Abstract
Background
There is increasing complexity in the management of patients with acute severe exacerbation of inflammatory bowel disease (IBD; Crohn’s disease (CD), ulcerative colitis (UC)) with frequent requirement for urgent surgery.
Aim
To determine whether a weekend effect exists for IBD care in the United States.
Methods
We used data from the Nationwide Inpatient Sample (NIS) 2007, the largest all-payer hospitalization database in the United States. Discharges with a diagnosis of CD or UC who underwent urgent intestinal surgery within 2 days of hospitalization were identified using the appropriate ICD-9 codes. The independent effect of admission on a weekend was examined using multivariate logistic regression adjusting for potential confounders.
Results
Our study included 7,112 urgent intestinal surgeries in IBD patients, 21% of which occurred following weekend admissions. There was no difference in disease severity between weekend and weekday admissions. Post-operative complications were more common following weekend than weekday hospitalizations in UC (odds ratio (OR) 1.71, 95% confidence interval (CI) 1.01–2.90). The most common post-operative complication was post-operative infections (Weekend 30% vs. weekday 20%, p=0.04). The most striking difference between weekend and weekday hospitalizations was for need for repeat laparotomy (OR 11.5), mechanical wound complications (OR 10.03) and pulmonary complications (OR 2.22). In contrast, occurrence of any post-operative complication in CD was similar between weekday and weekend admissions.
Conclusion
Patients with UC hospitalized on a weekend undergoing urgent surgery within 2 days have an increased risk for post-operative complications, in particular mechanical wound complications, need for repeat laparotomy, and post-operative infections.
Keywords: weekend effect, post-operative complications, Crohn’s disease, ulcerative colitis
INTRODUCTION
The weekend effect is the well-described phenomenon of worse outcomes for patients hospitalized on a weekend compared to a weekday1, 2. Such an effect has been demonstrated for a spectrum of medical and surgical illnesses ranging from gastrointestinal bleeding, myocardial infarction, abdominal aortic aneurysm, and pulmonary embolism1–6. However, this effect may not exist across all healthcare systems7, 8 and may in part relate to the greater severity of patients who present to the hospital on a weekend, potentially representing delayed seeking of care5, 9. In addition, the weekend effect could also be related to availability of specialist expertise, as many of the conditions for which a weekend effect has been demonstrated often require the input of specialist consultants or procedures1–3, 7, 10 while lower complexity illnesses may demonstrate an attenuated or non-significant weekend effect11.
Inflammatory bowel diseases (IBD; Crohn’s disease (CD), ulcerative colitis (UC)) are chronic inflammatory diseases of the intestine that often require hospitalizations for medical management or surgery12. Indeed, nearly one-fifth of UC patients and half of patients with CD will require at least one surgery in the management of their disease12–16. Often, many of these surgeries occur following an urgent or emergent hospitalization for a disease flare, such hospitalizations being associated with an increased risk of postoperative morbidity and mortality17, 18. There is also growing recognition of practice variation in the management of these patients, with higher volume hospitals demonstrating lower mortality and morbidity following IBD-related hospitalizations, particularly those that require surgery17–19.
There is increasing complexity in the management of IBD patients and often the pressing need for multi-disciplinary medical and surgical expertise for patients with an acute severe flare requiring urgent surgery. Consequently, we performed this study using a nationwide population-based database of hospitalizations to examine whether weekend hospitalizations are associated with an increased incidence of post-operative mortality or morbidity following urgent intestinal surgery in CD and UC.
METHODS
Data Source
The data source for our study was the Nationwide Inpatient Sample (NIS) 2007. The NIS is the largest all-payer inpatient hospitalization database in the United States and is maintained by the Agency for Healthcare Research and Quality (AHRQ)20. Using a stratified sample survey design, the NIS contains all hospitalizations from a 20% stratified random sample of hospitalizations from all participating states. For the year 2007, the NIS included nearly 1,000 hospitals from 37 states covering over 8 million discharges. Each hospitalization is coded with one primary diagnosis upon discharge, up to 14 secondary diagnoses and 15 procedures associated with the hospitalization using International Classification of Diseases, 9th edition, clinical modification (ICD-9-CM) disease codes. The NIS correlates well with other hospitalization databases in the United States and has been extensively used for research including on IBD.
Study Cohort and Variables
Our primary study population comprised of all individuals hospitalized with a primary or secondary discharge diagnosis of CD (ICD-9-CM 555.x) or UC (ICD-9-CM 556.x). Each discharge is designated as a weekday (Monday-Friday) or weekend (Saturday-Sunday) hospitalization based on the date of admission. First, we compared the characteristics of all patients admitted on a weekend compared to a weekday (Table 1). As it is intuitive that a weekend hospitalization is of the greatest relevance among patients of the highest acuity who undergo the intervention of interest also during the weekend or soon thereafter, we further refined our cohort to include only those patients who underwent urgent intestinal surgery using the appropriate ICD-9 CM codes (Supplementary Table 1). Each hospitalization is further coded as elective, urgent, or emergent as was as if the admission source was a transfer from another hospital. For each procedure, the NIS indicates the timing of the procedure in relation to date of admission. Our primarily analysis included non-elective hospitalizations where the intestinal surgery occurred within 2 days of hospitalization (“urgent intestinal surgery”) (Figure 1).
