Abstract
Aims
The aim of this study was to examine the short-term and long-term cumulative risk of coronary heart disease (CHD) and stroke separately based on age, sex, smoking status, systolic blood pressure, and total serum cholesterol.
Methods and results
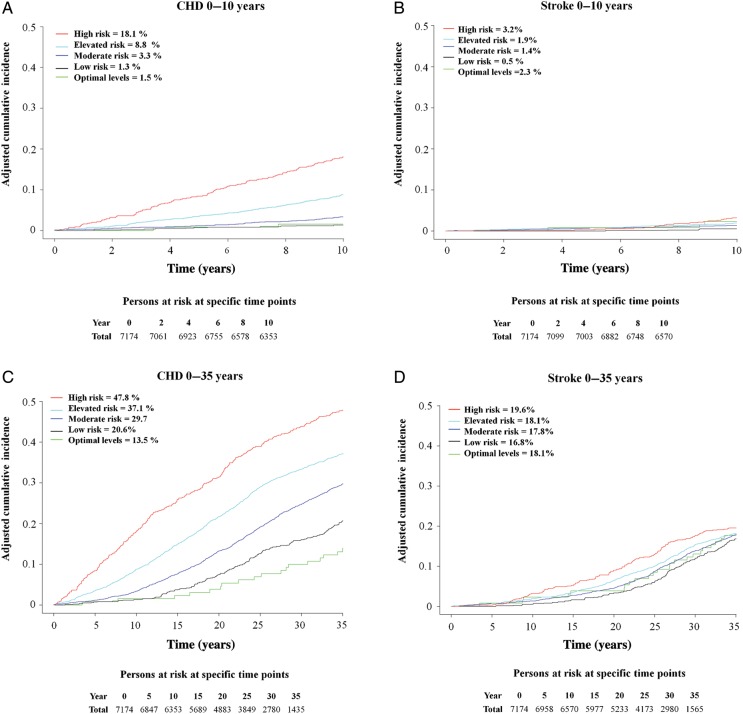
The Primary Prevention Study comprising 7174 men aged between 47 and 55 free from a previous history of CHD, stroke, and diabetes at baseline examination (1970–73) was followed up for 35 years. To estimate the cumulative effect of CHD and stroke, all participants were stratified into one of five risk groups, defined by their number of risk factors. The estimated 10-year risk for high-risk individuals when adjusted for age and competing risk was 18.1% for CHD and 3.2% for stroke which increased to 47.8 and 19.6%, respectively, after 35 years. The estimates based on risk factors performed well throughout the period for CHD but less well for stroke.
Conclusion
The prediction of traditional risk factors (systolic blood pressure, total serum cholesterol, and smoking status) on short-term risk (0–10 years) and long-term risk (0–35 years) of CHD of stroke differs substantially. This indicates that the cumulative risk in middle-aged men based on these traditional risk factors can effectively be used to predict CHD but not stroke to the same extent.
Keywords: Score models, Stroke, CHD, Risk prediction, Risk factors
Introduction
Today, cardiovascular disease (CVD) is one of the leading causes of mortality, disability, and morbidity in adults worldwide.1 To identify persons at an increased risk of CVD, several score systems have previously been developed.2 The European Society of Cardiology (ESC) has created a systematic coronary risk evaluation (SCORE system) chart based on five well-established risk factors: age, sex, total serum cholesterol (s-cholesterol), systolic blood pressure (SBP), and smoking.3 In contrast to the Framingham risk score,4,5 which was based on a single North-American community, the ESC model is derived from 12 large European cohort studies. This would make the ESC model more reliable and applicable to European conditions. However, the European score model uses only fatal CVD events which may limit the predictive power substantially. In addition, various risk models predict only the 10-year risk for a population aged up to 65 years, whereas the majority of CVD events occur in elderly people which may lead to underestimation of the real importance of these risk factors.6 Finally many risk models focus on both coronary heart disease (CHD) and stroke simultaneously, and these two outcomes may differ considerably in predictability.
To address these issues, we investigated the differences between the short-term and long-term (10 year and 35 year) cumulative risk of developing either a first time CHD or stroke, based on the risk factors used by the ESC SCORE model in 7174 middle-aged men from Gothenburg in Sweden who were followed for 35 years. Additionally, we estimated the long-term impact of individual risk factors for both CHD and stroke separately.
