Abstract
Aim:
Prevention of periodontal disease progression is the primary goal of periodontal therapy. When conventional therapy is found to be inadequate in achieving periodontal health in chronic periodontitis, local antimicrobial agents are used as an adjunct to scaling and root planing (SRP), which produces encouraging results. In the present study, an attempt was made to develop a low-dose controlled-release delivery system for the treatment of periodontal infections. A new sustained release drug system of poly e-caprolactone (PCL) nanofibers containing metronidazole (MET) was successfully electrospun and evaluated clinically for periodontal diseases. The retentive nanofibres were shown to provide a controlled delivery of the drugs.
Materials and Methods:
Nanofibers were prepared with MET in PCL by electrospinning technique. The drug-coated nanofibers provided sustained effect up to a period of 11 days (264 h) and followed first-order release. Forty sites in seven patients (four females and three males) with chronic periodontitis (5–8 mm probing depth) were allocated in two experimental treatment groups: Group A treated with SRP + MET nanofibers and Group B treated with SRP alone (control group). All these patients were evaluated clinically for probing depth (PD), plaque index (PI), and gingival index (GI).
Results:
Both the treatment groups were found to be efficacious in the treatment of periodontal disease as demonstrated by improvement in PD, PI, and GI.
Conclusion:
Combination of SRP + MET nanofibers (Group A) resulted in added benefits, compared to the control group.
Keywords: Chronic periodontitis, local drug delivery, metronidazole, nanofibers
INTRODUCTION
The oral cavity has a diverse environment for colonization of a wide variety of microorganisms. The early oro-dental infections are due to facultative or strict aerobes, and at later stages most bacteria in oral infections are anaerobic species. Facultative indigenous oral streptococci and anaerobic species, especially the Bacteroides, Fusobacterium, anaerobic cocci, and Actinomyces species, are the most common agents of pyogenic submucosal oro-facial infections.[1] There are many antibiotics which are commonly released in simulated gingival fluid for about 5 days.[2] Tetracycline is an antibiotic with the highest level of drug being released during 24-h broad-spectrum antibiotic that inhibits the anaerobic and followed by sustained effect up to 5 days.[3] The first literature about using monolithic fibers as a drug delivery system for periodontal diseases was by Goodson et al. who studied on ethylene vinyl acetate fibers incorporated tetracycline hydrochloride, which exhibited in vitro drug release up to 9 days.[4] Subsequently, other researchers attempted to develop controlled-release devices using various polymers and antibiotics and evaluated them in vitro or in vivo for the treatment of periodontal diseases. Metronidazole (MET) is the most common broad-spectrum antibiotic and is active against most of the periodontal pathogens due to the low minimum inhibitory concentration (MIC).[5] Poly e-caprolactone (PCL) is a semi-crystalline biodegradable aliphatic polyester which is well known for its slow biodegradability, high biocompatibility, and good drug permeability.[6] Unlike the commonly used biodegradable polymers such as poly (d, l-lactic-co-glycolic acid), PCL does not produce a local acidic environment as it degrades. This, along with its comparatively low cost, renders PCL an attractive biomedical polymer.[7] However, PCL, in the form of homopolymer, has not been used for periodontal diseases successfully yet. The main objective of the present study was to develop a local delivery system in the form of MET electrospun PCL nanofibers for treatment of periodontal infections.
MATERIALS AND METHODS
MET (99.90% purity) was received as a gift sample from Nandlal and Bankatlal, Mumbai, India. PCL was from Sigma Aldrich Chemicals, Mumbai, India. All the chemicals used were of analytical grade.
