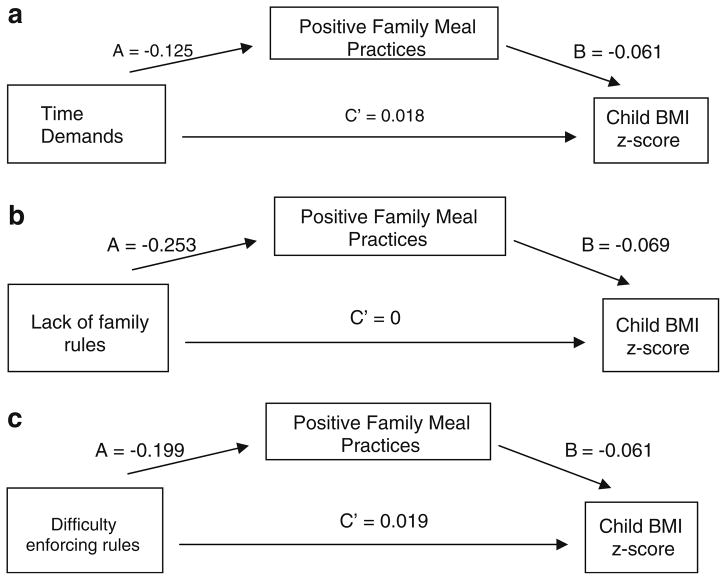
The statistical significance of the mediation analysis is identified through the z statistic and the tested relationship is illustrated in Fig. 1. For the sample that included a healthy weight parent, there was no evidence that positive family meal practices mediated the relationship between the family stressors and BMI. However, for the total sample and overweight parents, the positive family meal practice index appeared to mediate the relationship between time demands, lack of family rules and difficulty enforcing family rules and the child’s BMI. Figure 1 shows the mediation model using the total sample for the three family stressors that show statistical significance. Lack of family rules had the strongest impact in the models tested with 37.8% of the relationship between family rules and child BMI explained through family meal practices. The relationships are stronger in the overweight sample for time demands, lack of family rules and difficulty enforcing rules; in the overweight sample 42.1% of the relationship between lack of family rules and child BMI is explained through family meal practices (Table 3).
Fig. 1.
Mediation models for the effect of positive family meal practices on the relationship between significant family stressors on child BMI z scores (n=368) (Adjusted for student age, student gender, parental college education (Y/N), qualify for free or reduced cost lunch (Y/N) and parental race). a Time demands as family stressor; z score=2.13 (p<0.05); % mediation=18.6%. b Lack of family rules as a family stressor; z score=2.4 (p<0.05); % mediation=37.8. c Difficulty enforcing rules as a family stressor; z score=2.13 (p<0.05); percent mediation=23.9
Discussion
The purpose of this research was to examine the relationships between family meal practices, family stressors and the weight of youth and adult family members and to examine parental weight status as a moderator of these relationships. This research presents the positive family meal practice index as a robust construct that is related to family stressors. In addition, in families where at least one of the parents is overweight, the positive family meal practice index was negatively related to child BMI-z score and was a mediator between several family stressors and child BMI. This research also presents three newly developed constructs to assess family stressors related to time demands, lack of family rules and difficulty enforcing rules. The internal consistency and the construct validity of the scales were demonstrated.
We examined how family meal practices and family level stressors may differ by families represented by a healthy weight versus an overweight parent (Table 2). Families represented by an overweight parent reported fewer positive family meal practices as compared to families represented by a healthy weight parent (p< 0.0001). Looking at the more general measures of stress and depression, we saw differences in reported levels of stress and depression in overweight versus healthy weight families. Perceptions of time demands and lack of family rules differed by families represented by an overweight as compared to a healthy weight adult. It appears that difficulty enforcing family rules around mealtime and “giving into” children’s requests when they feel that they have disappointed their child is a stressor for all families, including families where at least one parent is at a healthy weight. We also found that the positive family meal practice index appears to be an important mediating variable in the pathway between family stressors (particularly time demands, lack of family rules and difficulty enforcing family rules) and child-level BMI but only in families where the participating adult was overweight or obese.