Methods
Study population
The Multifactor Primary Prevention Study was first established in 1970 and was designed as an intervention trial. It included all men in Gothenburg born between 1915 and 1925 (with the exception of 1923). A third of the men were randomly selected for the intervention group which comprised 10 000 men, with interventions directed against smoking, hypertension, and hypercholesterolaemia.7 Additionally, two control groups with 10 000 men each were established. For the intervention group that forms the basis for this investigation, a postal questionnaire with an invitation letter was sent to all the men. Those who responded (n= 7495) were invited for a first baseline screening in 1970–73. After 4 and 10 years, re-examinations were performed in a random sample (20%) of both the intervention and control groups. No significant differences were found in risk factor levels [e.g. s-cholesterol, blood pressure (BP), and smoking status], cardiovascular, cancer, or all-cause mortality between the intervention and control groups. Consequently, any changes observed in the intervention group occurred to the same extent as in the general population. Thus, the present study group is considered to be representative of the background population in the city. Further details of study design and criteria for entering the study have previously been described.7
The present study uses baseline information from those individuals in the intervention group with no previous history of CHD, stroke, or diabetes and with a complete data set, leaving a total of 7174 men aged 47–55 years (mean age 51). In addition, all participants gave their informed consent to participate in the study. The study complies with the Declaration of Helsinki and was approved by the Ethics Committee for Medical Research at University of Gothenburg.
Definition of risk factors
In the current study, CVD is defined as CHD (myocardial infarction) and stroke. To estimate the risk of developing a CVD event, the following major risk factors were used: SBP, diastolic blood pressure (DBP), s-cholesterol, hypertension, antihypertensive treatment, and smoking status at baseline. All screening examinations were performed during the afternoon, including weight, height, and BP (taken after 5 min rest with the subject seated). Hypertension was defined as SBP >140 or DBP >90 or receiving antihypertensive treatment. For the determination of s-cholesterol, samples were taken after ≥2 h fasting and s-cholesterol concentration was determined according to standard laboratory procedures. Information on smoking habits and previous history of CHD or stroke was collected from the postal questionnaire. Non-smokers were defined as either never or ex-smoker (>3 months) and the rest as current smokers.
Definition of risk groups
The following five risk groups were created based on the ESC SCORE chart for men aged 50 using the risk factors SBP, s-cholesterol, and smoking status.3 All participants were stratified into one of five risk groups based on their number of risk factors at baseline (1970–73). According to the ESC SCORE chart, optimal levels for SBP and s-cholesterol are set to 120 mmHg and 4 mmol/L. However, at the time of baseline investigation, the mean BP (SBP and DBP) were high in comparison with levels of today. To create a sufficiently large group, optimal levels for SBP and s-cholesterol was defined at higher cut-off points than would currently have been the case.
Optimal risk: SBP <140 mmHg without antihypertensive treatment, s-cholesterol <5.0 mmol/L and non-smoker.
Low risk: SBP 140–159 mmHg without antihypertensive treatment and/or s-cholesterol 5.0–5.9 mmol/L and non-smoker.
Moderate risk: SBP ≥160 mmHg or antihypertensive treatment or s-cholesterol ≥6.0 mmol/L or current smoker.
Elevated risk: SBP ≥160 mmHg or antihypertensive treatment and/or s-cholesterol ≥6.0 mmol/L and/or current smoker.
High risk: SBP ≥160 mmHg or antihypertensive treatment, s-cholesterol ≥6.0 mmol/L and current smoker.
Men with low risk were selected as the reference group.
Follow-up procedure
The follow-up was extended through 2008 with endpoints of first time CHD and stroke events registered from several sources. For individuals up to 65 years of age, both CHD and stroke events were recorded using criteria from the local CHD and stroke registers.8,9 Case records for all hospital diagnoses were checked manually by one nurse and one medical technician from the start of the study. Furthermore, all hospital discharges from Gothenburg have been reported to the national register since 1970 (except for 1976 due to legislative changes). A file of all participants of the study was run against the national register of hospital discharges 1970–2008. In addition, all men in the study were matched against the Swedish Cause of Death register.
The International Classification of Disease (ICD) was used to identify CHD and stroke events and for this purpose ICD version 8 was used until 1986, ICD-9 from 1987 to 1996 and the last revision ICD-10 was used from 1997. In this present study, both non-fatal and fatal events were considered. For CHD, the following discharge codes were used: ICD-8 and ICD-9 code 410 and ICD-10 code I21. For stroke: ICD-9 codes 431, 433, 434, and 436 and ICD-10 codes I61-I64 were used.
Statistical analysis
Statistical analyses were performed with the SAS (ver. 9.2) and R statistical system (ver. 2.15.1). Descriptive statistics with baseline characteristics are presented for each risk factor and risk groups. The individual risk factors were categorized into different levels where the age-adjusted incidence rate ratios (IRRs) were calculated for stroke and CHD, respectively.
