Abstract
The objective of this non-systematic review of the literature is to highlight some of the neural systems and pathways that are affected by the various intake-promoting aspects of the modern food environment and explore potential modes of interaction between core systems such as hypothalamus and brainstem primarily receptive to internal signals of fuel availability and forebrain areas such as the cortex, amygdala and meso-corticolimbic dopamine system, primarily processing external signals. The modern lifestyle with its drastic changes in the way we eat and move puts pressure on the homoeostatic system responsible for the regulation of body weight, which has led to an increase in overweight and obesity. The power of food cues targeting susceptible emotions and cognitive brain functions, particularly of children and adolescents, is increasingly exploited by modern neuromarketing tools. Increased intake of energy-dense foods high in fat and sugar is not only adding more energy, but may also corrupt neural functions of brain systems involved in nutrient sensing as well as in hedonic, motivational and cognitive processing. It is concluded that only long-term prospective studies in human subjects and animal models with the capacity to demonstrate sustained over-eating and development of obesity are necessary to identify the critical environmental factors as well as the underlying neural systems involved. Insights from these studies and from modern neuromarketing research should be increasingly used to promote consumption of healthy foods.
Keywords: Obesity, Food cues, Neuromarketing, Conditioned appetite, High-fat diet
Given the enormous amount of food eaten, it is remarkable that for most of us, body weight remains stable throughout adulthood. This weight stability is ascribed to a homoeostatic regulatory system in the hypothalamus that senses the nutritional and metabolic state of the body and controls energy intake and expenditure. Yet, an increasing portion of the population, including many children and adolescents develop obesity and the predisposition to a host of other debilitating diseases. The conundrum of high rates of obesity in the face of homoeostatic energy balance regulation has led to an intense scientific debate and at least three different views have emerged. The first is that in order for body weight (used here interchangeably with adiposity) to digress from the norm, there must be something wrong with the homoeostatic regulator located in the hypothalamus(1). Another characteristic often associated with this view is a rigidly defended body weight ‘set point’. This view is supported by the fact that if there is something wrong with the homoeostatic regulator, e.g. impaired leptin and/or melanocortin-signalling, obesity is inevitable(2). However, only a very small percentage of obesity can be allocated to defects in the presently known machinery of the homoeostatic regulator(3). The overwhelming majority of obese people do not seem to have faulty genes presently associated with obesity.
A second view is that the homoeostatic regulator acts mainly to defend against undersupply but not oversupply of nutrients, that it is organised with considerable flexibility to accommodate different internal and external contingencies such as pregnancy and seasonal variations, and that there is no rigidly defended body weight ‘set point’(4–7). The implication would be that digressions from ideal body weight need not always be pathological, but can be physiological adaptations to special circumstances.
A third view is to include, besides the hypothalamus, other brain areas such as the brainstem, basal ganglia and cortico-limbic systems in the greater circuitry of the homoeostatic regulator(8–12). This view is supported by observations of lasting effects on food intake and energy balance by manipulating such extra-hypothalamic areas. It would also be much better to explain how obesity can develop in a rapidly changing environment that primarily interacts with the cognitive and emotional brain.
In the following non-systematic review, I will discuss how this greater neural circuitry, considered by the third view stated earlier, could be involved in managing the sometimes competing influences of intero- and extero-sensory signals in the control of food intake, energy expenditure and body weight regulation.
The modern environment: temptations to eat and avoid physical activity
The way we live, particularly what, when and how we eat and work has drastically changed with the gradual transformation from an agriculture based to a consumer society over the last 50 years or so. Foods are readily available to a large segment of the population, while the opportunity to work physically and expend energy has decreased. With the ascent of electronic communication, the brain plays a much more prominent role in the procurement and consumption of food and in the management of daily activities. There is a daily onslaught with cues associated with food and pictures of food(13,14). The advertisement and food industry relies more and more on expertise from neuroscientists and psychologists, and neuromarketing is the new buzzword. Neuromarketing in children is particularly profitable, as it generates loyal future buyers of brand name products. An unfiltered PubMed search using the terms ‘food marketing’ and ‘children’ yielded 756 papers, 600 of them published after the year 2000. Considering the many hours of daily exposure to media and electronic devices by children and adolescents(15–17) and the persuasive techniques used(18–21), the term being ‘brain-washed’ is not inaccurate. Of course, the same powerful methods could be used to induce children to consume healthy foods(22,23), but this possibility remains little explored. Although cutting edge technology is applied by the food industry to find neurological markers for food-liking and wanting, much of this insight is unfortunately not shared with the research community.
Conditioned food intake in the absence of metabolic need
As we are increasingly exposed to cues evoking memories and images of foods throughout the day, this happens more and more frequently when we are satiated and metabolically replete. It is not clear how this hedonic hunger can be induced in the absence of metabolic depletion signals or during the postprandial phase when there is still plenty of absorbable energy in the gut. Why are we not simply ignoring such cues and stimuli? Several explanations are possible.
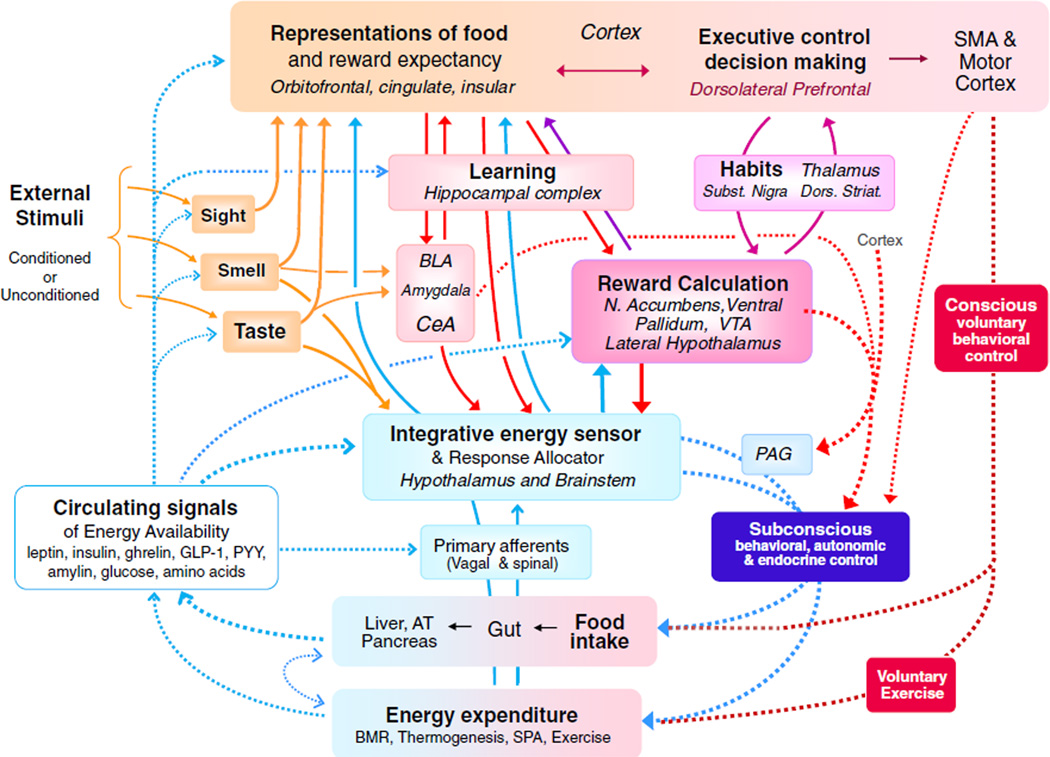
A model for cue-induced, conditioned food intake in satiated rats was developed by Weingarten(24). After temporally pairing a tone or light (conditioned stimulus, CS+) with the presentation of a retractable food cup in food-restricted animals, rats learned quickly to go to the food cup every time the CS+ was on. After rats had been returned to ad libitum feeding and were fully satiated, the CS+ continued to elicit food cup approach and a small meal(24), closely mimicking conditioned food intake through external cues in human subjects. In a series of elegant studies, Petrovich demonstrated the importance of a neural network including the amygdala, medial prefrontal cortex and lateral hypothalamus for this phenomenon to occur(25–27). It appears that inputs to the hypothalamus from both the amygdala and medial prefrontal cortex (see Fig. 1) are necessary to link specific conditioned stimuli to appetitive action. It will be interesting to investigate the role of lateral hypothalamic orexin neurons and their projections to the mesolimbic dopamine system, as these neurons have been implicated in µ-opioid-induced food intake(28), depletion-induced salt intake(29) and reinstatement of drug seeking(30). As the lateral hypothalamus is a major behavioural and autonomic output venue for the mediobasal hypothalamic integrative energy sensor, this modulatory input from the amygdala and prefrontal cortex may provide a basis for the overriding of homoeostatic regulation by external signals. However, it should be noted that neither the Weingarten(24) nor the Petrovich studies(25) tested whether prolonged repetition of CS+ exposure led to chronic overeating and development of obesity and whether transection of the critical amygdala-hypothalamic projections prevented it.
