Abstract
Oxidative stress has been identified as an important contributor to neurodegeneration associated with acute CNS injuries and diseases such as spinal cord injury (SCI), traumatic brain injury (TBI), and ischemic stroke. In this review, we briefly detail the damaging effects of oxidative stress (lipid peroxidation, protein oxidation, etc.) with a particular emphasis on DNA damage. Evidence for DNA damage in acute CNS injuries is presented along with its downstream effects on neuronal viability. In particular, unchecked oxidative DNA damage initiates a series of signaling events (e.g. activation of p53 and PARP-1, cell cycle re-activation) which have been shown to promote neuronal loss following CNS injury. These findings suggest that preventing DNA damage might be an effective way to promote neuronal survival and enhance neurological recovery in these conditions. Finally, we identify the telomere and telomere-associated proteins (e.g. telomerase) as novel therapeutic targets in the treatment of neurodegeneration due to their ability to modulate the neuronal response to both oxidative stress and DNA damage.
Keywords: CNS injury, oxidative stress, DNA damage, neuron death, telomere, telomerase
Introduction
Substantial evidence indicates that oxidative stress is a major contributor to the pathophysiology of a variety of neurodegenerative disorders including Alzheimer’s disease, Parkinson’s disease, and acute central nervous system (CNS) injuries such as spinal cord injury (SCI) and traumatic brain injury (TBI) which will be the focus of this review. The CNS, and neurons in particular, are especially vulnerable to oxidative stress due to their high metabolic rate, limited capacity for regeneration, and high iron/copper content. Damaging reactive oxygen species (ROS) and reactive nitrogen species (RNS) are formed as unavoidable by-products of metabolism but their damaging effects are normally counteracted by endogenous anti-oxidant enzymes (e.g catalase, superoxide dismutase, glutathione peroxidase, and glutathione reductase) and substances (e.g. glutathione, metallothionein, vitamin A, vitamin C, and vitamin E) (Duffy et al., 1998; Suemori et al., 2006; Vatassery, 1998). However, oxidative stress represents a state in which these anti-oxidant defenses are overwhelmed and no longer capable of protecting the cell from oxidative damage.
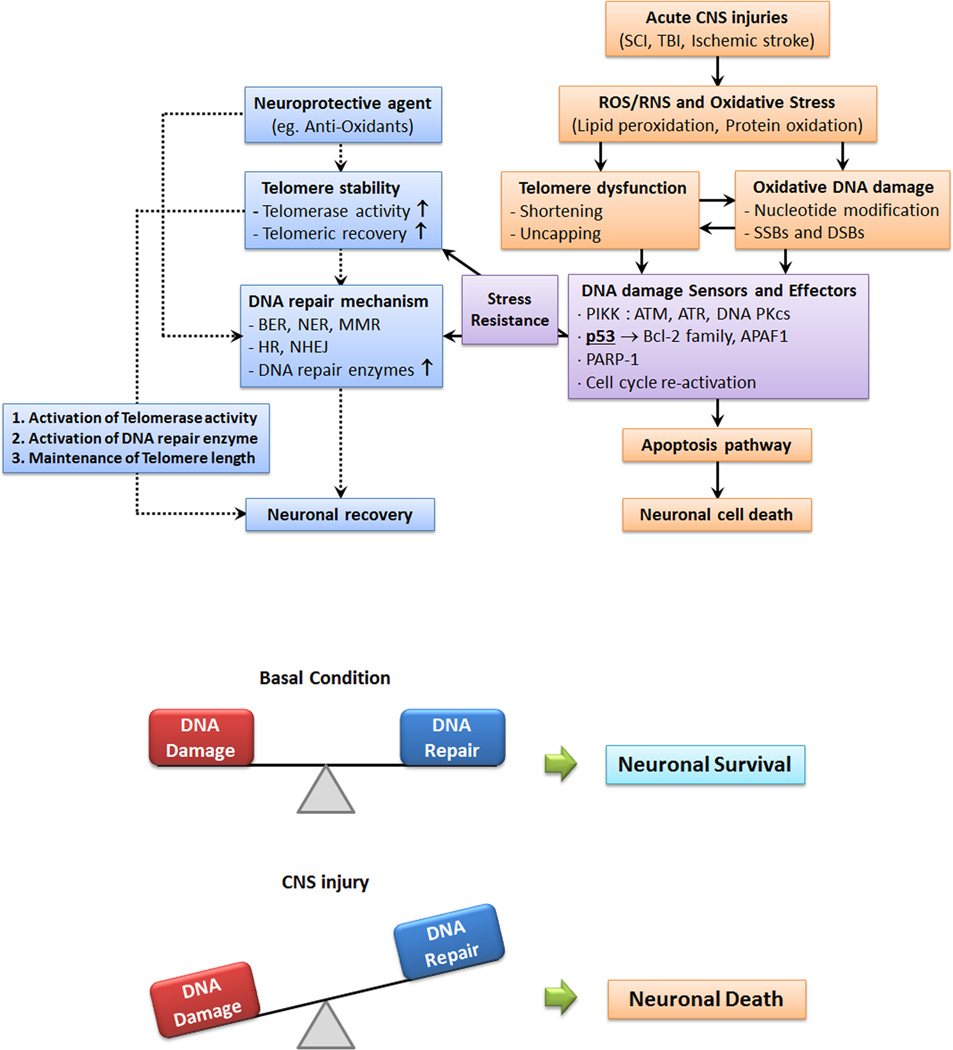
Accumulation of ROS/RNS can result in a number of detrimental effects such as lipid peroxidation, protein oxidation, and DNA damage. Lipid peroxidation disrupts normal structure and function of lipid bilayers surrounding both the cell itself and membrane-bound organelles (Catala, 2011, 2012). In particular, peroxidation of lipids may alter membrane permeability, transport processes, and fluidity. In addition, lipid peroxidation may ultimately result in the production of multiple aldehyde species (e.g. acrolein, malondialdehyde (MDA)) that further contribute to toxicity associated with lipid peroxidation. Elevated