In long-term follow-up studies, it is important to apply a statistical model which accounts for competing events (e.g. death as a competing risk) that could potentially end the follow-up for a study subject in such a way that violates the random censoring assumption when calculating risk differences in risk factors. To calculate the risk of stroke and CHD, a modified Cox regression analysis as described by Fine JP and Gray RJ was used in a competing risk setting.10 From the competing risk regression analysis the subdistribution hazard ratio (SHR) with two-sided 95% confidence intervals (CI) was estimated for individual risk factors and risk groups. All estimates were adjusted for age where each categorized risk level (based on the different levels of the categorized risk factors) was compared with the corresponding reference group. In addition, both the short-term (0–10 year) and long-term (0–35 year) cumulative incidence (cuminc) curves were estimated. The R package ‘cmprsk’ which is publicity available at the R archive network site (http://cran.r-project.org/ was used to calculate the SHR and cuminc).10–12
Results
Long-term effect of individual risk factors
Among the 7174 men in the study, 2417 (33.7%) experienced a first CHD event and 1335 (18.6%) a first stroke over the 35-year follow-up. In total, 3752 (52.3%) of the men experienced a CVD event over the 35-year follow-up. The distribution of risk factors and groups at baseline is outlined in Table 1.
Table 1.
Baseline characteristics of the study population
| Mean (SD)a | Number of men, n = 7174 (% of total) | |
|---|---|---|
| Age (years) | 51.5±2.3 | |
| S-cholesterol levels | ||
| <5.0 mmol/L | 6.5±1.1 | 703 (9.8) |
| 5.0–5.9 mmol/L | 1986 (27.7) | |
| 6.0–6.9 mmol/L | 2364 (32.9) | |
| ≥7.0 mmol/L | 2121 (29.6) | |
| SBP | ||
| <140 mmHg | 148.5±21.8 | 2552 (35.6) |
| 140–159 mmHg | 2573 (35.9) | |
| ≥160 mmHg | 2049 (28.6) | |
| Smoking habits | ||
| Non-smoker | 3577 (49.9) | |
| Smoker | 3597 (50.1) | |
| Hypertension | ||
| Non-hypertensive | 2171 (30.3) | |
| Hypertensive | 5003 (69.7) | |
| Antihypertensive medication | 367 (5.1) | |
| Risk groupsb | ||
| Optimal risk | 130 (1.8) | |
| Low risk | 842 (11.7) | |
| Moderate risk | 2867 (40.0) | |
| Elevated risk | 2645 (36.9) | |
| High risk | 690 (9.6) | |
aSD, standard deviation.
bOptimal risk: SBP ≤140 mmHg without antihypertensive treatment, s-cholesterol <5.0 mmol and non-smoker; low risk: SBP = 140–159.9 mmHg without antihypertensive treatment, s- cholesterol 5.0–5.59 mmol, and non-smoker; moderate risk: SBP ≥160 mmHg or antihypertensive treatment or s-cholesterol ≥6.0 mmol/L or current smoker; elevated risk: SBP ≥160 mmHg or antihypertensive treatment and/or s-cholesterol ≥6.0 mmol/L, and/or current smoker; high risk: SBP ≥160 or antihypertensive treatment and s-cholesterol ≥6.0 mmol/L, and current smoker or diabetic.
Table 2 shows the age-adjusted SHR for individual risk factors (SBP, s-cholesterol, hypertension, antihypertensive medication, and smoking status) after 35 years of follow-up. High s-cholesterol (SHR: 1.93, 95% CI: 1.65–2.26) and SBP (SHR: 1.68, 95% CI: 1.52–1.86) at baseline were the two most significant risk factors for CHD, followed by antihypertensive medication (SHR: 1.55, 95% CI: 1.31–1.82), hypertension (SHR:1.51, 95% CI: 1.38–1.66) and current smoking at baseline (SHR: 1.26, 95% CI: 1.16–1.36). For stroke, a significant risk increase was found for high SBP (SHR: 1.37, 95% CI: 1.20–1.57), antihypertensive medication (SHR: 1.31, with 95% CI: 1.05–1.64), and hypertension (SHR: 1.28, 95% CI: 1.13–1.44) at baseline. In contrast, high s-cholesterol (SHR: 1.06, 95% CI: 0.87–1.30) was not significantly related to stroke and being a smoker at baseline (SHR: 0.86, 95% CI: 0.77–0.95) was paradoxically associated with a lower risk.
Table 2.