Fig. 1.
(colour online) Major neural systems and pathways involved in the control of ingestive behaviour and energy balance regulation with emphasis on interactions between the classical homoeostatic energy regulatory system in the hypothalamus and brainstem (blue boxes and arrows in lower half) and cognitive/emotional brain systems (red boxes and arrows in upper half). Bottom-up modulation of cognitive and emotional processes by metabolic signals and their derivatives is accomplished by (a) circulating hormones and metabolites acting not only on the hypothalamus and brainstem but also on external sensory processing pathways as well as on components of the corticolimbic system (open blue arrows with broken lines), (b) a stream of vagal and spinal sensory information from within the body to all levels of the neuraxis, including the cortex (full blue arrows with solid lines) and (c) neural signals generated by the integrative hypothalamic energy sensor and distributed to areas involved in reward-based decision making (full blue arrows with solid lines). Together, these ascending modulatory influences determine the level of incentive salience directed to specific nutrients. Top-down modulation of food intake and energy expenditure by cognitive and emotional/reward systems is accomplished by (a) direct external (taste and smell) sensory input to the hypothalamic energy sensor and response allocator (dark yellow lines), (b) input from the amygdala, cortex and reward processing systems to mainly the lateral hypothalamus, responsible for conditioned external signals to elicit food intake (full red lines and arrows), (c) inputs from cortex, amygdala and basal ganglia to midbrain extrapyramidal motor pathways (emotional motor system, broken red lines and full arrows) and (d) pyramidal motor system for voluntary behavioural control (broken red lines on the right). N. Accumbens, nucleus accumbens; SMA, supplemental motor area; BLA, basolateral amygdala; CeA, central nucleus of the amygdala; VTA, ventral tegmental area; PAG, periaqueductal gray; GLP-1, glucgon-like-peptide-1; PYY, peptide YY; AT, adipose tissue; SPA, spontaneous physical activity. Adapted from(12).
The phenomenon of sensory-specific satiety(31) may facilitate conditioned food intake in the satiated state. An example of this facilitation is the appeal of a new sensory food experience, typically dessert, at the end of a satiating meal. Little is known regarding the neural mechanisms involved in this phenomenon, but it has been shown that a reduction in the electrical activity of neurons in the orbitofrontal cortex, a part of the frontal cortex, of macaque monkeys, can reflect sensory-specific satiety(32). It is conceivable that some of the neurons in the orbitofrontal cortex direct their output to the lateral hypothalamus and thereby amplify vulnerability to conditioned food cues between meals.
It is also possible that the so-called cephalic phase responses to the sight and smell (or just thinking about) food can trigger appetitive behaviour (33,34). Perhaps the small increases in saliva, gastric acid, insulin and ghrelin secretion that constitute the cephalic response stimulate appetitive drive by acting on sensory nerves or directly on the brain and thereby enhance the neural effects of conditioned stimuli. We may also be more vulnerable to conditioned food cues when under stress. Food consumption as a form of self-medication to relieve stress has been demonstrated(35), although we do not know the neural mechanisms involved. Finally, a history of uncertainty about the food supply could also increase reactivity to food cues in the absence of direct metabolic hunger.
In summary, it has been clearly shown that conditioned stimuli can induce food intake in satiated rats and some of the critical neural circuitry has been identified. Thus, stimuli from the environment clearly have the capacity to temporarily overwhelm homoeostatic regulation. However, there is no animal or human study directly demonstrating that long-term exposure to conditioned stimuli leads to obesity.
Amplification of hedonic hunger by metabolic need
When conditioned cues such as food advertisements are present at times of metabolic depletion such as shortly before or during a meal, they are more likely to stimulate overingestion, because metabolic depletion amplifies their incentive salience(36,37). It is well known that metabolic hunger makes us more responsive to cues signalling food and drug reward(38,39). The neural pathways and mechanisms involved in this attribution of salience are not completely understood, but progress has recently been made. Specifically, it has been demonstrated that metabolic depletion signals in the form of high levels of circulating ghrelin as well as low levels of leptin, insulin, gut hormones and various metabolites can act not only on the classical brain areas involved in energy balance homoeostasis such as the hypothalamus and brainstem but also on brain areas involved in sensory processing, cognition and reward (Fig. 1; also see(40) for a more detailed discussion).
Modern eating habits: increased availability, variety and portion size
Even in the absence of food advertisements, we are finding ourselves more and more exposed to opportunities to eat. Compared with the relatively fixed-meal patterns of the past, availability of food has drastically increased at home, at the work place and in the larger community. In addition to the birthday cakes and vending machines at work and school and the increasing number of fast food places, the refrigerator at home is also always stacked with ready to eat foods. In addition, typical plate and serving size has increased dramatically and self-serve buffets are common(41). Although there are plenty of studies showing that manipulations of availability, variety and portion size have short-term effects on food intake in human subjects(42–45), few studies have looked at the longer-term consequences on intake and weight gain. In one such controlled clinical study, it was clearly demonstrated that increasing portion size resulted in sustained increase in food intake and weight gain over an 11 d observation period(46). However, it is inherently difficult and expensive to measure food intake in human subjects accurately in long-term studies. Thus, direct evidence that availability, opportunity and variety of food can cause human obesity is not as strong as commonly assumed. Furthermore, indirect evidence from cross-sectional studies comparing lean and obese subjects(45) is limited by the fact that it cannot distinguish cause and effect.
Animal studies provide much better experimental control over longer time periods. Clearly, exposing animals to ad libitum high-fat and variety (cafeteria) diets can cause hyperphagia and obesity(47). Standardised high-fat diets have now been commercially available for more than a decade and thousands of studies have been conducted; the role of diet composition and palatability is discussed in the next section. In stark contrast, there is only one study examining the role of availability in rodents. Rats that had access to four drinking spouts of sucrose and one spout of water ingest more energy and gained more weight over a 30 d observation period than rats that had access to one spout of sucrose and four spouts of water(48). These findings are truly startling. Although the acute overingestion could be easily explained by the initial curiosity to sample from each available spout, it is difficult to understand why there is no adaptation over time and why the homoeostatic regulatory feedback mechanisms failed. The authors entitled the paper ‘Obesity by Choice’, suggesting that it is the rat’s failure to make the sensible choice(48). It is critical to verify the results of this experiment, as it could not be replicated by another group of scientists (A Sclafani, personal communication).
What are the neural mechanisms responsible for eating more energetic food when availability, variety and portion size is high? Availability-induced hyperphagia in normal-weight subjects is likely to depend on neural mechanisms similar to those involved in food cue-induced hyperphagia as discussed earlier. The difference is that with cue-induced overeating, the stimuli are more immediate. That is, if signals indicating food availability coincide with signals of metabolic depletion shortly before a meal, their salience will be amplified resulting in an earlier start of the meal. Under metabolically replete conditions, the circuitry including amygdala, prefrontal cortex and lateral hypothalamus, shown to be responsible for conditioned food intake in satiated rats(25,27,49) is likely to be involved.
