Abstract
We evaluate whether hospitals serving a higher proportion of minorities experience disproportionate emergency department crowding, as proxied by ambulance diversion. In 202 hospitals across California, the median number of annual diversion hours was 374. After controlling for hospital characteristics, hospitals at the tenth percentile of fraction of minority visitors were on diversion only seventy-five hours per year, compared with hospitals at the ninetieth percentile, with 306 annual diversion hours. Emergency department crowding disproportionately affects minorities, and may contribute to health disparities in these communities. These findings suggest that establishing more uniform criteria regulating diversion may be one step toward decreasing disparities in access to emergency care.
Keywords: Disparities, Organization and Delivery of Care, Public Health, Safety-Net Systems
Introduction
Disparities in health care, including poorer outcomes experienced by racial and ethnic minorities, are well documented in the United States.1-6 One possible contributor to health disparities is differential access to timely emergency care. Although minority populations disproportionately use emergency departments for safety net care,7 there are limited data about the association between hospitals serving a large portion of minorities and access to emergency care. Specifically, no studies have observed whether emergency department crowding disproportionately affects minority populations.
Examining disparities in the acute care system is important, as utilization trends have strained the emergency care delivery system.8 The number of nonrural emergency departments dropped 27 percent from 1990 to 2009,9 while the number of visits to such facilities increased 40 percent.10 Moreover, emergency department closures affect minority populations more, as financial pressures force hospitals in low socioeconomic status communities to close.9,11
Ambulance diversion rates are often used as a proxy for emergency department overcrowding.18 Ambulances are diverted to other facilities when an emergency department is too crowded to safely care for new patients.12,13 Diversion is an increasingly common occurrence; it has been estimated that approximately one ambulance is diverted every minute in the United States.13 Beyond indicating overcrowding, diversion is harmful in itself, as it increases time to definitive care and is associated with poor outcomes for patients with certain conditions, for instance acute myocardial infarction.14 If crowding and subsequent diversion occurs disproportionately among hospitals serving minority populations, they may suffer poorer outcomes.15-17
We examined ambulance diversion data across all hospitals providing emergency services in the state of California in 2007. We hypothesized that hospitals serving high proportions of minority populations have disproportionately overcrowded emergency departments, as indicated by higher ambulance diversion rates.
Methods
Conceptual model
As described by Asplin et al.,18 emergency departments provide three kinds of care: emergency care (where the patient needs immediate treatment for a potentially life-threatening condition), unscheduled urgent care (where the patient seeks after-hours treatment for an acute but non-life-threatening condition, such as a painful ear infection), and safety-net care (where the patient uses the emergency department because of a lack of access to primary care or specialty services). Since ambulances typically transport patients needing true emergency care, diversion reroutes the neediest patients away from their nearest hospital, representing a failure of the system to provide the intended care.
We included hospital-level summaries of patient characteristics that are known to be associated with emergency department utilization including the: race, age, gender, income, and insurance status of emergency department visitors to individual hospitals.11,19-21 This allowed us to obtain a granular analysis of local demographics rather than simply using data at the county level.
As a measure of emergency department capacity, we calculated the ratio of daily emergency department visits to emergency department beds. Some hospitals may report hallway beds that are constantly in use and others may not.
To measure hospital capacity, known to be a major blockage in patient throughput,18,22 we calculated the ratio of annual inpatient admissions to staffed bed-days. Finally, we prespecified our model to include hospital characteristics that have been associated with emergency department crowding in other literature, including ownership (county, for-profit, or not-for-profit), trauma center status, teaching status, and operating margin.23
Study Design and Population
This retrospective cohort study included all emergency departments at acute, nonfederal hospitals operating in California in 2007. The study cohort includes hospitals that offer either basic or comprehensive emergency department services,24 based on California's Office of Statewide Health Planning and Development (OSHPD) data. As defined by the California Code of Regulations (Title 22, Division 5, Sections 70413-70419), basic services include a 24-hour presence of an emergency physician on call. A comprehensive ED includes 24-hour presence of certain specialist surgeons (thoracic, neurosurgery, orthopedics, and pediatric) and provides burn care, dialysis, and cardiovascular surgery. We excluded freestanding emergency departments and hospitals with standby emergency department services either because they were not staffed by medical doctors or they were not open twenty-four hours a day. Additionally, we excluded pediatric hospitals given that they generally do not treat adult patients, and hospitals whose emergency departments were not open for all of 2007. Finally, certain counties forbid the practice of ambulance diversion for either the entire county or certain hospitals. Therefore, we excluded all hospitals and counties that did not allow ambulance diversion for the full year of 2007 (n=86 hospitals, and 28 counties) and analyzed only hospitals where diversion was allowed for all of 2007, giving n=202 hospitals in 20 counties. Characteristics of included and excluded counties and hospitals are included in Appendix 1, with no significant differences except in population density and hospital ownership.
This study was approved by the California Committee for Protection of Human Subjects, the University of California Los Angeles Institutional Review Board, and the University of California San Francisco Committee on Human Research.