A 35-year follow-up with subdistribution hazard ratio (95% CI) adjusted for age for coronary heart disease and stroke with regard to individual risk factors at baseline
| Risk factors | Number at risk | Eventsa | Total observation years | IRRb (95% CI) | Adjusted SHRb (95% CI) |
|---|---|---|---|---|---|
| CHD (mmol/L) | |||||
| S-cholesterol | |||||
| <5.0 | 703 | 180 | 18 000 | 1 (ref) | 1 (ref) |
| 5.0–5.9 | 1986 | 543 | 51 090.5 | 1.08 (0.91–1.27) | 1.10 (0.93–1.30) |
| 6.0–6.9 | 2364 | 818 | 57 901.9 | 1.45 (1.24–1.71) | 1.50 (1.28–1.76) |
| ≥7.0 | 2121 | 876 | 48 799 | 1.86 (1.58–2.19) | 1.93 (1.65–2.26) |
| SBP (mmHg) | |||||
| <140 | 2552 | 692 | 66 570.9 | 1 (ref) | 1 (ref) |
| 140–159 | 2573 | 878 | 63 377 | 1.31 (1.18–1.45) | 1.31 (1.19–1.45) |
| ≥160 | 2049 | 847 | 45 843.5 | 1.72 (1.55–1.90) | 1.68 (1.52–1.86) |
| Smoking | |||||
| Non-smoker | 3577 | 1112 | 95 528.8 | 1 (ref) | 1 (ref) |
| Smoking | 3597 | 1305 | 80 262.6 | 1.38 (1.27–1.49) | 1.26 (1.16–1.36) |
| Hypertension | |||||
| Non-hypertensive | 2171 | 568 | 57 501.2 | 1 (ref) | 1 (ref) |
| Hypertensive | 5003 | 1849 | 11 8290 | 1.54 (1.40–1.69) | 1.51 (1.38–1.66) |
| Antihypertensive medication | 367 | 166 | 7794.7 | 1.56 (1.33–1.83) | 1.55 (1.31–1.82) |
| Stroke (mmol/L) | |||||
| S-cholesterol | |||||
| <5.0 | 703 | 128 | 18 031.4 | 1 (ref) | 1 (ref) |
| 5.0–5.9 | 1986 | 353 | 52 106.9 | 0.97 (0.79–1.18) | 0.99 (0.81–1.21) |
| 6.0–6.9 | 2364 | 457 | 60 870.4 | 1.09 (0.89–1.32) | 1.09 (0.90–1.33) |
| ≥7.0 | 2121 | 397 | 52 590.5 | 1.10 (0.90–1.35) | 1.06 (0.87–1.30) |
| SBP (mmHg) | |||||
| <140 | 2552 | 418 | 68 831.8 | 1 (ref) | 1 (ref) |
| 140–159 | 2573 | 468 | 66 617.5 | 1.13 (0.99–1.29) | 1.11 (0.97–1.26) |
| ≥160 | 2049 | 449 | 48 149.9 | 1.48 (1.29–1.69) | 1.37 (1.20–1.57) |
| Smoking | |||||
| Non-smoker | 3577 | 715 | 98 698.1 | 1 (ref) | 1 (ref) |
| Smoking | 3597 | 620 | 84 901.1 | 0.99 (0.89–1.11) | 0.86 (0.77–0.95) |
| Hypertension | |||||
| Non-hypertensive | 2171 | 341 | 59 374.1 | 1 (ref) | 1 (ref) |
| Hypertensive | 5003 | 994 | 12 4225 | 1.35 (1.19–1.53) | 1.28 (1.13–1.44) |
| Antihypertensive medication | 367 | 85 | 8131.4 | 1.43 (1.15–1.79) | 1.31 (1.05–1.65) |
aFirst ever occurrence of a CHD or stroke.
bAge-adjusted incidence ratio (IRR) and subdistribution hazard ratio (SHR).
Effect of risk groups
To estimate the cumulative effect of developing a first CHD or stroke event, all participants were stratified into one of five risk groups (optimal levels, low risk, moderate risk, elevated risk, and high risk) based on their burden of risk factors at baseline in 1970–73. Table 3 shows the long-term SHR with 95% CI and the cumulative effect on CHD and stroke separately after 35 years when adjusted for age and competing risk. In general, each additional risk factor at baseline increased the risk of developing a CHD or stroke. Individuals with several risk factors at baseline (s-cholesterol ≥6.0 mmol/L, SBP ≥160 mmHg or antihypertensive treatment and being a current smokers at baseline) had a SHR of 2.89 (95% CI: 2.41–3.47) for CHD but 1.21 (95% CI: 0.96–1.53) for stroke compared with low-risk individuals (Table 3).
Table 3.
A 35-year follow-up with subdistribution hazard ratio (95% CI) adjusted for age for coronary heart disease and stroke with regard to risk groups
| Risk groups | Number at risk | Eventsa | Total observation years | IRRb (95% CI) | Adjusted SHRb (95% CI) |
|---|---|---|---|---|---|
| CHD | |||||
| Risk groupsb | |||||
| Optimal risk | 130 | 20 | 3855.6 | 0.77 (0.49–1.23) | 0.69 (0.44–1.07) |
| Low risk | 842 | 184 | 24 047.7 | 1 (ref) | 1 (ref) |
| Moderate risk | 2867 | 877 | 74 150 | 1.54 (1.31–1.80) | 1.48 (1.27–1.73) |
| Elevated risk | 2645 | 1001 | 60 530.8 | 2.16 (1.84–2.52) | 2.01 (1.73–2.35) |
| High risk | 690 | 335 | 13 207.3 | 3.22 (2.69–3.86) | 2.89 (2.41–3.47) |
| Stroke | |||||
| Risk groupsb | |||||
| Optimal risk | 130 | 24 | 3760.2 | 1.12 (0.72–1.72) | 1.10 (0.72–1.70) |
| Low risk | 842 | 144 | 24 429.2 | 1 (ref) | 1 (ref) |
| Moderate risk | 2867 | 535 | 76 677.2 | 1.18 (0.98–1.42) | 1.10 (0.92–1.32) |
| Elevated risk | 2645 | 494 | 64 196 | 1.30 (1.08–1.56) | 1.12 (0.93–1.35) |
| High risk | 690 | 138 | 14 536.6 | 1.56 (1.24–1.97) | 1.21 (0.96–1.53) |
aFirst ever occurrence of a CHD or stroke.
bAge-adjusted incidence ratio (IRR) and subdistribution hazard ratio (SHR).