The literature on the relationship between family meal patterns and their impact on the weight of children has paid insufficient attention to how family meal time and stressors may vary in homes where at least one parent is overweight as compared to homes where at least one parent is at a healthy weight. In doing so, the normative influence of the parent’s own behaviors and potential struggles with their weight have been ignored. Just as adults who smoke may struggle to counsel their children not to smoke, adults who are overweight may feel hypocritical or ill equipped to advise their child to practice healthy behaviors related to weight. In addition, parents’ own preferences about what, when, where to eat and what to do or not do while eating should not be ignored as important influences on family meal patterns and behaviors and health outcomes of youth. Health professionals that are interested in preventing childhood obesity must realize that the advice we give about healthy meal practices must be heard and accepted by the adults in the family. At the very least, we must acknowledge that adults in the family may be struggling with their own attempts to maintain or achieve a healthy weight and to create healthier environments for themselves and their families. Our findings also suggest that educating parents on the importance of the 11 behaviors that compose the positive family meal practice index, regardless of other rules and stressors, may have a positive influence on the weight of children. Counseling parents to do a number of very specific mealtime behaviors as delineated in the positive family meal practice index (e.g., always serve at least one fruit and vegetable at meals, don’t offer soft drinks at meals, have an adult present at meals, turn the television off, etc.) may be easier and have a greater impact on weight status than attempting to eliminate or control stressors.
Findings from the mediation analysis suggest that in families where at least one adult is overweight, family stressors affect child level BMI both directly and through their impact on family meal practices. This finding suggests that family-based interventions may benefit from a focus on the stressors that appear to have the most potent impact on child BMI, including managing time demands, making family rules around what occurs during meal time and enforcing those rules and not giving in to children’s demands when we worry that we have disappointed them.
The findings from this research need to be viewed in light of the study’s limitations. The external validity of the study is limited by the study’s small sample of adults and youth from one metropolitan area. Further testing in larger, more diverse samples is warranted. In addition, this research only examines one adult and one child in each family. Certainly the weight of other adults and children in the family may affect the relationship between family stressors, mealtime practices and the overall meal and weight culture of family members in the household. However, to date, population level data on entire families that examine these factors are not available and would be costly to collect. Our results suggest that even having one parent that is at a healthy weight may offer some protective benefit to children in the home through more healthy family meal practices and family rules, lower levels of stress and depression and fewer perceived time demands.
Another limitation is that we did not examine how the stressors or family meal practices affect specific eating behaviors or nutrient intake. For this study we chose to use BMI as the outcome of interest, both because of its direct relationship to health outcomes and because of the minimal bias in an objective measurement of weight. Research examining which specific dietary behaviors are affected by family stressors and family meal patterns may be useful.
A final limitation is that we employed a GEE analysis for the mediation work. Mediation analyses are typically run with general linear models or general linear mixed models. We could not use these models because it was not possible to correctly model the complex correlation pattern in our data. The regression coefficients should be unaffected by GEE, and the standard errors should be correctly estimated using GEE. But we recognize that this approach has not been validated requiring caution in our interpretation.
In conclusion, this research introduces several new measures that can be used in population-based research representing family stressors and family meal practices. In addition, this research strongly suggests that the weight of adults in the family may moderate the relationship between family stressors, family meal practices and the BMI of youth in the family. These findings have implications for designing family-based programs related to promoting the healthy weight of children and for etiologic research to better understand the relationship between family meal practices, family stressors and weight of children in the family.
Footnotes
Conflict of Interest Statement The authors have no conflict of interest to disclose.
