Abstract
Non-union of a proximal clavicle fracture is rare. When it does occur, it poses a difficult problem causing severe pain and shoulder impairment that must be dealt with surgically. We report a 29-year-old woman who suffered a proximal clavicle fracture and received plate and screws fixation. Six months later, after constant pain and a diminished range of shoulder motion, she sought help at our clinic and was diagnosed with symptomatic non-union. Reconstruction with bone graft and interosseous sutures was performed in vain as pain persisted and follow-up radiograph showed no healing. A salvage procedure with partial claviculectomy was then carried out. The patient has been pain free after 3.5 years of follow-up, a full range of motion and is quite satisfied with the cosmetics. This outcome demonstrates that claviculectomy can be used successfully in a clinical situation where restoration of clavicular non-union fails.
Background
Most published articles about partial claviculectomy have focused its use on tumours, arthritis, dislocation or infection. We present a rare case report describing this particular method for treatment of non-union of proximal clavicle fracture following failures of two reconstructive procedures.
Case presentation
The patient is a 29-year-old woman who has been visiting the pain clinic in our hospital. According to her statement, she was beaten by her boyfriend about 6 months ago and suffered a proximal clavicle fracture. She received surgery via open reduction and internal fixation with plate and screws at another local hospital and has been complaining of persistent clavicular pain ever since. She describes the pain as sharp and severe, and this has led to multiple visits to the emergency department for intramuscular analgesic injections. In addition, she has shoulder weakness and hears a clicking sound over the clavicle when she moves, which affects her daily activities. Most importantly, even though no deformity or neurovascular deficits exist, she is dissatisfied cosmetically with the protuberance over her clavicle due to evident skin tenting from the prostheses.
Investigations
She was then referred to the orthopaedics clinic, where physical examination confirmed tenderness and pain over the sternoclavicular area with visible skin tenting. Radiograph revealed a non-union of the proximal clavicle with loosening of the prostheses (figure 1). After discussing the various treatment options with the patient, reconstruction of the clavicle without insertion of any metallic implants was decided because she did not want to see any prominence on her anterior chest.
Figure 1.
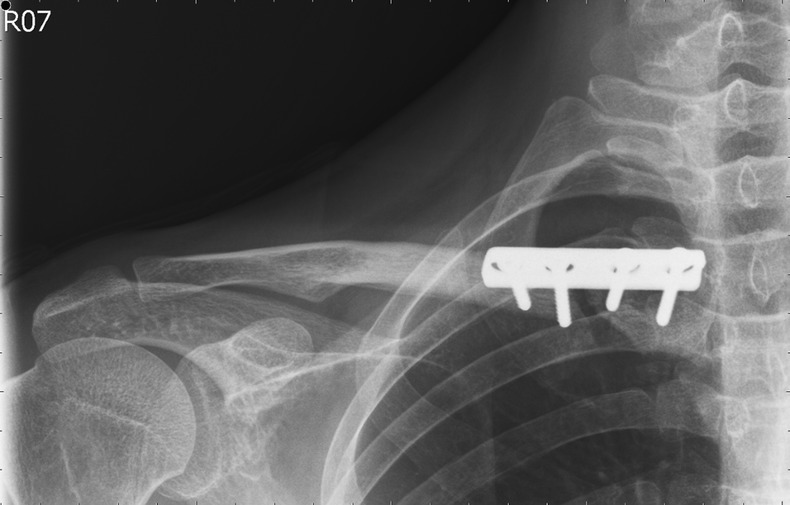
Radiograph of the right clavicle 6 months after primary surgery showing non-union at the proximal end with loosening of the prostheses.