Data sources
We linked data from the Emergency Medical System (EMS) agencies in 20 California counties allowing diversion in 2007, OSHPD, the US Census,25 and the Area Resource File.26
Each EMS system provided electronic logs that contained information on all episodes of diversion, including: facility, date, duration in minutes, and reason for diversion. For the purposes of this analysis, we excluded diversion episodes for causes other than emergency department saturation, such as internal disaster and unavailability of specialty services (for instance, trauma, cardiac catheterization lab, computed tomography imaging). All episodes of ambulance diversion were aggregated to generate annual facility-specific summaries of diversion hours.
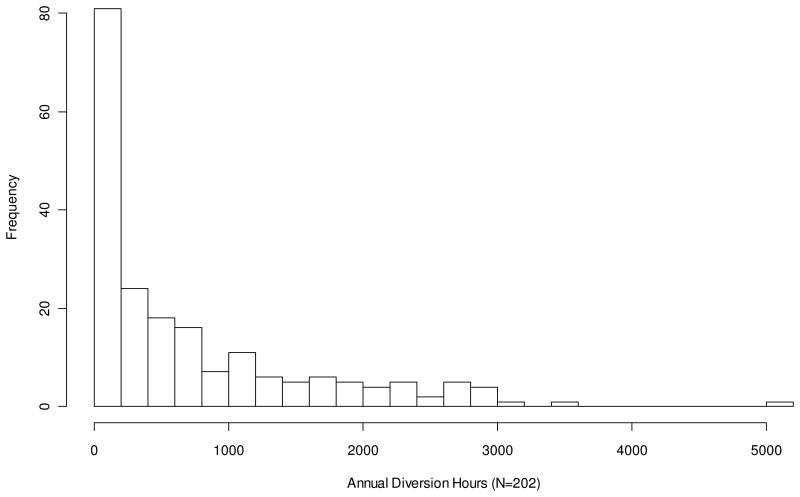
Four of the EMS systems were missing data due to software upgrades; three underwent such upgrades for two to four weeks and one for three months. For these, we estimated the annual diversion hours by inflating available diversion data proportionate to the amount of missing data. Systems issues were the only cause for missing data. Because the distribution of annual diversion hours was highly skewed, we transformed this variable to log (annual diversion hours+1) prior to analysis.
Each EMS system implemented unique diversion policies for specific counties or hospitals. The directors of all EMS systems verified their diversion policies for the year 2007 (some of which have subsequently changed). We included only those hospitals where diversion was allowed for all of 2007.
We obtained OSHPD non-public use files for all emergency department visits in 2007. All non-federal hospitals in California are mandated to report visit-level data on emergency department encounters that did not result in hospitalization (Emergency Discharge Data, or EDD), emergency department encounters that did result in hospitalizations (Patient Discharge Data, or PDD), and hospital-level structural and financial characteristics to OSHPD on an annual basis. Hospital financial and structural data were extracted from year 2007 OSHPD public-use files. Further details on the creation of the analytic cohort are presented in Appendix 2.
Outcome Measure
The primary outcome of this study was the annual number of diversion hours in 2007 for each hospital in the cohort. Diversion data is self-reported annually to OSHPD, however, this information underestimates the true diversion hours when compared with reports by local EMS agencies.27 Therefore, we used the “gold standard” ambulance diversion data directly from EMS agencies for the twenty counties. Our own comparisons using actual ambulance diversion data with self-reported data from hospitals were similar, although as reported elsewhere27 were slightly lower when they differed from the actual EMS reports, likely due to more conservative estimates when personnel filled out the forms rather than using actual data.
Minority population
We calculated the proportion of minorities treated by the emergency department of each hospital by aggregating all visits from the EDD and PDD from OSHPD in 2007 to the facility level. Minority population was determined by calculating what percentage of all patients with known race/ethnicity were non-White, as done in our previous work.23 This definition includes traditionally underrepresented minorities (African Americans and Hispanics) as well as Asians, Pacific Islanders, Native Americans, and any other category designated as “other.”
Covariates
We constructed other socioeconomic characteristics identified in our Conceptual Model, by creating facility-specific socioeconomic status profiles by aggregating episode-level OSHPD data from all emergency department visits in 2007 for age, gender, insurance, and income.29 Insurance was categorized into four groups: (i) private; (ii) Medicare; (iii) Medi-Cal and uninsured/self-pay; and (iv) other (including Worker's Compensation, other federal programs, automobile, or disability coverage). Patient income is not available in the hospital patient data. Instead, we imputed the median household income reported for a patient's residential ZIP code from the 2000 U.S. Census socioeconomic data. This method of using aggregate information from the Census as a proxy for individual socioeconomic status has been verified in previous studies.28,30 We averaged these within each hospital to calculate the facility mean of the ZIP code median income.