Table 1.
Characteristics of the all primary inflammatory bowel disease hospitalizations, stratified by weekend admission status
| Parameter | Weekend Hospitalization (n = 5,623) % | Weekday hospitalization (n = 65,241) % | p-value |
|---|---|---|---|
| Age (in years) | 0.11 | ||
| 18 – 35 | 35 | 35 | |
| 36 – 50 | 29 | 29 | |
| 51 – 65 | 19 | 20 | |
| 66 and older | 17 | 16 | |
| Female | 55 | 56 | 0.39 |
| Charlson score | 0.12 | ||
| 0 | 74 | 74 | |
| 1 | 17 | 17 | |
| 2 | 5 | 6 | |
| 3 or more | 4 | 3 | |
| IBD type | |||
| Ulcerative colitis | 38 | 39 | 0.11 |
| Crohn’s disease | 62 | 61 | |
| Anemia | 27 | 28 | 0.56 |
| Malnutrition | 5.0 | 5.9 | 0.02 |
| Blood transfusion | 9.1 | 10.6 | 0.01 |
| Parenteral nutrition | 3.7 | 5.5 | < 0.001 |
| Clostridium difficile infection | 2.2 | 1.8 | 0.11 |
| Smoking | 20.8 | 20.1 | 0.44 |
| Any bowel surgery (non-elective) | 7.3 | 9.3 | 0.001 |
| Urgent bowel surgery (within 2 days) | 2.8 | 2.9 | 0.68 |
| Died | 0.4 | 0.6 | 0.17 |
IBD – Inflammatory bowel disease
Figure 1.
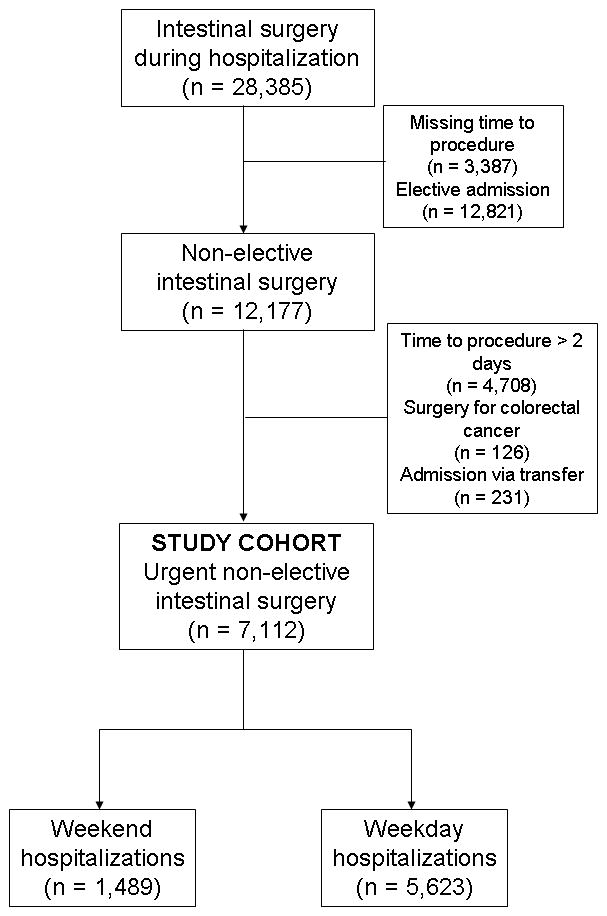
Derivation of the study cohort of patients with inflammatory bowel disease undergoing urgent intestinal surgery within 2 days of hospitalization
We extracted age, gender, race, zip code level income, and hospital characteristics (bedsize, teaching hospital) from the database. General co-morbidity was quantified using the Deyo modification of the Charlson score, a widely accepted and used measure21, 22. For disease-specific co-morbidity we used indicators that we had previously shown to be important in determining severity of hospitalized CD and UC patients, namely anemia, malnutrition, total parenteral nutrition, need for blood transfusion, and occurrence of Clostridium difficile (C difficile) infection23, 24.
Outcomes
Our primary outcomes were post-operative morbidity defined as the occurrence of any post-operative complication. This was further subdivided into specific post-operative complications which included infections, cardiovascular, pulmonary, gastrointestinal, or urinary complications, and surgery-specific complications such as mechanical wound complications and need for repeat laparotomy (Supplementary Table 1)10, 17, 18. Our secondary outcomes included post-operative mortality, length of stay, and total hospitalization charges.
