Abstract
Both substance use and obesity are prevalent among youth. As youth age, substance use rates increase and over the past three decades, obesity rates among youth have tripled. While these two factors have both short- and long-term health impacts, little research has explored how substance use and obesity among youth may be related. This study explores the bi-directional longitudinal relationships between substance use and body composition. Participants (N = 704; 50.7% female) were mostly white (86.4%) with a baseline mean age of 14.7 years. Objectively measured body composition was used to calculate body mass index z-scores (BMI z-score) and percent body fat. Cross-lagged structural equation models, accounting for clustering at the school level, were run to determine the longitudinal association between body composition and self-reported substance use (alcohol, cigarette, and marijuana), adjusting for socio-demographic characteristics, pubertal status, and weight satisfaction. Baseline alcohol use predicted decreased BMI z-score at follow-up and a similar association with percent body fat approached significance. Baseline cigarette use predicted increased percent body fat. No longitudinal associations were seen between baseline body composition and future substance use. Our results suggest that substance use contributes to subsequent body composition; however, body composition does not contribute to subsequent substance use. Continued research that explores these relationships longitudinally is greatly needed.
Keywords: Body composition, Adolescents, Substance use, Obesity
Introduction
While the determinants of both substance use and obesity among youth have been well established, little research has explored the relationships between substance use and obesity. These two factors contribute to much of the disease burden in the US and other countries and, as such, their interrelationships are important to understand. Problem Behavior Theory suggests that traditional risk behaviors such as substance use and delinquency, or those behaviors that are not sanctioned by society, tend to cluster together (Jessor and Jessor 1977). While research has focused on the clustering of these traditional “risky” behaviors, it may be that additional factors should be considered in this behavioral cluster. Obesity, an important public health threat, is one such factor. Obesity among youth has not typically been thought of as a traditional risk behavior as youth substance use and delinquency commonly are. However, just as substance use and delinquency are not sanctioned by society, obesity may also fall into this domain. Therefore, we may need to re-conceptualize our definition of “risky behavior” to include factors that put youth “at risk” for negative health outcomes, such as obesity. In the present study, we propose that there are several mechanisms by which substance use and obesity may be related and test, using longitudinal, cross-lagged models, the directionality of these mechanisms.
As youth transition through adolescence, substance use becomes increasingly more common. In 2010, 14% of eighth graders in the US reported using alcohol, 8% reported using marijuana and 7% reported smoking cigarettes in the past month (Johnston et al. 2011). By the time youth reach 12th grade, these figures increase two- to three- fold; 41% will have used alcohol in the past month, 19% will have used marijuana in the past month, and 20% will have smoked cigarettes in the past month (Johnston et al. 2011). Although some engagement in substance use may be expected as a result of the individuation that occurs during adolescence, overall experimentation may be harmful in that experimentation with substance use may become problematic when individuals choose to use alcohol or marijuana as a means of coping with stressful situations.
As obesity rates among youth continue to remain high with 32% of adolescents in the US being overweight or obese (Ogden et al. 2010), it is important to also examine the co-occurrence of obesity and substance use. Overweight in youth has been defined as having a body mass index (BMI) for age and gender between the 85th and 95th percentile and obesity is defined as a BMI for age and gender greater than the 95th percentile (Ogden et al. 2010). Relatively little is known about the longitudinal associations of body composition and these prevalent youth substance use behaviors. Only recently have researchers begun to explore the relationship between weight status and the multiple risk factors that tend to co-occur among adolescents. Positive associations have been found between BMI and alcohol, cigarette and marijuana use (Farhat et al. 2010; Fonseca et al. 2009; Pasch et al. 2008). Fonseca et al. (2009) conducted a cross-sectional study to identify lifestyle factors that would differentiate overweight and obese adolescents from their peers (Fonseca et al. 2009). Using self-reported measures of height and weight to calculate BMI, the researchers found that obese teens were significantly more likely to report engaging in daily alcohol use than their healthy weight peers. Similar cross-sectional research from Farhat et al. (2010) found frequent drinking and smoking were more prevalent among younger overweight and obese girls (age <15) and older obese girls (age ≥15), compared to similar aged healthy weight counterparts, while marijuana use was more common among younger overweight girls, compared to healthy weight girls (Farhat et al. 2010). Other work from Pasch et al. (2008) found that significant cross-sectional associations between self-reported BMI and substance use (binge drinking and alcohol, tobacco, and other drug use) were not present among 7th graders, but were detected a year and a half later, among 8th grade students (Pasch et al. 2008). While these cross-sectional associations do establish the inter-relatedness of body composition and substance use, longitudinal models are needed which help to determine directionality of the casual relationships.
The relationship between youth substance use and body composition may develop through several mechanisms. One possible mechanism is that overweight and obese adolescents may use substances as a way to cope with the negative social and emotional consequences of being overweight or obese (coping model). In cross-sectional work, overweight and obese youth have been found to be victims of aggression and weight stigmatization, particularly by their peers (Pearce et al. 2002). Other research has found that nearly one-quarter to one-third of all adolescents have been teased about their weight (Neumark-Sztainer et al. 2002); however, among adolescents with the highest BMI, nearly one-half to two-thirds had been teased about their weight (Neumark-Sztainer et al. 2002). Such stigmatization could exacerbate the already difficult transition into adolescence by hindering social and emotional growth, especially since adolescents become increasingly reliant on their peers for support during this time.
Another mechanism that could explain how being overweight may increase the risk for smoking and substance use is through the use of cigarettes as a weight control strategy (weight control model). Many studies have examined the relationship between weight status and smoking. For example, Caria et al. (2009) studied the association between weight and smoking initiation in a 7-year prospective cohort study of middle adolescents (Caria et al. 2009). Using both objective and subjective reports of weight and self-reported smoking status, the researchers found that overweight was not associated with smoking initiation among males. However, among females, being overweight at baseline was significantly associated with smoking initiation. Other research has found that being overweight is predictive of smoking continuation. For example, research from O'Loughlin et al. (1998) found that weight status was not associated with smoking initiation among a sample of 9–12 year olds (O'Loughlin et al. 1998); however, among girls who had ever smoked, those who were overweight were 3.5 times more likely to continue smoking than their non-overweight counterparts. In addition, longitudinal research has shown that adolescent males with higher self-reported BMIs were more likely to smoke as young adults, but the same relationship was not found among females (Koval et al. 2008). In a sample of Dutch adolescents, weight control motivations for smoking significantly predicted the onset of smoking (Harakeh et al. 2010). Smoking as a weight control strategy is of particular concern given the many negative outcomes associated with cigarette use (United States Department of Health and Human Services 2000).
While research has found that overweight youth may use smoking as a weight control strategy, little research has explored how increased substance use, especially alcohol and marijuana use, may increase the risk of future weight gains (weight gain model). Alcohol may have an effect on energy balance as calories in alcohol could lead to weight gain over time. A recent systematic literature review conducted by the Dietary Guidelines Advisory Committee indicated that, among adults, moderate drinking is not associated with weight gain, but heavier consumption over longer periods of time may be associated with such gains (United States Department of Agriculture 2010). Marijuana use has been linked to increased appetite leading to over-consumption of calories (Kirkham 2005; Kirkham and Williams 2001). Additionally, marijuana use may decrease inhibitions which could result in excessive calorie intake or, alternatively, marijuana use may dull the incentive to be physically active. Given these outcomes associated with cigarette and marijuana use, it is important that research explores how the use of these substances may be related to subsequent changes in body composition.
