Abstract
Objective
To evaluate the effect of combining photo-activation therapy with platelet-rich plasma injections for the novel treatment of osteoarthritis.
Design
We present a case report of osteoarthritis of the knee treated with photo-activated platelet-rich plasma injections (PAPRP).
Methods
After utilising conventional osteoarthritis treatment methods a patient underwent a course of PAPRP injections. The patient outcome was measured using the numerical pain rating scale (NPRS) and the Western Ontario and McMaster Universities Arthritis (WOMAC) Index.
Results
Following treatment the patient reported improvements in both pain and function as measured by the NPRS and WOMAC Index, respectively. The patient was followed up for 18 weeks, at which time no significant complications were noted.
Conclusions
In this case report of osteoarthritis, with strict control of conventional therapy variables, PAPRP injections demonstrated improvement in all recorded outcome measures. The results of this case report highlight the need to further investigate the use of PAPRP in the treatment of symptomatic knee osteoarthritis.
Background
Arthritis is a major cause of disability and chronic pain and has a significant economical impact.1–3 Osteoarthritis (OA) is a progressive and degenerative form of arthritis that does not discriminate against age. Osteoarthritis is difficult to treat, with most current medical treatment strategies aimed at pain reduction and/or symptom control rather than biochemical disease modification. Available pharmacological treatments are limited and often bear unwanted side effects.4
Viscosupplement/hyaluronic acid (HA) intra-articular injections have been used for many years as an adjunctive treatment in conservative management of osteoarthritis. However, the mechanism of action of HA is uncertain,5 with some studies suggesting little improvement beyond that achieved with placebo injections.6
Recent research has focused on the catabolic cytokines involved in destruction of hyaline cartilage and joint degeneration. Interleukin-1 (IL-1) has been identified as a potent mediator of cartilage loss 7–9 and reciprocally IL-1 receptor antagonist (IL-1RA) has been shown to limit the intra-articular actions of IL-1.10–12 Autologous conditioned serum (ACS) is an injectable IL-1RA medium that has been used in Europe for the treatment of osteoarthritis.12 Research has indicated significant improvement in symptoms of OA post ACS therapy,12 however, further research is required to determine whether ACS is actually disease modifying. Use of ACS is limited due to cost and logistical hurdles such as incubating the autolgous blood overnight prior to reinjection.
Owing to the limitations of ACS, the research focus has shifted towards platelet-rich plasma (PRP) injections, where reports have demonstrated improved cartilage matrix expression in animal and in-vitro studies, along with the synthesis of hylauronic acid.13–17 Platelets, once originally thought to act solely in haemostasis at sites of vascular injury, are now known to contain an abundance of growth factors and cytokines, crucial to soft-tissue healing. In fact, a retrospective cohort study has indicated significant reduction in pain postintrarticular injection of PRP compared with hyaluroinc acid supplements.16 Similarly, a recent study of patients with grades I–III OA, demonstrated significantly improved pain and function following PRP, when compared with the hyaluronic acid injection control group.18
Beside PRP, photo-activation therapy has been shown to increase expression of leucocyte-derived anti-inflammatory cytokines (IL-1RA) and also to cause reduction in proinflammatory cytokines (IL-2 and 6).19 20 Thus, a combined photo-activated PRP (PAPRP) preparation may offer a novel method for treatment of osteoarthritis that combines the proven benefits of ACS with potentially disease-modifying properties of PRP.
Case presentation
A 50-year-old woman presented to a Sports and Exercise Medicine Clinic with progressive and symptomatic left knee osteoarthritis. Radiological examination using x-ray (Kellgren and Lawrence Protocol21) confirmed tricompartmental osteoarthritis with grade IV medial compartment chondromalacia and grades II–III changes of both her lateral and patellofemoral compartments.
The pre-existing conservative management programme included podiatric biomechanical assessment and orthotic alteration, daily weight bearing, moderate-intensity exercise and significant weight loss in the preceding 12 months (>30 kg). In addition, glucosamine sulfate (1500 mg daily) along with other daily supplements were being taken. Non-steroidal anti-inflammatory drugs (NSAIDs) were not prescribed due to a strong paternal family history of ischaemic heart disease at an early age. Strict regular long-acting paracetamol (1330 mg twice daily) was prescribed at her initial consultation.
The patient sought advice on possible additional treatments for her knee arthritis and made specific enquiries regarding PRP intra-articular injections. As such, written information and education was provided regarding PRP and its use within osteoarthritis, including relevant alternatives and possible risks involved. Given that the patient had radiological proven osteoarthritis, failed conservative treatments and was otherwise well, she was assessed as a suitable candidate for the trial of intra-articular PRP. Formal written informed consent was obtained prior to commencement of treatment.
