Abstract
Pyogenic granuloma (PG) is a kind of inflammatory hyperplastic soft tissue lesion of the oral cavity. The lesion, however, is not related to infection and arise as a reactive growth in response to various stimuli. It has a very high vascularity because of the presence of numerous prominent capillaries. The lesion has a bleeding tendency, even after a minor traumatic episode, such as during mastication. Bleeding may be at times very severe and difficult to control. We present the case of a profusely bleeding young PG in a young teenage child.
Background
Pyogenic granuloma (PG) is a non-neoplastic tumour-like growth of the oral cavity or the skin.1 It is an inflammatory hyperplastic lesion, which is usually considered to be a reactive lesion arising in relation to various stimuli. Initially the lesion was called botryomycosis homoinis and thought to be a botryomycotic infection. However, it is now believed that it is not related to infection. The term ‘pyogenic granuloma’, which is widely used in the literature, is a misnomer because the lesion neither contains pus, nor it represents a granuloma histologically.2 3 The alternative term ‘granuloma telangiectacticum’ was suggested by Cawson et al,4 as the tumour contains numerous blood vessels.
Clinically, PG is a soft, smooth or lobulated exophytic lesion, which manifests as a small, red erythmatous papule on a pedunculated or sessile base.1 2 PG has a higher incidence in women (1.5:1 ratio) and occurs most frequently in the second and third decades of life.5 6 The most common site of occurrence of PG is gingiva, followed by lips, tongue and buccal mucosa. No radiographic findings are present in PG. The final diagnosis of PG can be established through histological examination only.7
The vascularity of PG is very high as it is composed predominantly of hyperplastic granulation tissue in which capillaries are prominent.7 Owing to its high vascularity, it may bleed spontaneously after a small traumatic injury. We present a case report of PG in a teenage girl, who reported to us with gingival growth and overnight bleeding.
Case presentation
A 14-year-old female patient reported to the department of paediatric and preventive dentistry, with the complaint of severe bleeding in her mouth, since overnight, in her posterior left side of the upper jaw. The swelling was evident for last 2 weeks and progressively increased in size. The medical history of the patient was non-significant. Extraoral examination of the patient revealed no noticeable findings. Intraoral examination revealed the presence of a large bleeding soft tissue lesion (figure 1). On the first clinical impression, the lesion appeared to be highly vascular. The saliva and blood were sucked with the help of suction evacuation. Upon careful examination of the lesion, it was sessile and originated from the buccal and lingual gingival tissues in relation to the permanent left maxillary second molar.
Figure 1.

Intraoral view showing bleeding soft tissue lesion.
Investigations
Prior to excisional biopsy, routine blood examination was advised. All the blood counts were within normal limits except a slightly less haemoglobin concentration (10 gm%, Wintrobe method).
Differential diagnosis
Differential diagnosis of PG includes peripheral giant cell granuloma, haemangioma, pregnancy tumour, peripheral ossifying fibroma, conventional granulation tissue, inflammatory gingival hyperplasia, metastatic cancer, Kaposi's sarcoma, angiosarcoma, bacillary angiomatosis and non-Hodgkin's lymphoma. Since the lesion in the present case was highly vascular, as evident clinically, a provisional diagnosis of PG and oral haemangioma was considered. Oral haemangiomas, however, are mostly located on the tongue, are multilocular and bluish-red in colour.8 The final diagnosis cannot be established until the histopathological examination is performed. In the present case as well, the final diagnosis could have been established only after the histopathological report.
Treatment
Excisional biopsy of the soft tissue lesion was performed under local anaesthesia and sutures were given. The excised tissue (figure 2) was sent for histopathological examination which showed fibrovascular connective tissue exhibiting dense inflammatory infiltrate predominantly plasma cells, lymphocytes, neutrophils and foam cells (figure 3). The tissue also showed numerous small and large blood vessels, endothelial proliferation and extravasated red blood cells, with connective tissue lined by fibrous capsule (figure 4). Thus, based on the clinical and histopathological examinations, a definitive diagnosis of pyogenic granuloma was established.
Figure 2.

Excised lesion.
Figure 3.
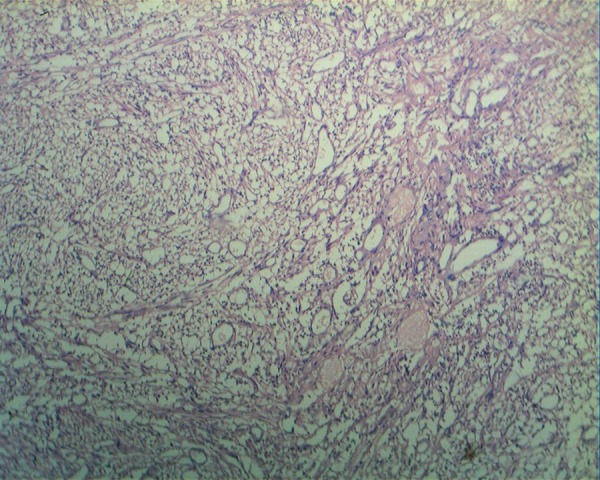
Microphotograph showing inflammatory infiltrates predominantly plasma cells, lymphocytes and neutrophils and foam cells (H&E ×10).