The key ingredients used in the formulation and their functions in the formulation are as follows:
MET: Active pharmaceutical ingredient (API)
PCL: Drug carrier, fiber formation, and release retardation
Methods
Solution of PCL with MET was prepared, and the nanofibers were prepared by electrospinning technique in Department of Pharmaceutics, IIT, BHU, Varanasi (UP), India. Scanning Electron Microscopy (SEM) was used to investigate the morphology and average diameter of the electrospun nanofibers. Electrospinning is an inexpensive method that creates polymeric fibers with diameters in the range of nano to a few microns through electrically charged jet of polymer solution or polymer melt. When charges within a polymer droplet at the tip of a needle reach a critical amount, a fluid jet will erupt from the droplet. The electrospinning jet will travel toward a grounded collector. As the solvent evaporates, the jet solidifies and the polymeric fibers collect on the grounded target.[8] Drugs can be capsulated directly into electrospun fibers by electrospinning of a mixture solution of a drug and polymer. The solubility and compatibility of drugs in the drug–polymer–solvent system are the effective factors on drug release behavior although both hydrophobic and hydrophilic drugs can be incorporated in electrospun fibers.[9,10] Electrospun nanofibers offer advantages such as higher drug loading efficiency in comparison with some other methods like encapsulation. Furthermore, the drug release profile can be tailored by a modulation on the morphology, porosity, and composition of nanofibers.[11] Very small diameter of nanofibers can provide a short diffusion passage length and their high surface area is helpful to mass transfer and efficient drug release.[12,13]
Electrospinning was carried out using 13% w/v solution of PCL in methanol and chloroform mixtures at ratios of 3.5:1.5 v/v. Then, the drug was added, which is soluble in polymer solution. The drug concentration was in the range of 25%-35% w/w with respect to the polymer used. The resulting clear solution was transferred to a 5-ml syringe pump with a right angle-shaped needle of 0.6 mm inner diameter attached to it. The flow rate of the polymer solution was 1.50-2.50 ml/h, and the applied positive voltage was in the range of 12-14 kV. The resulting fibers were collected on a grounded aluminum plate. The distance between the needle tip and the grounded target was 15 cm. The thickness of all nanofibers webs ranged from 300 to 340 μm. For preparation of electrospun nanofiber, horizontal setup was used.
Evaluation of electrospun nanofiber
The uniformity of thickness was determined by measuring the thickness of selected nanofiber (surface area 1 cm2) of each formulation using a screw gauge. The uniformity of weight was determined by weighing each nanofiber film (surface area 1 cm2) of each formulation on electronic balance. The drug-loaded nanofiber film of surface area 1 cm2 was cut and kept in 100 ml McIlvaine buffer of pH 6.6 by vigorous stirring for 6 h in a tightly closed conical flask. The amount of drug present was measured spectrophotometrically.
Scanning electron microscope studies
Surface morphology of nanofiber was studied by SEM. The mounted samples were sputter coated for 5 min with gold using fine coat ion sputter and examined under SEM [Figure 1]. The SEM photographs demonstrated that no beaded fibers were obtained by electrospinning of these solutions containing various amounts of MET.
Figure 1.
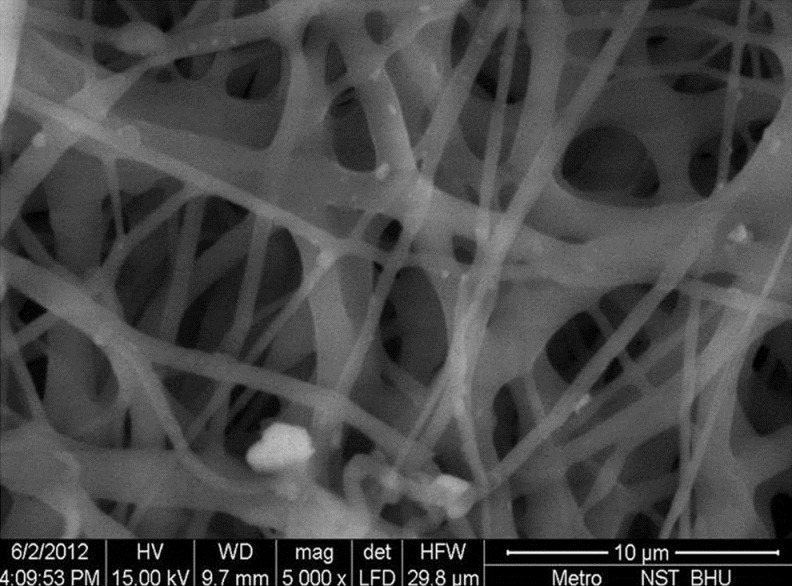
Scanning electron microscope photograph
The present study included 40 bleeding sites, with a probing depth (PD) of 5-8 mm, which were selected in seven patients of both genders (four females and three males) aged between 20 and 50 years from the outpatient department at Faculty of Dental Sciences, Institute of Medical Sciences (IMS), BHU, Varanasi. The ethical committee of IMS, BHU, Varanasi approved the study, and written informed consent was obtained from all patients. Patients with good systemic health, had not received any surgical or non-surgical periodontal therapy in the past 6 months, and were diagnosed as suffering from chronic generalized periodontitis were enrolled. Individuals with history of using antimicrobial mouthrinses within 2 months of the baseline visit or on routine basis or patients having a history of allergy to MET or lidocaine were excluded from the study.