In the final analysis, we estimated the short-term and long-term cumulative effect after adjusting for age and competing risk. For the first 10 years, individuals with adverse levels of risk factors at baseline (high risk) had an 18.1% risk of CHD compared with 1.3% for those with low risk (reference group). Corresponding results for stroke during the first 10 years were 3.2% compared with 0.5% (Figure 1). In the second part, the follow-up time was extended to 35 years in order to estimate the long-term effect of multiple risk factors. For CHD those with the most adverse levels of risk factors at baseline had a 47.8% risk compared with 19.6% for stroke after 35 years (Figure 1).
Figure 1.
Cumulative incidence curves adjusted for competing risk of death by different risk groups for coronary heart disease and stroke, respectively. The 10-year cumulative risk for (A) coronary heart disease, (B) stroke and the 35-year cumulative risk for (C) coronary heart disease, and (D) stroke.
Discussion
Principal findings
In the present study, we aimed to determine to what extent the use of age, s-cholesterol, SBP, and smoking status at baseline can be used to predict the short-term and long-term risk of both CHD and stroke separately among 7174 middle-aged men over an extended follow-up. For the first 10 years, we observed that these risk factors could effectively predict the cumulative risk of CHD but not stroke to the same extent. This did not change over time when the follow-up time was extended until old age. As a result, high-risk individuals had a markedly high-cumulative risk for CHD but not in a similar manner for stroke after 35 years.
Effect on individual risk factors
We found that the five major risk factors were all related to CHD and stroke after 35 years with the exception of s-cholesterol. However, the impact of each factor differed according to both the endpoint under study and the outcome. Consistent with previous reports, hypertension, antihypertensive medication, and high SBP at baseline were related to both CHD and stroke.13–17 High s-cholesterol levels were strongly associated with CHD but not stroke. Findings from previous epidemiological studies in this subject are inconsistent. For example, some have reported an inverse association of s-cholesterol and haemorrhagic stroke while other suggests that the ratio of HDL cholesterol and LDL cholesterol levels may be a better predictor.17–19 However, most epidemiological studies have failed to find a direct association between total cholesterol and overall stroke risk.20–22For the smoking status, we found that being a current smokers at baseline were associated with an increased risk of CHD but not for stroke after adjusting for competing risk. However, this result should not be interpreted to mean that smoking has no effect on stroke. On the contrary, previous epidemiological evidences have showed a strong association between smoking and having an increased risk of stroke.17,23,24 In an earlier 28-year follow-up period of this study population by Harmsen et al.25 smoking was found to be a risk factor for stroke during the first 21 years, but for the final period of 7 years no significant association was found. This effect could possibly be attributed to a decreasing proportion of smokers over time. For example, in Gothenburg smoking decreased from 50% in 1970–73 to <30% in 1995.26 Accordingly a diminishing number of smokers might have contributed to an underestimation of the true risk of smoking.25,27
The effect of cumulative risk factors
In a long-term perspective, the SHR among high-risk individuals, compared with those with low risk, was approximately twice as high for CHD compared with stroke after 35 years when adjusted for age and competing risk (Table 3). In the next step, we focused on the short-term and long-term effect on CHD and stroke.
For the first 10 years, we observed that the predictability of CHD and stroke based on the risk factors age, s-cholesterol, SBP, and smoking status differed considerably, with the cumulative risk among high-risk individuals being substantially higher for CHD than stroke. The difference between the two conditions is chiefly due to the small number of stroke events, since stroke is uncommon among younger and middle-aged people (in this study only numbering 118 stroke events for the first 10 years).6
After 35 years, when the follow-up time was extended until old age individuals with adverse levels of risk factors at baseline had a markedly high risk of CHD but not for stroke to the same extent. For the individual risk factors, only high SBP had a major impact on stroke. Therefore, our findings suggest that the effect of the sum of the individual risk factors differs for CHD and stroke. In addition, early deaths from CHD occur mainly among high risk individuals and as a result, the number of men with high risk decreases at higher rate over time which in a longer follow-up could have an effect on the risk estimates for stroke. To further improve the risk assessment, it is our belief that stroke should be separated from the general concept of CVD when developing risk models for use in middle-aged populations. Adding other major risk factors such as diabetes, obesity, or lack of exercise may be a more effective way to predict the short-term and long-term risk of stroke than focusing on any single-risk factor.