Contributor Information
Leslie A. Lytle, Email: lalytle@umn.edu, Division of Epidemiology and Community Health, School of Public Health, University of Minnesota, Minneapolis, MN 55454, USA
Mary O. Hearst, Division of Epidemiology and Community Health, School of Public Health, University of Minnesota, Minneapolis, MN 55454, USA
Jayne Fulkerson, School of Nursing, University of Minnesota, Minneapolis, MN 55454, USA
David M. Murray, Division of Epidemiology, College of Public Health, Ohio State University, Columbus, OH 43210, USA
Brian Martinson, HealthPartners Research Foundation, Minneapolis, MN, USA
Elizabeth Klein, Division of Epidemiology, College of Public Health, Ohio State University, Columbus, OH 43210, USA
Keryn Pasch, Kinesiology and Health Education, University of Texas at Austin, Austin, TX 78701, USA
Anne Samuelson, Division of Epidemiology and Community Health, School of Public Health, University of Minnesota, Minneapolis, MN 55454, USA
References
- 1. [Accessed 2006];Changes in Median Household Income: 1969 to 1996. 1998 http://www.census.gov/prod/3/98pubs/p23-196.pdf.
- 2.Patrick H, Nicklas TA. A review of family and social determinants of children’s eating patterns and diet quality. J Am Coll Nutr. 2005 Apr;24(2):83–92. doi: 10.1080/07315724.2005.10719448. [DOI] [PubMed] [Google Scholar]
- 3.Oliveria SA, Ellison RC, Moore LL, Gillman MW, Garrahie EJ, Singer MR. Parent-child relationships in nutrient intake: the Framingham children’s study. American Journal of Clinical Nutrition. 1992;56:593–598. doi: 10.1093/ajcn/56.3.593. [DOI] [PubMed] [Google Scholar]
- 4.Johnson S, Birch L. Parents’ and children’s adiposity and eating style. Pediatrics. 1994;94:653–661. [PubMed] [Google Scholar]
- 5.Gillman MW, Rifas-Shiman S, Frazier AL, et al. Family dinner and diet quality among older children and adolescents. Archives of Family Medicine. 2000;9(3):235–240. doi: 10.1001/archfami.9.3.235. [DOI] [PubMed] [Google Scholar]
- 6.Videon TM, Manning CK. Influence on adolescent eating patterns: the importance of family meals. Journal of Adolescent Health. 2003;32(5):365–373. doi: 10.1016/s1054-139x(02)00711-5. [DOI] [PubMed] [Google Scholar]
- 7.Neumark-Sztainer D, Hannan PJ, Story M, Croll J, Perry C. Family meal patterns: associations with sociodemographic characteristics and improved dietary intake among adolescents. Journal of the American Dietetic Association. 2003;103(3):317–322. doi: 10.1053/jada.2003.50048. [DOI] [PubMed] [Google Scholar]
- 8.Schmitz KH, Lytle LA, Phullips GA, Murray DM, Birnbaum AS, Kubik MY. Psychosocial correlates of physical acitivty and sedentary leisure habits in young adolescents: the teens eating for energy and nutrition at school study. Preventive Medicine. 2002;34:266–278. doi: 10.1006/pmed.2001.0982. [DOI] [PubMed] [Google Scholar]
- 9.Nicklas TA, Baranowski T, Baranowski JC, Cullen K, Rittenberry L, Olvera N. Family and child-care provider influences on preschool children’s fruit juice and vegetable consumption. Nutrition Reviews. 2001;59:224–235. doi: 10.1111/j.1753-4887.2001.tb07014.x. [DOI] [PubMed] [Google Scholar]
- 10.Kremers S, Bruga J, Hein de Vriesa D, Rutger C. Parenting style and adolescent fruit consumption. Appetite. 2003;41:43–50. doi: 10.1016/s0195-6663(03)00038-2. [DOI] [PubMed] [Google Scholar]
- 11.Gillman MW, Rifas-Shiman S, Frazier L, et al. Family dinner and diet quality among older children and adolescents. Archives of Family Medicine. 2000;9:235–240. doi: 10.1001/archfami.9.3.235. [DOI] [PubMed] [Google Scholar]