The selected sites were randomly divided into two groups:
Test Group A [scaling and root planing (SRP) + MET nanofibers] – Included 20 sites treated by SRP with MET nanofibers
Test Group B (SRP alone) – Included 20 sites treated with SRP alone
The clinical parameters recorded were the PD using UNC-15 periodontal probe, plaque index (PI), and gingival index (GI). After recording clinical parameters from each site at baseline, a thorough SRP was done in both the groups. The clinical parameters were assessed at baseline, after 15 days, and 1 month after receiving treatment in the same patient; as it is a split-mouth study.
Administration
Probing depth was measured before insertion of fiber, with help of UNC-15 probe [Figure 2]. It was 5mm. Subgingival administration of these nanofibers was accomplished by inserting the fibers directly into the base of the pocket. Gentle force was used with a straight probe, so that the material fills the depths and curves of the pocket [Figure 3]. The gingiva was subsequently and carefully adapted to close the entrance of the gingival margin and hand pressure was applied for just a few minutes to encourage hemostasis and initial setting of the material inside the pocket. The gingival margin was sealed with Coe-Pak to prevent the dislodgement of the drug and the ingress of oral fluids. As degradation of PCL is slow in aqueous medium due to its semi-crystalline and hydrophobic nature, the drug release from PCL electrospun nanofibers over these periods of time was controlled by diffusion mechanism. Patients were recalled after 7 days for Coe-Pak removal and were evaluated for any inflammatory response. Patients were instructed not to chew any hard, crunchy, or sticky food for at least 1 week, postpone brushing and flossing on the treated site for 1 week, not to disturb the area with tongue, finger, or tooth pick, and to report immediately if the material is dislodged before the scheduled recall visit or if pain, swelling, or any other problem occurs. After 15 days the post-operative probing depth was measured 3mm [Figure 4].
Figure 2.
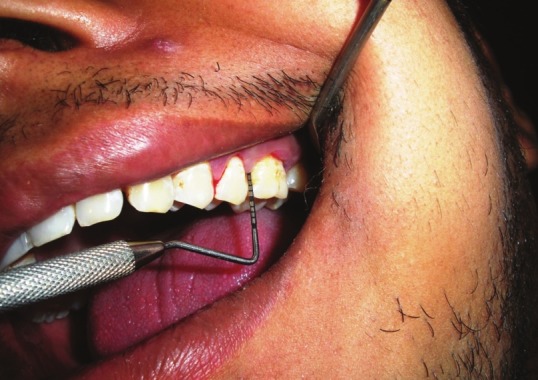
Measurement of probing depth at baseline
Figure 3.

Insertion of the nanofiber into the pocket
Figure 4.

Measurement of probing depth after 1 month
RESULTS
Results are presented in Table 1 . The recording of all the clinical parameters was done at baseline and after 15 and 30 days. Finally, the complete data were statistically analyzed using paired “t” test. None of the subjects reported any oral symptoms such as toothache (including dental or gingival), painful symptomatology (including oral pain, tenderness, soreness, discomfort, or sensitivity), inflammation, allergy, abscess, altered taste or increased salivation, etc.
Table 1.
Comparison of Group A with Group B
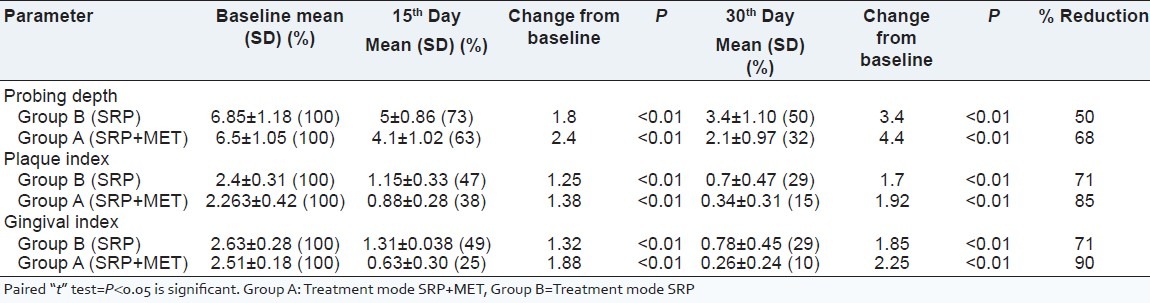
Comparison of two groups
Group A was treated with SRP + MET and Group B with SRP alone. At the end of the observation interval (i.e. 15th and 30th day), all sites got healed unevenly. The mean values for PD, PI, and GI score were measured at 15th and 30th days following treatment. The percentage reduction in PD, PI, and GI scores from baseline was 68%, 85%, and 90%, respectively, in the patients treated with SRP + MET (Group A), whereas in the patients treated SRP alone (Group B), the values were about 50%, 71%, and 71%, respectively, which shows that the formulation containing MET was significantly better.