markers of lipid peroxidation, including MDA, 4-hydroxynonenal (4-HNE), and acrolein, have been shown in animal models of both SCI and TBI, indicating that lipid peroxidation may be an important contributor to the pathophysiology of these disorders (Ansari et al., 2008; Hall et al., 2004; Hamann et al., 2008; Inci et al., 1998; Lin et al., 2007; Seligman et al., 1977). Protein modifications by accumulated ROS/RNS include protein fragmentation, protein misfolding, proteinprotein cross-linkages, production of protein carbonyls, and priming of oxidized proteins for proteasomal degradation (Berlett and Stadtman, 1997; Radak et al., 2011). Substantial evidence suggests that protein aggregation or misfolding may be involved in the pathogenesis of neurodegenerative conditions. Severe protein aggregation was noted in hippocampal CA1 neurons after ischemia/reperfusion injury, appearing first at 4 hr. and accumulating over a period of 48 hr. (Hu et al., 2000). Increases in heat shock protein 70 (HSP70), which functions as an intracellular chaperon of protein folding, have also been observed after TBI, indicating induction of HSP70 to clear misfolded or aggregated proteins (Zhao et al., 1998). Conversely, overexpression of HSP70 has been shown to reduce neuronal injury both in vitro and in animal models of stroke (Rajdev et al., 2000). These studies suggest that increased ROS/RNS in the context of CNS injury may also contribute to protein aggregation and misfolding. Together, these alterations can profoundly impact normal protein/enzymatic activity and disrupt a variety of biochemical processes. Given the role of oxidative stress in the pathology of acute CNS injury and disease, it is not surprising that increased levels of protein carbonyls have been demonstrated in experimental models of both SCI and TBI as well as in experimental autoimmune encephalomyelitis (EAE) an animal model of multiple sclerosis (MS) which is also characterized by a neurodegenerative component (Jin et al., 2004; Smerjac and Bizzozero, 2008; Xiong et al., 2007). Such elevated levels of protein carbonyls have also been described in both grey and white matter in tissue obtained from patients with MS. Although the importance of lipid peroxidation and protein oxidation in cellular damage resulting from CNS injuries should not be overlooked, the remainder of this review will focus on DNA damage and telomeric dysfuction as effects of oxidative stress generated as a result of acute CNS injury (Figure 1). We use the term acute neurodegeneration to differentiate CNS injury from other, more chronic forms of neurodegenerative disorders such as AD, PD, and ALS. It should be noted, however, that it is still difficult to differentiate the biochemical pathways which are active during DNA damage/repair in the “acute” and “chronic” phases of CNS injury. For this reason, we have placed less emphasis on classifying cellular changes related to DNA damage as “acute” or “chronic” in the context of CNS injury in this review.