Finally, another less explored mechanism for the relationships between substance use and body composition is that engagement in substance use may be the first stages in the development of a risk profile that makes youth more likely to also engage in other health compromising behaviors such as poor eating and activity-related behaviors (risk profile model). While not typically considered risky behaviors, poor eating and activity-related behaviors do put youth at risk for health problems later in life. As such, it may be necessary to consider lifestyle behaviors, along with substance use behaviors, as behaviors that put youth at risk of experiencing other health problems. In a longitudinal study of approximately 3,000 7th grade youth who were followed over 1.5 years, self-reported BMI in 7th grade was not predictive of substance use in 8th grade, however, 7th grade substance use was positively associated with 8th grade BMI. Specifically, alcohol, tobacco, and other drug use as well as fighting and depression were significant predictors of increased BMI in 8th grade (Pasch et al. 2008). These findings suggest that youth who engage in substance use at an early age may be at heightened risk for also engaging in obesity-related behaviors later in adolescence. Similarly, previous work from Lytle et al. (1995), which used serial cross-sectional samples over a 7-year period, found that smoking, poor food choices, and lower activity patterns clustered together among adolescents; prevalence rates for weekly smoking among 12th grade males were 8.8 times higher among males reporting poor eating and activity levels as compared to males reporting healthy eating and activity (Lytle et al. 1995). Additionally, cigarette and marijuana use have been found to result in poorer lung functioning (Gold et al. 1996; Hall and Degenhardt 2009) and this reduced lung function may affect youth's levels of physical activity, thus putting them at increased risk for obesity. While socio-economic status may be one explanation for these associations, there may be other possible mechanisms at play. In research by Laska et al. (2009), latent class analysis was used and found similar behavioral patterning of traditional risk and weight behaviors among young adult males and females (Laska et al. 2009), suggesting that health risk and lifestyle behaviors may be related. Further, early substance use also may encourage social connections with other youth who take risks, including overeating and being more sedentary, or early substance use may be isolating, distancing the youth who uses substances from healthy normative influences to take care of oneself.
Overall, however, previous research examining the relationships between body composition and substance use is limited. First, much of the research conducted has used cross-sectional study designs. While useful in establishing associations, the nature of the data for these studies does not allow for causal inferences to be made for the relationships found or for an examination of the change and/or stability of the behavior over time. Additionally, cross-sectional research does not allow for the exploration of the longitudinal bi-directional relationships between body composition and substance use. For example, body composition may influence substance use and substance use may influence composition. Third, both cross-sectional and longitudinal studies have tended to rely on self-reported measures of height and weight in calculating BMI. Although previous research has found these measures to be highly correlated with objectively measured height and weight (Goodman et al. 2000; Sherry et al. 2007), important biases and differential reporting errors may exist in these data. In addition, it is also possible that measures of body fat may be better predictors of future morbidity than BMI (Lahmann et al. 2002), however, previous work has focused primarily on BMI. Thus, objective body composition measures, which include both BMI and body fat, collected by trained professionals may provide more valid and robust findings. Finally, substance use in adolescence is highly clustered (Donovan et al. 1988; Jessor and Jessor 1977) and previous work has not accounted for the co-variation present among substance use behaviors. Therefore, understanding the bi-directional relationships between substance use and obesity will help to develop interventions which target the pre-cursors to the behaviors (substance use or obesity) which put youth at risk for future health problems.
Hypotheses
The purpose of the current study was to determine the bi-directional, longitudinal associations between objective measures of body composition and youth substance use. Using longitudinal analysis, we are able to add to our understanding of the causal pathways through which these behaviors develop. Specifically, the following research questions were examined. First, does body composition, assessed using objectively measured height and weight predict youth substance use 2 years later? Second, do substance use behaviors predict body composition 2 years later? We hypothesize that substance use and body composition will be associated. Specifically, body composition will predict changes in substance use through one of two mechanisms, the coping model or the weight-control model. Substance use will predict changes in body composition through one of two mechanisms, the weight gain model and the risk profile model. The limited longitudinal research in this area suggests that the weight gain or risk profile models are the most likely pathways.
Methods
Participants
Participants in this study are from two independent longitudinal samples of adolescents and one parent who took part in either the IDEA (Identifying the Determinants of Eating and Activity) or ECHO (Etiology of Childhood Obesity) cohort studies, both of which were conducted in the Twin Cities Metropolitan Area of Minnesota. IDEA and ECHO were both 2-year longitudinal studies whose purpose was to understand the social and environmental influences on unhealthy weight gain during adolescence (Lytle 2009). Baseline data for the present study were collected in 2006–2007 (IDEA) and 2007–2008 (ECHO) and follow-up data collected in 2008–2009 (IDEA) and 2009–2010 (ECHO). For both studies, parent/adolescent pairs were excluded from participating in either study if they planned to move from the area in the next 3 years, had a medical condition that affected their growth (e.g., hypo/hyperthyroidism), were non-English speaking, and/or had any other physical or emotional condition that would affect their diet/activity levels or make it difficult to complete surveys or measurements.
IDEA participants were recruited from (1) an existing cohort of youth participating in the Minnesota Adolescent Community Cohort (MACC) Tobacco Study (Widome et al. 2007), (2) a Minnesota Department of Motor Vehicle (DMV) list restricted to the 7-county metro area, and (3) a convenience sample drawn from local communities. The MACC cohort was recruited from a random sample of 60 geographical and political units (GPU) (out of a total of 129) which were created to provide a sample of the local tobacco control environments in Minnesota. A total of 3,637 teens divided into five cohorts based on initial age (i.e., 12, 13, 14, 15, 16) with each cohort having approximately 725 youth were recruited and followed over time. Recruitment letters for the IDEA study were mailed to the MACC cohort and their age-eligible siblings beginning in August 2006 and continuing through March 2007. In total, 506 letters were sent to the MACC cohort/siblings. The DMV sample included youth ages 14–17 who applied for a learner's permit or driver's license through the State of Minnesota. After obtaining the DMV list, the MACC Study data programmer provided a list of the 49 zip codes in the seven-county Twin Cities Metro area. Based on the age criteria (and corresponding birth date ranges) in the 49 zip codes provided, the Data Collection and Support Services department in the Division of Epidemiology and Community Health at the University of Minnesota drew a random sample of 2,877 youth from the DMV list. Recruitment letters mailed to the DMV sample began in July 2006 and continued through October 2006. The convenience sample was recruited in several ways: (1) current participants were asked to tell friends, colleagues and family members with age-eligible children about the study and to pass on contact information to the TREC IDEA recruitment coordinator; (2) recruitment flyers were sent to the Minneapolis Park and Recreation Board and posted at several parks in the Minneapolis area; (3) a Boy Scout troop leader requested flyers at an event and passed them out to his troop; and (4) TREC IDEA staff members distributed fliers at a local high school's parent-teacher conferences and distributed an e-mail announcement to a group of parent volunteers from the local middle school.