Statistical Analysis
Data were analyzed with Stata Intercooled 11.0 (StataCorp, College Station, TX) using the appropriate survey commands and survey weights provided within the NIS. Continuous variables were summarized using means and standard deviations with the use of proportions for categorical variables. The chi-square test was used to compare categorical variables; the t-test was used for the continuous variables. Univariate logistic regression was performed with weekend hospitalization as the main predictor variable. Those that achieved statistical significance at p < 0.05 in this model were included in the final multivariate model that adjusted for potential confounders. All p-values were two-sided and significant when ≤ 0.05. The study was approved by the Institutional Review Board of Partners Healthcare.
RESULTS
Study Cohort
Table 1 presents a comparison of all hospitalizations with a primary diagnosis of CD or UC, stratified by admission on a weekend. Weekend and weekday hospitalizations were not different with respect to age, gender, or co-morbidity distribution. Weekday admissions were slightly more likely to require blood transfusion, parenteral nutrition, and any bowel surgery (excluding elective admissions for surgery). There was no difference in undergoing urgent surgery within 2 days of hospitalization, or in-hospital death between both groups.
An estimated 28,385 patients with a diagnosis of CD or UC underwent intestinal surgery during hospitalization. Figure 1 depicts the flow of the study cohort. After excluding patients with missing time to procedure or who were coded as having elective admissions, we were left with 12,177 non-elective admissions resulting in intestinal surgery. After excluding patients who were also diagnosed as having colorectal cancer, admitted via transfer from another hospital, or those who had surgery > 2 days after admission, we were left with a final study cohort of 7,112 urgent non-elective intestinal surgeries in IBD patients. Among these, 1,489 occurred following a weekend hospitalization (21%) while the remaining 5,623 (79%) were following weekday hospitalizations.
Table 2 compares the characteristics of patients admitted on a weekend and weekday who underwent urgent intestinal surgery. There was no significant difference in age, gender or Charlson co-morbidity score between the two groups. Nearly three-quarters of patients in each group had a diagnosis of Crohn’s disease. Disease-specific co-morbidity – anemia, malnutrition, need for blood transfusion, or parenteral nutrition -was also not different between the two groups. An estimated 5% of weekend and 4% of weekday hospitalizations resulting in urgent surgery had a diagnosis of C difficile infection.
Table 2.
Characteristics of IBD patients undergoing urgent intestinal surgery within 2 days of hospitalization
| Parameter | Weekend Hospitalization (n = 1,489) % | Weekday hospitalization (n = 5,623) % | p-value |
|---|---|---|---|
| Age (in years) | 0.31 | ||
| 18 – 35 | 29 | 32 | |
| 36 – 50 | 32 | 27 | |
| 51 – 65 | 20 | 23 | |
| 66 and older | 19 | 18 | |
| Female | 49 | 53 | 0.33 |
| Charlson score | 0.51 | ||
| 0 | 72 | 72 | |
| 1 | 13 | 16 | |
| 2 | 6 | 5 | |
| 3 or more | 9 | 7 | |
| IBD type | 0.70 | ||
| Ulcerative colitis | 27 | 26 | |
| Crohn’s disease | 73 | 74 | |
| Anemia | 25 | 25 | 0.94 |
| Malnutrition | 7 | 8 | 0.49 |
| Blood transfusion | 13 | 15 | 0.57 |
| Parenteral nutrition | 10 | 13 | 0.17 |
| Clostridium difficile infection | 5 | 4 | 0.50 |
| Smoking | 20 | 20 | 0.81 |
IBD – Inflammatory bowel disease
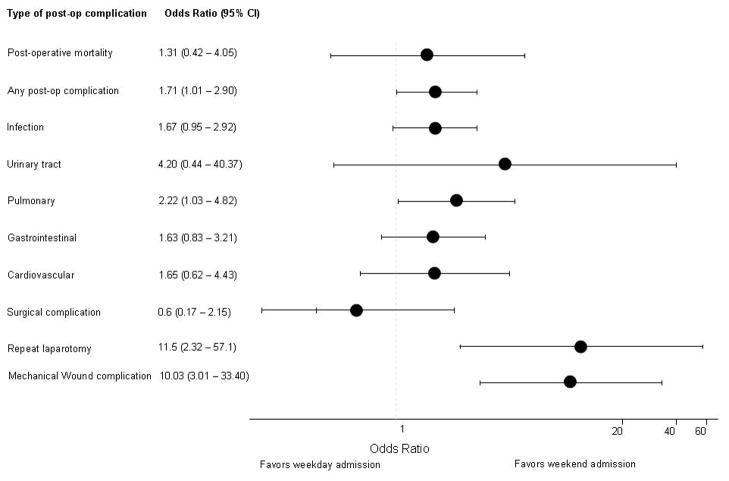
Post-operative complications in ulcerative colitis
Post-operative mortality following urgent intestinal surgery occurred in 7% of weekend compared to 6% of weekday hospitalizations for ulcerative colitis (p=0.64) (Table 3). In contrast, post-operative morbidity was more common in weekend (56%) compared to weekday (42%, p=0.03) hospitalizations. Adjusting for potential confounders, this difference persisted on multivariate analysis (odds ratio (OR) 1.71, 95% confidence interval 1.01 – 2.90) (Figure 2). The most common post-operative complications were post-operative infections, occurring in 30% of weekend and 20% of weekday hospitalizations after urgent intestinal surgery (p=0.04); this difference was slightly attenuated on multivariate analysis (OR 1.71, 95% CI 0.95 – 2.92). The most striking difference between weekend and weekday hospitalizations were for need for repeat laparotomy (OR 11.5, 95% CI 2.32 – 57.1), mechanical wound complications (OR 10.03, 95% CI 3.01 – 33.40), and pulmonary complications (OR 2.22, 95% CI 1.03 – 4.82) while there was no difference in cardiovascular, gastrointestinal or urinary complications. There was also no difference in the rates of undergoing a stoma procedure for an urgent surgery following weekend compared to weekday hospitalizations (30% vs. 32%, p=0.65). There was also no difference in the overall length of stay or hospitalization charges.