Figure 4.
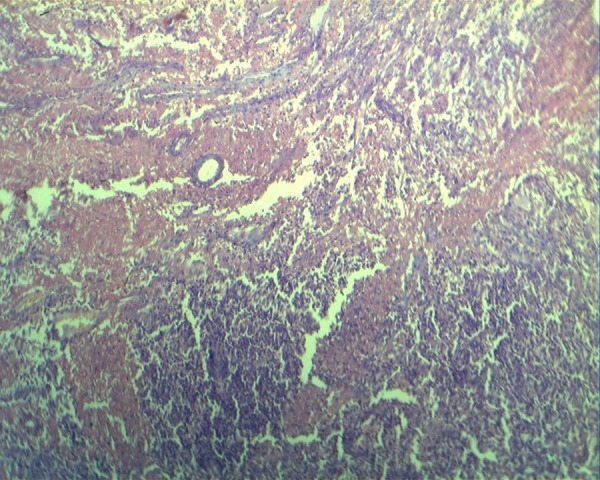
Microphotograph showing numerous small and large blood vessels, endothelial proliferation and extravasated red blood cells (H&E ×10).
Outcome and follow-up
The patient was followed up till next day for any postoperative haemorrhage. However, no bleeding was obvious from the surgical site. The patient was called 1 week after the surgery for removal of sutures. The healing was uneventful and the patient was satisfied with the results. Thorough scaling and curettage were performed, as they may serve as potential causative agents for recurrence. The patient was periodically followed up for the next 1 year. During this time, the lesion did not recur.
Discussion
Oral pyogenic granuloma is a mucosal vascular hyperplasia, the exact etiopathogenesis of which is still debatable. It is however, usually considered as a reactive lesion, which is thought to arise in response to various stimuli such as chronic low-grade local irritation,1 traumatic injury, hormones,9 drugs,10 viral11 and bacterial infections.12 In approximately one-third cases, the history of trauma is present.13 Poor oral hygiene has also been noticed to be associated with PGs by some authors.1 3 8 The pregnancy tumour, which occurs in up to 5% pregnancies because of hormonal changes, is considered a variant of PG.4 The lesion, however, does not contain pus, and seems to be unrelated to the infection, as was thought earlier. Some drugs, for example, cylosporin, have been suggested to have an important role in the genesis of PG.14 In the present case, the possible aetiology of PG was the presence of calculus, which acted as the persistent irritant, leading to the origin of PG. An unnoticed traumatic injury may also be the aetiological factor. Any history of drug intake, however, was not present.
Although haemorrhage is not an uncommon finding in PG, but in the present case the haemorrhage was very severe. Because of the high vascularity of the lesion, even a minor trauma can cause a considerable haemorrhage. The chances of haemorrhage are more in young PGs because of the abundant presence of hyperplastic granulation tissue and prominent capillaries. As the lesion becomes older, they tend to become more collagenised.1 The colour of the lesion changes with age, young lesions are red to purple whereas older lesions are pink. In the present case, the lesion was young, with a rapid growth and appeared deep red in colour. In the present case, the lesion bled overnight, this could have led to serious consequences. The patient belonged to a remote place, where she visited a local hospital in the night. She was, however, not given any treatment and was referred to our institute for the diagnosis and management. No previous history of spontaneous bleeding or excessive bleeding after minor trauma could be found. However, an unnoticed trauma during mastication could have led to the rupture of the capillaries, leading to profuse bleeding.
Histologically, the lesion shows a highly vascular proliferation resembling granulation tissue.1 The lesion often exhibited numerous small and large blood vessels, separated by less vascular fibrotic septa. One of the consistent findings in PG is the presence of polymorphs and chronic inflammatory cells throughout the oedematous stroma, with microcyst formation.8 The major bulk of the lesion is formed by a non-lobulated mass of angiomatous tissue.15 The histological findings of this case were consistent with those previously reported in the literature.
Treatment of PG depends on the size and location of the lesion. Excisional biopsy is the treatment of choice in the majority of the cases, however, other treatment alternatives can also be considered. In cases of larger lesions, an incisional biopsy is indicated to avoid deformity. Neodymium-doped yttrium aluminum garnet laser has been indicated to surgically excise the lesion owing to its superior coagulation properties and lesser intraoperative bleeding. Other conservative treatment alternatives include cryosurgery, electrodessication, an injection of absolute ethanol,16 and sodium tetradecyl sulfate sclerotherapy.17 In the present case, excision was considered the treatment of choice, as the lesion was moderate in size, accessible and it was possible to completely excise the lesion.