As a result of these recruitment efforts, a total of 26% of the youth were recruited from the MACC cohort, 49% were recruited from the DMV sample, and 25% were recruited from the convenience sample. The recruitment rate was 18% and 6% for the MACC and DMV samples, respectively; however, a recruitment rate cannot be calculated for the convenience sample because the denominator is unknown. Participants in the IDEA study (n = 349) were adolescents ranging in age from 10.8 to 17.7, and were 50.7% female, 93.6% White, 1.5% African–American, 0.3% Asian and 4.6% other race/ethnicity. A total of 328 adolescents in the IDEA study completed both the baseline and 2 year follow-up surveys, a 94% response rate.
The ECHO study (n = 374) also included adolescents (ages 11.0–17.6) from the same catchment area as the IDEA study. However, in the ECHO study, participants were recruited from the membership of HealthPartners® (HP) health plan from within the seven-county metropolitan area of Minneapolis/St. Paul, Minnesota. The recruitment strategy was designed to recruit a racially-diverse sample of adolescents that represented both healthy weight and overweight individuals. To be eligible for enrollment, youth were required to be current HP members, in grades 6th through 11 in the fall of 2007, living in one of the randomly selected middle or high-school districts included in the sample, have a parent willing to participate and be willing to allow their names and contact information to be sent from HP to the study team at the University of Minnesota for further eligibility screening, consent and measurement. A total of 374 parent/adolescent dyads were recruited; 33% of parent/adolescent dyads had an overweight parent and normal weight adolescent, 9% had a normal-weight parent and an overweight adolescent, 32% had a parent- adolescent concordance for normal weight and 26% concordant for overweight. Of these dyads, 27% represented racial or ethnic minorities. Study participants in ECHO were 51.5% female, 79.4% White, 10.0% African–American, 1.7% Asian, 0.3% Native Hawaiian/Pacific Islander, 0.8% American Indian, and 7.8% other race/ethnicity. A total of 320 adolescents in the ECHO study completed both the baseline and 2 year follow-up surveys, resulting in an 85.6% response rate.
The measures collected in both the IDEA and ECHO studies were identical for all participants. Using identical measures was done for the purpose of combining data from the two studies in order to provide a larger, more racially and economically diverse sample. However, the ECHO study recruitment did focus on a representative sample for weight, therefore the two samples do differ significantly on body mass index z-score and baseline percentage body fat. Table 1 includes demographic data for each sample at baseline and two-year follow-up, as well as for the combined sample. The combined sample included 723 adolescents. Adolescent participants were 14.7 years of age on average at baseline, approximately 49% were male, 86.4% were White, 5.3% African–American, 1% Asian, 0.1% Native Hawaiian/Pacific Islander, 0.4% American Indian, 6.3% other race/ethnicity and 12% received free or reduced cost lunch. Approximately 5% of the sample indicated they were of Latino or Hispanic or Mexican–American or Spanish origin in a separate question similar to the question used in the US Census. The present study uses cohort data from baseline and the two-year follow-up. All study protocols were approved by the University of Minnesota Institutional Review Board.
Table 1. Descriptive data on body composition, substance use, and covariates, by sample and data collection wave (N = 704).
| Combined sample | IDEA sample | ECHO sample | ||||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| Baseline | Follow-up | Baseline | Follow-up | Baseline | Follow-up | |
| Body composition, M (SD) | ||||||
| BMI z-score | 0.40 (1.02) | 0.42 (1.00) | 0.28 (0.95)a | 0.30 (0.96)a | 0.52 (1.04)a | 0.53 (1.01)a |
| Percent body fat | 21.46 (10.48) | 22.17 (10.28) | 20.33 (10.02)a | 21.37 (9.68) | 22.47 (10.68)a | 22.84 (10.68) |
| Substance use (proportion) | ||||||
| Cigarette use | 5.1% | 15.0% | 7.0%b | 17.9%b | 3.3%b | 12.0%b |
| Alcohol use | 11.7% | 36.8% | 18.6%a | 44.8%a | 5.0%a | 29.3%a |
| Marijuana use | 3.1% | 13.1% | 4.1% | 16.0%a | 2.2% | 10.1%a |
| Covariates | ||||||
| Age, M (SD) | 14.68 (1.83) | 16.65 (1.85) | 15.40 (1.70)a | 17.38 (1.73)a | 13.99 (1.67)a | 15.91 (1.68)a |
| Female | 51.1% | 50.7% | 51.5% | |||
| White | 86.4% | 93.6%a | 79.4%a | |||
| Pubertal status, M (SD) | 2.90 (.73) | 3.04 (.67) | 2.77 (0.76) | |||
| Parent education, M (SD) | 4.96 (1.14) | 4.99 (1.12) | 4.92 (1.00) | |||
| Weight satisfaction, M (SD) | 3.41 (1.01) | 3.45 (1.02) | 3.38 (1.00) | |||
Comparison of studies differed significantly p < 0.001
Comparison of studies differed significantly p ≤ 0.05
Measures
Youth and one parent attended a visit at the Epidemiology Clinical Research Center at the University of Minnesota to complete self-reported surveys and to have their height and weight objectively measured by trained clinic staff. At the start of the visit, parents and youth were both given informed consent/assent forms to read and sign. Youth completed a self-report survey, in a separate room from their parents, which included questions on substance use as part of a larger survey to assess a broad range of adolescent health behaviors as well as the etiology of child/adolescent obesity. Each survey was identified only by the youth's identification number. Parents also completed a self-report survey, however, only a measure of parental education from this survey was used for the present study. Trained staff also measured each participant's height using a Shorr height board (Irwin Shorr, Olney, MD), and weight and percentage body fat using a Tanita scale, a bioelectrical impedance device that assesses body weight, lean and fat mass (TanitaTBF-300A Body Composition Analyzer, Arlington Heights, IL).
Body Mass Index Z-Score
The objectively measured height and weight values were transformed into body mass index for age z-scores (BMI z-score) using national reference data (Kuczmarksi et al. 2002). A BMI z-score represents body measurements in standard deviation units, or deviations from the mean. BMI z-score allows for the comparison across ages as well as the relative weight status of youth at the distribution extremes (Kuczmarksi et al. 2002).
Percentage Body Fat
Percentage body fat (percent body fat) was measured directly on the Tanita scale. The scale provided a print out of the percent body fat value for each youth.
Tobacco Use
Past month smoking was assessed with one question that asked how much the student currently smoked with 10 response options ranging from “I don't smoke” to “a pack or more each day.” This item has been used previously with youth (Johnston et al. 1998). To create a past month smoking item, the response options were recoded so that those who indicated any cigarette smoking in the past month were coded as “1” and all others were coded as “0.”
Alcohol Use
To assess alcohol use, students completed one question which asked how many times in the past month they had alcohol to drink, including beer, wine, and liquor, but not including sips, with response options ranging from 0 to 40 or more times (Johnston et al. 1998). The response options were recoded so that students who had used any alcohol in the past month were assigned a “1” and all other students were assigned a “0.”
Marijuana Use
To assess marijuana use, students were asked to report the number of times they used marijuana in the past month with response options ranging from 0 to 40 or more times (Johnston et al. 1998). The response options were recoded so that all students who indicated any marijuana use in the past month were assigned a “1” and all other students were assigned a “0.”