Treatment
During surgery, the loosened plate and screws were removed and the fractured site thoroughly debrided. There was no evidence of callus formation and intermittent fragments were missing from the fracture site. Allomatrix bone graft (Wright, Arlington, Tennessee, USA) was then placed for structural support and the ends of the clavicle were then fixated interosseously with multiple sutures (Ethibond: Ethicon, Somerville, New Jersey, USA; FiberWire: Arthrex, Naples, Florida, USA). Postoperative radiograph showed good reduction and alignment (figure 2). Her shoulder was immobilised in a shoulder sling and she was only allowed to use the hand with her elbow by her side for simple daily tasks. However, when she returned 2 weeks later, the sling had been taken off and she again complained of the same severe pain over the same area. Even though swelling was evident, no signs of infection were present and inflammatory markers such as the erythrocyte sedimentation rate and C reactive protein were within normal range. In addition, precautionary radiograph did not show any marked displacement of the previously reduced fracture. The patient was sent home and told to wear the shoulder sling for another 6 weeks.
Figure 2.
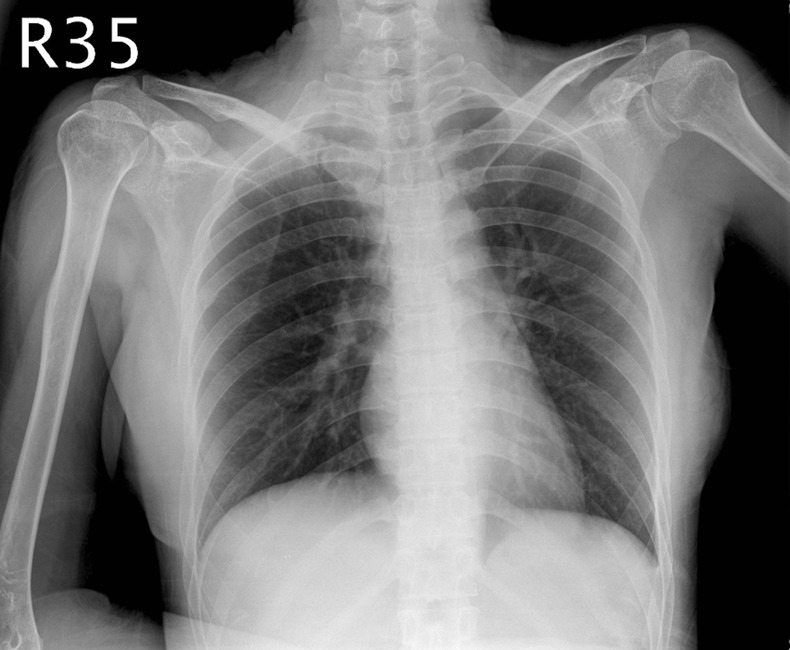
Radiograph after removal of the prostheses and fixation of the non-union with interosseous sutures and bone graft.
Outcome and follow-up
When the patient returned for her postoperative 2-month follow-up, she confessed to having visited the pain clinic on more than one occasion for analgesic injections due to recurring pain. Radiograph taken at this time revealed noticeable bone resorption at the fracture site with no evidence of osseous regeneration (figure 3). After explaining the lack of healing to the patient, the option of a salvage procedure via partial claviculectomy was explained and accepted by the patient. Once the fibrous tissue was removed around the fracture site, approximately 3.5 cm of the proximal clavicle was resected. Postoperative radiograph showed proper alignment of the clavicle compared to the contralateral side and the patient was discharged a few days later.
Figure 3.
Radiograph at 2 months after the secondary surgery revealing evident bone resorption at the previous fracture site with no osseous regeneration.
During subsequent follow-ups, the recurring pain gradually subsided. And at the most recent visit at 3.5 years postpartial-claviculectomy, the patient has been pain free and displays a full range of shoulder motion without loss of motor strength. Cosmetically, there is no tenting of the skin, the shoulders appear evenly aligned, and there is no clinical evidence of bony crepitation from the resected site. Radiograph shows good alignment of the remaining clavicle with about 0.5 cm of osseous regeneration visible (figure 4).
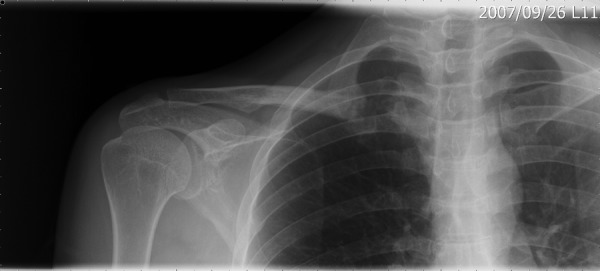
Figure 4.