Modern foods: from palatable to addictive
Palatability is clearly one of the main drivers of food intake and it can lead to the development of obesity in susceptible individuals. However, the link between palatability and development of obesity is still not clear. Known as the ‘French Paradox’, the consumption of highly palatable French/Mediterranean cuisine produces less risk for obesity, suggesting that there are factors other than palatability that lead to chronic overconsumption. Energy-dense foods that are high in sugar and fat, and low in vitamins and minerals (also called empty energies), may be a more important factor. Foods such as this may be addictive.
Neural representations of the pleasure of eating
It is clear that the reward value of food is not only represented by its taste and flavour during the consumatory phase. A variety of sensory stimuli and emotional states or feelings with vastly different temporal profiles contribute to the experience of reward. Specifically, during the post-consumatory phase, nutrients interact with sensors in the gastrointestinal tract, other peripheral organs and the brain itself. It has recently been demonstrated that when all taste processing is eliminated by genetic manipulation, mice still learn to prefer sugar over water, suggesting the generation of food reward by processes of glucose utilisation(50).
Given the multifaceted involvement of pleasure and reward in ingestive behaviour, it is clear that multiple neural systems are involved (for a more detailed analysis, see(51)). Briefly, the most primitive form of liking and disliking appears to be inherent to components of the peripheral gustatory pathways in the brainstem(52–55). However, for the full sensory impact of palatable food and the subjective feeling of pleasure in human subjects, taste is integrated with other sensory modalities such as smell and mouth-feel. Integration takes place in forebrain areas including the amygdala, as well as primary and higher order sensory cortical areas including the insular and orbitofrontal cortex, where sensory representations of particular foods are formed(56–62). The exact neural pathways through which such sensory percepts or representations lead to the generation of subjective pleasure are not clear. Neuroimaging studies in human subjects suggest that pleasure, as measured by subjective ratings, is computed within portions of the orbitofrontal and perhaps insular cortex(55,63).
Neural systems representing the motivation to eat
The ultimate goal of food advertisement is to entice an individual to buy a specific food product and get hooked on it. This goal can be linked to what happens in addiction to drugs and alcohol, and it is not surprising that similar neural mechanisms have been implicated. Although ‘liking’ a branded food item seems necessary, ‘wanting’ it and buying it is more important for successful marketing. According to the liking/wanting distinction in food reward, it is possible to ‘want’ something that is not liked(64). Berridge defined wanting as ‘Incentive salience, or motivation for reward typically triggered by reward-relatedcues’(36). The mesolimbic dopamine system with projections from the ventral tegmental area to the nucleus accumbens, prefrontal cortex, amygdala and hippocampus seems to be a key neural substrate for wanting (Fig. 1). Phasic activity of dopamine neurons projecting from the ventral tegmental area to the nucleus accumbens in the ventral striatum is involved in the decision-making process during the preparatory (appetitive) phase of ingestive behaviour(65,66). In addition, when palatable foods such as sucrose are actually consumed, a sustained and sweetness-dependent increase and turnover in dopamine levels occurs in the nucleus accumbens(67–69). Dopamine signalling in the nucleus accumbens thus appears to play a role in both the appetitive and consumatory phases of an ingestive bout. The nucleus accumbens shell is thereby part of a neural loop including the lateral hypothalamus and the ventral tegmental area, with orexin neurons playing a key role(28,70–74). This loop appears to be important for transmitting metabolic state signals from the lateral hypothalamus and thus attributing incentive salience to goal objects, as discussed earlier.
Eating and ‘free will’
In human subjects, there is also wanting at a more conscious level, described by Berridge as a ‘cognitive desire for a declarative goal in the ordinary sense of the word wanting’(36). In addition to the mesolimbic dopamine system, a number of cortical areas, such as the dorsolateral prefrontal cortex and other components of a decision-making system are likely involved(75). Ultimately, a conscious decision can be made to eat a food item or to abstain from eating it. Although this appears to be up to the ‘free will’ of every individual, even apparently conscious decisions may have a subconscious component. This was demonstrated in a neuroimaging study in human subjects which was designed to decode the outcome of decisions before and after they reached awareness(76). Notably, when the subject’s decision reached conscious awareness, it already had been influenced for up to 10 s by unconscious (unaware) brain activity in the lateral and medial fronto-polar as well as anterior cingulate cortex and the precuneus(76). That prefrontal activity is necessary to choose advantageously in a gambling task was shown in a study in patients with prefrontal lesions(77). Normal subjects began to choose advantageously before they realised which strategy worked best, and they exhibited anticipatory skin conductance responses before they knew explicitly that it was a risky choice. In contrast, prefrontal patients continued to make disadvantageous choices and never showed an anticipatory autonomic response(77). These findings strongly suggest that subconscious neural activity can guide ingestive behaviour before conscious explicit knowledge does. The neural pathways for behavioural and autonomic control that escapes awareness is not well understood. Nevertheless, pathways from various prefrontal cortical areas and particularly strong descending pathways from the amygdala to areas in the midbrain (including the periaqueductal grey), brain stem and spinal cord are known to be part of the emotional motor system that exist outside the bounds of conscious control(78–80) (Fig. 1). Interestingly, many areas of the limbic system, including the cortex have direct, monosynaptic inputs to autonomic preganglionic neurons(81), providing an avenue for subconscious modulation of peripheral organs involved in metabolic processes (Fig. 1).
Overlap of neural pathways for food intake and drug addiction
Based on the observation that dopamine receptor-2 availability within the dorsal striatum is similarly reduced in both obese subjects and cocaine addicts(82), a heated discussion about the similarities between food and drug addiction has ensued(83–92).
As repeated exposure to drugs of abuse causes neuro-adaptive changes leading to elevations in reward thresholds (tolerance resulting in decreased reward) that drive accelerated drug intake(93–98), similar neural and behavioural changes can be predicted from repeated exposure to addictive foods. For example, repeated sucrose access is known to up-regulate dopamine release(99) and dopamine transporter expression(100), as well as to change dopamine D1 and D2-receptor availability in the nucleus accumbens(99,101). These changes may be responsible for the observed escalation of sucrose binging, cross-sensitisation to amphetamine-induced locomotor activity, withdrawal symptoms, such as increased anxiety and depression(99) and the reduced reinforcing efficacy of normal foods(102).
Exposure to a palatable cafeteria diet in Wistar rats led to sustained hyperphagia over 40 d and lateral hypothalamic electrical self-stimulation threshold increased in parallel to body weight gain(103). A similar insensitivity of the reward system was previously seen in addicted rats that self-administered intravenous cocaine or heroin(93,94). Dopamine D2-receptor expression in the dorsal striatum was significantly reduced, in parallel to worsening of the reward threshold(103), to levels found in cocaine addicted rats(104). Interestingly, after 14 d of abstinence from the palatable diet, reward threshold did not normalise even though the rats were hypophagic and lost about 10% body weight(103). This is in contrast to the relatively rapid (about 48 h) normalisation in reward thresholds in rats that abstained from cocaine self-administration(94), and may indicate the presence of irreversible changes caused by the high-fat content of the diet (see next section). Given the observation that cocaine addicts and obese human subjects exhibit low D2-receptor availability in the dorsal striatum(105), dopamine plasticity due to repeated consumption of palatable food may be similar to what occurs with repeated consumption of drugs of abuse. On the other hand, there is less convincing evidence for development of dependence on high-fat food(106,107), although intermittent access to corn oil can stimulate dopamine release in the nucleus accumbens(108).
Modern foods: from energy dense to toxic
There is mounting evidence from rodent studies that eating a high-fat diet not only puts pressure on energy balance by providing extra energy, but that it can cause brain damage. The very brain area that is supposed to tightly regulate energy balance, the hypothalamus, appears to get corrupted by eating high-fat food(109–115). The complex cascades of molecular changes through which high-fat feeding appears to impair leptin and insulin signalling, most critical for body weight regulation and glucose homoeostasis have recently been reviewed by Ryan et al.(116).