Socio-Economic Status
Socio-economic status was measured using a proxy of parent's highest level of education and was assessed on the parent survey. This one item question asked “Among all of the adults in your home, what is the highest level of education completed?” Response options included “Did not finish high school,” “Finished high school (or got a GED),” “Went to vocational school (computer/electrician/mechanic/healthcare/beauty school),” “Took some college (but did not graduate),” “Graduated from college or a university,” “Professional training beyond a four-year college degree.” Socio-economic status was used as a continuous covariate (values 1–6) due to previously documented associations with both substance use (Goodman and Huang 2002) and body composition (Murasko 2011).
Race/Ethnicity
Race/ethnicity was measured with one item asking “Do you think of yourself as…? (Check ALL that apply).” Response options included “White,” “Black or African– American,” “Asian,” “Native Hawaiian or other Pacific Islander,” “American Indian or Alaskan Native,” “Other,” and “I don't know.” Race was dichotomized into White/Non-White. Race was included as a covariate as there are racial/ethnic differences in both substance use (Shih et al. 2010) and body composition (Flegal et al. 2010; Freedman et al. 2008).
Pubertal Development
Pubertal development was measured with the 5-item self-report Pubertal Development Scale (Petersen et al. 1988) and was included as a continuous covariate due to previous associations with both substance use and body composition (Patton and Viner 2007).
Weight Satisfaction
Weight satisfaction was measured with one item, which asked the student how satisfied s/he was with her/his weight. Response options ranged from very dissatisfied to very satisfied and this variable was included as a continuous covariate (values of 1–5) as weight satisfaction has been associated with substance use (Page et al. 1995) and body composition (van den Berg et al. 2010).
Gender
Gender was assessed with one question where the youth indicated if s/he was male or female and was coded with female = 1 and male = 0. Gender differences have been found for both substance use (Eaton et al. 2010) and body composition (Ogden et al. 2010).
Age
Youth completed a question which asked them to indicate their birthdates including day, month, and year. Age at the time of survey completion was then calculated by subtracting the birthdate from the date of the survey and used as a continuous covariate due to differences in age for both substance use (Eaton et al. 2010) and body composition (Ogden et al. 2010).
Analysis
Data Analyses
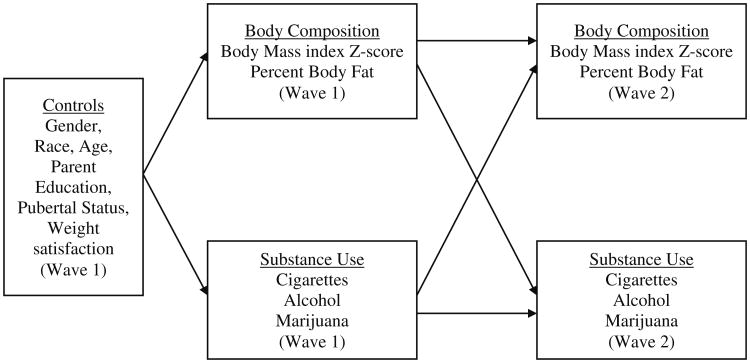
An autoregressive cross-lagged (ARCL) model was tested using MPlus 6.1 (Muthen and Muthen 1998–2010) to determine the bi-directional relationship between body composition and substance use (Bollen and Curran 2006). This type of structural equation model tests the significance of the cross-lagged paths (i.e., baseline substance use to follow-up body composition and baseline body composition to follow-up substance use) while controlling for across-time stability of the variables of interest as well as covariates. One model was fit, with both body composition variables (BMI z-score and percent body fat) and all three substance use variables (cigarettes, alcohol, and marijuana). Cross-lagged paths were tested by estimating six paths from each Wave 1 body composition variable to the three Wave 2 substance use variables (cigarettes, alcohol, and marijuana) and by estimating six paths from the three Wave 1 substance use variables to each of the Wave 2 body composition variables. Cross-stability paths were tested by estimating five paths from the two Wave 1 body composition and three substance use variables to the equivalent Wave 2 variables. The interpretation of the cross-lagged paths is thus the influence of the baseline measure “above and beyond the influence” of the cross-stability path (Bollen and Curran 2006). The covariates of interest were controlled for by adding paths to the Wave 1 body composition and substance use measures. The two body composition variables were allowed to co-vary at each wave and the three substance use measures were allowed to co-vary at each wave (Fig. 1).
Fig. 1. Conceptual model of the cross-lagged relations between body composition and substance use.
MPlus is able to include both dichotomous (substance use) and continuous (body composition) variables as outcomes, but to accommodate for the dichotomous outcomes the weighted least-squares with mean and variance adjustment (WLSMV) estimator was used, an estimator shown to be more optimal for categorical outcomes (Muthen et al. 1997). Participants missing information on the exogenous covariates were excluded from analyses (N = 19), resulting in a final sample size of 704. Several criteria were used to assess the fit of the two models: the X2 statistic; the Tucker-Lewis Index (TLI) and the Comparative Fit Index (CFI), both of which are recommended to be .95 or higher; and the Root Mean Squared Error of Approximation (RMSEA), which is recommended to be .06 or lower (Hu and Bentler 1999).
Results
At baseline, the average BMI z-score was 0.40, which increased slightly by the time of follow-up 2 years later to 0.42 (see Table 1). Percent body fat also increased slightly from baseline to follow-up from 21.46% to 22.17%. Based on BMIs, approximately 24% of the participants would be considered overweight or obese at baseline and 25% overweight or obese at follow-up. At baseline, all substance use behaviors in the past month had a relatively low prevalence (5.1% cigarette use, 11.7% alcohol use, and 3.1% marijuana use). At the time of follow-up 2 years later, however, past month cigarette use increased to 15%, alcohol use increased to 36.8% and marijuana use increased to 13.1%.
Correlations Between Study Variables
The correlations between body composition, substance use, and the covariates are presented in Table 2. BMI z-score and percent body fat were highly correlated at both Waves 1 and 2. BMI z-score at Wave 1 was positively associated with cigarette use at Wave 2, but all other associations between body composition and substance use were non-significant.
Table 2. Correlations among study variables (N = 704).