DISCUSSION
A periodontal disease essentially comprises a group of oral infections, whose primary etiological factor is dental plaque, which results in an inflammatory lesion in the supporting tissues. Removal of the cause (and its effects) is the primary aim of both non-surgical and surgical treatment regimens. The major non-surgical therapeutic approach involves mechanical SRP. The infective nature of the disease has led to the widespread use of antimicrobials as an adjunct to SRP. Local delivery of antimicrobial agents is becoming more prevalent since it leads to higher concentration of the drug at the intended site of action using a lower dose, with an associated reduction in side effects relative to systemic administration. Local route of drug delivery provides direct access to the systemic circulation through the jugular vein bypassing the first pass hepatic metabolism leading to high bioavailability.[14] Other advantages include excellent accessibility, low enzymatic activity, and painless administration. In the present study, an attempt was made to evaluate the effectiveness of MET nanofibers in the treatment of chronic periodontitis, as an adjunct to SRP. MET was chosen in the present study because of its proven efficacy in the management of periodontal diseases. It is known for its antibacterial actions and it inhibits the bacterial protein synthesis. The results from the present study suggest that the application of MET nanofibers combined with SRP is beneficial in the treatment of chronic periodontitis and improving periodontal parameters for 1 month duration. The drug concentration and a sustained release of drugs were achieved from the nanofibers for at least 19 days with low burst release. This could be an ideal treatment period for periodontal diseases. All electrospun nanofibers remained smooth and quite flexible, without shrinkage during the period of our treatments, which may offer a desirable texture to be used comfortably. In order to be effective, a pharmaceutical agent should reach the entire periodontal pocket up to the bottom and should be maintained long enough at a sufficient concentration for the intended pharmaceutical effect to occur. Periodontal pockets, however, possess complicating anatomic characteristics. Furthermore, periodontal pathogens in the subgingival environment reside in a biofilm adhering to the exposed root cementum or to the soft tissue, or even invading the pocket epithelium, the underlying connective tissue, or the root dentin.[15] The aggregation of bacteria in a biofilm impairs the diffusion or may even inactivate antimicrobial agents. Thus, high concentrations of antimicrobial agents are needed before a beneficial effect can be expected. Various biofilm experiments indicate that the necessary MICs of antimicrobial agents are at least 50 times higher (or even 210,000 times) than for bacteria growing under planktonic conditions.[16–18] However, as this material, i.e. MET nanofiber, is of Indian origin, and is easy to place in the periodontal pocket, less time consuming, and relatively cost effective, its use can be expanded easily in the Indian population.