Investigations
Radiological examination using x-ray confirmed tricompartmental osteoarthritis with grade IV medial compartment chondromalacia and grades II–III changes of both her lateral and patellofemoral compartments.
Treatment
Photo-activated PRP preparation
Autologous blood (24 mls) was taken from the study participant and separated into 3×8.5 ml BD Vacutainers (BD, Franklin Lakes, New Jersey, USA) containing ACD (trisodium citrate 22 g/l, citric acid 8 g/l and dextrose 24.5 g/l) to prevent clotting. The tubes were centrifuged at 1000 rpm for 10 min to create a platelet-poor plasma (PPP) level, a middle buffy coat level (high in platelets and leucocytes) and a red blood cell layer.
PPP was withdrawn from each tube to the level of 10 mm above the buffy coat and discarded. The remaining plasma, along with the buffy coat and 2 mm of the red cell layer were withdrawn into a single sterile tube and exposed to photo-activation for 10 min. Photo-activation was achieved using the commercial Adi-Light 2 device (AdiStem Ltd, Hong Kong).
Injection method
Under strict sterile conditions and ultrasound guidance, a sterile 21-gauge needle was inserted using a medial approach to the medial knee compartment. Four millilitres of PAPRP was injected with no concurrent use of local anaesthetic. Overall, the patient received three PAPRP injections, each 1 week apart (weeks 0, 1 and 2).
Potential adverse effects
Previous studies using PRP therapy have indicated minimal adverse effects.18 22 Spakova et al documented a short self-limited aggrevation of osteoarthritis symptoms in some patients. As this is an intra-articular injection the most significant risk is that of infection.
Analysis method and outcome measures
Prospective analysis of patient outcomes to intra-articular PAPRP injection included the Numerical Pain Rating Scale (NPRS)23 and Western Ontario and McMaster Universities Arthritis Index (WOMAC Index 3.0).24 25 The WOMAC Knee Score is a validated disease-specific functional quality-of-life instrument developed to assess pain, stiffness and physical function in patients with knee osteoarthritis.24 25
NPRS was recorded prior to and 2 weeks following commencement of paracetamol, and prior to each injection, with follow-up intervals occurring at weeks 3, 6, 10, 14 and 18. The WOMAC Knee Score was recorded prior to the first injection and at weeks 6, 10, 14 and 18. In addition to the above treatment outcome measures, patient satisfaction with treatment was further assessed at week 18 by recording a percentage perceived improvement.
Outcome and follow-up
Results
Following 2-weeks commencement of regular paracetamol and prior to undergoing PAPRP therapy, the patient reduced their pain from 5 to 4 on the NPRS. NPRS improved further after the first injection of PAPRP and reduced to 0 by week 6. NPRS remained between 0 and 1 from week 4 to final data collection in week 18 (figure 1).
Figure 1.
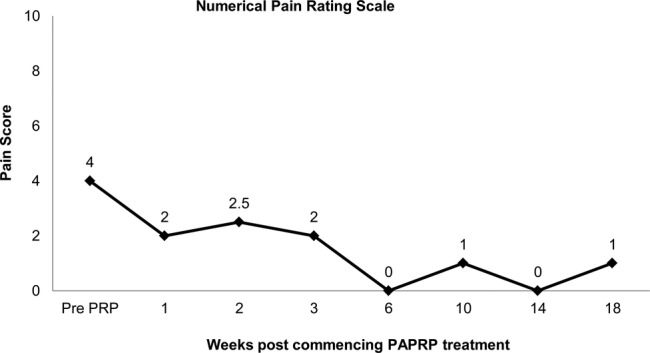
Numerical pain rating scale. Pain reduced following photo-activated platelet-rich plasma injections for the treatment of osteoarthritis in the knee.
WOMAC Knee Score at baseline indicated significant pain, physical and functional impairment (Global WOMAC Score 59.38). At week 6, the Global WOMAC Score had improved by 65% and remained so up to the final data collection at week 18 (figure 2).
Figure 2.
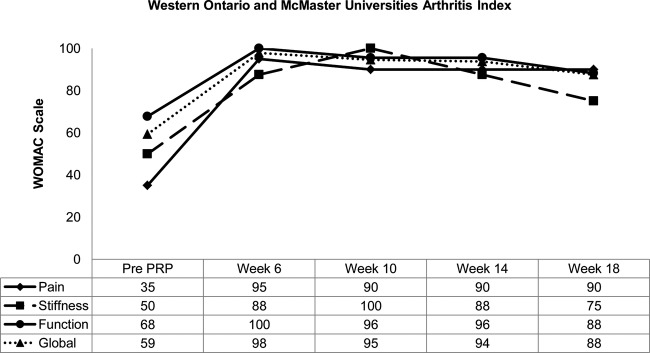
Western Ontario and McMaster Universities Arthritis Index. Pain, stiffness and function improved following photo-activated platelet-rich plasma injections for the treatment of osteoarthritis in the knee.