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | |
|---|---|---|---|---|---|---|---|---|---|
| 1. Body mass index z-score Wave 1 | – | ||||||||
| 2. Percent body fat Wave 1 | .70*** | – | |||||||
| 3. Cigarette use Wave 1 | .09 | .06 | – | ||||||
| 4. Alcohol use Wave 1 | −.02 | .02 | .61*** | – | |||||
| 5. Marijuana use Wave 1 | −.003 | −.003 | .77*** | .65*** | – | ||||
| 6. Body mass index z-score Wave 2 | .91*** | .61*** | .05 | −.09 | .04 | – | |||
| 7. Percent body fat Wave 2 | .67*** | .90*** | .05 | −.02 | .01 | .67*** | – | ||
| 8. Cigarette use Wave 2 | .14* | .04 | .80*** | .62*** | .67*** | .08 | .001 | – | |
| 9. Alcohol use Wave 2 | .07 | .03 | .60*** | .66*** | .63*** | −.01 | −.04 | .68*** | – |
| 10. Marijuana use Wave 2 | .11 | –.05 | .68*** | .62*** | .79*** | .08 | −.06 | .82*** | .73*** |
| 11. Gender (female) | −.05 | .57*** | −.12 | −.05 | −.22 | −.09 | .63*** | −.20** | −.02 |
| 12. Race (non-White) | .29*** | .30*** | −.13 | −.08 | .000 | .19*** | .25*** | −.07 | .10 |
| 13. Age | −.02 | −.001 | .46*** | .62*** | .49*** | −.06 | .004 | .42*** | .50*** |
| 14. Weight satisfaction | −.48*** | −.57*** | −.09 | −.08 | −.10 | −.45*** | −.48*** | −.14* | −.11* |
| 15. Pubertal status | .16*** | .33*** | .33** | .42*** | .25 | .11** | .36*** | .32*** | .38*** |
| 16. Parent education | −.13*** | −.17*** | −.06 | −.03 | −.05 | −.07 | −.14*** | .001 | −.11* |
|
| |||||||||
| 10 | 11 | 12 | 13 | 14 | 15 | 16 | |||
|
| |||||||||
| 1. Body mass index z-score Wave 1 | |||||||||
| 2. Percent body fat Wave 1 | |||||||||
| 3. Cigarette use Wave 1 | |||||||||
| 4. Alcohol use Wave 1 | |||||||||
| 5. Marijuana use Wave 1 | |||||||||
| 6. Body mass index z-score Wave 2 | |||||||||
| 7. Percent body fat Wave 2 | |||||||||
| 8. Cigarette use Wave 2 | |||||||||
| 9. Alcohol use Wave 2 | |||||||||
| 10. Marijuana use Wave 2 | – | ||||||||
| 11. Gender (female) | −.35*** | – | |||||||
| 12. Race (non-White) | −.02 | .08 | – | ||||||
| 13. Age | .40*** | −.003 | −.08 | – | |||||
| 14. Weight satisfaction | −.17** | −.16*** | −.14* | −.08* | – | ||||
| 15. Pubertal status | .20** | .51*** | .07 | .65*** | −.17*** | – | |||
| 16. Parent education | −.01 | −.08 | −.27*** | .02 | .17*** | −.03 | – | ||
p < .05,
p < .01,
p < .001
Auto-Regressive Cross-Lagged Model Results
The fit of the ARCL model was excellent [X2 = 66.12 (50, p = .06), CFI = .99, TLI = .99, RMSEA = .02 (CI = .000, .034)]. All of the stability paths (or the paths between the baseline and follow-up levels of the same variable) were significant and positive (Table 3). All of the substance use variables were significantly positively associated with each other at both Waves 1 and 2 and the two body composition variables were significantly positively associated at both waves (covariance paths). Controlling for all other variables in the model, age, gender, race, pubertal status, and weight satisfaction were all significantly correlated with body composition. Age was negatively associated with BMI z-score and percent body fat and females had lower BMI z-scores but higher percent body fat than males, White adolescents had lower BMI z-scores and percent body fat than non-White adolescents, BMI z-scores and percent body fat increased with increasing pubertal status, and as BMI z-scores and percent body fat increased, weight satisfaction decreased. Parental education was not related to BMI z-scores, but was negatively associated with percent body fat, such that adolescents whose parents had a higher education level had a lower percent body fat. Age was positively associated with all three substance use variables, and gender was significantly associated with cigarette and marijuana use, such that females were less likely to be using than males. Pubertal status was significantly positively associated with cigarette use, while weight satisfaction was significantly negatively associated with cigarette and marijuana use. Furthermore, parent education was significantly negatively associated with alcohol use.
Table 3. Standardized path coefficients (N = 704).
| Path coefficient | p-value | |
|---|---|---|
| Stability paths (Wave 1 → Wave 2) | ||
| Body mass index z-score | .91 | <.001 |
| Percent body fat | .92 | <.001 |
| Cigarette use | .83 | <.001 |
| Alcohol use | .73 | <.001 |
| Marijuana use | .88 | <.001 |
| Covariance paths | ||
| Body mass index z-score Wave 1 ↔ percent body fat Wave 1 | .78 | <.001 |
| Cigarette use Wave 1 ↔ alcohol use Wave 1 | .63 | <.001 |
| Cigarette use Wave 1 ↔ marijuana use Wave 1 | .75 | <.001 |
| Alcohol use Wave 1 ↔marijuana use Wave 1 | .64 | <.001 |
| Body mass index z-score Wave 2 ↔ percent body fat Wave 2 | .90 | <.001 |
| Cigarette use Wave 2 ↔ alcohol use Wave 2 | .60 | <.001 |
| Cigarette use Wave 2 ↔ marijuana use Wave 2 | .85 | <.001 |
| Alcohol use Wave 2 ↔marijuana use Wave 2 | .86 | <.001 |
| Control paths (Wave 1 → Wave 1) | ||
| Female gender → body mass index z-score | −.29 | <.001 |
| Non-White race → body mass index z-score | .11 | <.001 |
| Age → body mass index z-score | −.31 | <.001 |
| Weight satisfaction → body mass index z-score | −.47 | <.001 |
| Pubertal status → body mass index z-score | .40 | <.001 |
| Parent education → body mass index z-score | −.02 | .46 |
| Female gender → percent body fat | .36 | <.001 |
| Non-White race → percent body fat | .13 | <.001 |
| Age → percent body fat | −.17 | <.001 |
| Weight satisfaction → percent body fat | −.43 | <.001 |
| Pubertal status → percent body fat | .23 | <.001 |
| Parent education → percent body fat | −.05 | .04 |
| Female gender → cigarette use | −.20 | .03 |
| Non-White race → cigarette use | −.07 | .26 |
| Age → cigarette use | .29 | .002 |
| Weight satisfaction → cigarette use | −.12 | .04 |
| Pubertal status → cigarette use | .34 | .005 |
| Parent education → cigarette use | −.06 | .41 |
| Female gender → alcohol use | −.11 | .10 |
| Non-White race → alcohol use | .04 | .34 |
| Age → alcohol use | .58 | <.001 |
| Weight satisfaction → alcohol use | −.03 | .42 |
| Pubertal status → alcohol use | .12 | .12 |
| Parent education → alcohol use | −.08 | .05 |
| Female gender → marijuana use | −.36 | <.001 |
| Non-White race → marijuana use | −.004 | .95 |
| Age → marijuana use | .34 | <.001 |
| Weight satisfaction → marijuana use | −.18 | .006 |
| Pubertal status → marijuana use | .18 | .11 |
| Parent education → marijuana use | −.02 | .66 |
| Cross-lagged paths (Wave 1 → Wave 2) | ||
| Body mass index z-score → cigarette use | .15 | .17 |
| Body mass index z-score → alcohol use | .02 | .75 |
| Body mass index z-score → marijuana use | .03 | .69 |
| Cigarette use → body mass index z-score | .08 | .42 |
| Alcohol use → body mass index z-score | −.18 | .02 |
| Marijuana use → body mass index z-score | .04 | .66 |
| Percent body fat → cigarette use | −.15 | .20 |
| Percent body fat → alcohol use | .01 | .88 |
| Percent body fat → marijuana use | −.04 | .72 |
| Cigarette use → percent body fat | .24 | .01 |
| Alcohol use → percent body fat | −.14 | .07 |
| Marijuana use → percent body fat | −.11 | .16 |
None of the cross-lagged paths from Wave 1 body composition (BMI z-score or percent body fat) to substance use were significant. Only one path from Wave 1 substance use to Wave 2 BMI z-score was significant; adolescents who used alcohol at Wave 1 had a lower BMI z-score at Wave 2 compared with adolescents who did not use alcohol at Wave 1, controlling for all other paths (β = −.18, p = .02). One path from Wave 1 substance use to Wave 2 percent body fat was significant; adolescents who smoked cigarettes at Wave 1 had a higher percent body fat at Wave 2 compared with adolescents who did not smoke cigarettes (β = .24, p = .01). Also, the path between Wave 1 alcohol use and Wave 2 percent body fat approached significance, in the same direction as BMI z-score (β = −.14, p = .07).
