Abstract
We describe a case of previously healthy 72-year-old man, who presented with rest angina. The ECG revealed sinus rhythm, biphasic T waves with preserved R waves in V1–V4 precordial leads. Subsequent evaluation revealed the normal serum cardiac marker levels and echocardiography with the coronary angiography showing a critical lesion in the proximal left anterior descending artery. Thus it was diagnosed as Wellens’ syndrome. In our case, we highlight the subtle though classical ECG findings of Wellens’ syndrome and its specific angiographic correlation. It can be of vital importance to identify these changes and intervene in time appropriately so as to avoid the development of myocardial infarction that carries a substantial morbidity and mortality. Important aspects of diagnosis and management have also been reviewed.
Background
We presented this case to emphasise the classic ECG finding of Wellens’ syndrome and its specific angiographic correlation. It can be of vital importance for timely identification of this condition and intervene appropriately as these patients may develop extensive myocardial infarction that carries a significant morbidity and mortality.
Case presentation
A 72-year-old man presented with the complaints of retrosternal chest pain at rest for last 2 days. He had not experienced such pain in the past. No history of diabetes, hypertension or smoking or any family history of ischaemic heart disease was noted.
Investigations
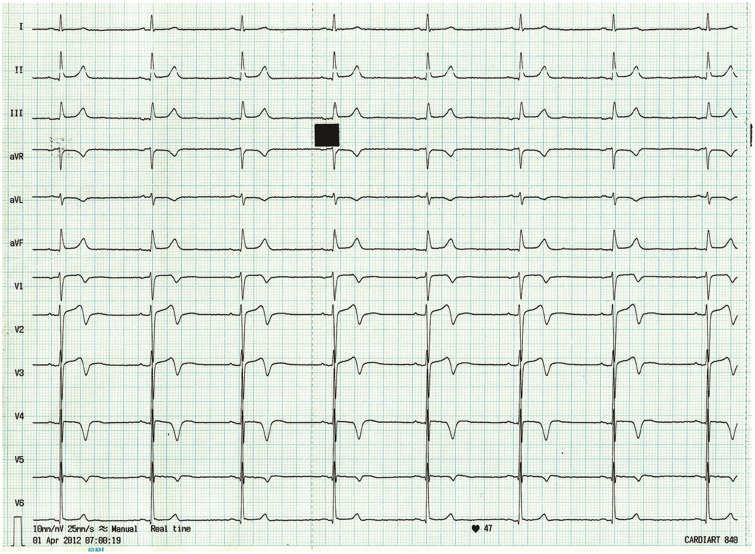
Cardiovascular examination was normal and cardiac serum marker levels were normal. The chest x-ray showed clear lung fields and a normal cardiac silhouette. The admission ECG (figure 1) showed sinus rhythm and biphasic T wave with preserved R waves in V1–V4 precordial leads. Transthoracic echocardiogram revealed no evidence of regional wall motion abnormality with normal biventricular function.
Figure 1.
ECG showing normal sinus rhythm, and biphasic T wave inversions with preserved R wave progression in V1–V4 leads.
Differential diagnosis
The relevant differential diagnosis included aortic dissection, pulmonary embolism, ST elevation myocardial infarction and acute pericarditis. These were excluded by appropriate investigations.
Treatment
The patient was treated for acute coronary syndrome (ACS) with aspirin, clopidogrel, β-blocker, nitroglycerine, high-dose statin and low-molecular-weight heparin. Serial cardiac biomarkers were negative and a follow-up ECG showed persistence of biphasic T wave inversions in precordial leads.
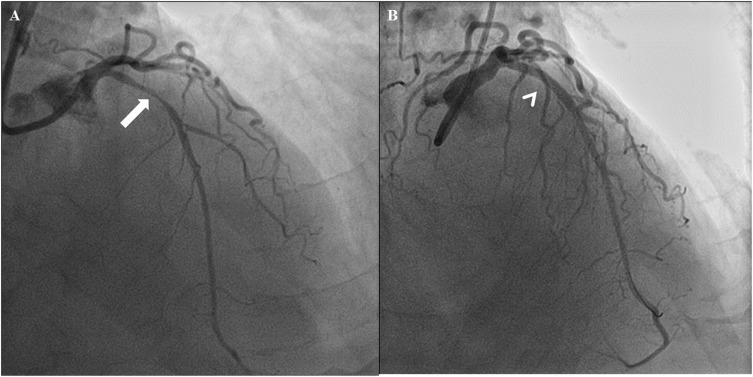
In view of intermittent chest pain and ECG changes, the patient underwent a conventional coronary angiogram (CAG). The CAG revealed a discrete 90% stenosis in the proximal segment of the left anterior descending (LAD) artery (figure 2A and video 1) just before the first septal branch. The rest of the coronary system was normal. The patient successfully underwent a percutaneous transluminal coronary angioplasty and stenting to LAD (figure 2B).
Figure 2.
Left coronary angiogram in right anterior oblique cranial projection (A, thick arrow) showing critical proximal left anterior descending lesion just before major diagonal which was addressed successfully by angioplasty (B, arrow head).
Left coronary angiogram in right anterior oblique cranial projection showing critical proximal left anterior descending lesion just before major diagonal.
Outcome and follow-up
Postintervention, the symptoms subsided and the ECG changes normalised. He was discharged on dual antiplatelets, high-dose statin and β-blocker and is doing well at a 6-month follow-up.