Observations from experiments using fatty acid administration or blockade of fatty acid-induced inflammation in the brain suggest that a short period of fat feeding(115,117) and even a single high-fat meal(118,119) are enough to rapidly inflict hypothalamic injury and impairment of normal nutrient-sensing and energy balance functions of the hypothalamus. An even worse scenario is that fetal exposure to the mouse dam’s high-fat diet is apparently enough to cause hypothalamic dysfunction(120). Thus, pro-inflammatory signalling is no longer regarded as a consequence of the obese state, but appears to be one of the first causative steps in high-fat diet-induced obesity. The only encouraging news is that unsaturated fatty acids directly infused into the brain of mice appear to almost completely reverse hypothalamic inflammation and obesity induced by eating a high-fat diet rich in saturated fats for 8 weeks(121). It is thus possible that specifically saturated fats can cause these debilitating effects to the brain(122).
In addition to direct deleterious effects on the hypothalamus, high-fat diets also appear to disrupt normal satiety-signalling from the gut. High-fat diets can stimulate inflammatory signalling via increased mucosal permeability and Toll-like receptors in rats that become hyperphagic and obese, but not in rats that are resistant(123). It looks more and more like a distinct possibility that changes in the composition of the gut microbiota via stimulation of the innate immune response, the inflammasome, are at the origin of the intestinal and eventually systemic and brain inflammation(124–127); and see recent review by Harris et al.(128). As microbiota can be transferred between subjects, the resulting obesity and fatty-liver disease may even be looked at as a communicable disease(129). The sensitivity of vagal afferent chemo- and mechano-sensors communicating to the brain is also reduced in high-fat diet obese rats and mice(130–135).
These new findings discussed earlier raise a lot of new questions. It is hard to believe that eating one fat-rich meal should start a cascade of events that eventually lead to obesity, diabetes and dementia. Why should eating the macronutrient fat that provides valuable energy and prevents starvation have such clear-cut maladaptive consequences? It is unlikely that eating just one ‘forbidden fruit’ is a nutritional sin, and it remains to be seen whether the acute effects obtained with pharmacological manipulations in the brain mimic real physiological mechanisms. Furthermore, it is not known whether such acute effects occur in human subjects. If they do occur, acute numbing of hypothalamic nutrient sensing by fat-rich meals might have been adaptive in the past by providing a mechanism to take advantage of rare moments of nutritional abundance.
The chronic effects of high-fat eating are more difficult to ignore, although they seem just as maladaptive as the acute effects. Why does the mouse not avoid high-fat food that apparently makes it sick? What happened to the ‘wisdom of the body’? How is it that animals and man evolved elaborate taste perception and rapid learning mechanisms to avoid toxic foods, but they are easily fooled by toxic fat?
Modern environment: less opportunity to burn energy
This review has almost entirely focused on energy intake, but it is clear that the modern environment also affects energy expenditure in a number of ways. Although we are beginning to understand the neurobiology of food intake in the modern world, we remain almost completely ignorant regarding the neurobiological controls of physical activity and exercise and the integrative processes that comprise the regulation of energy balance(136). One reason might be that we have a limited understanding of hormonal (or neural) inter-organ communication. Although we know a lot about gut–brain and adipose tissue–brain signalling, we know virtually nothing about communication between the exercising muscle and the brain and other organs. Only very recently, the muscle-derived hormone irisin was discovered which appears to induce browning of white adipose tissue(137). It will be interesting to see whether this hormone also signals to the brain systems regulating energy balance.
Conclusions
Clearly, appetitive drive and food intake are affected by signals from inside the body and the environment, and the latter are exploited by the food industry through the newly established field of neuromarketing. Although these techniques would be just as powerful to stimulate eating of healthy foods, not much effort has been made towards this goal. Environmental signals affecting food intake interact almost exclusively with corticolimbic brain areas involved in cognition, emotion, motivation and decision making. These systems, although modulated in a bottom-up manner by metabolic signals, can exert strong and overpowering top-down control of food intake and energy balance regulation, as demonstrated by eating in the complete absence of nutritional need. However, most of these demonstrations of top-down control act only in an acute fashion, and more long-term studies are necessary to demonstrate a lasting impact on body weight. Finally, the neural pathways linking corticolimbic functions with hypothalamic and brainstem structures involved in the control of food intake and energy balance need to be better defined. Specifically, the respective contributions of conscious and subconcious determinants of behavioural action and autonomic control should be further investigated.
Acknowledgements
I would like to thank Katie Bailey for editorial assistance and Christopher Morrison, Heike Münzberg and Brenda Richards for valuable comments on an earlier draft of this manuscript. This work was supported by the National Institutes of Health Grants DK047348 and DK0871082.
Footnotes
The author declares no conflict of interest.
References
- 1.Guyenet SJ, Schwartz MW. Clinical review + : regulation of food intake, energy balance, and body fat mass: implications for the pathogenesis and treatment of obesity. J Clin Endocrinol Metab. 2012;97:745–755. doi: 10.1210/jc.2011-2525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Farooqi S, O’Rahilly S. Genetics of obesity in humans. Endocr Rev. 2006;27:710–718. doi: 10.1210/er.2006-0040. [DOI] [PubMed] [Google Scholar]
- 3.Bouchard C. Genetics of obesity: an update on molecular markers. Int J Obes Relat Metab Disord. 1995;19(Suppl. 3):S10–S13. [PubMed] [Google Scholar]
- 4.Speakman JR. Thrifty genes for obesity, an attractive but flawed idea, and an alternative perspective: the ‘drifty gene’ hypothesis. Int J Obes (Lond) 2008;32:1611–1617. doi: 10.1038/ijo.2008.161. [DOI] [PubMed] [Google Scholar]
- 5.Harris RB. Role of set-point theory in regulation of body weight. FASEB J. 1990;4:3310–3318. doi: 10.1096/fasebj.4.15.2253845. [DOI] [PubMed] [Google Scholar]
- 6.Hall KD, Heymsfield SB, Kemnitz JW, et al. Energy balance and its components: implications for body weight regulation. Am J Clin Nutr. 2012;95:989–994. doi: 10.3945/ajcn.112.036350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Speakman JR, Levitsky DA, Allison DB, et al. Set points, settling points and some alternative models: theoretical options to understand how genes and environments combine to regulate body adiposity. Dis Model Mech. 2011;4:733–745. doi: 10.1242/dmm.008698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Grill HJ, Kaplan JM. The neuroanatomical axis for control of energy balance. Front Neuroendocrinol. 2002;23:2–40. doi: 10.1006/frne.2001.0224. [DOI] [PubMed] [Google Scholar]