Discussion
Adolescence is a time of change and exploration as well as a time when youth begin to develop autonomy and make their own decisions. As such, there are many challenges adolescents face when trying to make healthy decisions. Engagement in substance use and risk of obesity are two such challenges. As substance use and obesity are prevalent in the lives of many adolescents, it is important to understand how they may be related, however, limited research has explored their inter-relatedness. To our knowledge, this study is the first study to explore the longitudinal, bi-directional relationships between objectively measured body composition, including BMI z-score and percent body fat, and youth substance use, controlling for the co-variation between substance use behaviors. Several proposed mechanisms for the association between substance use and obesity were advanced: the coping model, weight control model, weight gain model, and the risk profile model. Findings suggest that the weight gain model fit best for cigarette use, as current cigarette use at baseline predicted subsequent increases in percent body fat. In contrast to our hypotheses and the proposed mechanisms, alcohol use predicted decreases in BMI z-score and a similar relationship approached significance for percent body fat. While not completely in-line with our suggested hypotheses, findings from this study begin to elucidate the substance use/obesity relationship.
Similar to previous longitudinal research (Pasch et al. 2008), measures of body composition did not predict engagement in substance use 2 years later. These non-significant findings suggest that overweight or obese youth are not more likely to engage in subsequent substance use. However, this study found that cigarette smoking at baseline significantly predicted increased percent body fat, but not an increase in BMI 2 years later. The relationship between smoking and percent body fat was significant after controlling for several covariates related to substance use and body composition, as well as other substance use behaviors including alcohol and marijuana use. The present study suggests that, contrary to the weight control model which proposes that overweight youth are likely to use cigarettes as a weight control strategy, smoking may actually lead to increased body fat over time. The potential biological mechanisms behind this relationship are not clear; however, it is hypothesized that smoking negatively impacts levels of physical activity which increases adiposity relative to muscle mass. While the present study did not find associations between BMI z-score and cigarette use, previous research has documented this association specifically among girls (Caria et al. 2009; Farhat et al. 2010; O'Loughlin et al. 1998). This inconsistency may be due to the fact that in the present study BMI was treated as a continuous variable while previous research has tended to look at the associations among those who were overweight or obese. Additionally, previous research has used self-reported height and weight to create BMI values, while the present study used objectively measured height and weight, these differences in data collection may have impacted study findings. It is also possible that the low prevalence of smoking coupled with the relatively low prevalence of youth with higher BMI z-scores could have reduced the power to detect this difference. Finally, because of the low prevalence of substance use at baseline, we were unable to explore gender differences in the model which may also account for the differences in findings.
In contrast to previous cross-sectional research documenting the association between substance use and overweight/obesity (Farhat et al. 2010; Fonseca et al. 2009) and contrary to our proposed weight gain model, the present study found a significant negative association between alcohol use and subsequent BMI z-score suggesting that alcohol use at baseline was related to a decreased BMI z-score 2 years later. In addition, a similar relationship between alcohol use and subsequent percent body fat approached significance. While not in line with our proposed mechanisms, there are potential explanations for these findings. Unlike previous research examining the relationship between body composition and each substance individually, the current study looked at the relationship between each substance and body composition while controlling for other substance use. The covariance paths between the three substances ranged from .60 to .86 in this study, indicating that adolescents who used one substance had a strong likelihood of using other substances. By controlling for the use of other substances, this study was able to isolate the effects of each individual substance on body composition. Additionally, it is plausible that youth who use substances in adolescence adopt less healthful eating patterns that result in a restriction of their caloric intake, leading to a lower BMI z-score and percent body fat later in adolescence. Future research that controls for caloric intake to see if patterns hold is warranted. In addition, it is possible that youth who use substances in adolescence are at later risk for underweight. Future research examining obesity risk as a categorical variable (underweight, healthy weight, overweight) rather than a continuous variable, as done in the present study, may shed some light on these findings.
It is also possible that youth who engage in substance use may be doing so as one way to fit in with their peers, as these youth may be particularly sensitive to social pressures. Research has shown that popularity is positively associated with substance use (Killeya-Jones et al. 2007; Lahmann et al. 2002). Additionally, youth who are concerned about social image and popularity are likely to want to avoid having a higher BMI as increased BMI has been associated with decreased popularity and social marginalization (Strauss and Pollack 2003) and increased teasing (Neumark-Sztainer et al. 2002; Pearce et al. 2002). As such, these youth may also engage in more weight restrictive behaviors (Gold et al. 1996) leading to declines in BMI z-score. Thus, while weight satisfaction was included as a covariate in the present study, future research should explore how unhealthy weight control behaviors may moderate or mediate the substance use-body composition relationship. Another variable to consider in future research is physical activity, as levels of physical activity may be associated with both substance use and body composition as physical activity levels lead to a healthier body composition and possibly lower levels of substance use.
This study has several limitations. It was conducted with primarily White, middle class, adolescents, which limits the generalizability of the findings. Further longitudinal work is needed to continue to explore measures of overweight and obesity in more diverse samples. Additionally, while this research explored longitudinal associations between substance use and body composition, it did not attempt to identify risk behavior clusters or risk profiles that might be used to help tailor more specific, and possibly more effective, interventions to sub-groups of youth. Future research which uses techniques such as latent class analysis or other cluster analysis methods would help to determine how these behaviors cluster among youth. Additionally, due to the low prevalence of substance use in this population we were unable to test for the potential moderating effects of age or gender. This low prevalence of substance use, particularly at baseline, may also have reduced our ability to detect associations. Future research should recruit larger samples of younger youth to increase the variability in substance use at early ages to test for possible gender or age differences in these relationships. Finally, the differing recruitment methods for the two combined studies may have impacted study findings.
While this study does have limitations, there are also several strengths. In this study, we were able to look at the bi-directional longitudinal relationships between body composition and substance use and control for baseline values and associations between variables, which allows us to examine the relationship between body composition and substance use by removing some of the “noise” that is inherent when independent models of substance use behaviors are used. In addition, we were able to control for a number of covariates that have been shown to be associated with body composition and/or substance use as well as the influence of weight satisfaction as a potential motivator for behavioral choices. Overall, this study is one of the first to document the longitudinal bi-directional relationships between youth substance use and body composition.