There are limitations to our study. First, risk factors in our study were generally high. This applies particularly to BP levels. However, different methodologies have been used, for instance using the lowest BP reading in a series or measuring in the morning as opposed to in the late afternoon (4:30–7:00 p.m.).28–30 In a separate analysis, a subsample of the men was selected and screened during the morning in a more relaxed environment, resulting in lower mean BP levels, where a cut-off point of 175/115 mmHg measured in the afternoon would correspond to a morning level of 162/101 mmHg.31 Moreover, BP levels have been shown to be generally lower in North America compared with European populations.32 Additionally, BP levels in Northern Europe have declined, with Gothenburg levels not dramatically different to other communities at the time.33,34 Secondly, s-cholesterol levels were also high; however, the mean value was lower in the present study than in other populations at the time such as the Oslo study and the FINRISK study (North Karelia and Savoy county area in 1972).33,35,36 As a result, the risk factors in the present study are comparable with other communities at the time. In addition, smoking rates were quite high and accordingly the optimal group was very small (1.8% of the total population). To provide meaningful comparisons, the low-risk group was therefore used as the reference group when calculating the SHR. Thirdly, we used only single measurements for the risk factors and these may have changed during the 35-year follow-up time. Even so, and with these limitations in mind, one-single measurement of these main risk factors in midlife was quite predictive for events occurring decades after the baseline investigation.
Conclusions
In conclusion, the prediction of CHD and of stroke in middle-aged men differs substantially when using the conventional risk factors SBP, s-cholesterol, and smoking. Our results indicate that the cumulative risk based on these traditional risk factors can effectively be used to predict both the short-term and long-term risk of CHD but not stroke to the same extent.
Funding
This work was supported by The Bank of Sweden Tercentenary Fund; The Swedish Research Council; The Swedish Council for Working Life and Social Research and The Swedish Heart and Lung Foundation.
Conflict of interest: none declared.
References
- 1.Strong K, Mathers C, Bonita R. Preventing stroke: saving lives around the world. Lancet Neurol. 2007;6:182–187. doi: 10.1016/S1474-4422(07)70031-5. doi:10.1016/S1474-4422(07)70031-5. [DOI] [PubMed] [Google Scholar]
- 2.Hobbs FD, Jukema JW, Da Silva PM, McCormack T, Catapano AL. Barriers to cardiovascular disease risk scoring and primary prevention in Europe. QJM. 2010;103:727–739. doi: 10.1093/qjmed/hcq122. doi:10.1093/qjmed/hcq122. [DOI] [PubMed] [Google Scholar]
- 3.Conroy RM, Pyorala K, Fitzgerald AP, Sans S, Menotti A, De Backer G, De Bacquer D, Ducimetiere P, Jousilahti P, Keil U, Njolstad I, Oganov RG, Thomsen T, Tunstall-Pedoe H, Tverdal A, Wedel H, Whincup P, Wilhelmsen L, Graham IM. Estimation of ten-year risk of fatal cardiovascular disease in Europe: the SCORE project. Eur Heart J. 2003;24:987–1003. doi: 10.1016/s0195-668x(03)00114-3. doi:10.1016/S0195-668X(03)00114-3. [DOI] [PubMed] [Google Scholar]
- 4.Anderson KM, Wilson PW, Odell PM, Kannel WB. An updated coronary risk profile. A statement for health professionals. Circulation. 1991;83:356–362. doi: 10.1161/01.cir.83.1.356. [DOI] [PubMed] [Google Scholar]
- 5.D'Agostino RB, Wolf PA, Belanger AJ, Kannel WB. Stroke risk profile: adjustment for antihypertensive medication. The Framingham Study. Stroke. 1994;25:40–43. doi: 10.1161/01.str.25.1.40. doi:10.1161/01.STR.25.1.40. [DOI] [PubMed] [Google Scholar]
- 6.Chen RL, Balami JS, Esiri MM, Chen LK, Buchan AM. Ischemic stroke in the elderly: an overview of evidence. Nat Rev Neurol. 2010;6:256–265. doi: 10.1038/nrneurol.2010.36. doi:10.1038/nrneurol.2010.36. [DOI] [PubMed] [Google Scholar]