- 9.Berthoud HR. Multiple neural systems controlling food intake and body weight. Neurosci Biobehav Rev. 2002;26:393–428. doi: 10.1016/s0149-7634(02)00014-3. [DOI] [PubMed] [Google Scholar]
- 10.Berthoud HR. Mind versus metabolism in the control of food intake and energy balance. Physiol Behav. 2004;81:781–793. doi: 10.1016/j.physbeh.2004.04.034. [DOI] [PubMed] [Google Scholar]
- 11.Berthoud HR, Morrison C. The brain, appetite, and obesity. Annu Rev Psychol. 2008;59:55–92. doi: 10.1146/annurev.psych.59.103006.093551. [DOI] [PubMed] [Google Scholar]
- 12.Berthoud HR. Metabolic and hedonic drives in the neural control of appetite: who is the boss? Curr Opin Neurobiol. 2011;21:888–896. doi: 10.1016/j.conb.2011.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jones SC, Mannino N, Green J. ‘Like me, want me, buy me, eat me’: relationship-building marketing communications in children’s magazines. Public Health Nutr. 2010;13:2111–2118. doi: 10.1017/S1368980010000455. [DOI] [PubMed] [Google Scholar]
- 14.Levitsky DA, Pacanowski CR. Free will and the obesity epidemic. Public Health Nutr. 2011;19:1–16. doi: 10.1017/S1368980011002187. [DOI] [PubMed] [Google Scholar]
- 15.Effertz T, Wilcke AC. Do television food commercials target children in Germany? Public Health Nutr. 2011;14:1–8. doi: 10.1017/S1368980011003223. [DOI] [PubMed] [Google Scholar]
- 16.Powell LM, Szczypka G, Chaloupka FJ. Trends in exposure to television food advertisements among children and adolescents in the United States. Arch Pediatr Adolesc Med. 2010;164:794–802. doi: 10.1001/archpediatrics.2010.139. [DOI] [PubMed] [Google Scholar]
- 17.Mink M, Evans A, Moore CG, et al. Nutritional imbalance endorsed by televised food advertisements. J Am Diet Assoc. 2010;110:904–910. doi: 10.1016/j.jada.2010.03.020. [DOI] [PubMed] [Google Scholar]
- 18.Pettigrew S, Roberts M, Chapman K, et al. The use of negative themes in television food advertising. Appetite. 2012;58:496–503. doi: 10.1016/j.appet.2011.12.014. [DOI] [PubMed] [Google Scholar]
- 19.Boyland EJ, Harrold JA, Kirkham TC, et al. Persuasive techniques used in television advertisements to market foods to UK children. Appetite. 2012;58:658–664. doi: 10.1016/j.appet.2011.11.017. [DOI] [PubMed] [Google Scholar]
- 20.Hebden L, King L, Kelly B. Art of persuasion: an analysis of techniques used to market foods to children. J Paediatr Child Health. 2011;47:776–782. doi: 10.1111/j.1440-1754.2011.02025.x. [DOI] [PubMed] [Google Scholar]
- 21.Speers SE, Harris JL, Schwartz MB. Child and adolescent exposure to food and beverage brand appearances during prime-time television programming. Am J Prev Med. 2011;41:291–296. doi: 10.1016/j.amepre.2011.04.018. [DOI] [PubMed] [Google Scholar]
- 22.de Droog SM, Valkenburg PM, Buijzen M. Using brand characters to promote young children’s liking of and purchase requests for fruit. J Health Commun. 2011;16:79–89. doi: 10.1080/10810730.2010.529487. [DOI] [PubMed] [Google Scholar]
- 23.Corsini N, Slater A, Harrison A, et al. Rewards can be used effectively with repeated exposure to increase liking of vegetables in 4–6-year-old children. Public Health Nutr. 2011;7:1–10. doi: 10.1017/S1368980011002035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Weingarten HP. Conditioned cues elicit feeding in sated rats: a role for learning in meal initiation. Science. 1983;220:431–433. doi: 10.1126/science.6836286. [DOI] [PubMed] [Google Scholar]
- 25.Petrovich GD, Setlow B, Holland PC, et al. Amygdalo-hypothalamic circuit allows learned cues to override satiety and promote eating. J Neurosci. 2002;22:8748–8753. doi: 10.1523/JNEUROSCI.22-19-08748.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Petrovich GD, Holland PC, Gallagher M. Amygdalar and prefrontal pathways to the lateral hypothalamus are activated by a learned cue that stimulates eating. J Neurosci. 2005;25:8295–8302. doi: 10.1523/JNEUROSCI.2480-05.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Petrovich GD, Ross CA, Holland PC, et al. Medial prefrontal cortex is necessary for an appetitive contextual conditioned stimulus to promote eating in sated rats. J Neurosci. 2007;27:6436–6441. doi: 10.1523/JNEUROSCI.5001-06.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zheng H, Patterson LM, Berthoud HR. Orexin signaling in the ventral tegmental area is required for high-fat appetite induced by opioid stimulation of the nucleus accumbens. J Neurosci. 2007;27:11075–11082. doi: 10.1523/JNEUROSCI.3542-07.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Liedtke WB, McKinley MJ, Walker LL, et al. Relation of addiction genes to hypothalamic gene changes subserving genesis and gratification of a classic instinct, sodium appetite. Proc Natl Acad Sci USA. 2011;108:12509–12514. doi: 10.1073/pnas.1109199108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Aston-Jones G, Smith RJ, Sartor GC, et al. Lateral hypothalamic orexin/hypocretin neurons: a role in reward-seeking and addiction. Brain Res. 2010;1314:74–90. doi: 10.1016/j.brainres.2009.09.106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rolls BJ, Rolls ET, Rowe EA, et al. Sensory specific satiety in man. Physiol Behav. 1981;27:137–142. doi: 10.1016/0031-9384(81)90310-3. [DOI] [PubMed] [Google Scholar]
- 32.Rolls ET, Sienkiewicz ZJ, Yaxley S. Hunger modulates the responses to gustatory stimuli of single neurons in the caudolateral orbitofrontal cortex of the macaque monkey. Eur J Neurosci. 1989;1:53–60. doi: 10.1111/j.1460-9568.1989.tb00774.x. [DOI] [PubMed] [Google Scholar]
- 33.Parra-Covarrubias A, Rivera-Rodriguez I, Almaraz-Ugalde A. Cephalic phase of insulin secretion in obese adolescents. Diabetes. 1971;20:800–802. doi: 10.2337/diab.20.12.800. [DOI] [PubMed] [Google Scholar]
- 34.Powley TL. The ventromedial hypothalamic syndrome, satiety, and a cephalic phase hypothesis. Psychol Rev. 1977;84:89–126. [PubMed] [Google Scholar]
- 35.Dallman MF, Pecoraro N, Akana SF, et al. Chronic stress and obesity: a new view of ‘comfort food’. Proc Natl Acad Sci USA. 2003;100:11696–11701. doi: 10.1073/pnas.1934666100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Berridge KC, Ho CY, Richard JM, et al. The tempted brain eats: pleasure and desire circuits in obesity and eating disorders. Brain Res. 2010;1350:43–64. doi: 10.1016/j.brainres.2010.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Berridge KC. The debate over dopamine’s role in reward: the case for incentive salience. Psychopharmacology (Berl) 2007;191:391–431. doi: 10.1007/s00213-006-0578-x. [DOI] [PubMed] [Google Scholar]
- 38.Highfield DA, Mead AN, Grimm JW, et al. Reinstatement of cocaine seeking in 129X1/SvJ mice: effects of cocaine priming, cocaine cues and food deprivation. Psychopharmacology (Berl) 2002;161:417–424. doi: 10.1007/s00213-002-1047-9. [DOI] [PubMed] [Google Scholar]
- 39.Carr KD. Chronic food restriction: enhancing effects on drug reward and striatal cell signaling. Physiol Behav. 2007;91:459–472. doi: 10.1016/j.physbeh.2006.09.021. [DOI] [PubMed] [Google Scholar]
- 40.Berthoud HR. Interactions between the ‘cognitive’ and ‘metabolic’ brain in the control of food intake. Physiol Behav. 2007;91:486–498. doi: 10.1016/j.physbeh.2006.12.016. [DOI] [PubMed] [Google Scholar]