For hospital structure and process characteristics identified in the Conceptual Model that could affect ambulance diversion and crowding, we used the public-use utilization and financial databases from OSHPD. Hospital structural characteristics include teaching hospital (yes=1), trauma center (1 for Level 1 or 2 trauma designation, otherwise 0), two indicators for ownership (county, for-profit, or not-for-profit),23 and operating margin. Operating margin was defined as net from operations divided by total operating revenue. This definition has been used in the economic literature to identify financially distressed hospitals.31 We generated proxy measures of demand relative to supply for emergency department and for inpatient services. For emergency department demand relative to supply, we divided the number of daily emergency department visits by the number of emergency department treatment stations. For inpatient demand relative to supply, we divided the total number of patient bed-days by licensed bed-days, which is equivalent to the mean inpatient occupancy rate. These proxy measures of demand are modeled on Reeder and Garrison's methods of assessing overcrowding in EDs.32
Finally, we acquired county population for 2007 from the 2008 Area Resource File,26 which includes statistics from numerous health professional organizations including the Centers for Medicare and Medicaid Services as well as the Bureau of Labor Statistics. We calculated population density and transformed it with a log transformation because it is skewed.
Statistical analysis
To identify hospital-level factors associated with ambulance diversion, we fit hierarchical multivariate models. The outcome was log (annual diversion hours + 1), and the unit of analysis was the hospital. To account for clustering of hospitals by county, our models included a random county effect. In other words, our model contains a separate level for each county. To improve interpretability of the results, we provide back-transformed coefficients corresponding to percentage changes in (annual diversion hours plus one).
We identified a single outlier with 5,087 annual diversion hours (58 percent of 8,760 possible hours in a year), which was almost 70 percent higher than the facility with the next highest diversion hours. Diversion hours reported from the EMS agency and in OSHPD were concordant for this facility. In exploratory analysis, the qualitative interpretation of all variables except inpatient occupancy was unchanged when this outlier was removed.
To illustrate the effects of each factor on annual diversion hours, we estimated annual diversion at the 10th and 90th percentile value of each continuous factor while holding other covariates fixed. We held categorical variables at the modal values, using the most common value of each variable to calculate predicted diversion hours. To investigate effects of categorical variables, we varied each variable separately. We used SAS 9.2 (Cary, NC) for all analyses, and multivariate modeling was performed using SAS Proc Mixed.
Limitations
This study has several potential limitations. Diversion is an imperfect measure of crowding and may fail to capture more accurate specifications of crowding. Diversion prevents access to the ED only for patients arriving via ambulance. Approximately 70 percent of patients are transported to the ED by private vehicle or walk-in and lawfully cannot be turned away.33 Even when an emergency department is on diversion, certain patients--depending on the rules governing the particular emergency medical services system--can still be brought to a hospital. For example, if a hospital is the only trauma center in the county, that particular hospital may divert only non-trauma patients and still accept trauma patients. Thus, diversion does not completely reroute all emergency department volume. However, diversion has face and construct validity, and has been proposed as a candidate measure for emergency department crowding given that it is simple, objective, and readily-measured.34,35 Furthermore, diversion is a barrier to access for patients being transported by ambulance independent of crowding. Other crowding indices have been reported, including the Emergency Department Work Index,36 the National Department Overcrowding Scale,37 the Real-time Emergency Analysis of Demand Indicators,38 and the Work Scale.39 However, these formula-based scales require input on various patient and operational measures, such as patient acuity, emergency department and hospital occupancy rates, and provider staffing, and are limited by their complexity, need for specialized data measurement, and lack of reproducibility.40,41
Second, there were ten hospitals that were missing race data in more then 20 percent of patients. We found that the majority of missing data were in the emergency department data file (patients who were not admitted). In a sensitivity analysis, we imputed the race data for hospitalized patients to non-hospitalize patients for these ten hospitals. There were no qualitative differences in our results.
Finally, our data are limited to California and therefore may not generalize elsewhere.
Results
Characteristics of the 20 counties and the 202 hospitals in our study are presented in Exhibit 1. The mean number of hours on diversion for these hospitals was 724 per year (SD 889), with a median of 374 (IQR 52–1082) and a range of 0–5088. The distribution of annual diversion hours within county is illustrated in Exhibit 2. There is substantial inter- and intra-county variation in annual diversion hours. The magnitude of intra-county variance increases as a function of the median diversion hours. Appendix 3 illustrates the distribution of annual diversion hours for the 202 hospitals that were allowed to divert. Our multivariate model is presented in Exhibit 3. Hospitals serving high proportions of minority populations, our main predictor, were at higher risk of experiencing diversion (mean ratio 1.02 for each 1 percent increase in minority emergency department visitors [95% CI: 1.00, 1.04]). When we calculated the predicted number of annual hours on diversion for the hospitals with the tenth and ninetieth percentile of minority emergency department visitors, holding all others constant at their mean, hospitals at the 90th percentile of percent of minority emergency department visitors experienced 306 hours (95% CI: 104, 899) of annual diversion, which is 4.1 times (95% CI: 1.26, 13.3) that of hospitals serving the tenth percentile of percent of minority emergency department visitors, which experienced only seventy-five hours (95% CI: 27, 210).
Exhibit 1.