- 7.Wilhelmsen L, Berglund G, Elmfeldt D, Tibblin G, Wedel H, Pennert K, Vedin A, Wilhelmsson C, Werko L. The multifactor primary prevention trial in Goteborg, Sweden. Eur Heart J. 1986;7:279–288. doi: 10.1093/oxfordjournals.eurheartj.a062065. [DOI] [PubMed] [Google Scholar]
- 8.Elmfeldt D, Wilhelmsen L, Tibblin G, Vedin JA, Wilhelmsson CE, Bengtsson C. Registration of myocardial infarction in the city of Goteborg, Sweden. J Chronic Dis. 1975;28:173–186. doi: 10.1016/0021-9681(75)90005-3. doi:10.1016/0021-9681(75)90005-3. [DOI] [PubMed] [Google Scholar]
- 9.Harmsen P, Tibblin G. A stroke register in Goteborg, Sweden. Acta Med Scand. 1972;191:463–470. [PubMed] [Google Scholar]
- 10.Jason PF, Gray RJ. A proportional hazards model for the subdistribution of a competing risk. JASA. 1999;94:496–509. [Google Scholar]
- 11.Gray RJ. A class of K-sample tests for comparing the cumulative incidence of a competing risk. Ann Stat. 1988;16:1141–1154. doi:10.1214/aos/1176350951. [Google Scholar]
- 12.Gray B. Subdistribution analysis of competing risks. 2011 R package Version 2.2–2. [Google Scholar]
- 13.Lewington S, Clarke R, Qizilbash N, Peto R, Collins R. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360:1903–1913. doi: 10.1016/s0140-6736(02)11911-8. doi:10.1016/S0140-6736(02)11911-8. [DOI] [PubMed] [Google Scholar]
- 14.Franklin SS, Larson MG, Khan SA, Wong ND, Leip EP, Kannel WB, Levy D. Does the relation of blood pressure to coronary heart disease risk change with aging? The Framingham Heart Study. Circulation. 2001;103:1245–1249. doi: 10.1161/01.cir.103.9.1245. doi:10.1161/01.CIR.103.9.1245. [DOI] [PubMed] [Google Scholar]
- 15.Kannel WB, Gordon T, Schwartz MJ. Systolic versus diastolic blood pressure and risk of coronary heart disease. The Framingham study. Am J Cardiol. 1971;27:335–346. doi: 10.1016/0002-9149(71)90428-0. doi:10.1016/0002-9149(71)90428-0. [DOI] [PubMed] [Google Scholar]
- 16.Yusuf S, Hawken S, Ounpuu S, Dans T, Avezum A, Lanas F, McQueen M, Budaj A, Pais P, Varigos J, Lisheng L. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. 2004;364:937–952. doi: 10.1016/S0140-6736(04)17018-9. doi:10.1016/S0140-6736(04)17018-9. [DOI] [PubMed] [Google Scholar]
- 17.O'Donnell MJ, Xavier D, Liu L, Zhang H, Chin SL, Rao-Melacini P, Rangarajan S, Islam S, Pais P, McQueen MJ, Mondo C, Damasceno A, Lopez-Jaramillo P, Hankey GJ, Dans AL, Yusoff K, Truelsen T, Diener HC, Sacco RL, Ryglewicz D, Czlonkowska A, Weimar C, Wang X, Yusuf S. Risk factors for ischaemic and intracerebral haemorrhagic stroke in 22 countries (the INTERSTROKE study): a case-control study. Lancet. 2010;376:112–123. doi: 10.1016/S0140-6736(10)60834-3. doi:10.1016/S0140-6736(10)60834-3. [DOI] [PubMed] [Google Scholar]
- 18.Yano K, Reed DM, MacLean CJ. Serum cholesterol and hemorrhagic stroke in the Honolulu Heart Program. Stroke. 1989;20:1460–1465. doi: 10.1161/01.str.20.11.1460. doi:10.1161/01.STR.20.11.1460. [DOI] [PubMed] [Google Scholar]
- 19.Suzuki K, Izumi M, Sakamoto T, Hayashi M. Blood pressure and total cholesterol level are critical risks especially for hemorrhagic stroke in Akita, Japan. Cerebrovasc Dis. 2011;31:100–106. doi: 10.1159/000321506. doi:10.1159/000321506. [DOI] [PubMed] [Google Scholar]
- 20.Qizilbash N, Lewington S, Duffy S, Peto R. Cholesterol, diastolic blood pressure, and stroke: 13,000 strokes in 450,000 people in 45 prospective cohorts. Prospective studies collaboration. Lancet. 1995;346:1647–1653. doi:10.1016/S0140-6736(95)92836-7. [PubMed] [Google Scholar]
- 21.Endres M, Heuschmann PU, Laufs U, Hakim AM. Primary prevention of stroke: blood pressure, lipids, and heart failure. Eur Heart J. 2011;32:545–552. doi: 10.1093/eurheartj/ehq472. doi:10.1093/eurheartj/ehq472. [DOI] [PubMed] [Google Scholar]
- 22.Lewington S, Whitlock G, Clarke R, Sherliker P, Emberson J, Halsey J, Qizilbash N, Peto R, Collins R. Blood cholesterol and vascular mortality by age, sex, and blood pressure: a meta-analysis of individual data from 61 prospective studies with 55,000 vascular deaths. Lancet. 2007;370:1829–1839. doi: 10.1016/S0140-6736(07)61778-4. doi:10.1016/S0140-6736(07)61778-4. [DOI] [PubMed] [Google Scholar]