Table 3.
Post-operative complications following urgent intestinal surgery for ulcerative colitis
| Parameter | Weekend Hospitalization (n = 372) % | Weekday hospitalization (n = 1,388) % | p-value |
|---|---|---|---|
| Post-operative mortality | 7 | 6 | 0.64 |
| Any post-operative complication | 56 | 42 | 0.03 |
| Specific complications | |||
| Infectious | 30 | 20 | 0.04 |
| Mechanical wound | 12 | 2 | 0.0001 |
| Urinary | 3 | 1 | 0.14 |
| Gastrointestinal | 16 | 12 | 0.23 |
| Pulmonary | 24 | 13 | 0.04 |
| Cardiovascular | 10 | 6 | 0.24 |
| Surgical complication | 5 | 8 | 0.48 |
| Repeat laparotomy | 6 | 1 | 0.008 |
| Length of stay (mean) | 9.5 days | 11.4 days | 0.12 |
| Hospitalization charges (mean) | $ 69,612 | $ 89,920 | 0.06 |
Figure 2. Multivariate† analysis of post-operative complications following urgent intestinal surgery for ulcerative colitis.
† Adjusted for age, gender, Charlson co-morbidity index, hospital bed-size and teaching status, and zip code level income
Among all urgent surgeries, 43% occurred on the day of hospitalization, 35% on day 1, and 21% on day 2. This distribution was not statistically different between weekday and weekend hospitalizations (p=0.42). Hospitalization day of surgery did not influence post-operative outcomes. Excluding patients who may have undergone surgery on day 2 of hospitalizations (i.e. potentially accounting for Saturday or Sunday admissions admitted on a weekend but operated on a weekday), our findings of increased any post-operative complications (OR 1.74, 95% CI 1.00 – 3.10), pulmonary complications (OR 3.46, 95% CI 1.43 – 8.38), mechanical wound complications (OR 5.71, 95% CI 1.55 – 21.04), or repeat laparotomy (OR 8.45, 95% CI 1.51 – 47.32) remained, supporting the robustness of our findings. The effect sizes for any postoperative complication (OR 1.67), pulmonary complications (OR 1.78), mechanical wound complications (OR 3.08), and repeat laparotomy (OR 5.32) were slightly attenuated when the definition for surgery was expanded to include those occurring within 4 days of admission. There was no statistically significant interaction between hospital teaching status, size, location, and geographic region and weekend admission status in influencing patient outcomes (p > 0.10 for all). Expanding our analysis to all surgeries indicated that both weekend hospitalization (OR 1.61, 95% CI 1.20 – 2.14) and urgent / emergent admission (OR 1.79, 95% CI 1.44 – 2.22) were independently associated with post-operative complications.
Post-operative complications in Crohn’s disease
In contrast to the findings for UC, both post-operative mortality and overall occurrence of any post-operative complication was less frequent in CD and similar between weekday and weekend admissions (Table 3). There was a lower rate of postoperative infections for CD patients hospitalized on the weekend, but a trend towards a higher rate of cardiovascular complications post-operatively (OR 2.26, 95% CI 0.91 – 5.52) (Figure 3). Unlike results observed in UC, there was also no difference in repeat laparotomy or mechanical wound complications between weekend and weekday hospitalizations for CD. Requirement for a stoma was uncommon among both weekend (10%) and weekday (8%, p = 0.57) hospitalizations. Similar to that observed for UC, three-quarters of all surgery occurred on days 0 or 1 of hospitalization, with similar distribution between weekend and weekday hospitalizations. Hospitalization day of surgery did not influence patient outcomes. In an analysis including all bowel surgeries, only emergent / urgent admission status (OR 1.26, 95% CI 1.08 – 1.45) but not weekend admission (OR 1.10, 95% CI 0.94 – 1.36) was predictive of occurrence of any postoperative complication.
Figure 3. Multivariate† analysis of post-operative complications following urgent intestinal surgery for Crohn’s disease.