Radiograph at 3.5 years after partial claviculectomy showing good alignment and symmetry of the clavicles bilaterally.
Discussion
In general, proximal clavicle fractures can be treated non-operatively except for open fractures, neurovascular involvement, threatened overlying skin and fractures with displacement1–4; however, about 8% of these patients still develop non-union.5 When this occurs, severe pain and functional impairment of the shoulder girdle result. Despite restorative efforts through either reconstruction or salvage procedures, non-union poses a great challenge to surgeons as it is often associated with high complication and failure rates.
On the basis of the past reports and our experience, surgery for proximal clavicle fractures tends to fail for two reasons. First, inadequate initial immobilisation along with early shoulder motion usually transfers the weight and tension from the shoulder girdle to the medial third of the clavicle and the sternoclavicular joint, thereby causing instability of the prostheses.6 Second, most proximal fragments are usually short and their bone stock remains insufficient for fixation by any type of prosthesis.3 Our patient admittedly took off her shoulder sling early and began moving her shoulder; and the remaining medial fragment from her fracture only measured about 2.5 cm, far too short for stable fixation. Both of these factors can contribute directly to improper healing and thereby results in non-union.
Non-union has been defined as the lack of proper healing either clinically or radiographically between 6 and 9 months after the injury.7 On the contrary, some clinicians believe that a fracture should be considered non-united if no healing has occurred after 4 months of injury.8 Regardless of time, all patients with non-union present pain as their most prominent symptom. Other forms of disability may include altered shoulder mechanics or dysfunction such as drooping, stiffness or weakness of the shoulder. In addition, some patients may complain of a limited sense of motion or crepitation on the injured clavicle.7 8 Most importantly, the loss of reduction from improper healing, along with the aforementioned symptoms, warrant operative treatment which is mandatory for much needed relief.
In general, treatment for symptomatic non-union can be divided into two major categories: reconstruction and salvage.9 Because the clavicle serves and participates in several vital functions, and damage results in significant disability, it is of utmost importance to restore and preserve its length and continuity when treating a clavicular non-union. Reconstruction includes a diverse range of methods, but wire or plate fixation and interosseous sutures represent the mainstream of stabilisation. While success has been confirmed by many, failures have been just as frequent with resultant recurrent pain, loss of reduction, implant migration, poor cosmetics, malunion, non-union and even death.1–4 10 11 When all attempts to achieve union for non-united symptomatic clavicular fracture have been made and failed, surgeons must decide whether to reduce and stabilise the clavicle again, or proceed with resection. Therefore, it is reasonable to inform patients that after reconstruction they can anticipate improved outcome. However, they should be warned that up to 8% might not heal properly.12
In contrast to reconstruction which aims to achieve bone union in an anatomic position, salvage procedure attempts to alleviate symptoms and deformities without achieving bone union.7 Although Gurd first described claviculectomy as early as 1912, it is a rare procedure usually reserved for conditions such as tumour, vascular compression or injury, arthritis or subluxation/dislocation of the sternoclavicular joint, osteomyelitis and symptomatic malunion and non-union.13 Although few cases are documented and long-term follow-ups are lacking, most have yielded fair results. However, some patients continued to complain of pain and clicking at the resected end, while others have expressed dissatisfaction about the cosmetic appearance of a prominence in the anterior chest region.14 Through a literature search, Acus et al11 were found to have published the largest series of proximal clavicle excisions up to date, although none of the 15 patients underwent the procedure because of symptomatic non-union of clavicular fracture. After an average follow-up of 4.6 years, 14 of the 15 patients received significant pain relief from the operation, all displayed a full range of motion of their operated shoulders, and all were satisfied with their cosmetics. The authors believe that one patient who had recurrent pain after the surgery can blame the result on the massive osseous regeneration (3.2 cm) on the resected end. But overall, patients undergoing partial claviculectomy can expect remarkable pain relief, full range of motion, and acceptable cosmetics.