At 18 weeks following the initial PAPRP injection, a percentage perceived improvement of 80% was reported by the patient.
A small ‘flare up’ of knee discomfort following the second PAPRP injection, lasting 2 days, was reported by the patient. This was not associated with a knee effusion and no increase in analgesia was required. No other complications were noted.
Discussion
This report highlights the novel treatment of osteoarthritis by combining the anti-inflammatory characteristics of photo-activation with the disease-modifying properties of PRP. Post-PAPRP therapy, the patient demonstrated improvement in all the recorded treatment outcome measures. NPRS improved at week 1 (7 days post first injection), suggesting an immediate anti-inflammatory and analgesic benefit of PAPRP. Sustained improvements in NPRS were observed for 18 weeks post-therapy. Concurrent results were observed in the pain subset of the WOMAC index. Both stiffness and function were also improved on the WOMAC when measured at 6 weeks post-PAPRP.
A small ‘flare up’ of discomfort was observed following the second PAPRP injection; however, this was short-lived and did not occur with the first or third injection. Similar short-term pain increases have been observed in the literature following injection, which also resulted in no long-term complications.18 22
At present PRP literature is limited; however, the small but growing body of evidence promotes the use of PRP therapy in OA. In two separate studies, PRP therapy (without photo-activation) has demonstrated improved pain and function when compared to hyaluronic acid injections for OA.16 18 This limited single case report does not aim at providing conclusive evidence for the combined use of PAPRP, rather it aims to promote further discussion and thought into optimising current PRP protocols and developing controlled-randomised studies to further investigate the role of photo-activation in PRP preparation.
Our preliminary findings suggest that PAPRP may have promise in the treatment of symptomatic knee OA. In a single case report with strict control of other treatment variables and prior maximisation of conservative OA treatment, PAPRP therapy was associated with improvement in all the recorded treatment outcome measures. Symptomatic improvement was achieved within 1 week of the first injection.
The novel method of combining photo-activation of PRP for the treatment of symptomatic arthritis has not previously been described within the scientific literature. Previous publications have shown the potential of PRP in the treatment of osteoarthritis but unlike this single case report have not recorded short-term treatment outcome data (within 1 month).16–18 This case study indicates the potential for photo-activated PRP to have both short-term and extended benefits in improving symptomatic arthritis.
While recognising the low level of evidence, the results of this limited case report highlight the need to further investigate—through a more structured and appropriately powered randomised-controlled trial—the combined use of photo-activation and PRP and so to determine both the clinical efficacy and mechanistic properties of PAPRP.
Depending on the results of further research, PAPRP may have a role in the non-surgical management of knee osteoarthritis. This is a promising development for the patient population who remain symptomatic despite maximal conservative management and who are unsuitable for surgical intervention.
Learning points.
Current pharmacological treatments for osteoarthritis are limited.
Photo-activated platelet-rich plasma (PRP) shows promise in the treatment of symptomatic knee osteoarthritis.
Photo-activation therapy of PRP may improve its anti-inflammatory properties and result in earlier symptomatic improvement.
Further research is required to determine if photo-activated PRP has structural disease-modifying properties.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Australia, Arthritis http://www.arthritisaustralia.com.au/index.php/arthritis-information/what-is-arthritis.html (updated July 2010) (accessed Mar 2012).