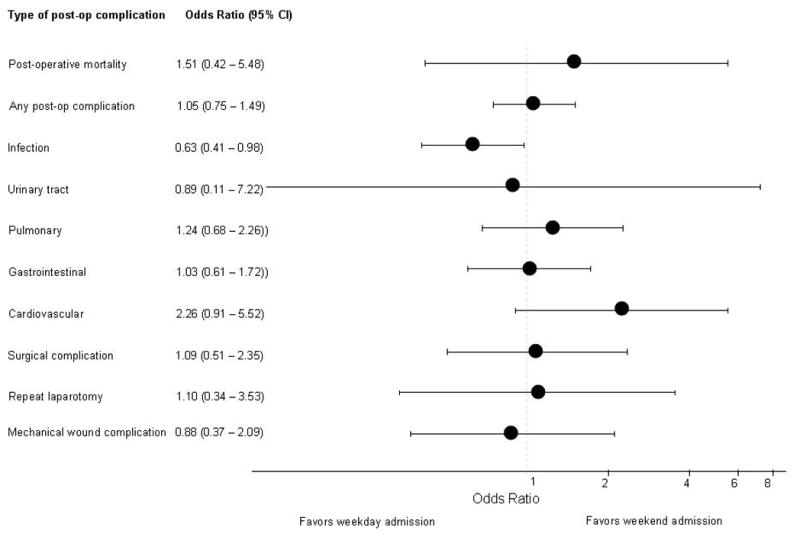
† Adjusted for age, gender, Charlson co-morbidity index, hospital bed-size and teaching status, and zip code level income
DISCUSSION
The effect of weekend hospitalizations have been examined for a number of different conditions with many studies suggesting increased mortality and morbidity among such patients1, 2, 5. However, most conditions where this effect has been demonstrated have involved high complexity medical or surgical illnesses, or relatively less frequent diagnoses requiring specialist care. For conditions that are common or have low complexity, there may be only an attenuated weekend effect1, 3–6, 10, 11. In this analysis using a nationwide hospitalization database, we demonstrated an increased incidence of post-operative complications among UC patients hospitalized on a weekend who require urgent intestinal surgery within 2 days. There was no similar effect for CD.
Several plausible reasons for the weekend effect have been postulated and explored. These could include patient related factors with many seeking care on a weekend delaying their presentation to a healthcare facility during the work week or requiring urgent care on the weekend due to severity of disease5. We did not find evidence of this in our study as measured using several markers of disease-specific co-morbidity such as anemia, malnutrition, or need for transfusions. Indeed, among all primary IBD hospitalizations, markers of disease severity were greater on weekday compared to weekend admissions. More attention has been focused on provider and institution factors including weekend staffing, ratio of patients to nurses or physicians, and on-site or on-call availability of expertise for complex illnesses and surgical procedures. However, it is likely, given the spectrum of conditions for which a weekend effect has been demonstrated, that the reason behind it is multifactorial. Within the context of our study, the lack of individual provider identification in the NIS precluded our being able to examine whether the differences observed for weekend hospitalizations and emergent surgery outcomes was related to individual surgeon volume, surgeon training (general surgeon or colorectal surgeon), or non-surgical factors related to medical optimization and other supportive care involved in the management of these patients. However, given that our strongest effects were for complications that related to the surgical procedure, namely need for repeat laparotomy and post-operative mechanical wound complications with a trend towards increased risk for post-operative infections, it is likely that factors directly related to the surgery play a stronger role in the weekend effect we identified for IBD patients. The exact reason for the lower rate of postoperative infectious complications in CD patients admitted on a weekend is unclear. First, it is possible that this contrast with what we observed for UC could be due to the different surgical operations that are performed for acute exacerbations of CD compared to UC. It is possible that provider (surgical and non-surgical experience) plays a different role in the management of CD and UC such that weekend hospitalization may not be an important determinant of patient outcomes among hospitalized CD patients. Unmeasured confounders beyond what we were able to capture in our study could also influence the estimates.
Considerable interest exists regarding the impact of specialist care and practice variation in the management of IBD. An early study using the Nationwide Inpatient Sample by Kaplan et al. demonstrated that emergent hospitalization and undergoing a colectomy at a low-volume hospital were associated with an increased post-operative mortality18. Expanding the analysis to CD, Nguyen et al. and our group have also previously demonstrated a similar association with hospital volume for CD, with a greater effect among those undergoing surgery during the hospitalization17, 19. There is increasing complexity in the management of patients with severe CD and UC, particularly in the acutely ill setting. However, early ambulatory gastroenterologist care may improve outcomes in IBD patients, thereby suggesting the need for specialist input and expertise25, 26. Furthermore, hospitalized UC patients also demonstrated improved outcomes when admitted under a specialist compared to a generalist27.