- 12.Taveras EM, Rifas-Shiman S, Berkey CS, et al. Family dinner and adolescent overweight. Obesity Research. 2005;13(5):900–906. doi: 10.1038/oby.2005.104. [DOI] [PubMed] [Google Scholar]
- 13.Sen B. Frequency of family dinner and adolescent body weight status: evidence from the national longitudinal survey of youth, 1997. Obesity (Silver Spring) 2006;14(12):2266–2276. doi: 10.1038/oby.2006.266. [DOI] [PubMed] [Google Scholar]
- 14.Fulkerson JA, Neumark-Sztainer D, Hannan PJ, Story M. Family meal frequency and weight status among adolescents: Cross-sectional and 5-year longitudinal associations. Obesity (Silver Spring) 2008;16(11):2529–2534. doi: 10.1038/oby.2008.388. [DOI] [PubMed] [Google Scholar]
- 15.Singh GK, Siahpush M, Kogan MD. Rising social inequalities in US childhood obesity, 2003–2007. Ann Epidemiol. 2010 Jan;20 (1):40–52. doi: 10.1016/j.annepidem.2009.09.008. [DOI] [PubMed] [Google Scholar]
- 16.Patterson JM. Integrating Family Resilience and Family Stress Theory. Journal of Marriage and the Family. 2002;64(2):349–360. [Google Scholar]
- 17.Keith PM, Schafer RB. Role Strain and Depression in Two-Job Families. Family Relations. 1980;29(4):483–488. [Google Scholar]
- 18.Voydanoff P. Work Role Characteristics, Family Structure Demands, and Work/Family Conflict. Journal of Marriage and the Family. 1988;50(3):749–761. [Google Scholar]
- 19.Fulkerson JA, Kubik MY, Story M, Lytle LA, Arcan C. Are there nutritional and other benefits associated with family meals among at-risk youth? Journal of Adolescent Health. doi: 10.1016/j.jadohealth.2009.02.011. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Doherty W. The Intentional Family: How to build family ties in our modern world. Reading, Massachuesetts: Addison-Wesley; 1997. [Google Scholar]
- 21.Hayes S, Strosahl K, Wilson K. Acceptance and Commitment Therapy. New York, New York: The New Guilford Press; 1999. [Google Scholar]
- 22.Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999–2004. JAMA. 2006;295(13):1549–1555. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- 23.Francis L, Lee Y, Birch L. Parental weight status and girls’ television viewing, snacking, and body mass indexes. Obesity Research. 2003;11:143–151. doi: 10.1038/oby.2003.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lytle LA. Examining the etiology of childhood obesity: The IDEA study. American Journal of Community Psychology. 2009;11:143–151. doi: 10.1007/s10464-009-9269-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Centers for Disease Control and Prevention. Growth Charts 2000. United States: 2000. [Accessed January 28, 2008]. http://www.cdc.gov/growthcharts. [Google Scholar]
- 26.Kandel DB, Davies M. Epidemiology of depressive mood in adolescents: an empirical study. Arch Gen Psychiatry. 1982 Oct;39(10):1205–1212. doi: 10.1001/archpsyc.1982.04290100065011. [DOI] [PubMed] [Google Scholar]
- 27.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. Journal of Health and Social Behavior. 1983;24(4):385–396. [PubMed] [Google Scholar]
- 28.MacKinnon DP, Fairchild AJ, Fritz MS. Mediation analysis. Annual Review of Pscyhology. 2007;58:593–614. doi: 10.1146/annurev.psych.58.110405.085542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.MacKinnon DP, Dwyer JH. Estimating mediated effects in prevention studies. Evaluation Review. 1993;17(2):144–158. [Google Scholar]
- 30.Sobel M. Some new results on indirect effects and their standard errors in covariance structure analysis. San Francisco, CA: Jossey-Bass; 1986. [Google Scholar]