Discussion
ACS can be detrimental if not treated appropriately. The prognosis depends on the earliest recognition of the symptoms along with subtle clues on the ECG which would lead the physician to stratify the patients into low-risk, medium-risk or high-risk categories and thus to act accordingly. Rupture of atheromatous plaque in the coronary arteries plays an important role in the whole spectrum of ACS. Stabilisation of the plaque by medical management in low-risk patients or revascularisation by any mode of intervention in medium-risk/high-risk patients is the primary requirement.
T wave inversion in the anterior precordial leads takes many forms, has multiple causes and is a normal variant in the persistent juvenile T wave pattern. In 1982, de Zwaan et al1 called attention to the specificity of a unique type of anterior T wave inversion for ischaemia and/or injury in the distribution of the LAD. In this, the ST segment and the first-half of the T wave are essentially normal. At its peak the T wave makes a sharp >90° turn and its terminal portion is negative (figure 1). These changes have come to be known as Wellens’ warning. It is usually is seen hours or days after myocardial ischaemic pain subsides. During pain, T waves are usually upright with ST elevation or ST depression.
The characteristic changes of this ECG syndrome occur in the T wave and occur in two forms. More common (classical form), which occurs 76% of the time, is deep inversion of the T wave segment in the precordial leads.2 The ST segment is straight or concave, and passes into a deep negative T wave at an angle of 60–90°. The T wave is symmetric. In Wellens’ syndrome, these changes generally occur in leads V1–V4, but may also occasionally involve V5 and V6. V1 is involved in approximately 66% of patients and lead V4 nearly 75% of the time.3 The less common (24% of patients) variant of Wellens’ syndrome, as seen in this case, consists of biphasic T waves, most commonly in leads V2 and V3, but also can include V1–V5/V6.4
In Wellens’ syndrome, cardiac biomarkers can be falsely reassuring, as they are typically normal or only minimally elevated. Only 12% of patients with this syndrome have elevated cardiac biomarker levels, and these are always less than twice the upper limit of normal.4
Recognition of this ECG abnormality is of paramount importance because this syndrome represents a preinfarction stage of coronary artery. Since the LAD supplies the anterior myocardium, failure to recognise this pattern can result in anterior wall infarction, significant left ventricular dysfunction and/or death. Approximately 75% of patients with Wellens’ syndrome who are only medically managed and not revascularised (either through coronary bypass surgery or angioplasty) go on to develop extensive anterior wall infarction within days.1 5 Evolution to an anterior wall infarction is rapid, with a mean time of 8.5 days from the onset of Wellens’ syndrome to infarction.1 Thus, it is of utmost importance to recognise this pattern promptly.
Patients with this syndrome have been found to have at least a 50% stenosis of the LAD on angiography.4 These patients should ideally bypass stress testing and an emergency angiography should be conducted to determine the extent of disease and potentially provide information regarding the need for percutaneous coronary intervention, coronary artery bypass graft or medical management.2 6
Thus, this case very well illustrates that a patient presenting with chest pain, the subtle T wave inversions especially in anterior leads (V1–V4) may be as detrimental as acute myocardial infarction or alarms quite precisely about the impending myocardial infarction and thus specifying the need for timely recognition and appropriate management.
Learning points.
In suspected acute coronary syndrome, Wellens’ sign is often overlooked on ECG.
Deep/biphasic T wave inversion in the anterior precordial leads (V1–V4) in a patient with acute coronary syndrome (ACS) stratifies the patient into a high-risk category.
In ACS patient, the presence of Wellens’ sign in ECG suggests critical proximal left anterior descending stenosis.
Wellens’ syndrome patients should be ideally allowed to bypass stress testing and an emergency coronary angiography should be carried out to plan the revascularisation.
Approximately 75% of patients with Wellens’ syndrome who are only medically managed and not revascularised go on to develop extensive anterior wall infarction within days (mean time 8.5 days).
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.de Zwaan C, Bar FW, Wellens HJ. Characteristic electrocardiographic pattern indicating a critical stenosis high in left anterior descending coronary artery in patients admitted because of impending myocardial infarction. Am Heart J 1982;103:730–6 [DOI] [PubMed] [Google Scholar]
- 2.Tandy TK, Bottomy DP, Lewis JG. Wellens’ syndrome. Ann Emerg Med 1999;33:347–51 [DOI] [PubMed] [Google Scholar]
- 3.Rhinehardt J, Brady WJ, Perron AD, et al. Electrocardiographic manifestations of Wellens’ syndrome. Am J Emerg Med 2002;20:638–43 [DOI] [PubMed] [Google Scholar]
- 4.de Zwaan C, Bar FW, Janssen JH, et al. Angiographic and clinical characteristics of patients with unstable angina showing an ECG pattern indicating critical narrowing of the proximal LAD coronary artery. Am Heart J 1989;117:657–65 [DOI] [PubMed] [Google Scholar]
- 5.Movahed MR. Wellens’ syndrome or inverted U-waves? Clin Cardiol 2008;31:133–4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tatli E, Aktoz M, Buyuklu M, et al. Wellens’ syndrome: the electrocardiographic finding that is seen as unimportant. Cardiol J 2009;16:73–5 [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Left coronary angiogram in right anterior oblique cranial projection showing critical proximal left anterior descending lesion just before major diagonal.