To our knowledge, there is no prior literature directly examining this effect in patients with IBD. However, our findings are consistent with a study by Worni et al. who found higher rates of overall post-operative complications among weekend hospitalizations for diverticulitis undergoing surgery10. Similar to the results in our study, this effect was pronounced for mechanical wound complications and need for repeat laparotomy, with only a modest increase in post-operative cardiovascular complications. In contrast, the same group examined whether there is a weekend effect for a less complex diagnosis, namely appendicitis, and found no difference in the overall rate of post-operative complications among weekend hospitalizations11.
Our study has a few implications. The identification of a weekend effect for urgent IBD-related surgery in UC patients suggests a need for more systematic study regarding the mechanisms behind such an effect, and replication of our findings in different health care systems. Given the strength of association was greater for postoperative complications directly related to the surgical procedure, there is need to further examine whether surgeon experience and volume play an important role in determining short- and long-term outcomes after increasingly complex urgent IBD-related surgery. If such is the case, then one must consider whether availability of specialist expertise needs to be factored into the decision making regarding the appropriate timing of surgery when possible. In addition, it is also necessary to further study the impact of medical optimization prior to surgery, such as minimizing exposure to corticosteroids or narcotics if possible, both of which have been linked to adverse outcomes in IBD patients28, and management of nutritional status and immunosuppression which could all impact post-surgical outcomes. Variations in such non-surgery related measures between weekends and weekdays could also result in differences in post-surgical outcomes. In addition, consistent with the ongoing focus on practice standardization and quality improvement in the management of IBD, with the growing panoply of therapeutic options available, there is need for ongoing study on the impact of specialist expertise and experience on patient outcomes.
We readily acknowledge several limitations to our study. First, the NIS is a de-identified administrative database making it impossible to validate individual ICD-9 codes. Nevertheless, the codes for CD and UC have demonstrated good positive predictive value29, and prior studies using administrative data for analysis of postoperative complications have relied on similar codes to those used in our study, and have arrived at results consistent with that observed using individual patient level data18, 30, 31. Second, as discussed above, we did not have information on individual provider level details which would be important to examine further. Several studies have suggested a correlation between hospitalization volume and surgical outcomes in patients with IBD. Furthermore, early specialist care has also been associated with superior outcomes in hospitalized UC patients27. We did not observe a statistically significant interaction between any of the hospital characteristics and weekend admission status in determining patient outcomes suggesting generalizability to our results across different patient care settings and likely both specialist and generalist care. We also did not have information on potentially important medications and laboratory values; nevertheless rough estimates of these where possible using ICD-9 codes did not reveal a difference in severity between weekday and weekend hospitalizations. While weekend admission may not always imply weekend surgical intervention, that over three-quarters of the patients were operated on day 0 or 1 of hospitalizations suggests that this was frequently the case. Furthermore, any bias introduced by misclassification of weekend hospitalizations operated on a weekday is likely to bias our results towards the null, suggesting that our estimates are conservative. Finally, since the NIS does not contain a unique person-level identifier, we were unable to determine whether an individual was hospitalized more than once in the database.
In conclusion, we identify a weekend effect following urgent intestinal surgery for UC whereby such patients were more likely to develop post-operative complications, in particular mechanical wound complications and the need for repeat laparotomy. Further studies examining the mechanism behind such an association are required to institute the appropriate interventions, be it medical optimization, wider availability of surgical expertise, or supportive staffing measures, in order to ensure optimal patient outcomes regardless of the day of hospitalization.
Supplementary Material
Table 4.
Post-operative complications following urgent intestinal surgery for Crohn’s disease
| Parameter | Weekend Hospitalization (n = 1,117) % | Weekday hospitalization (n = 4,235) % | p-value |
|---|---|---|---|
| Post-operative mortality | 2 | 1 | 0.61 |
| Any post-operative complication | 35 | 34 | 0.91 |
| Specific complications | |||
| Infectious | 10 | 16 | 0.03 |
| Mechanical wound | 4 | 5 | 0.62 |
| Urinary | 1 | 1 | 0.86 |
| Gastrointestinal | 15 | 15 | 0.94 |
| Pulmonary | 7 | 6 | 0.50 |
| Cardiovascular | 4 | 2 | 0.11 |
| Surgical complication | 4 | 4 | 0.90 |
| Repeat laparotomy | 2 | 2 | 0.92 |
| Length of stay (mean) | 7.4 days | 8.2 days | 0.12 |
| Hospitalization charges (mean) | $ 45,225 | $49,600 | 0.26 |
Acknowledgments
Source of funding: Ananthakrishnan is supported in part by a grant from the National Institutes of Health (K23 DK097142)
Footnotes
Conflicts of interest: None
Author contributions: Ananthakrishnan - study concept and design, analysis and interpretation, drafting of the manuscript; McGinley – obtained data for analysis, critical revision and approval of final manuscript.
