Abstract
A 52-year-old man presented with abdominal pain with a background of splenectomy 25 years previously. Initial investigations lead to suspicion of a neuroendocrine tumour. Positron emission tomography octreotide scanning and chromogranin were raised. He subsequently underwent a lateral segmentectomy. The histopathology was consistent with splenosis.
1. Splenosis must be considered as differential in any patient with abdominal symptoms post-traumatic splenectomy.
2. Positron emission tomography (PET) octreotide scanning can detect splenosis giving false positives for a neuroendocrine tumour. This is the first case to describe such an association.
Case presentation
A 56-year-old man initially presented to his general practitioner with chronic epigastric abdominal pain without any other associated symptoms. Relevant background history included being involved in a previous helicopter accident resulting in a total splenectomy as well as a left nephrectomy many years previously. He had been well in the interim.
Investigations
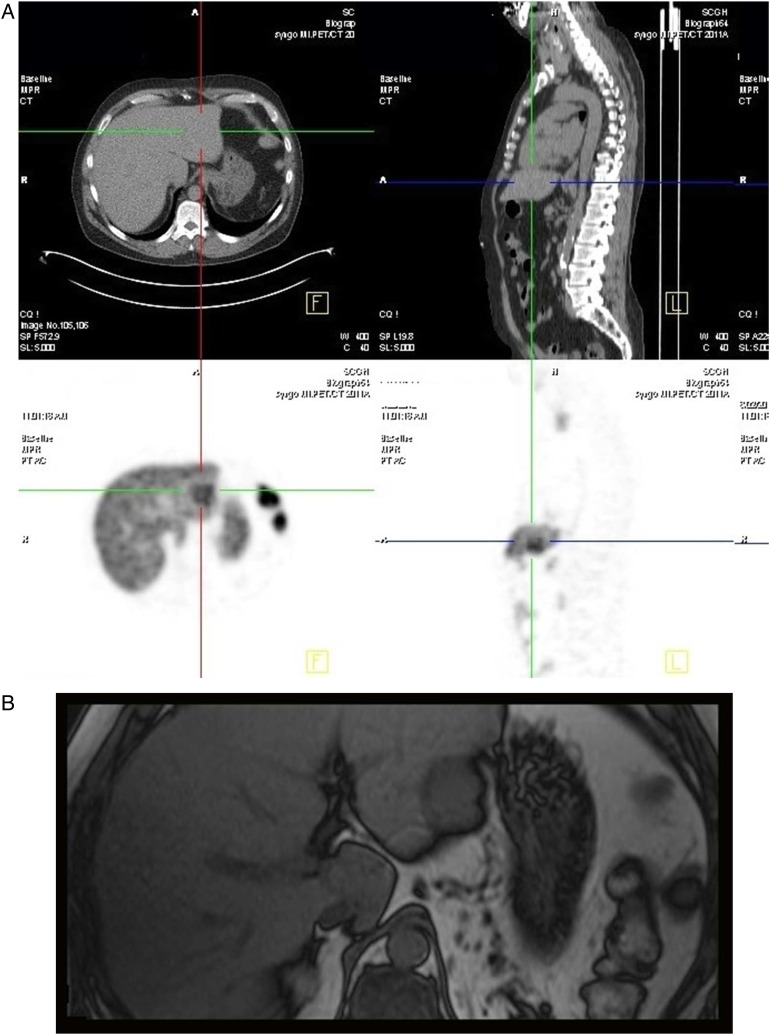
An abdominal CT scan showed an intrahepatic lesion with hypervascularity which was further confirmed by an abdominal ultrasound and MRI which demonstrated a non-cystic irregular lesion in segment 3 measuring approximately 37×46×31 mm with features suggestive of a neuroendocrine tumour (figure 1B). Endoscopy and colonoscopy was performed to exclude a primary neuroendocrine tumour. Both tests were negative. A chromogranin level was abnormally elevated at over 300, consistent with the possible diagnosis of a carcinoid neuroendocrine tumour. A PET octreotide scan was then performed, which showed uptake in the corresponding intrahepatic lesion in segment 3 with moderate intensity (figure 1A).
Figure 1.
(A) Positron emission tomography (PET) octreotide scan showing PET Avid lesion. (B) MRI scan showing irregular lesion in segment 2/3.
Treatment
The patient underwent a left lateral liver segmentectomy for the suspected primary intrahepatic neuroendocrine tumour. During surgery, an intraoperative ultrasound of the liver and careful examination of the abdomen did not detect any other tumours. The patient had a good postoperative recovery and was discharged.