Adolescence is a time of dramatic changes across all domains of life. In previous cross-sectional work, overweight/obesity has been shown to be significantly associated with youth substance use, including alcohol, tobacco, and marijuana use (Farhat et al. 2010; Fonseca et al. 2009; Koval et al. 2008; Pasch et al. 2008). While these cross-sectional studies are very important to the establishment of a body of research in the area of the co-occurrence of youth substance use and weight status, these studies do not provide insight into the directionality of these associations. Longitudinal studies, like the present study, allow for further exploration into the possible causal pathways that may be involved. We do not believe that our findings suggest that alcohol use is protective against unhealthy weight gain later in adolescence. Rather, we believe that results suggest a relationship between substance use and obesity that is mediated through energy balance, clustering of risk behaviors and/or social influence. As these two factors, substance use and obesity, contribute to much of the public health burden in the US and other nations, it is important that we continue to explore the potential interactive relationship between body composition and substance use behaviors among youth to elucidate the directionality of the associations as well as identify potential intervention points to reduce both substance use and obesity among youth.
Acknowledgments
This research was funded through a grant from the National Cancer Institute as part of their Transdisciplinary Research in Energetics and Cancer (TREC) Initiative. Grant # 1U54CA116849 and through a grant supported by the Etiology of Childhood Obesity (ECHO) with funding from the National Heart, Lung and Blood Institute, Grant #R01HL085978. The content of this manuscript is solely the responsibility of the authors and does not necessarily represent the official views of the National Cancer Institute, National Heart, Lung and Blood Institute, or the National Institutes of Health.
Biographies
Keryn E. Pasch is an Assistant Professor in the Department of Kinesiology and Health Education in the College of Education at the University of Texas, Austin. Her research interests include the co-occurrence of risk behaviors in adolescence and early adulthood and the influence of media on adolescent health behavior.
Cayley E. Velazquez is a Doctoral Candidate in Health Education in the Department of Kinesiology and Health Education in the College of Education at the University of Texas at Austin. Her research interests include child and adolescent health, nutrition, obesity, and media influences.
Jessica Duncan Cance is an Assistant Professor in the Department of Kinesiology and Health Education in the College of Education at the University of Texas at Austin. Her research interests are in the prevention and etiology of adolescent health risk behaviors. She is specifically interested in how longitudinal interactions of biological, psychological, and social factors impact substance use.
Stacey G. Moe is a Project Coordinator in the Division of Epidemiology and Community Health in the School of Public Health at the University of Minnesota. Her research interests include school-and community-based programs to study primary prevention of childhood obesity and youth health promotion.
Leslie A. Lytle is a Professor in the Division of Epidemiology and Community Health in the School of Public Health at the University of Minnesota. Her research interests include youth health promotion and the prevention of childhood obesity using an ecological framework.
Contributor Information
Keryn E. Pasch, Email: kpasch@mail.utexas.edu, Department of Kinesiology and Health Education, University of Texas, 1 University Station, D3700, Austin, TX 78712, USA.
Cayley E. Velazquez, Department of Kinesiology and Health Education, University of Texas, 1 University Station, D3700, Austin, TX 78712, USA
Jessica Duncan Cance, Department of Kinesiology and Health Education, University of Texas, 1 University Station, D3700, Austin, TX 78712, USA.
Stacey G. Moe, Division of Epidemiology and Community Health, School of Public Health, University of Minnesota, Minneapolis, MN 55454, USA
Leslie A. Lytle, Division of Epidemiology and Community Health, School of Public Health, University of Minnesota, Minneapolis, MN 55454, USA
References
- Bollen KA, Curran PJ. Latent curve models: A structural equation perspective. Hoboken, NJ: Wiley-Interscience; 2006. [Google Scholar]
- Caria MP, Bellocco R, Zambon A, Horton NJ, Galanti MR. Overweight and perception of overweight as predictors of smokeless tobacco use and of cigarette smoking in a cohort of Swedish adolescents. Addiction. 2009;104(4):661–668. doi: 10.1111/j.1360-0443.2009.02506.x. [DOI] [PubMed] [Google Scholar]
- United States Department of Agriculture. Report of the dietary guidelines advisory committee on the dietary guidelines for Americans. Washington, DC: U.S. Department of Agriculture, Agricultural Research Service; 2010. [Google Scholar]
- Donovan JE, Jessor R, Costa FM. Syndrome of problem behavior in adolescence: A replication. Journal of Consulting and Clinical Psychology. 1988;56(5):762–765. doi: 10.1037//0022-006x.56.5.762. [DOI] [PubMed] [Google Scholar]
- Eaton DK, Kann L, Kinchen S, Shanklin S, Ross J, Hawkins J, et al. Youth risk behavior surveillance—United States, 2009. MMWR Surveillance Summaries: Morbidity and Mortality Weekly Report Surveillance Summaries/CDC. 2010;59(5):1–142. [PubMed] [Google Scholar]
- Farhat T, Iannotti RJ, Simons-Morton BG. Overweight, obesity, youth, and health-risk behaviors. American Journal of Preventive Medicine. 2010;38(3):258–267. doi: 10.1016/j.amepre.2009.10.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flegal KM, Ogden CL, Yanovski JA, Freedman DS, Shepherd JA, Graubard BI, et al. High adiposity and high body mass index-for-age in US children and adolescents overall and by race-ethnic group. The American Journal of Clinical Nutrition. 2010;91(4):1020–1026. doi: 10.3945/ajcn.2009.28589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fonseca H, Matos MG, Guerra A, Pedro JG. Are overweight and obese adolescents different from their peers? International Journal of Pediatric Obesity. 2009;4(3):166–174. doi: 10.1080/17477160802464495. [DOI] [PubMed] [Google Scholar]
- Freedman DS, Wang J, Thornton JC, Mei Z, Pierson RN, Jr, Dietz WH, et al. Racial/ethnic differences in body fatness among children and adolescents. Obesity. 2008;16(5):1105–1111. doi: 10.1038/oby.2008.30. [DOI] [PubMed] [Google Scholar]
- Gold DR, Wang X, Wypij D, Speizer FE, Ware JH, Dockery DW. Effects of cigarette smoking on lung function in adolescent boys and girls. The New England Journal of Medicine. 1996;335(13):931–937. doi: 10.1056/NEJM199609263351304. [DOI] [PubMed] [Google Scholar]
- Goodman E, Hinden BR, Khandelwal S. Accuracy of teen and parental reports of obesity and body mass index. Pediatrics. 2000;106:52–58. doi: 10.1542/peds.106.1.52. [DOI] [PubMed] [Google Scholar]
- Goodman E, Huang B. Socioeconomic status, depressive symptoms, and adolescent substance use. Archives of Pediatric & Adolescent Medicine. 2002;156(5):448–453. doi: 10.1001/archpedi.156.5.448. [DOI] [PubMed] [Google Scholar]