Characteristics of included California Counties and Hospitals in 2007
Source: Authors analysis of California OSHPD, U.S. Census Bureau & Area Resource File data as cited above (references 26 & 27)
| Description of counties | |
|---|---|
| Number of Counties | 20 |
| With 1 Hospital | 0 |
| With 2 Hospitals | 4 |
| With > 2 Hospitals | 16 |
| Number of Hospitals | 202 |
| Total Number of ED Visits | 7,148,712 |
| Hospital Mean (SD) | |
|
| |
| Age (Yr) | 39.91 (7.41) |
| Male (%) | 46.37 (3.45) |
| Non-White Visitors (%) | 53.38 (23.16) |
| Income (in $1000) | 48.92 (12.15) |
| Insurance – Medi-cal +Uninsured (%) | 40.87 (19.94) |
| Operating Margin (%) | -1.88 (18.78) |
| Population Density (Log Population per Sq Mile) | 7.00 (1.36) |
| Ratio of ED visits to ED beds per day | 4.83 (1.43) |
| Inpatient occupancy rate (%) | 62.5 (45.4) |
| Number of Hospitals (%) | |
|
| |
| Teaching Hospital (%) | 20 (9) |
| Ownership (%) | |
| County | 13 (6) |
| For Profit | 57 (27) |
| Not-for-Profit | 144 (66) |
| Trauma Center (%) | |
| Yes | 34 (16) |
Exhibit 2.
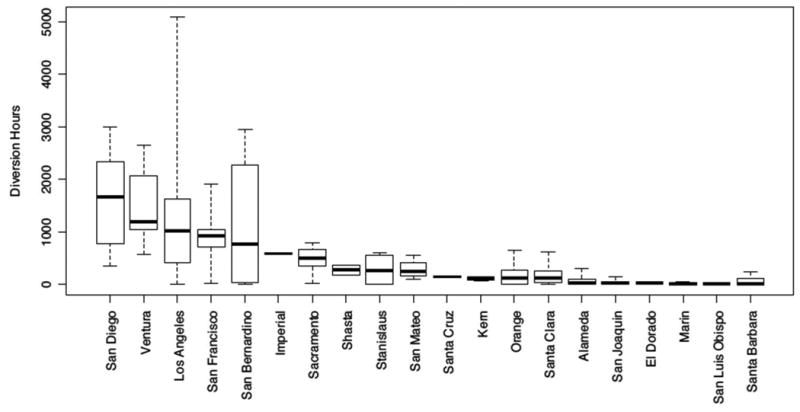
Boxplots of diversion hours in the 20 counties in California allowing diversion
Source: Authors' analysis of California OSHPD, U.S. Census Bureau & Area Resource File data as cited above (references 26 & 27)
Exhibit 3.
Predictors of Ambulance Diversion Using Hierarchical Hospital-level analysis* (n=202)
Source: Authors' analysis of California OSHPD, U.S. Census Bureau & Area Resource File data as cited above (references 26 & 27)
| Predictor | Multiplicative Increase for Unit Change in Predictor | 95%CI Lower Bound | 95%CI Upper Bound | p-value |
|---|---|---|---|---|
| Non-White (%) | 1.024 | 1.004 | 1.044 | 0.0193 |
| Other socioeconomic determinants of ED care | ||||
| Age (years) | 0.999 | 0.933 | 1.071 | 0.9833 |
| Gender – Male (%) | 0.999 | 0.891 | 1.119 | 0.9806 |
| Income (per $1000) | 0.988 | 0.948 | 1.028 | 0.5482 |
| Insurance (% Med-Cal + % Uninsured) | 0.963 | 0.941 | 0.985 | 0.0013 |
| Population Density (Log Scale) | 1.392 | 0.829 | 2.339 | 0.2219 |
| Supply of ED Care010 | ||||
| Ratio of ED Visits to ED Beds per Day | 1.261 | 1.041 | 1.527 | 0.0191 |
| Inpatient admissions to inpatient bed-days (%) | 1.022 | 1.004 | 1.041 | 0.0177 |
| Hospital Structural Characteristics | ||||
| Trauma status (Ref=No) | 2.874 | 1.306 | 6.325 | 0.0096 |
| Ownership (Ref=NFP) | 0.0988 | |||
| County | 2.153 | 0.457 | 10.14 | 0.3335 |
| For Profit | 0.576 | 0.314 | 1.057 | 0.0772 |
| Teaching status (Ref=No) | 1.339 | 0.451 | 3.971 | 0.6000 |
| Operating Margin | 0.994 | 0.978 | 1.010 | 0.4314 |
Hierarchical model with hospitals nested in county. Outcome is transformed annual diversion hours (log of annual diversion hours + 1)
Discussion
Our study provides a unique hospital-level analysis of how vulnerable populations are affected by emergency department crowding in California. We found that hospitals serving minorities were more likely to divert, even when controlling for hospital ownership, emergency department capacity, and other hospital-level demographic and structural factors. Other studies have examined system-level predictors of diversion,13,29,42,43 but none have evaluated the association of diversion with race/ethnicity. Our results indicating disproportionate diversion from hospitals serving greater numbers of minority patients are concerning given that ambulance diversion has been associated with poorer health outcomes.17
The disparate effect of diversion on hospitals serving a large proportion of minorities may indicate a fundamental mismatch in supply and demand of emergency department services. Minority populations may live in areas where there are fewer emergency departments or trauma centers and thus may face higher rates of emergency department crowding and consequent diversion. This is concordant with literature suggesting that both emergency departments and trauma centers are closing more frequently in areas with vulnerable populations, including racial and ethnic minorities,44,45 and that non-White patients have longer lengths of stay when admitted to the hospital.46
Our findings take on increased urgency as our study establishes a higher prevalence and raw number of diversion hours in California than previously reported in national studies.22,29 Almost all hospitals that could be on diversion were so in 2007 (188 out of 202, or 92 percent). Three potential explanations for the comparatively high levels of diversion hours in our study could be that (i) we used more recent data, suggesting that emergency department crowding could be worsening, (ii) that California experiences more crowding than most states, or (iii) we used actual EMS data rather than self-reported data from state or regional agencies. This final point highlights another important contribution of this work, given the increased accuracy of using computerized tracking data from each local EMS agency and calculation of diversion hours. Finally, these results add to the literature of alternative measures of emergency department crowding. These studies also indicate that emergency department crowding is worsening nationally when measured by the rate of patients who leave without being seen,23 wait times,47 and length of stay.48
Our findings provide substantive evidence on which to base policy decisions concerning ambulance diversion. It is known that hospitals have different thresholds to activate diversion.49 It is precisely this variation, along with our findings, that allows us to conclude that system-level policies regulating ambulance diversion provides policy-makers, healthcare providers, and hospital administrations may help reduce diversion and its associated inequalities. Indeed, statewide and national efforts have been undertaken to implement no-diversion policies, although none yet in California.50,51 There have been individual attempts in various counties to reduce crowding and encourage a higher threshold for activating diversion, but there are no statewide criteria regulating diversion policies.