- 2.Gupta S, Hawker GA, Laporte A, et al. The economic burden of disabling hip and knee osteoarthritis (OA) from the perspective of individuals living with this condition. Rheumatology (Oxford) 2005;44:1531–7 [DOI] [PubMed] [Google Scholar]
- 3.Peat G, McCarney R, Croft P. Knee pain and osteoarthritis in older adults: a review of community burden and current use of primary health care. Ann Rheum Dis 2001;60:91–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Abraham NS, El-Serag HB, Hartman C, et al. Cyclooxygenase-2 selectivity of non-steroidal anti-inflammatory drugs and the risk of myocardial infarction and cerebrovascular accident. Aliment Pharmacol Ther 2007;25:913–24 [DOI] [PubMed] [Google Scholar]
- 5.Bagga H, Burkhardt D, Sambrook P, et al. Long term effects of intraarticular hyaluronan on synovial fluid in osteoarthritis of the knee. J Rheum 2006;33:946–50 [PubMed] [Google Scholar]
- 6.Baltzer AWA, Moser C, Jansen SA, et al. Autologous conditioned serum is an effective treatment for knee osteoarthritis. Osteoarthritis Cartilage 2009;17:152–60 [DOI] [PubMed] [Google Scholar]
- 7.Goldring MB. Osteoarthritis and cartilage: the role of cytokines . Curr Rheumatol Rep 2000;2:459–65 [DOI] [PubMed] [Google Scholar]
- 8.Goldring SR, Goldring MB. The role of cytokines in cartilage matrix degeneration in osteoarthritis. Clin Orthop Relat Res 2004;(Suppl 427):27–36 [DOI] [PubMed] [Google Scholar]
- 9.Fernandes JC, Martel-Pelletier J, Pelletier JP. The role of cytokines in osteoarthritis pathophysiology. Biorheol 2002;39:237–46 [PubMed] [Google Scholar]
- 10.Arend WP, Malyak M, Guthridge CJ, et al. Interleukin-1 receptor antagonist: role in biology. Annu Rev Immunol 1998;16:27–55 [DOI] [PubMed] [Google Scholar]
- 11.Dinarello CA. Interleukin-1 and interleukin-1 antagonism. Blood 1991;77:1627–52 [PubMed] [Google Scholar]
- 12.Dinarello CA. The role of the interleukin-1-receptor antagonist in blocking inflammation mediated by interleukin-1. N Engl J Med 2000;343:732–4 [DOI] [PubMed] [Google Scholar]
- 13.Saito M, Takahashi KA, Arai Y, et al. Intraarticular administration of platelet-rich plasma with biodegradable gelatin hydrogel microspheres prevents osteoarthritis progression in the rabbit knee. Clin Exp Rheumatol 2009;27:201–7 [PubMed] [Google Scholar]
- 14.Drengk A, Zapf A, Sturmer EK, et al. Influence of platelet-rich plasma on chondrogenic differentiation and proliferation of chondrocytes and mesenchymal stem cells . Cells Tissues Organs 2009;189:317–26 [DOI] [PubMed] [Google Scholar]
- 15.Schmidt MB, Chen EH, Lynch SE. A review of the effects of insulin-like growth factor and platelet derived growth factor on in vivo cartilage healing and repair. Osteoarthritis Cartilage 2006;14:403–12 [DOI] [PubMed] [Google Scholar]
- 16.Sanchez M, Anitua E, Azofra J, et al. Intra-articular injection of autologous preparation rich in growth factors for the treatment of knee OA: a retrospective cohort study. Clin Exp Rheumatol 2008;26:910–13 [PubMed] [Google Scholar]
- 17.Anitua E, Sanchez M, Nurden AT, et al. Platelet-released growth factors enhance the secretion of hyaluronic acid and induce hepatocyte growth factor production by synovial fibroblasts from arthritic patients. Rheumatology (Oxford) 2007;46:1769–72 [DOI] [PubMed] [Google Scholar]
- 18.Spakova T, Rosocha J, Lacko M, et al. Treatment of knee joint osteoarthritis with autologous platelet-rich plasma in comparison with hyaluronic acid. Am J Phys Med Rehab 2012;91:411–17 [DOI] [PubMed] [Google Scholar]
- 19.Sigmundsdottir H, Johnston A, Gudjonsson JE, et al. Narrowband-UVB irradiation decreased the production of pro-inflammatory cytokines by simulated T cells. Arch Dermatol Res 2005;297:39–42 [DOI] [PubMed] [Google Scholar]
- 20.Zhevago NA, Samoilova KA. Pro- and anti-inflammatory cytokine content in human peripheral blood after its transcutaneous (in vivo) and direct (in vitro) irradiation with polychromatic visible and infrared light, Photomed Laser Sur 2006;24:129–39 [DOI] [PubMed] [Google Scholar]
- 21.Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthritis. Ann Rheum Dis 1957;16:494–502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sampson S, Reed M, Silvers H, et al. Injection of platelet-rich plasma in patients with primary and secondary knee osteoarthritis. Am J Phys Med Rehab 2010;89:961–9 [DOI] [PubMed] [Google Scholar]
- 23.McCaffery M, Pasero C. Pain: clinical manual. 2nd edn St Louis, MO: Mosby, 1999:16 [Google Scholar]
- 24.Bellamy N, Buchanan WW, Goldsmith CH, et al. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheum 1988;15:1833–40 [PubMed] [Google Scholar]
- 25.Roos EM, Roos HP, Ekdahl C, et al. Knee injury and Osteoarthritis Outcome Score (KOOS): development of a self-administered outcome measure . J Orthopc Sports Phys Ther 1998;28:88–96 [DOI] [PubMed] [Google Scholar]