Figure 1. Mechanisms linking oxidative stress, DNA damage/repair, and telomere dysfunction in CNS injury.
Oxidative stress results in the accumulation of cellular ROS/RNS which in turn leads to DNA damage, lipid peroxidation, and protein oxidation, in neuronal cells. As a result of DNA damage and associated telomere dysfunction, a number of downstream signaling cascades are activated that may determine cellular fate. Induction of appropriate DNA repair systems may reverse oxidative modifications and promote neuronal survival. However, when oxidative DNA damage overwhelms repair systems, cell cycle reentry and p53 may initiate neuronal apoptosis. Neuroprotective agents may act a number of points in the proposed pathway (including ROS/RNS production, telomerase expression/activity, etc.) to prevent neuronal loss in the context of acute neurodegeneration.
DNA Damage as a Result of Oxidative Stress
Oxidative stress and the resultant accumulation of ROS/RNS can lead to a number of different DNA lesions including direct modification of nucleotide bases, formation of apurinic/apyrimidinic sites, DNA single strand breaks (SSBs), and, much less frequently, DNA double strand breaks (DSBs). Direct nucleotide modifications have been widely reported as consequences of oxidative/nitrosative damage to the cell. Of all the nucleotide bases, guanine is the most susceptible to oxidative modifications due to the fact that it has the lowest reduction potential. Hydroxyl radicals have been shown to interact with the C4, C5, and C8 positions in the imidazole ring of guanine. Of these, formation of 8-hydroxyguanosine (8-OxoG) is the most well studied and has been reported in a wide variety of disease states as recently reviewed in (Cooke et al., 2003). This oxidative modification represents a potentially mutagenic DNA lesion, as 8-OxoG can undergo a conformational change allowing it to aberrantly pair with adenine and thus promote G to T transversion (Bruner et al., 2000). Peroxynitrite is also capable of reacting with guanine to form 8-nitroguanine (8-NO(2)-G) which is considered a marker of nitrosative DNA damage. Like its ROS-induced counterpart, 8-NO(2)-G promotes formation of mutagenic DNA lesions due to G to T transversion (Yermilov et al., 1995). Similar oxidative/nitrosative modifications have been reported for adenine, thymine, and cytosine (reviewed in (Dizdaroglu and Jaruga, 2012)).
One common consequence of direct oxidative modification of nucleotide bases is formation of apurinic/apyrmidinic (AP) sites along the DNA. For example, the presence of 8-OxoG is known to engage the base excision repair (BER) system resulting in removal of the oxidized guanine by glycosylases including 8-oxoguanine DNA glycosylase (also known as OGG1) (Hazra et al., 2001). AP sites may also result from direct base modifications that disrupt the N-glycosidic bond linking them to deoxyribose and thereby resulting in spontaneous loss of nucleobases (Otterlei et al., 2000). ROS have also been shown to interact with the sugar moieties of nucleotides. In particular, hydroxyl radicals appear to target the C-1 and C-4 positions of the deoxyribose ring. Hydroxyl attack of deoxyribose may result in the formation of multiple oxidation products including 2-deoxyribonolactone, 2 deoxypentos-4-ulose, 3’-phosphates, and 3’-phosphoglycolate esters. These modifications may result in the formation of AP sites by the release of free bases or by initiating the activity of other members of the BER pathway (e.g. AP endonucleases) (Demple and DeMott, 2002; Wilson et al., 2003). It should be noted that AP sites are also formed at an estimated rate of 50,000 – 200,000 per mammalian cell per day under normal physiologic conditions. Interestingly, the rat CNS appears to accumulate a greater number of AP sites when compared to other organ systems (Nakamura and Swenberg, 1999).