Although “diversion ban” policies address only a symptom of the larger problem of emergency department crowding (and diversion is only a symptom crowding issues), banning diversion may force hospitals to examine issues such as hospital flow, which may contribute to emergency department crowding.8,52 Preliminary data from Massachusetts's ban on diversion, implemented as of January 2009, reveal that thus far the policy has created no significant increases in waiting times. This may be due to improvements in hospital flow mechanisms that are regionally applied.53,54 EMS agencies and regional health authorities could reduce diversion with more carefully crafted policies such as explicit criteria for enacting diversion, limiting its duration and frequency, and requiring hospital CEOs to approve diversion episodes.55
Our study provides evidence that minority patients in the acute care system disproportionately experience crowding when measured by ambulance diversion. Our findings suggest that disparities arise from “upstream” causes before patients reach their hospital destination and that intervention at this level to decrease disparities may be warranted.
Appendix 1
Characteristics of Included and Excluded Hospitals*
| Variable | Included | Excluded | p-value |
|---|---|---|---|
| Number of Counties | 20 | 28 | |
| Number of Hospitals in County | |||
| With 1 hospital | 0 | 13 | |
| With 2 hospitals | 4 | 5 | |
| With >2 hospitals | 16 | 10 | |
| Number of Hospitals | 214 | 74 | |
| Hospital-Level Mean Profile of ED Visitors | |||
| Age (Years, SD) | 38.91 (7.41) | 38.66 (7.09) | 0.7985 |
| Male (%, SD) | 46.37 (3.45) | 46.24 (3.05) | 0.7739 |
| Non-White (%, SD) | 53.38 (23.16) | 39.09 (23.88) | <.0001 |
| Income (in $1000, SD) | 48.92 (12.15) | 43.83 (11.94) | 0.002 |
| Insurance - Med-Cal+Uninsured (%, SD) | 40.87 (19.94) | 42.61 (18.78) | 0.5041 |
| Operating Margin (%, SD) | -1.88 (18.78) | 2.33 (13.55) | 0.0539 |
| Population Density (Log Scal per Sq Mile, SD) | 7.00 (1.36) | 4.91 (1.30) | <.0001 |
| Ratio of ED visits to ED beds per day (SD) | 4.83 (1.43) | 5.24 (1.81) | 0.0835 |
| Inpatient occupancy rate (%, SD) | 62.5 (45.4) | 59.8 (16.9) | 0.4695 |
| Hospital Characteristics | |||
| Teaching Hospital (n, %) | 20 (9) | 2 (3) | 0.0637 |
| Ownership (n, %)* | 0.0032 | ||
| County | 13 (6) | 4 (5) | |
| For Profit | 57 (27) | 6 (8) | |
| Non Profit | 144 (67) | 64 (87) | |
| Trauma Center (%) | 34 (16) | 8 (11) | 0.2861 |
We studied 48 unique counties in our dataset; while there are 58 counties in California, 10 counties did not have eligible hospitals (no hospitals, or no hospitals with basic/comprehensive EDs).