Outcome
The subsequent histopathology of the resected segment revealed a single focus of intrahepatic splenosis with haemorrhage contained in the left lateral segment. The haemorrhage was the likely source of his abdominal pain (figures 2 and 3).
Figure 2.
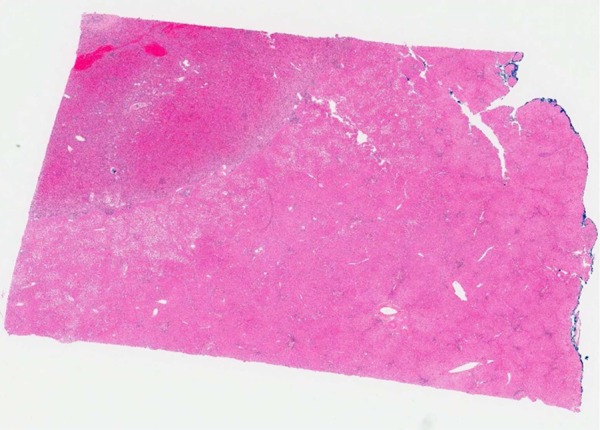
H&E of splenosis.
Figure 3.
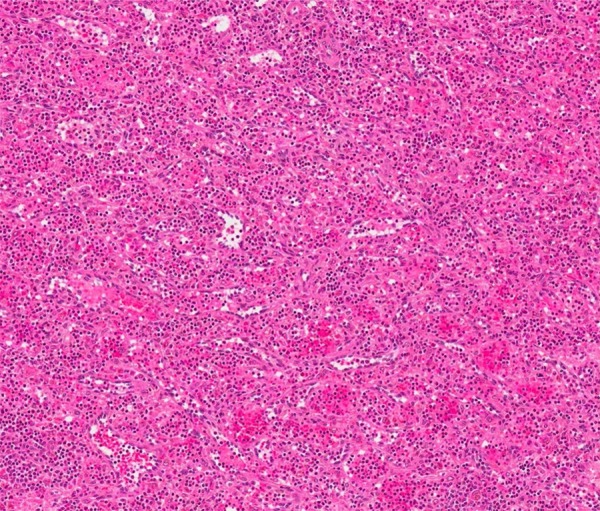
H&E of engorged red pulp.
Follow-up
The patient was followed-up regularly. On review, there was no longer any abdominal pain. The chromogranin levels at follow-up 6 months post-surgery remained elevated. The cause is currently being followed up. One possibility is the use of proton pump inihibitors for the management of gastritis.
Discussion
Splenosis is a benign acquired condition where there is heterotopic, viable splenic tissue. This can occur after splenic rupture by trauma or surgery, with incidence rates reported up to 67%.1–3 In contrast, accessory spleens and splenuncules are ectopic congenital splenic tissue which arise from the left side of the dorsal mesogastrium during the embryological period of development.4 Splenosis most commonly occurs intra-abdominally. Heterotopic splenic tissue, within other organs such as in the liver, pericardium, brain and thoracic cavity has been reported but rarely. Intra-abdominal splenosis is due to autotransplantation that commonly occurs during surgical removal or trauma with intra-abdominal seeding.5
The mechanism by which intrahepatic splenosis occurs is that the splenic erythrocytic progenitor cells enter haematogenously via the portal vein and grow in response to tissue hypoxia.6–8 Most patients present with non-specific complaints or abdominal pain owing to infarction of heterotopic splenic tissue with its limited blood supply. Intrahepatic splenosis is often also misdiagnosed as malignancy.9 10
Heat-damaged technetium-99 m RBC scan or iridium III labelled platelets nuclear scintigraphy scan is often described as the investigation of choice for splenosis.11–13 Modern CT scanning often reveals the number, shape and size, but not the identity of the nodules, while standard MRI is not useful in narrowing the differential diagnosis. This is the first case of octreotide scanning detecting splenosis reported in the literature. PET octreotide scanning utilises Somatostatin receptor (SSTR)-based radio-ligands for the localisation of primary and metastatic neuroendocrine tumours. These ligands have an affinity for the SSTR. Both T-cell and B-cell lymphocytes including monocytes express SSTR. The immune system and its organs including the spleen with its abundance of T and B cells therefore can often be visualised by PET octreotide scanning. There are reports of up to 40% of lymphocytes in the spleen being visualised. 14–19
Learning points.
Splenosis should always be differential for a patient who presents with abdominal symptoms post-traumatic splenectomy.
Splenosis can be positron emission tomography (PET) avid on PET octreotide scanning and mimic a neuroendocrine tumour.