Oxidative stress can also cause DNA damage in the form of both single-stranded breaks (SSBs) and double-stranded breaks (DSBs). SSBs form as a result of the interaction of hydroxyl radicals with deoxyribose and subsequent generation of peroxyl radicals. These peroxyl radicals are then responsible for nicking phosphodiester bonds that form the backbone of each helical strand of DNA (Dedon, 2008). In addition, SSBs have also been shown to indirectly form under oxidative/nitrosative conditions through the actions of the BER system in the repair of AP sites (Hegde et al., 2008). Topoisomerase I has also been shown to preferentially cleave nucleotides at the site of oxidative DNA lesions further resulting in the generation of SSBs (Pommier et al., 2003). SSBs found in closely associated sites on complementary DNA strands may also result in the formation of DSBs. Interestingly, peroxynitrite has also been shown as a potent mediator of DSBs in vitro (Jia et al., 2009).
Evidence for DNA Damage in Acute CNS Injuries and Neurodegeneration
DNA Damage in Neurodegenerative Disorders
Perhaps the strongest link between neurodegeneration and DNA damage thus far comes from neurodegenerative phenotypes seen in a variety of hereditary disorders of DNA damage repair. One such example is xeroderma pigmentosum (XP) which occurs as a result of mutations in genes encoding members of the nucleotide excision repair (NER) system. Early-onset, progressive neurological symptoms in xeroderma pigmentosum include peripheral neuropathy, sensorineural deafness, mental disability, bulbar, extrapyramidal, and cerebellar disturbances (e.g. chorea, ataxia, etc.), and dysfunction of the corticospinal tract (Kassubek et al., 2012). Magnetic resonance imaging (MRI) of patients with XP demonstrates cerebral and cerebellar atrophy and accompanying ventricular enlargement (Kraemer et al., 2007). Histological examination of post-mortem tissue from XP patients demonstrates widespread neuronal loss in the corticospinal tract, basal ganglia, substantia nigra pars compacta, cerebellum, and dorsal root ganglia (DRG), explaining many of the clinical findings (Rapin et al., 2000). Recently, neuron-specific knockdown of XPA in different brain regions (forebrain, cerebellum) in transgenic mice has also been shown to cause neuronal loss in these areas (Jaarsma et al., 2011). Another example of neurodegenerative phenotype associated with dysfunctional DNA repair is ataxia-telangiectasia (A–T). A–T results from loss of function mutations in the gene encoding ATM, a serine/threonine kinase that coordinates the cellular response to DNA DSBs (discussed later). Classical neurological symptoms defining A–T include ataxia, speech disturbances, choreoathetosis, and progressive neurodegeneration leaving the individual confined to a wheelchair within the first decade of life (Biton et al., 2008; Jeppesen et al., 2011). Post-mortem tissue demonstrates extensive degeneration of the cerebellar cortex including Purkinje and granule cells. However, neuronal loss is not confined to the cerebellum as late-stage degeneration has also been detected in the cerebral cortex, spinal cord, basal ganglia, and brain stem (Verhagen et al., 2012).