Appendix 2
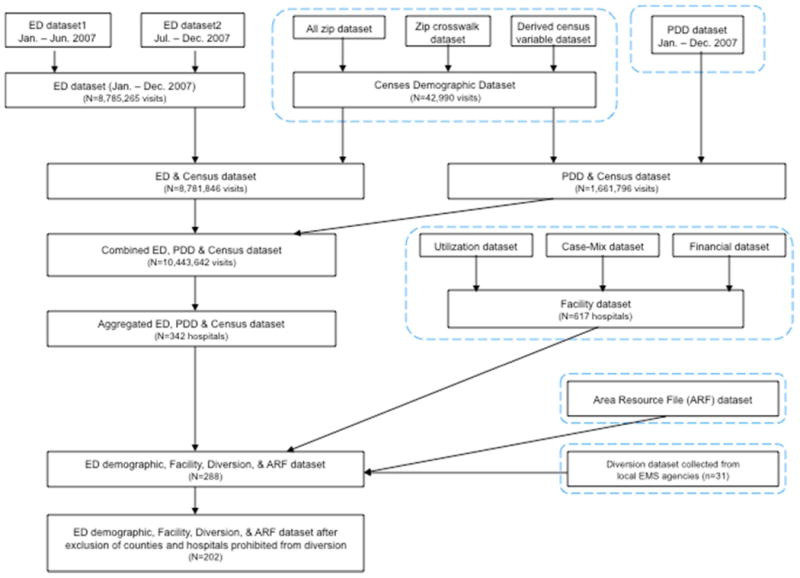
Creation of analytic cohort
Appendix 3
Histogram of Annual Diversion Hours (N=202; “frequency” represents number of hospitals)
Notes
- 1.Racial disparities in total knee replacement among Medicare enrollees, United States, 2000-2006. JAMA. 2009;302(14):1525–6. [PubMed] [Google Scholar]
- 2.Castel LD, Saville BR, Depuy V, Godley PA, Hartmann KE, Abernethy AP. Racial differences in pain during 1 year among women with metastatic breast cancer: a hazards analysis of interval-censored data. Cancer. 2008;112(1):162–70. doi: 10.1002/cncr.23133. [DOI] [PubMed] [Google Scholar]
- 3.Jha AK, Fisher ES, Li Z, Orav EJ, Epstein AM. Racial trends in the use of major procedures among the elderly. N Engl J Med. 2005;353(7):683–91. doi: 10.1056/NEJMsa050672. [DOI] [PubMed] [Google Scholar]
- 4.Vaccarino V, Rathore SS, Wenger NK, Frederick PD, Abramson JL, Barron HV, et al. Sex and racial differences in the management of acute myocardial infarction, 1994 through 2002. N Engl J Med. 2005;353(7):671–82. doi: 10.1056/NEJMsa032214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Disparities in deaths from stroke among persons aged <75 years, United States, 2002. Centers for Disease Control MMWR. 2005 May;54(19):477–381. [PubMed] [Google Scholar]
- 6.Weitzman M, Gortmaker SL, Sobol AM, Perrin JM. Recent trends in the prevalence and severity of childhood asthma. JAMA. 1992;268(19):2673–77. [PubMed] [Google Scholar]
- 7.Tang N, Stein J, Hsia RY, Maselli JH, Gonzales R. Trends and characteristics of U.S. emergency department visits, 1997-2007. JAMA. 2010;304(6):664–70. doi: 10.1001/jama.2010.1112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Warden GL, Altman SH, Asplin BR, Babor TF, Bass RR, Chu BK, et al. Hospital-based emergency care: at the breaking point. Washington, DC: National Academies Press; 2007. [Google Scholar]
- 9.Hsia RY, Kellermann AL, Shen YC. Factors associated with closures of emergency departments in the United States. JAMA. 2011;305(19):1978–85. doi: 10.1001/jama.2011.620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.TrendWatch Chartbook 2009. Chicago (IL): The American Hospital Association c; 2006-2011. Trends Affecting Hospitals and Health Systems. Internet. Available from: http://www.aha.org/research/reports/tw/chartbook/ch5.shtml. [Google Scholar]
- 11.Burt CW, Arispe IE. Characteristics of emergency departments serving high volumes of safety-net patients: United States, 2000. Vital Health Stat 13. 2004;(155):1–16. [PubMed] [Google Scholar]
- 12.Warden CR, Bangs C, Norton R, Huie J. Temporal trends in ambulance diversion in a mid-sized metropolitan area. Prehosp Emerg Care. 2003;7(1):109–113. doi: 10.1080/10903120390937201. [DOI] [PubMed] [Google Scholar]
- 13.Burt CW, McCaig LF, Valverde RH. Analysis of ambulance transports and diversions among US emergency departments. Ann Emerg Med. 2006;47(4):317–326. doi: 10.1016/j.annemergmed.2005.12.001. [DOI] [PubMed] [Google Scholar]
- 14.Shen YC, Hsia RY. Association between ambulance diversion and survival among patients with acute myocardial infarction. JAMA. 2011;305(23):2440–47. doi: 10.1001/jama.2011.811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Williams RM. Ambulance diversion: economic and policy considerations. Ann Emerg Med. 2006;48(6):711–12. doi: 10.1016/j.annemergmed.2006.06.009. [DOI] [PubMed] [Google Scholar]
- 16.Asplin BR. Does ambulance diversion matter? Ann Emerg Med. 2003;41(4):477–480. doi: 10.1067/mem.2003.112. [DOI] [PubMed] [Google Scholar]
- 17.Schull MJ, Morrison LJ, Vermeulen M, Redelmeier DA. Emergency department gridlock and out-of-hospital delays for cardiac patients. Acad Emerg Med. 2003;10(7):709–16. doi: 10.1111/j.1553-2712.2003.tb00064.x. [DOI] [PubMed] [Google Scholar]
- 18.Asplin BR, Magid DJ, Rhodes KV, Solberg LI, Lurie N, Camargo CA., Jr A conceptual model of emergency department crowding. Ann Emerg Med. 2003;42(2):173–80. doi: 10.1067/mem.2003.302. [DOI] [PubMed] [Google Scholar]
- 19.DeLia D, Cantor J. Emergency department utilization and capacity. The Robert Wood Johnson Foundation. 2009 [Google Scholar]