- 41.Rolls BJ. The supersizing of America: portion size and the obesity epidemic. Nutr Today. 2003;38:42–53. doi: 10.1097/00017285-200303000-00004. [DOI] [PubMed] [Google Scholar]
- 42.Levitsky DA, Youn T. The more food young adults are served, the more they overeat. J Nutr. 2004;134:2546–2549. doi: 10.1093/jn/134.10.2546. [DOI] [PubMed] [Google Scholar]
- 43.Wansink B, Kim J. Bad popcorn in big buckets: portion size can influence intake as much as taste. J Nutr Educ Behav. 2005;37:242–245. doi: 10.1016/s1499-4046(06)60278-9. [DOI] [PubMed] [Google Scholar]
- 44.Wansink B, van Ittersum K, Painter JE. Ice cream illusions bowls, spoons, and self-served portion sizes. Am J Prev Med. 2006;31:240–243. doi: 10.1016/j.amepre.2006.04.003. [DOI] [PubMed] [Google Scholar]
- 45.Wansink B, Payne CR. Eating behavior and obesity at Chinese buffets. Obesity (Silver Spring) 2008;16:1957–1960. doi: 10.1038/oby.2008.286. [DOI] [PubMed] [Google Scholar]
- 46.Rolls BJ, Roe LS, Meengs JS. Larger portion sizes lead to a sustained increase in energy intake over 2 days. J Am Diet Assoc. 2006;106:543–549. doi: 10.1016/j.jada.2006.01.014. [DOI] [PubMed] [Google Scholar]
- 47.Sclafani A, Springer D. Dietary obesity in adult rats: similarities to hypothalamic and human obesity syndromes. Physiol Behav. 1976;17:461–471. doi: 10.1016/0031-9384(76)90109-8. [DOI] [PubMed] [Google Scholar]
- 48.Tordoff MG. Obesity by choice: the powerful influence of nutrient availability on nutrient intake. Am J Physiol Regul Integr Comp Physiol. 2002;282:R1536–R1539. doi: 10.1152/ajpregu.00739.2001. [DOI] [PubMed] [Google Scholar]
- 49.Petrovich GD, Gallagher M. Amygdala subsystems and control of feeding behavior by learned cues. Ann N Y Acad Sci. 2003;985:251–262. doi: 10.1111/j.1749-6632.2003.tb07086.x. [DOI] [PubMed] [Google Scholar]
- 50.de Araujo IE, Oliveira-Maia AJ, Sotnikova TD, et al. Food reward in the absence of taste receptor signaling. Neuron. 2008;57:930–941. doi: 10.1016/j.neuron.2008.01.032. [DOI] [PubMed] [Google Scholar]
- 51.Berthoud HR, Lenard NR, Shin AC. Food reward, hyperphagia, and obesity. Am J Physiol Regul Integr Comp Physiol. 2011;300:R1266–R1277. doi: 10.1152/ajpregu.00028.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Grill HJ, Norgren R. The taste reactivity test. I. Mimetic responses to gustatory stimuli in neurologically normal rats. Brain Res. 1978;143:263–279. doi: 10.1016/0006-8993(78)90568-1. [DOI] [PubMed] [Google Scholar]
- 53.Steiner JE. The gustofacial response: observations on normal and anancephalic newborn infants. Bethesda, MD: U. S. Department of Health, Education, and Welfare; 1973. [PubMed] [Google Scholar]
- 54.Berridge KC. Measuring hedonic impact in animals and infants: microstructure of affective taste reactivity patterns. Neurosci Biobehav Rev. 2000;24:173–198. doi: 10.1016/s0149-7634(99)00072-x. [DOI] [PubMed] [Google Scholar]
- 55.Berridge KC, Kringelbach ML. Affective neuroscience of pleasure: reward in humans and animals. Psychopharmacology (Berl) 2008;199:457–480. doi: 10.1007/s00213-008-1099-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Verhagen JV. The neurocognitive bases of human multimodal food perception: cconsciousness. Brain Res Brain Res Rev. 2006;53:271–286. doi: 10.1016/j.brainresrev.2006.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Rolls ET, Verhagen JV, Kadohisa M. Representations of the texture of food in the primate orbitofrontal cortex: neurons responding to viscosity, grittiness, and capsaicin. J Neurophysiol. 2003;90:3711–3724. doi: 10.1152/jn.00515.2003. [DOI] [PubMed] [Google Scholar]
- 58.Rolls ET. The orbitofrontal cortex and reward. Cereb Cortex. 2000;10:284–294. doi: 10.1093/cercor/10.3.284. [DOI] [PubMed] [Google Scholar]
- 59.Small DM, Jones-Gotman M, Zatorre RJ, et al. A role for the right anterior temporal lobe in taste quality recognition. J Neurosci. 1997;17:5136–5142. doi: 10.1523/JNEUROSCI.17-13-05136.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Small DM, Zald DH, Jones-Gotman M, et al. Human cortical gustatory areas: a review of functional neuroimaging data. Neuroreport. 1999;10:7–14. doi: 10.1097/00001756-199901180-00002. [DOI] [PubMed] [Google Scholar]
- 61.de Araujo IE, Kringelbach ML, Rolls ET, et al. Representation of umami taste in the human brain. J Neurophysiol. 2003;90:313–319. doi: 10.1152/jn.00669.2002. [DOI] [PubMed] [Google Scholar]
- 62.de Araujo IE, Rolls ET, Kringelbach ML, et al. Taste-olfactory convergence, and the representation of the pleasantness of flavour, in the human brain. Eur J Neurosci. 2003;18:2059–2068. doi: 10.1046/j.1460-9568.2003.02915.x. [DOI] [PubMed] [Google Scholar]
- 63.Kringelbach ML. Food for thought: hedonic experience beyond homeostasis in the human brain. Neuroscience. 2004;126:807–819. doi: 10.1016/j.neuroscience.2004.04.035. [DOI] [PubMed] [Google Scholar]
- 64.Berridge KC, Robinson TE, Aldridge JW. Dissecting components of reward: ‘liking’, ‘wanting’, and learning. Curr Opin Pharmacol. 2009;9:65–73. doi: 10.1016/j.coph.2008.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Schultz W, Dayan P, Montague PR. A neural substrate of prediction and reward. Science. 1997;275:1593–1599. doi: 10.1126/science.275.5306.1593. [DOI] [PubMed] [Google Scholar]
- 66.Carelli RM. The nucleus accumbens and reward: neurophysiological investigations in behaving animals. Behav Cogn Neurosci Rev. 2002;1:281–296. doi: 10.1177/1534582302238338. [DOI] [PubMed] [Google Scholar]
- 67.Hernandez L, Hoebel BG. Feeding and hypothalamic stimulation increase dopamine turnover in the accumbens. Physiol Behav. 1988;44:599–606. doi: 10.1016/0031-9384(88)90324-1. [DOI] [PubMed] [Google Scholar]
- 68.Hajnal A, Smith GP, Norgren R. Oral sucrose stimulation increases accumbens dopamine in the rat. Am J Physiol Regul Integr Comp Physiol. 2004;286:R31–R37. doi: 10.1152/ajpregu.00282.2003. [DOI] [PubMed] [Google Scholar]
- 69.Smith GP. Accumbens dopamine mediates the rewarding effect of orosensory stimulation by sucrose. Appetite. 2004;43:11–13. doi: 10.1016/j.appet.2004.02.006. [DOI] [PubMed] [Google Scholar]
- 70.Stratford TR, Kelley AE. Evidence of a functional relationship between the nucleus accumbens shell and lateral hypothalamus subserving the control of feeding behavior. J Neurosci. 1999;19:11040–11048. doi: 10.1523/JNEUROSCI.19-24-11040.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Harris GC, Wimmer M, Aston-Jones G. A role for lateral hypothalamic orexin neurons in reward seeking. Nature. 2005;437:556–559. doi: 10.1038/nature04071. [DOI] [PubMed] [Google Scholar]
- 72.Peyron C, Tighe DK, van den Pol AN, et al. Neurons containing hypocretin (orexin) project to multiple neuronal systems. J Neurosci. 1998;18:9996–10015. doi: 10.1523/JNEUROSCI.18-23-09996.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Nakamura T, Uramura K, Nambu T, et al. Orexin-induced hyperlocomotion and stereotypy are mediated by the dopaminergic system. Brain Res. 2000;873:181–187. doi: 10.1016/s0006-8993(00)02555-5. [DOI] [PubMed] [Google Scholar]