- 23.Boysen G, Nyboe J, Appleyard M, Sorensen PS, Boas J, Somnier F, Jensen G, Schnohr P. Stroke incidence and risk factors for stroke in Copenhagen, Denmark. Stroke. 1988;19:1345–1353. doi: 10.1161/01.str.19.11.1345. doi:10.1161/01.STR.19.11.1345. [DOI] [PubMed] [Google Scholar]
- 24.Bonita R, Duncan J, Truelsen T, Jackson RT, Beaglehole R. Passive smoking as well as active smoking increases the risk of acute stroke. Tob Control. 1999;8:156–160. doi: 10.1136/tc.8.2.156. doi:10.1136/tc.8.2.156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Harmsen P, Lappas G, Rosengren A, Wilhelmsen L. Long-term risk factors for stroke: twenty-eight years of follow-up of 7457 middle-aged men in Goteborg, Sweden. Stroke. 2006;37:1663–1667. doi: 10.1161/01.STR.0000226604.10877.fc. doi:10.1161/01.STR.0000226604.10877.fc. [DOI] [PubMed] [Google Scholar]
- 26.Wilhelmsen L. ESC population studies lecture 1996. Cardiovascular monitoring of a city over 30 years. Eur Heart J. 1997;18:1220–1230. doi: 10.1093/oxfordjournals.eurheartj.a015433. doi:10.1093/oxfordjournals.eurheartj.a015433. [DOI] [PubMed] [Google Scholar]
- 27.Wilhelmsen L, Lappas G, Rosengren A. Risk of coronary events by baseline factors during 28 years follow-up and three periods in a random population sample of men. J Intern Med. 2004;256:298–307. doi: 10.1111/j.1365-2796.2004.01372.x. doi:10.1111/j.1365-2796.2004.01372.x. [DOI] [PubMed] [Google Scholar]
- 28.Wilhelmsen L, Berglund G, Werko L. Prevalence and management of hypertension in a general population sample of Swedish men. Prev Med. 1973;2:57–66. doi: 10.1016/0091-7435(73)90008-x. doi:10.1016/0091-7435(73)90008-X. [DOI] [PubMed] [Google Scholar]
- 29.Boe J, Humerfelt S, Wedervang F. The blood pressure in a population; blood pressure readings and height and weight determinations in the adult population of the city of Bergen. Acta Med Scand Suppl. 1957;321:1–336. [PubMed] [Google Scholar]
- 30.Kagan A, Gordon T, Kannel W, Dawber T. Blood pressure and its relation to coronary heart disease in the Framingham Study. Hypertension 7. 1959;4:53–81. [Google Scholar]
- 31.Wilhelmsen L. Treatment of hypertension in a Swedish community—the problem of borderline hypertension. Acta Med Scand. 1975;197(S576):99–108. doi:10.1111/j.0954-6820.1975.tb14815.x. [Google Scholar]
- 32.Wolf-Maier K, Cooper RS, Banegas JR, Giampaoli S, Hense HW, Joffres M, Kastarinen M, Poulter N, Primatesta P, Rodriguez-Artalejo F, Stegmayr B, Thamm M, Tuomilehto J, Vanuzzo D, Vescio F. Hypertension prevalence and blood pressure levels in 6 European countries, Canada, and the United States. JAMA. 2003;289:2363–2369. doi: 10.1001/jama.289.18.2363. doi:10.1001/jama.289.18.2363. [DOI] [PubMed] [Google Scholar]
- 33.Vartiainen E, Laatikainen T, Peltonen M, Juolevi A, Mannisto S, Sundvall J, Jousilahti P, Salomaa V, Valsta L, Puska P. Thirty-five-year trends in cardiovascular risk factors in Finland. Int J Epidemiol. 2010;39:504–518. doi: 10.1093/ije/dyp330. doi:10.1093/ije/dyp330. [DOI] [PubMed] [Google Scholar]
- 34.Bjorck L, Rosengren A, Bennett K, Lappas G, Capewell S. Modelling the decreasing coronary heart disease mortality in Sweden between 1986 and 2002. Eur Heart J. 2009;30:1046–1056. doi: 10.1093/eurheartj/ehn554. doi:10.1093/eurheartj/ehn554. [DOI] [PubMed] [Google Scholar]
- 35.Leren P, Askevold E, Foss O, Froili A, Grymyr D, Helgeland A, Hjermann I, Holme I, Lund-Larsen P, Norum K. The Oslo Study, Cardiovascular disease in middle-aged and young Oslo men. Acta Med Scand. 1975;588(Suppl):1–38. [PubMed] [Google Scholar]
- 36.Capewell S, Ford ES. Why have total cholesterol levels declined in most developed countries? BMC Public Health. 2011;11:641. doi: 10.1186/1471-2458-11-641. doi:10.1186/1471-2458-11-641. [DOI] [PMC free article] [PubMed] [Google Scholar]