- 20.May JH, Cunningham PJ, Hadley J. Most uninsured people unaware of health care safety net providers. Issue Brief Cent Stud Health Syst Change. 2004;(90):1–4. [PubMed] [Google Scholar]
- 21.Weber EJ, Showstack JA, Hunt KA, Colby DC, Callaham ML. Does lack of a usual source of care or health insurance increase the likelihood of an emergency department visit? Results of a national population-based study. Ann Emerg Med. 2005;45(1):4–12. doi: 10.1016/j.annemergmed.2004.06.023. [DOI] [PubMed] [Google Scholar]
- 22.Hoot NR, Aronsky D. Systematic review of emergency department crowding: causes, effects, and solutions. Ann Emerg Med. 2008;52(2):126–36. doi: 10.1016/j.annemergmed.2008.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hsia RY, Asch SM, Weiss RE, Zingmond D, Liang LJ, Han W, et al. Hospital determinants of emergency department left without being seen rates. Ann Emerg Med. 2011;58(1):24–32. doi: 10.1016/j.annemergmed.2011.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lambe S, Washington DL, Fink A, Herbst K, Liu H, Fosse JS, et al. Trends in the use and capacity of California's emergency departments, 1990-1999. Ann Emerg Med. 2002;39(4):389–96. doi: 10.1067/mem.2002.122433. [DOI] [PubMed] [Google Scholar]
- 25.United States Census 2000. Suitland (MD) The United States Census Bureau. c2000 Internet. [cited 2005 May 16] Available from: http://www.census.gov/
- 26.Area Resource File. Rockville [MD]: US Department of Health and Human Services, Health Resources and Services Administration, Bureau of Health Professions; 2008. [Google Scholar]
- 27.California Emergency Department Diversion Project. [Internet]. San Diego c. 2011- cited [2008 May 15]. Available from: http://www.chcf.org/topics/hospitals/index.cfm?itemID=13229
- 28.Krieger N. Overcoming the absence of socioeconomic data in medical records: validation and application of a census-based methodology. Am J Public Health. 1992;82(5):703–10. doi: 10.2105/ajph.82.5.703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Burt CW, McCaig LF. Staffing, capacity, and ambulance diversion in emergency departments: United States, 2003-04. Adv Data. 2006;(376):1–23. [PubMed] [Google Scholar]
- 30.Gornick ME, Eggers PW, Reilly TW, Mentnech RM, Fitterman LK, Kucken LE, et al. Effects of race and income on mortality and use of services among Medicare beneficiaries. N Engl J Med. 1996;335(11):791–99. doi: 10.1056/NEJM199609123351106. [DOI] [PubMed] [Google Scholar]
- 31.Graddy EA, Ye K. When do we “just say no”? Policy termination decisions in local hospital services. Policy Stud J. 2008;36(2):219–42. [Google Scholar]
- 32.Reeder TJ, Garrison HG. When the safety net is unsafe: real-time assessment of the overcrowded emergency department. Acad Emerg Med. 2001;8(11):1070–74. doi: 10.1111/j.1553-2712.2001.tb01117.x. [DOI] [PubMed] [Google Scholar]
- 33.Niska R, Bhuiya F, Xu J. National hospital ambulatory medical care survey: 2007 emergency department summary. National Health Statistics Reports (US) 2010 Feb;:32. Report No. 26. [PubMed] [Google Scholar]
- 34.Schull MJ, Slaughter PM, Redelmeier DA. Urban emergency department overcrowding: defining the problem and eliminating misconceptions. Cjem. 2002;4(2):76–83. doi: 10.1017/s1481803500006163. [DOI] [PubMed] [Google Scholar]
- 35.Solberg LI, Asplin BR, Weinick RM, Magid DJ. Emergency department crowding: consensus development of potential measures. Ann Emerg Med. 2003;42(6):824–34. doi: 10.1016/S0196064403008163. [DOI] [PubMed] [Google Scholar]
- 36.Bernstein SL, Verghese V, Leung W, Lunney AT, Perez I. Development and validation of a new index to measure emergency department crowding. Acad Emerg Med. 2003;10(9):938–42. doi: 10.1111/j.1553-2712.2003.tb00647.x. [DOI] [PubMed] [Google Scholar]
- 37.Weiss SJ, Derlet R, Arndahl J, Ernst AA, Richards J, Fernandez-Frackelton M, et al. Estimating the degree of emergency department overcrowding in academic medical centers: results of the National ED Overcrowding Study (NEDOCS) Acad Emerg Med. 2004;11(1):38–50. doi: 10.1197/j.aem.2003.07.017. [DOI] [PubMed] [Google Scholar]