Conclusively, such PCL electrospun nanofibers can be used as a locally controlled delivery system and the MET nanofibers have additive benefits when used as an adjunct to SRP in patients with chronic periodontitis.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Kornman KS. Mapping the pathogenesis of periodontitis: A new look. J Periodontol. 1993;64:782. doi: 10.1902/jop.2008.080213. [DOI] [PubMed] [Google Scholar]
- 2.Quirynen M, Teughels W, De Soete M, van Steenberghe D. Topical antiseptics and antibiotics in the initial therapy of chronic adult periodontitis: Microbiological aspects. Periodontol 2000. 2002;28:72–90. doi: 10.1034/j.1600-0757.2002.280104.x. [DOI] [PubMed] [Google Scholar]
- 3.Ahuja A, Ali J, Rahman S. Biodegradable periodontal intrapocket device containing metronidazole and amoxycillin: Formulation and characterization. Pharmazie. 2006;61:25–9. [PubMed] [Google Scholar]
- 4.Goodson JM. Pharmacokinetic principles controlling efficacy of oral therapy. J Dent Res. 1989;68:1625–32. [Google Scholar]
- 5.Tiwari G, Tiwari R, Srivastava B, Rai AK. Design and evaluation of target retentive device containing metronidazole for the treatment of periodontal disease. Res J Pharm Tech. 2008;1:390–4. [Google Scholar]
- 6.Kenawy ER, Abdel-Hay FI, El-Newehy MH, Wnek GE. Controlled release of ketoprofen from electrospun poly (vinyl alcohol) nanofibers. Mater Sci Eng. 2007;459:390–6. [Google Scholar]
- 7.Van EL, Grøndahl L, Chua KN, Leong KW, Nurcombe V, Cool SM. Controlled release of heparin from poly (e-caprolactone) electrospun fibers. Biomaterials. 2006;27:2042–50. doi: 10.1016/j.biomaterials.2005.10.028. [DOI] [PubMed] [Google Scholar]
- 8.Zamani M, Morshed M, Varshosaz J, Jannesari M. Controlled release of metronidazole benzoate from poly e-caprolactone electrospun nanofibers for periodontal diseases. Eur J Pharm Biopharm. 2010;75:179–85. doi: 10.1016/j.ejpb.2010.02.002. [DOI] [PubMed] [Google Scholar]
- 9.Zeng J, Yang L, Liang Q, Zhang X, Guan H, Xu X, et al. Influence of the drug compatibility with polymer solution on the release kinetics of electrospun fiber formulation. J Control Release. 2005;105:43–51. doi: 10.1016/j.jconrel.2005.02.024. [DOI] [PubMed] [Google Scholar]
- 10.Xu X, Yang L, Xu X, Wang X, Chen X, Liang Q, et al. Ultrafine medicated fibers electrospun from W/O emulsions. J Control Release. 2005;108:33–42. doi: 10.1016/j.jconrel.2005.07.021. [DOI] [PubMed] [Google Scholar]
- 11.Kim K, Luu YK, Chang C, Fang D, Hsiao BS, Chu B, et al. Incorporation and controlled release of a hydrophilic antibiotic using poly (lactide-co-glycolide)-based electrospun nanofibrous scaffolds. J Control Release. 2004;98:47–56. doi: 10.1016/j.jconrel.2004.04.009. [DOI] [PubMed] [Google Scholar]
- 12.Huang ZM, He CL, Yang A, Zhang Y, Han XJ, Yin J, et al. Encapsulating drugs in biodegradable ultrafine fibers through co-axial electrospinning. J Biomed Mater Res. 2006;77:169–79. doi: 10.1002/jbm.a.30564. [DOI] [PubMed] [Google Scholar]
- 13.Verreck G, Chun I, Rosenblatt J, Peeters J, Dijck AV, Mensch J, et al. Incorporation of drugs in an amorphous state into electrospun nanofibers composed of a water-insoluble, nonbiodegradable polymer. J Control Release. 2003;92:349–60. doi: 10.1016/s0168-3659(03)00342-0. [DOI] [PubMed] [Google Scholar]
- 14.Javali MA, Vandana KL. A comparative evaluation of atrigel delivery system (10% doxycycline hyclate) Atridox with scaling and root planing and combination therapy in treatment of periodontitis: A clinical study. J Indian Soc Periodontol. 2012;16:43–8. doi: 10.4103/0972-124X.94603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Srivastava R, Verma PK, Tandon P, Ramesh KM, Gupta KK, Srivastava A. Chlorhexidine chip and tetracycline fibers as adjunct to scaling and root planing – A clinical study. Braz J Oral Sci. 2009;8:201–5. [Google Scholar]
- 16.Rodrigues IF, Machion L, Casati MZ, Nociti FH, Jr, de Toledo S, Sallum AW, et al. Clinical evaluation of the use of locally delivered chlorhexidine in periodontal maintenance therapy. J Periodontol. 2007;78:624–8. doi: 10.1902/jop.2007.060317. [DOI] [PubMed] [Google Scholar]
- 17.Hussein I, Ranka M, Gilbert A, Davey K. Locally delivered antimicrobials in the management of periodontitis: A critical review of the evidence for their use in practice. Dent Update. 2007;34:494–506. doi: 10.12968/denu.2007.34.8.494. [DOI] [PubMed] [Google Scholar]
- 18.Barat R, Srinatha A, Pandit JK, Ridhurkar D, Balasubramaniam J, Mittal N, et al. Niridazole biodegradable inserts for local long-term treatment of periodontitis: Possible new life for an orphan drug. Drug Deliv. 2006;13:365–73. doi: 10.1080/10717540500398126. [DOI] [PubMed] [Google Scholar]