- 74.Korotkova TM, Sergeeva OA, Eriksson KS, et al. Excitation of ventral tegmental area dopaminergic and nondopaminergic neurons by orexins/hypocretins. J Neurosci. 2003;23:7–11. doi: 10.1523/JNEUROSCI.23-01-00007.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Hare TA, O’Doherty J, Camerer CF, et al. Dissociating the role of the orbitofrontal cortex and the striatum in the computation of goal values and prediction errors. J Neurosci. 2008;28:5623–5630. doi: 10.1523/JNEUROSCI.1309-08.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Soon CS, Brass M, Heinze HJ, et al. Unconscious determinants of free decisions in the human brain. Nat Neurosci. 2008;11:543–545. doi: 10.1038/nn.2112. [DOI] [PubMed] [Google Scholar]
- 77.Bechara A, Damasio H, Tranel D, et al. Deciding advantageously before knowing the advantageous strategy. Science. 1997;275:1293–1295. doi: 10.1126/science.275.5304.1293. [DOI] [PubMed] [Google Scholar]
- 78.Hurley KM, Herbert H, Moga MM, et al. Efferent projections of the infralimbic cortex of the rat. J Comp Neurol. 1991;308:249–276. doi: 10.1002/cne.903080210. [DOI] [PubMed] [Google Scholar]
- 79.Ghashghaei HT, Barbas H. Neural interaction between the basal forebrain and functionally distinct prefrontal cortices in the rhesus monkey. Neuroscience. 2001;103:593–614. doi: 10.1016/s0306-4522(00)00585-6. [DOI] [PubMed] [Google Scholar]
- 80.Tettamanti M, Rognoni E, Cafiero R, et al. Distinct pathways of neural coupling for different basic emotions. Neuroimage. 2012;59:1804–1817. doi: 10.1016/j.neuroimage.2011.08.018. [DOI] [PubMed] [Google Scholar]
- 81.Westerhaus MJ, Loewy AD. Central representation of the sympathetic nervous system in the cerebral cortex. Brain Res. 2001;903:117–127. doi: 10.1016/s0006-8993(01)02453-2. [DOI] [PubMed] [Google Scholar]
- 82.Volkow ND, Wise RA. How can drug addiction help us understand obesity? Nat Neurosci. 2005;8:555–560. doi: 10.1038/nn1452. [DOI] [PubMed] [Google Scholar]
- 83.Volkow ND, Wang GJ, Fowler JS, et al. Overlapping neuronal circuits in addiction and obesity: evidence of systems pathology. Philos Trans R Soc Lond B Biol Sci. 2008;363:3191–3200. doi: 10.1098/rstb.2008.0107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Pelchat ML. Of human bondage: food craving, obsession, compulsion, and addiction. Physiol Behav. 2002;76:347–352. doi: 10.1016/s0031-9384(02)00757-6. [DOI] [PubMed] [Google Scholar]
- 85.Levine AS, Kotz CM, Gosnell BA. Sugars: hedonic aspects, neuroregulation, and energy balance. Am J Clin Nutr. 2003;78:834S–842S. doi: 10.1093/ajcn/78.4.834S. [DOI] [PubMed] [Google Scholar]
- 86.Kelley AE, Berridge KC. The neuroscience of natural rewards: relevance to addictive drugs. J Neurosci. 2002;22:3306–3311. doi: 10.1523/JNEUROSCI.22-09-03306.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Grigson PS. Like drugs for chocolate: separate rewards modulated by common mechanisms? Physiol Behav. 2002;76:389–395. doi: 10.1016/s0031-9384(02)00758-8. [DOI] [PubMed] [Google Scholar]
- 88.Del Parigi A, Chen K, Salbe AD, et al. Are we addicted to food? Obes Res. 2003;11:493–495. doi: 10.1038/oby.2003.68. [DOI] [PubMed] [Google Scholar]
- 89.Corwin RL, Grigson PS. Symposium overview – Food addiction: fact or fiction? J Nutr. 2009;139:617–619. doi: 10.3945/jn.108.097691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Rogers PJ, Smit HJ. Food craving and food ‘addiction’: a critical review of the evidence from a biopsychosocial perspective. Pharmacol Biochem Behav. 2000;66:3–14. doi: 10.1016/s0091-3057(00)00197-0. [DOI] [PubMed] [Google Scholar]
- 91.Davis C, Carter JC. Compulsive overeating as an addiction disorder. A review of theory and evidence. Appetite. 2009;53:1–8. doi: 10.1016/j.appet.2009.05.018. [DOI] [PubMed] [Google Scholar]
- 92.Epstein DH, Shaham Y. Cheesecake-eating rats and the question of food addiction. Nat Neurosci. 2010;13:529–531. doi: 10.1038/nn0510-529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Ahmed SH, Kenny PJ, Koob GF, et al. Neurobiological evidence for hedonic allostasis associated with escalating cocaine use. Nat Neurosci. 2002;5:625–626. doi: 10.1038/nn872. [DOI] [PubMed] [Google Scholar]
- 94.Markou A, Koob GF. Postcocaine anhedonia. An animal model of cocaine withdrawal. Neuropsychopharmacology. 1991;4:17–26. [PubMed] [Google Scholar]
- 95.Russo SJ, Dietz DM, Dumitriu D, et al. The addicted synapse: mechanisms of synaptic and structural plasticity in nucleus accumbens. Trends Neurosci. 2010;33:267–276. doi: 10.1016/j.tins.2010.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Hyman SE, Malenka RC, Nestler EJ. Neural mechanisms of addiction: the role of reward-related learning and memory. Annu Rev Neurosci. 2006;29:565–598. doi: 10.1146/annurev.neuro.29.051605.113009. [DOI] [PubMed] [Google Scholar]
- 97.Koob GF, Le Moal M. Plasticity of reward neurocircuitry and the ‘dark side’ of drug addiction. Nat Neurosci. 2005;8:1442–1444. doi: 10.1038/nn1105-1442. [DOI] [PubMed] [Google Scholar]
- 98.Koob GF, Le Moal M. Addiction and the brain antireward system. Annu Rev Psychol. 2008;59:29–53. doi: 10.1146/annurev.psych.59.103006.093548. [DOI] [PubMed] [Google Scholar]
- 99.Avena NM, Rada P, Hoebel BG. Evidence for sugar addiction: behavioral and neurochemical effects of intermittent, excessive sugar intake. Neurosci Biobehav Rev. 2008;32:20–39. doi: 10.1016/j.neubiorev.2007.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Bello NT, Sweigart KL, Lakoski JM, et al. Restricted feeding with scheduled sucrose access results in an up-regulation of the rat dopamine transporter. Am J Physiol Regul Integr Comp Physiol. 2003;284:R1260–R1268. doi: 10.1152/ajpregu.00716.2002. [DOI] [PubMed] [Google Scholar]
- 101.Bello NT, Lucas LR, Hajnal A. Repeated sucrose access influences dopamine D2 receptor density in the striatum. Neuroreport. 2002;13:1575–1578. doi: 10.1097/00001756-200208270-00017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Cottone P, Sabino V, Steardo L, et al. Intermittent access to preferred food reduces the reinforcing efficacy of chow in rats. Am J Physiol Regul Integr Comp Physiol. 2008;295:R1066–R1076. doi: 10.1152/ajpregu.90309.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Johnson PM, Kenny PJ. Dopamine D2 receptors in addiction-like reward dysfunction and compulsive eating in obese rats. Nat Neurosci. 2010;13:635–641. doi: 10.1038/nn.2519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Dalley JW, Fryer TD, Brichard L, et al. Nucleus accumbens D2/3 receptors predict trait impulsivity and cocaine reinforcement. Science. 2007;315:1267–1270. doi: 10.1126/science.1137073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Wang GJ, Volkow ND, Thanos PK, et al. Similarity between obesity and drug addiction as assessed by neurofunctional imaging: a concept review. J Addict Dis. 2004;23:39–53. doi: 10.1300/J069v23n03_04. [DOI] [PubMed] [Google Scholar]
- 106.Boggiano MM, Chandler PC, Viana JB, et al. Combined dieting and stress evoke exaggerated responses to opioids in binge-eating rats. Behav Neurosci. 2005;119:1207–1214. doi: 10.1037/0735-7044.119.5.1207. [DOI] [PubMed] [Google Scholar]
- 107.Corwin RL. Bingeing rats: a model of intermittent excessive behavior? Appetite. 2006;46:11–15. doi: 10.1016/j.appet.2004.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Liang NC, Hajnal A, Norgern R. Sham feeding corn oil increases accumbens dopamine in the rat. Am J Physiol Regul Integr Comp Physiol. 2006;291:R1236–R1239. doi: 10.1152/ajpregu.00226.2006. [DOI] [PubMed] [Google Scholar]
- 109.De Souza CT, Araujo EP, Bordin S, et al. Consumption of a fat-rich diet activates a proinflammatory response and induces insulin resistance in the hypothalamus. Endocrinology. 2005;146:4192–4199. doi: 10.1210/en.2004-1520. [DOI] [PubMed] [Google Scholar]