References
- 1.Bell CM, Redelmeier DA. Mortality among patients admitted to hospitals on weekends as compared with weekdays. N Engl J Med. 2001;345:663–8. doi: 10.1056/NEJMsa003376. [DOI] [PubMed] [Google Scholar]
- 2.Cram P, Hillis SL, Barnett M, Rosenthal GE. Effects of weekend admission and hospital teaching status on in-hospital mortality. Am J Med. 2004;117:151–7. doi: 10.1016/j.amjmed.2004.02.035. [DOI] [PubMed] [Google Scholar]
- 3.Ananthakrishnan AN, McGinley EL, Saeian K. Outcomes of weekend admissions for upper gastrointestinal hemorrhage: a nationwide analysis. Clin Gastroenterol Hepatol. 2009;7:296–302e1. doi: 10.1016/j.cgh.2008.08.013. [DOI] [PubMed] [Google Scholar]
- 4.Barnett MJ, Kaboli PJ, Sirio CA, Rosenthal GE. Day of the week of intensive care admission and patient outcomes: a multisite regional evaluation. Med Care. 2002;40:530–9. doi: 10.1097/00005650-200206000-00010. [DOI] [PubMed] [Google Scholar]
- 5.Freemantle N, Richardson M, Wood J, Ray D, Khosla S, Shahian D, Roche WR, Stephens I, Keogh B, Pagano D. Weekend hospitalization and additional risk of death: an analysis of inpatient data. J R Soc Med. 2012;105:74–84. doi: 10.1258/jrsm.2012.120009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shaheen AA, Kaplan GG, Myers RP. Weekend versus weekday admission and mortality from gastrointestinal hemorrhage caused by peptic ulcer disease. Clin Gastroenterol Hepatol. 2009;7:303–10. doi: 10.1016/j.cgh.2008.08.033. [DOI] [PubMed] [Google Scholar]
- 7.Jairath V, Kahan BC, Logan RF, Hearnshaw SA, Travis SP, Murphy MF, Palmer KR. Mortality from acute upper gastrointestinal bleeding in the United kingdom: does it display a “weekend effect”? Am J Gastroenterol. 2011;106:1621–8. doi: 10.1038/ajg.2011.172. [DOI] [PubMed] [Google Scholar]
- 8.Nahon S, Pariente A, Latrive JP. Weekend admission does not influence the mortality of upper gastrointestinal bleeding caused by peptic ulcers: results of a French prospective study of the association nationale des gastroenterologues des hopitaux generaux group. Clin Gastroenterol Hepatol. 2009;7:911. doi: 10.1016/j.cgh.2009.03.018. author reply 912. [DOI] [PubMed] [Google Scholar]
- 9.Mikulich O, Callaly E, Bennett K, O’Riordan D, Silke B. The increased mortality associated with a weekend emergency admission is due to increased illness severity and altered case-mix. Acute Med. 2011;10:182–7. [PubMed] [Google Scholar]
- 10.Worni M, Schudel IM, Ostbye T, Shah A, Khare A, Pietrobon R, Thacker JK, Guller U. Worse outcomes in patients undergoing urgent surgery for left-sided diverticulitis admitted on weekends vs weekdays: a population-based study of 31 832 patients. Arch Surg. 2012;147:649–55. doi: 10.1001/archsurg.2012.825. [DOI] [PubMed] [Google Scholar]
- 11.Worni M, Ostbye T, Gandhi M, Rajgor D, Shah J, Shah A, Pietrobon R, Jacobs DO, Guller U. Laparoscopic appendectomy outcomes on the weekend and during the week are no different: a national study of 151,774 patients. World J Surg. 2012;36:1527–33. doi: 10.1007/s00268-012-1550-z. [DOI] [PubMed] [Google Scholar]
- 12.Bernstein CN, Loftus EV, Jr, Ng SC, Lakatos PL, Moum B. Hospitalisations and surgery in Crohn’s disease. Gut. 2012;61:622–9. doi: 10.1136/gutjnl-2011-301397. [DOI] [PubMed] [Google Scholar]
- 13.Cosnes J, Nion-Larmurier I, Beaugerie L, Afchain P, Tiret E, Gendre JP. Impact of the increasing use of immunosuppressants in Crohn’s disease on the need for intestinal surgery. Gut. 2005;54:237–41. doi: 10.1136/gut.2004.045294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ramadas AV, Gunesh S, Thomas GA, Williams GT, Hawthorne AB. Natural history of Crohn’s disease in a population-based cohort from Cardiff (1986–2003): a study of changes in medical treatment and surgical resection rates. Gut. 2010;59:1200–6. doi: 10.1136/gut.2009.202101. [DOI] [PubMed] [Google Scholar]
- 15.Targownik LE, Singh H, Nugent Z, Bernstein CN. The epidemiology of colectomy in ulcerative colitis: results from a population-based cohort. Am J Gastroenterol. 2012;107:1228–35. doi: 10.1038/ajg.2012.127. [DOI] [PubMed] [Google Scholar]