Surgical management for splenosis is only warranted when symptomatic.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Halpert B, Gyorkey F. Lesions observed in accessory spleens of 311 patients. Am J Clin Pathol 1959;32:165–8 [DOI] [PubMed] [Google Scholar]
- 2.Durand DV, Joliot AY, Beaumont X, et al. La splenose: Revue de 117 observations. Gastroenterol Clin Biol 1981;5:758–64 [PubMed] [Google Scholar]
- 3.Losanoff JE, Jones JW. Splenosis after laparoscopic splenectomy. Surg Endosc 2001;15:1497. [DOI] [PubMed] [Google Scholar]
- 4.Brewster DC. Splenosis: report of two cases and review of the literature. Am J Surg 1973;126:14–19 [DOI] [PubMed] [Google Scholar]
- 5.Case Records of the Massachusetts General Hospital Weekly clinico-pathological exercises: case 29. N Engl J Med 1995;333:784–917643887 [Google Scholar]
- 6.Baack BR, Varsa EW, Burgdorf WH, et al. Splenosis. A report of subcutaneous involvement. Am J Dermatopathol 1990;12:585–8 [PubMed] [Google Scholar]
- 7.Rickert CH, Maasjosthusmann U, Probst-Cousin S, et al. A unique case of cerebral spleen. Am J Surg Pathol 1998;22:894–6 [DOI] [PubMed] [Google Scholar]
- 8.Yeh CJ, Chuang WY, Kuo TT. Case report: unusual subcutaneous splenosis occurring in a gunshot wound scar: pathology and immunohistochemical identification. Pathol Int 2006;56:336–9 [DOI] [PubMed] [Google Scholar]
- 9.Menth M, Herrmann K, Haug A, et al. Intra-hepatic splenosis as an unexpected cause of a focal liver lesion in a patient with hepatitis C and liver cirrhosis: a case report. Cases J 2009;2:8335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Short NJ, Hayes TG, Bhargava P. Intraabdominal splenosis mimicking metatatic cancer. Am J Med Sci 2011;341:246–9 [DOI] [PubMed] [Google Scholar]
- 11.Alvarez R, Diehl KM, Avram A, et al. Localization of splenosis using 99m Tc-damaged red blood cell SPECT/CT and intraoperative gamma probe measurements. Eur J Nucl Med Mol Imaging 2007;34:969. [DOI] [PubMed] [Google Scholar]
- 12.Hagan I, Hopkins R, Lyburn I. Superior demonstration of splenosis by heat-denatured Tc-99m red blood cell scintigraphy compared with Tc-99m sulfur colloid scintigraphy. Clin Nucl Med 2006;31:463–6 [DOI] [PubMed] [Google Scholar]
- 13.Schiff RG, Leonidas J, Shende A, et al. The noninvasive diagnosis of intrathoracic splenosis using technetium-99m heat-damaged red blood cells. Clin Nucl Med 1987;12:785–7 [DOI] [PubMed] [Google Scholar]
- 14.Lebtahi R, Cadiot G, Sarda L, et al. Clinical impact of somatostatin receptor scintigraphy in the management of patients with neuroendocrine gastroenteropancreatic tumors. J Nucl Med 1997;38:853–8 [PubMed] [Google Scholar]
- 15.Gibril F, Reynolds JC, Doppmann JL, et al. Somatostatin receptor scintigraphy: its sensitivity compared with that of other imaging methods in detecting primary and metastatic gastrinoma. A prospective study. Ann Intern Med 1996;125:26–34 [DOI] [PubMed] [Google Scholar]
- 16.Cadiot G, Lebtahi R, Sarda L, et al. Preoperative detection of duodenal gastrinomas and peripancreatic lymph nodes by somatostatin receptor scintigraphy. Gastroenterology 1996;111:845–54 [DOI] [PubMed] [Google Scholar]
- 17.Cadiot G, Bonnaud G, Lebtahi R, et al. Usefulness of somatostatin receptor scintigraphy in the management of patients with Zollinger-Ellison syndrome. Gut 1997;41:107–14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mignon M, Jaïs P, Cadiot G, et al. Clinical features and advances in biological diagnostic criteria for Zollinger-Ellison syndrome. In: Mignon M, Jensen RT, eds. Endocrine tumors of the pancreas: recent advances in research and management. Vol 23 of Frontiers of gastrointestinal research. Basel, Switzerland: Karger Publishers, 1995:223–39 [Google Scholar]
- 19.Norton JA, Doppman JL, Jensen RT. Curative resection in Zollinger Ellison syndrome: results of a 10-years prospective study. Ann Surg 1992;215:8–18 [DOI] [PMC free article] [PubMed] [Google Scholar]