- 110.Milanski M, Degasperi G, Coope A, et al. Saturated fatty acids produce an inflammatory response predominantly through the activation of TLR4 signaling in hypothalamus: implications for the pathogenesis of obesity. J Neurosci. 2009;29:359–370. doi: 10.1523/JNEUROSCI.2760-08.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Milanski M, Arruda AP, Coope A, et al. Inhibition of hypothalamic inflammation reverses diet-induced insulin resistance in the liver. Diabetes. 2012;61:1455–1462. doi: 10.2337/db11-0390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Arruda AP, Milanski M, Coope A, et al. Low-grade hypothalamic inflammation leads to defective thermogenesis, insulin resistance, and impaired insulin secretion. Endocrinology. 2011;152:1314–1326. doi: 10.1210/en.2010-0659. [DOI] [PubMed] [Google Scholar]
- 113.Calegari VC, Torsoni AS, Vanzela EC, et al. Inflammation of the hypothalamus leads to defective pancreatic islet function. J Biol Chem. 2011;286:12870–12880. doi: 10.1074/jbc.M110.173021. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 114.Clegg DJ, Gotoh K, Kemp C, et al. Consumption of a high-fat diet induces central insulin resistance independent of adiposity. Physiol Behav. 2011;103:10–16. doi: 10.1016/j.physbeh.2011.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Benoit SC, Kemp CJ, Elias CF, et al. Palmitic acid mediates hypothalamic insulin resistance by altering PKC-theta subcellular localization in rodents. J Clin Invest. 2009;119:2577–2589. doi: 10.1172/JCI36714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Ryan KK, Woods SC, Seeley RJ. Central nervous system mechanisms linking the consumption of palatable high-fat diets to the defense of greater adiposity. Cell Metab. 2012;15:137–149. doi: 10.1016/j.cmet.2011.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Thaler JP, Yi CX, Schur EA, et al. Obesity is associated with hypothalamic injury in rodents and humans. J Clin Invest. 2012;122:153–162. doi: 10.1172/JCI59660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Zhang X, Zhang G, Zhang H, et al. Hypothalamic IKKbeta/NF-kappaB and ER stress link overnutrition to energy imbalance and obesity. Cell. 2008;135:61–73. doi: 10.1016/j.cell.2008.07.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Posey KA, Clegg DJ, Printz RL, et al. Hypothalamic proinflammatory lipid accumulation, inflammation, and insulin resistance in rats fed a high-fat diet. Am J Physiol Endocrinol Metab. 2009;296:E1003–E1012. doi: 10.1152/ajpendo.90377.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Rother E, Kuschewski R, Alcazar MA, et al. Hypothalamic JNK1 and IKKbeta activation and impaired early postnatal glucose metabolism after maternal perinatal high-fat feeding. Endocrinology. 2012;153:770–781. doi: 10.1210/en.2011-1589. [DOI] [PubMed] [Google Scholar]
- 121.Cintra DE, Ropelle ER, Moraes JC, et al. Unsaturated fatty acids revert diet-induced hypothalamic inflammation in obesity. PLoS ONE. 2012;7:e30571. doi: 10.1371/journal.pone.0030571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Gupta S, Knight AG, Keller JN, et al. Saturated long-chain fatty acids activate inflammatory signaling in astrocytes. J Neurochem. 2012;120:1060–71. doi: 10.1111/j.1471-4159.2012.07660.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.de La Serre CB, Ellis CL, Lee J, et al. Propensity to high-fat diet-induced obesity in rats is associated with changes in the gut microbiota and gut inflammation. Am J Physiol Gastrointest Liver Physiol. 2010;299:G440–G448. doi: 10.1152/ajpgi.00098.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Mohammed N, Tang L, Jahangiri A, et al. Elevated IgG levels against specific bacterial antigens in obese patients with diabetes and in mice with diet-induced obesity and glucose intolerance. Metabolism. 2012 doi: 10.1016/j.metabol.2012.02.007. Epublication ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Lam YY, Ha CW, Campbell CR, et al. Increased gut permeability and microbiota change associate with mesenteric fat inflammation and metabolic dysfunction in diet-induced obese mice. PLoS ONE. 2012;7:e34233. doi: 10.1371/journal.pone.0034233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Henao-Mejia J, Elinav E, Jin C, et al. Inflammasome-mediated dysbiosis regulates progression of NAFLD and obesity. Nature. 2012;482:179–185. doi: 10.1038/nature10809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Elinav E, Strowig T, Kau AL, et al. NLRP6 inflammasome regulates colonic microbial ecology and risk for colitis. Cell. 2011;145:745–757. doi: 10.1016/j.cell.2011.04.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Harris K, Kassis A, Major G, et al. Is the gut microbiota a new factor contributing to obesity and its metabolic disorders? J Obes. 2012;2012 doi: 10.1155/2012/879151. 879151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Vijay-Kumar M, Gewirtz AT. Is predisposition to NAFLD and obesity communicable? Cell Metab. 2012;15:419–420. doi: 10.1016/j.cmet.2012.03.013. [DOI] [PubMed] [Google Scholar]
- 130.Paulino G, Barbier de la Serre C, Knotts TA, et al. Increased expression of receptors for orexigenic factors in nodose ganglion of diet-induced obese rats. Am J Physiol Endocrinol Metab. 2009;296:E898–E903. doi: 10.1152/ajpendo.90796.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.de Lartigue G, Barbier de la Serre C, Espero E, et al. Diet-induced obesity leads to the development of leptin resistance in vagal afferent neurons. Am J Physiol Endocrinol Metab. 2011;301:E187–E195. doi: 10.1152/ajpendo.00056.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Donovan MJ, Paulino G, Raybould HE. Activation of hindbrain neurons in response to gastrointestinal lipid is attenuated by high fat, high energy diets in mice prone to diet-induced obesity. Brain Res. 2009;1248:136–140. doi: 10.1016/j.brainres.2008.10.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Nefti W, Chaumontet C, Fromentin G, et al. A highfat diet attenuates the central response to within-meal satiation signals and modifies the receptor expression of vagal afferents in mice. Am J Physiol Regul Integr Comp Physiol. 2009;296:R1681–R1686. doi: 10.1152/ajpregu.90733.2008. [DOI] [PubMed] [Google Scholar]
- 134.Kentish S, Li H, Philp LK, O’Donnell TA, et al. Diet-induced adaptation of vagal afferent function. J Physiol. 2012;590:209–221. doi: 10.1113/jphysiol.2011.222158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Daly DM, Park SJ, Valinsky WC, et al. Impaired intestinal afferent nerve satiety signalling and vagal afferent excitability in diet induced obesity in the mouse. J Physiol. 2011;589:2857–2870. doi: 10.1113/jphysiol.2010.204594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Garland T, Jr, Schutz H, Chappell MA, et al. The biological control of voluntary exercise, spontaneous physical activity and daily energy expenditure in relation to obesity: human and rodent perspectives. J Exp Biol. 2011;214:206–229. doi: 10.1242/jeb.048397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Bostrom P, Wu J, Jedrychowski MP, et al. A PGC1-alpha-dependent myokine that drives brown-fat-like development of white fat and thermogenesis. Nature. 2012;481:463–468. doi: 10.1038/nature10777. [DOI] [PMC free article] [PubMed] [Google Scholar]