- Hall W, Degenhardt L. Adverse health effects of non-medical cannabis use. Lancet. 2009;374(9698):1383–1391. doi: 10.1016/S0140-6736(09)61037-0. [DOI] [PubMed] [Google Scholar]
- Harakeh Z, Engels RC, Monshouwer K, Hanssen PF. Adolescent's weight concerns and the onset of smoking. Substance Use and Misuse. 2010;45(12):1847–1860. doi: 10.3109/10826081003682149. [DOI] [PubMed] [Google Scholar]
- Hu LT, Bentler PM. Cutoff criteria for fit indices in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6:1–55. [Google Scholar]
- Jessor R, Jessor SL. Problem behavior and psychosocial development: A longitudinal study of youth. New York: Academic Press; 1977. [Google Scholar]
- Johnston LD, O'Malley PM, Bachman JG. National survey results on drug use from the monitoring the future study, 1975-1997 1998 [Google Scholar]
- Johnston LD, O'Malley PM, Bachman JG, Schulenberg JE. Monitoring the future national survey results on drug use, 1975–2010: Volume I, Secondary school students. Ann Arbor: Institute of Social Research, The University of Michigan; 2011. [Google Scholar]
- Killeya-Jones LA, Nakajima R, Costanzo PR. Peer standing and substance use in early-adolescent grade-level networks: A short-term longitudinal study. Prevention Science. 2007;8(1):11–23. doi: 10.1007/s11121-006-0053-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirkham TC. Endocannabinoids in the regulation of appetite and body weight. Behavioural Pharmacology. 2005;16(5–6):297–313. doi: 10.1097/00008877-200509000-00004. [DOI] [PubMed] [Google Scholar]
- Kirkham TC, Williams CM. Endogenous cannabinoids and appetite. Nutrition Research Reviews. 2001;14(1):65–86. doi: 10.1079/NRR200118. [DOI] [PubMed] [Google Scholar]
- Koval JJ, Pederson LL, Zhang X, Mowery P, McKenna M. Can young adult smoking status be predicted from concern about body weight and self-reported BMI among adolescents? Results from a ten-year cohort study. Nicotine Tobacco Research. 2008;10(9):1449–1455. doi: 10.1080/14622200802239140. [DOI] [PubMed] [Google Scholar]
- Kuczmarski RJ, Ogden CL, Guo SS, et al. 2000 CDC growth charts for the United States: Methods and development. National Center for Health Statistics. Vital Health Statistics. 2002;11(246):1–203. [PubMed] [Google Scholar]
- Lahmann PH, Lissner L, Gullberg B, Berglund G. A prospective study of adiposity and all-cause mortality: The Malmo diet and cancer study. Obesity Research. 2002;10(5):361–369. doi: 10.1038/oby.2002.50. [DOI] [PubMed] [Google Scholar]
- Laska MN, Pasch KE, Lust K, Story M, Ehlinger E. Latent class analysis of lifestyle characteristics and health risk behaviors among college youth. Prevention Science. 2009;10(4):376–386. doi: 10.1007/s11121-009-0140-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lytle LA. Examining the etiology of childhood obesity: The IDEA study. American Journal of Community Psychology. 2009;44(3–4):338–349. doi: 10.1007/s10464-009-9269-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lytle LA, Kelder SH, Perry CL, Klepp KI. Covariance of adolescent health behaviors: The Class of 1989 study. Health Education Research. 1995;10(2):133–146. doi: 10.1093/her/10.2.119-a. [DOI] [PubMed] [Google Scholar]
- Murasko JE. Trends in the associations between family income, height and body mass index in US children and adolescents: 1971–1980 and 1999–2008. Annals of Human Biology. 2011;38(3):290–306. doi: 10.3109/03014460.2010.537698. [DOI] [PubMed] [Google Scholar]
- Muthen BO, Du Toit SHC, Spisic D. Robust inference using weighted least squares and quadratic estimating equations in latent variable modeling with categorical and continuous outcomes 1997 [Google Scholar]
- Muthen LK, Muthen BO. Mplus user's guide. 6th. Los Angeles, CA: Muthen & Muthen; 1998–2010. [Google Scholar]
- Neumark-Sztainer D, Falkner N, Story M, Perry C, Hannan PJ, Mulert S. Weight-teasing among adolescents: Correlations with weight status and disordered eating behaviors. International Journal of Obesity Related Metabolic Disorders. 2002;26(1):123–131. doi: 10.1038/sj.ijo.0801853. [DOI] [PubMed] [Google Scholar]
- Ogden CL, Carroll MD, Curtin LR, Lamb MM, Flegal KM. Prevalence of high body mass index in US children and adolescents, 2007–2008. Journal of the American Medical Association. 2010;303(3):242–249. doi: 10.1001/jama.2009.2012. [DOI] [PubMed] [Google Scholar]
- O'Loughlin J, Paradis G, Renaud L, Sanchez Gomez L. One-year predictors of smoking initiation and of continued smoking among elementary schoolchildren in multiethnic, low-income, inner-city neighbourhoods. Tobacco Control. 1998;7(3):268–275. doi: 10.1136/tc.7.3.268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Page RM, Scanlan A, Allen O. Adolescent perceptions of body weight and attractiveness: Important issues in alcohol and illicit drug use? Journal of Child and Adolescent Substance Abuse. 1995;4(4):43–55. [Google Scholar]
- Pasch KE, Nelson MC, Lytle LA, Moe SG, Perry CL. Adoption of risk-related factors through early adolescence: Associations with weight status and implications for causal mechanisms. Journal of Adolescent Health. 2008;43(4):387–393. doi: 10.1016/j.jadohealth.2008.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patton GC, Viner R. Pubertal transitions in health. Lancet. 2007;369(9567):1130–1139. doi: 10.1016/S0140-6736(07)60366-3. [DOI] [PubMed] [Google Scholar]
- Pearce MJ, Boergers J, Prinstein MJ. Adolescent obesity, overt and relational peer victimization, and romantic relationships. Obesity Research. 2002;10(5):386–393. doi: 10.1038/oby.2002.53. [DOI] [PubMed] [Google Scholar]
- Petersen AC, Crockett LJ, Richards M, Boxer A. A self-report measure of pubertal status: Reliability, validity and initial norms. Journal of Youth and Adolescence. 1988;17(2):117. doi: 10.1007/BF01537962. [DOI] [PubMed] [Google Scholar]
- Sherry B, Jefferds ME, Grummer-Strawn LM. Accuracy of adolescent self-report of height and weight in assessing overweight status: A literature review. Archives of Pediatric & Adolescent Medicine. 2007;161(12):1154–1161. doi: 10.1001/archpedi.161.12.1154. [DOI] [PubMed] [Google Scholar]
- Shih RA, Miles JN, Tucker JS, Zhou AJ, D'Amico EJ. Racial/ethnic differences in adolescent substance use: Mediation by individual, family, and school factors. Journal of Studies on Alcohol and Drugs. 2010;71(5):640–651. doi: 10.15288/jsad.2010.71.640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strauss RS, Pollack HA. Social marginalization of overweight children. Archives of Pediatrics and Adolescent Medicine. 2003;157(8):746–752. doi: 10.1001/archpedi.157.8.746. [DOI] [PubMed] [Google Scholar]
- United States Department of Health and Human Services. Reducing tobacco use: A report of the surgeon general. Georgia: Atlanta; 2000. [Google Scholar]
- van den Berg PA, Mond J, Eisenberg M, Ackard D, Neumark-Sztainer D. The link between body dissatisfaction and self-esteem in adolescents: Similarities across gender, age, weight status, race/ethnicity, and socioeconomic status. Journal of Adolescent Health. 2010;47(3):290–296. doi: 10.1016/j.jadohealth.2010.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Widome R, Forster JL, Hannan PJ, Perry CL. Longitudinal patterns of youth access to cigarettes and smoking progression: Minnesota Adolescent Community Cohort (MACC) study (2000–2003) Preventive Medicine. 2007;45(6):442–446. doi: 10.1016/j.ypmed.2007.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]