Although proximal clavicle fractures can either be managed conservatively or surgically, they should always be treated to avoid potential healing complications. When non-union does occur, it is usually symptomatic and causes significant disability. Although treatment varies for clavicular non-union, emphasis should be placed on restoring normal shoulder mechanics and function. If reconstruction fails, as with our patient, then a salvage procedure such as partial claviculectomy can prove to be a viable secondary option for accomplishing good functional and cosmetic results.
Learning points.
Surgery for proximal clavicle fractures tends to fail because of inadequate initial immobilisation, early shoulder motion and short remaining fragments that have insufficient bone stock for fixation.
Non-union occurs in about 8% of all proximal clavicle fractures, with pain being the most prominent symptom.
Treatment for clavicular non-union should always emphasise on restoring normal shoulder mechanics and function and preserving its length and continuity; however, it often results in complications and failure.
If reconstruction fails, salvage procedure such as partial claviculectomy can prove to be a viable secondary option for accomplishing good functional and cosmetic results.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Throckmorton T, Kuhn JE. Fractures of the medial end of the clavicle. J Shoulder Elbow Surg 2007;16:49–54 [DOI] [PubMed] [Google Scholar]
- 2.Low AK, Duckworth DG, Bokor DJ. Operative outcome of displaced medial-end clavicle fractures in adults. J Shoulder Elbow Surg 2008;17:751–4 [DOI] [PubMed] [Google Scholar]
- 3.Bartonicek J, Fric V, Pacovsky V. Displaced fractures of the medial end of the clavicle: report of five cases. J Orthop Trauma 2010;24:e31–5 [DOI] [PubMed] [Google Scholar]
- 4.Van der Meijden OA, Gaskill TR, Millet PJ. Treatment of clavicle fractures: current concepts review. J Shoulder Elbow Surg 2012;21:423–9 [DOI] [PubMed] [Google Scholar]
- 5.Robinson CM, Court-Brown CM, McQueen MM, et al. Estimating the risk of nonunion following nonoperative treatment of a clavicular fracture. J Bone Joint Surg Am 2004;86:1359–65 [DOI] [PubMed] [Google Scholar]
- 6.Al-Yassari G, Hetzenauer M, Tauber M, et al. Novel method to treat sterno-clavicular joint instability and medial clavicle fracture symptomatic nonunion. J Shoulder Elbow Surg 2009;18:553–5 [DOI] [PubMed] [Google Scholar]
- 7.Jones GL, McCluskey GM, III, Curd DT. Nonunion of the fractured clavicle: evaluation, etiology, and treatment. J South Orthop Assoc 2000;9:3–54 [PubMed] [Google Scholar]
- 8.Mouzopoulos G, Morakis E, Stamatakos M, et al. Complications associated with clavicular fracture. Orthop Nurs 2009;28:217–24 [DOI] [PubMed] [Google Scholar]
- 9.Simpson NS, Jupiter JB. Clavicle nonunion and malunion: evaluation and surgical management. J Am Acad Orthop Surg 1993;4:1–8 [DOI] [PubMed] [Google Scholar]
- 10.Kim KC, Shin HD, Cha SM. Surgical treatment of displaced medial clavicle fractures using a small T-shaped plate and tension band sutures. Arch Orthop Trauma Surg 2011;131:1673–6 [DOI] [PubMed] [Google Scholar]
- 11.Acus RW, Bell RH, Fisher DL. Proximal clavicle excision: an analysis of results. J Shoulder Elbow Surg 1995;4:182–7 [DOI] [PubMed] [Google Scholar]
- 12.Der Tavitian J, Davison JNS, Dias JJ. Clavicular fracture non-union surgical outcome and complications. Injury 2002;33:135–43 [DOI] [PubMed] [Google Scholar]
- 13.Krishnan SG, Schiffern SC, Pennington SD, et al. Functional outcome after total claviculectomy as a salvage procedure. A series of six cases. J Bone Joint Surg Am 2007;89:1215–19 [DOI] [PubMed] [Google Scholar]
- 14.Middleton SB, Foley SJ, Foy MA. Partial excision of the clavicle for nonunion in National Hunt Jockeys. J Bone Joint Surg Br 1995;77:778–80 [PubMed] [Google Scholar]