- 16.Williet N, Pillot C, Oussalah A, Billioud V, Chevaux JB, Bresler L, Bigard MA, Gueant JL, Peyrin-Biroulet L. Incidence of and impact of medications on colectomy in newly diagnosed ulcerative colitis in the era of biologics. Inflamm Bowel Dis. 2012;18:1641–6. doi: 10.1002/ibd.21932. [DOI] [PubMed] [Google Scholar]
- 17.Ananthakrishnan AN, McGinley EL, Binion DG. Does it matter where you are hospitalized for inflammatory bowel disease? A nationwide analysis of hospital volume. Am J Gastroenterol. 2008;103:2789–98. doi: 10.1111/j.1572-0241.2008.02054.x. [DOI] [PubMed] [Google Scholar]
- 18.Kaplan GG, McCarthy EP, Ayanian JZ, Korzenik J, Hodin R, Sands BE. Impact of hospital volume on postoperative morbidity and mortality following a colectomy for ulcerative colitis. Gastroenterology. 2008;134:680–7. doi: 10.1053/j.gastro.2008.01.004. [DOI] [PubMed] [Google Scholar]
- 19.Nguyen GC, Steinhart AH. Nationwide patterns of hospitalizations to centers with high volume of admissions for inflammatory bowel disease and their impact on mortality. Inflamm Bowel Dis. 2008;14:1688–94. doi: 10.1002/ibd.20526. [DOI] [PubMed] [Google Scholar]
- 20.HCUP. Nationwide Inpatient Sample (NIS). Healthcare Cost and Utilization Project (HCUP) Agency for Healthcare Research and Quality; Rockville, MD: 2004. [Accessed 10 October 2012.]. www.hcup-us.ahrq.gov/nisoverview.jsp. [Google Scholar]
- 21.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–83. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 22.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45:613–9. doi: 10.1016/0895-4356(92)90133-8. [DOI] [PubMed] [Google Scholar]
- 23.Ananthakrishnan AN, McGinley EL, Binion DG, Saeian K. Simple score to identify colectomy risk in ulcerative colitis hospitalizations. Inflamm Bowel Dis. 2010;16:1532–40. doi: 10.1002/ibd.21225. [DOI] [PubMed] [Google Scholar]
- 24.Ananthakrishnan AN, McGinley EL, Binion DG, Saeian K. A novel risk score to stratify severity of Crohn’s disease hospitalizations. Am J Gastroenterol. 2010;105:1799–807. doi: 10.1038/ajg.2010.105. [DOI] [PubMed] [Google Scholar]
- 25.Nguyen GC, Nugent Z, Shaw S, Bernstein CN. Outcomes of patients with Crohn’s disease improved from 1988 to 2008 and were associated with increased specialist care. Gastroenterology. 2011;141:90–7. doi: 10.1053/j.gastro.2011.03.050. [DOI] [PubMed] [Google Scholar]
- 26.Nguyen GC, Saibil F, Steinhart AH, Li Q, Tinmouth JM. Postoperative health-care utilization in Crohn’s disease: the impact of specialist care. Am J Gastroenterol. 2012;107:1522–9. doi: 10.1038/ajg.2012.235. [DOI] [PubMed] [Google Scholar]
- 27.Murthy SK, Steinhart AH, Tinmouth J, Austin PC, Nguyen GC. Impact of gastroenterologist care on health outcomes of hospitalised ulcerative colitis patients. Gut. 2012;61:1410–6. doi: 10.1136/gutjnl-2011-301978. [DOI] [PubMed] [Google Scholar]
- 28.Lichtenstein GR, Feagan BG, Cohen RD, Salzberg BA, Diamond RH, Price S, Langholff W, Londhe A, Sandborn WJ. Serious Infection and Mortality in Patients With Crohn’s Disease: More Than 5 Years of Follow-Up in the TREAT Registry. Am J Gastroenterol. 2012;107:1409–22. doi: 10.1038/ajg.2012.218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Thirumurthi S, Chowdhury R, Richardson P, Abraham NS. Validation of ICD-9-CM diagnostic codes for inflammatory bowel disease among veterans. Dig Dis Sci. 2010;55:2592–8. doi: 10.1007/s10620-009-1074-z. [DOI] [PubMed] [Google Scholar]
- 30.de Silva S, Ma C, Proulx MC, Crespin M, Kaplan BS, Hubbard J, Prusinkiewicz M, Fong A, Panaccione R, Ghosh S, Beck PL, Maclean A, Buie D, Kaplan GG. Postoperative complications and mortality following colectomy for ulcerative colitis. Clin Gastroenterol Hepatol. 2011;9:972–80. doi: 10.1016/j.cgh.2011.07.016. [DOI] [PubMed] [Google Scholar]
- 31.Ma C, Crespin M, Proulx MC, Desilva S, Hubbard J, Prusinkiewicz M, Nguyen GC, Panaccione R, Ghosh S, Myers RP, Quan H, Kaplan GG. Postoperative complications following colectomy for ulcerative colitis: A validation study. BMC Gastroenterol. 2012;12:39. doi: 10.1186/1471-230X-12-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.