After the treatment is performed, careful oral hygiene maintenance is mandatory to prevent recurrence. Thorough oral prophylaxis, including removal of dental plaque and calculus should be carried out without fail after the management of PG. Any source of chronic irritation to soft tissues such as faulty restorations with overhanging margins, sharp cusp tips and fractured teeth with sharp margins should also be treated. The patient should be instructed to maintain oral hygiene, to use the soft toothbrush, and periodic oral follow-up examination. The present case was followed up to 1 year. No recurrence of the lesion was obvious during that period.
Oral PG, a benign slow-growing tumour-like growth in the oral cavity, may sometimes have serious consequences because of its structural characteristics and bleeding tendency, as was seen in the present case.
Learning points.
Pyogenic granuloma (PG) is an inflammatory hyperplastic soft tissue lesion of the oral cavity which arise as a reactive growth in response to various stimulating factors.
The lesion tends to bleed easily because of its very-high vascularity and presence of numerous prominent capillaries.
Treatment of PG depends on the size and location of the lesion. After the treatment is performed, any source of chronic infection should be removed to prevent recurrence.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Neville BW, Damm DD, Allen CM, et al. Oral & maxillofacial pathology. 2nd edn Philadelphia: WB Saunders, 2002:437–95 [Google Scholar]
- 2.Eversole LR. Clinical outline of oral pathology: diagnosis and treatment. 3rd edn Hamilton: BC Decker, 2002:113–14 [Google Scholar]
- 3.Regezi JA, Sciubba JJ, Jordan RCK. Oral pathology: clinical pathologic considerations. 4th edn Philadelphia: WB Saunders, 2003:115–16 [Google Scholar]
- 4.Cawson RA, Binnie WH, Speight PM, et al. Lucas Pathology of tumors of oral tissues. 5th edn Missouri: Mosby, 1998:252–4 [Google Scholar]
- 5.Aguilo L. Pyogenic granuloma subsequent to injury of primary tooth: a case report. Int J Paed Dent 2002;12:438–41 [DOI] [PubMed] [Google Scholar]
- 6.Shenoy SS, Dinkar AD. Pyogenic granuloma associated with bone loss in an eight-year-old child: a case report. J Indian Soc Pedod Prev Dent 2006;24:201–3 [DOI] [PubMed] [Google Scholar]
- 7.Jafarzadeh H, Sanatkhani M, Moshtasham N. Oral pyogenic granuloma: a review. J Oral Sci 2006;48:167–75 [DOI] [PubMed] [Google Scholar]
- 8.Greenberg MS, Glick M. Burket's oral medicine: diagnosis and treatment. 10th edn Hamilton: BC Decker, 2003:141–2 [Google Scholar]
- 9.Mussalli NG, Hopps RM, Johnson NW. Oral pyogenic granuloma as a complication of pregnancy and the use of hormonal contraceptives. Int J Gynaecol Obstet 1976;14:187–91 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Miller RA, Ross JB, Martin J. Multiple granulation tissue lesions occurring in isotretinoin treatment of acne vulgaris—successful response to topical corticosteroid therapy. J Am Acad Dermatol 1985;12:888–9 [DOI] [PubMed] [Google Scholar]
- 11.Lin RL, Janniger CK. Pyogenic granuloma. Cutis 2004;74:229–33 [PubMed] [Google Scholar]
- 12.Bhaskar SN, Jacoway JR. Pyogenic granuloma: clinical features, incidence, histology, and result of treatment-Report of 242 cases. J Oral Surg 1966;24:391–8 [PubMed] [Google Scholar]
- 13.Pilch BZ. Head and neck surgical pathology. 1st edn Philadelphia: Lippincott Williams & Wilkins, 2001:389–90 [Google Scholar]
- 14.Lee L, Miller PA, Maxymiw WG, et al. Intraoral pyogenic granuloma after allogeneic bone marrow transplant. Report of three cases. Oral Surg Oral Med Oral Pathol 1994;78:607–10 [DOI] [PubMed] [Google Scholar]
- 15.Kamal R, Dahiya P, Puri A. Oral pyogenic granuloma: various concepts of etiopathogenesis. J Oral Maxillofac Pathol 2012;16:79–82 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ichimiya M, Yoshikawa Y, Hamamoto Y, et al. Successful treatment of pyogenic granuloma with injection of absolute ethanol. J Dermatol 2004;31:342–4 [DOI] [PubMed] [Google Scholar]
- 17.Moon SE, Hwang EJ, Cho KH. Treatment of pyogenic granuloma by sodium tetradecyl sulfate sclerotherapy. Arch Dermatol 2005;141:644–6 [DOI] [PubMed] [Google Scholar]