- 38.Reeder TJ, Burleson DL, Garrison HG. The overcrowded emergency department: a comparison of staff perceptions. Acad Emerg Med. 2003;10(10):1059–64. doi: 10.1111/j.1553-2712.2003.tb00575.x. [DOI] [PubMed] [Google Scholar]
- 39.Epstein SK, Tian L. Development of an emergency department work score to predict ambulance diversion. Acad Emerg Med. 2006;13(4):421–6. doi: 10.1197/j.aem.2005.11.081. [DOI] [PubMed] [Google Scholar]
- 40.Raj K, Baker K, Brierley S, Murray D. National emergency department overcrowding study tool is not useful in an Australian emergency department. Emerg Med Australas. 2006;18(3):282–88. doi: 10.1111/j.1742-6723.2006.00854.x. [DOI] [PubMed] [Google Scholar]
- 41.Jones SS, Allen TL, Flottemesch TJ, Welch SJ. An independent evaluation of four quantitative emergency department crowding scales. Acad Emerg Med. 2006;13(11):1204–11. doi: 10.1197/j.aem.2006.05.021. [DOI] [PubMed] [Google Scholar]
- 42.Lagoe RJ, Hunt RC, Nadle PA, Kohlbrenner JC. Utilization and impact of ambulance diversion at the community level. Prehosp Emerg Care. 2002;6(2):191–98. doi: 10.1080/10903120290938535. [DOI] [PubMed] [Google Scholar]
- 43.Schull MJ, Lazier K, Vermeulen M, Mawhinney S, Morrison LJ. Emergency department contributors to ambulance diversion: a quantitative analysis. Ann Emerg Med. 2003;41(4):467–76. doi: 10.1067/mem.2003.23. [DOI] [PubMed] [Google Scholar]
- 44.Rice MF. Inner-city hospital closures/relocations: race, income status, and legal issues. Soc Sci Med. 1987;24(11):889–96. doi: 10.1016/0277-9536(87)90282-6. [DOI] [PubMed] [Google Scholar]
- 45.Shen YC, Hsia RY, Kuzma K. Understanding the risk factors of trauma center closures: do financial pressure and community characteristics matter? Med Care. 2009;47(9):968–78. doi: 10.1097/MLR.0b013e31819c9415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Pines JM, Russell Localio A, Hollander JE. Racial disparities in emergency department length of stay for admitted patients in the United States. Acad Emerg Med. 2009;16(5):403–10. doi: 10.1111/j.1553-2712.2009.00381.x. [DOI] [PubMed] [Google Scholar]
- 47.Lambe S, Washington DL, Fink A, et al. Waiting times in California's emergency departments. Ann Emerg Med. 2003;41(1):35–44. doi: 10.1067/mem.2003.2. [DOI] [PubMed] [Google Scholar]
- 48.Pines JM, Prabhu A, Hilton JA, Hollander JE, Datner EM. The effect of emergency department crowding on length of stay and medication treatment times in discharged patients with acute asthma. Acad Emerg Med. 2010;17(8):834–39. doi: 10.1111/j.1553-2712.2010.00780.x. [DOI] [PubMed] [Google Scholar]
- 49.Handel DA, Pines J, Aronsky D, Genes N, Ginde AA, Hackman J, et al. Variations in crowding and ambulance diversion in nine emergency departments. Acad Emerg Med. 2011;18(9):941–46. doi: 10.1111/j.1553-2712.2011.01149.x. [DOI] [PubMed] [Google Scholar]
- 50.Castillo EM, Vilke GM, Williams M, Turner P, Boyle J, Chan TC. Collaborative to decrease ambulance diversion: the California emergency department diversion project. J Emerg Med. 2011;40(30):300–7. doi: 10.1016/j.jemermed.2010.02.023. [DOI] [PubMed] [Google Scholar]
- 51.Patel PB, Derlet RW, Vinson DR, Williams M, Wills J. Ambulance diversion reduction: the Sacramento solution. Am J Emerg Med. 2006;24(2):206–13. doi: 10.1016/j.ajem.2005.09.005. [DOI] [PubMed] [Google Scholar]
- 52.Olshaker JS, Rathlev NK. Emergency department overcrowding and ambulance diversion: the impact and potential solutions of extended boarding of admitted patients in the emergency department. J Emerg Med. 2006;30(3):351–56. doi: 10.1016/j.jemermed.2005.05.023. [DOI] [PubMed] [Google Scholar]
- 53.Burke L. Ending ambulance diversion in Massachusetts. Virtual Mentor. 2010;12(6) doi: 10.1001/virtualmentor.2010.12.6.pfor2-1006. [DOI] [PubMed] [Google Scholar]
- 54.Scheck A. Diversion ban: no solution to ED crowding. Emergency Medicine News. 2010;32(12):1, 4, 5. [Google Scholar]
- 55.Lagoe RJ, Kohlbrenner JC, Hall LD, Roizen M, Nadle PA, Hunt RC. Reducing ambulance diversion: a multihospital approach. Prehosp Emerg Care. 2003;7(1):99–108. doi: 10.1080/10903120390937184. [DOI] [PubMed] [Google Scholar]