DNA Damage in Spinal Cord Injury
Substantial evidence suggests oxidative/nitrosative stress associated with secondary SCI results in DNA damage in the injured spinal cord. Using antibodies against 8-OxoG, oxidative modification of guanine has been demonstrated beginning at 1 day post-injury and continuing up to 21 days after rat spinal cord contusion by immunoblot analysis (Kotipatruni et al., 2011). Using the Single Cell Gel Electrophoresis (i.e. Comet) assay, DNA SSBs and DSBs were also detected which has been confirmed by other groups in a variety of injury models at both acute and chronic time points (Dagci et al., 2009; Huang et al., 2007; Martin and Liu, 2002). The same study also demonstrated up-regulation of a number of DNA damage response genes including ATM, 8-oxoguanine DNA glycosylase (OGG1), thymine DNA glycosylase, and p53 (see subsequent discussion) at both the protein and mRNA levels. A similar increase in expression of enzymes involved in both the response to and repair of DNA damage has also been reported after spinal cord ischemia-reperfusion injury in rabbits (Lin et al., 2003). Co-localization of the phosphorylated histone variant γH2AX, a reliable marker of DSB formation, with neurofilament proteins around the injury site also suggested that neurons in the injured spinal cord are preferential targets for DNA damage (Kotipatruni et al., 2011). Interestingly, Medalha et al. have demonstrated that acute DNA damage extends beyond the spinal cord in SCI rats to affect blood, liver, and the kidneys using the comet assay to detect DNA strand breaks (Medalha et al., 2012).
Targeting oxidative stress and DNA damage has provided promising results in the quest to find new treatments for SCI. A variety of known anti-oxidants have shown efficacy as therapies for SCI, providing both cellular protection and improved behavioral outcomes in experimental models and clinical trials (reviewed in (Hall, 2011; Jia et al., 2012)). One such anti-oxidant therapy is methylprednisolone (MP) which has been shown to provide a small but significant neurological benefit when given at high doses after acute SCI in humans (Bracken et al., 1990; Bracken et al., 1997). However, its efficacy remains under intense debate and administration of high dose MP is associated with a number of adverse side effects including immunosuppression and increased risk of infection (e.g. pneumonia, urinary tract infection, sepsis, etc.), hyperglycemia, adrenal insufficiency, and even death (Suberviola et al., 2008). Therefore, there is still a significant need for more effective and safer antioxidants for the treatment of spinal cord injury. Our group and others have shown that estrogen (17β-estradiol), a potent antioxidant and scavenger of free radicals, has neuroprotective effects following spinal cord injury (Samantaray et al., 2011; Sribnick et al., 2006; Sribnick et al., 2010; Yune et al., 2004). In particular, we found that both pharmacological and physiological doses of estrogen prevents apoptotic death of both neurons and myelin-producing oligodendrocytes and restores motor function using the Basso Beattie Bresnahan (BBB) locomotor scale following contusion injury in rats. We have also reported similar neuroprotective effects when administering melatonin, another endogenously produced anti-oxidant (Samantaray et al., 2008).
Stronger evidence that direct prevention of DNA damage following SCI results in neural cell protection and improved behavioral outcomes has also been provided using other neuroprotective agents. Administration of the omega-3 polyunsaturated fatty acid docosahexaenoic acid after compression SCI in rats was shown to reduce oxidative stress-associated changes including lipid peroxidation, protein oxidation, and nucleic acid oxidation via labeling of 8-OxoG (Huang et al., 2007). Most importantly, amelioration of oxidative changes including the formation of 8-OxoG by docosahexaenoic acid resulted in significant improvement in locomotor function beginning at 4 days and extending up to 6 weeks post-injury. Administration of a monoclonal antibody (mAb) against the CD11d integrin, an integral protein for leukocyte adhesion, has also been shown to reduce oxidative stress-related DNA oxidation after severe compression injury (Bao et al., 2004). In particular, CD11d mAb prevented infiltration of macrophages into the injured spinal cord and significantly reduced formation of both 8-OxoG and protein carbonylation, another marker of oxidative stress, up to 72 hours post-injury. This is an interesting finding given that CD11d mAb treatment was previously shown to improve a number of neurological outcomes including open-field locomotion (BBB scale and inclined plane scores), mechanical allodynia, and autonomic dysreflexia (changes in mean arterial pressure during balloon distention of the colon) in the same injury model (Gris et al., 2004). The free radical scavenger MCI-186 (Edaravone), given after ischemia-reperfusion injury of the rabbit spinal cord, also prevented acute formation of 8-OxoG and increased expression of apurinic/apyrimidinic endonuclease (APE), an important member of the BER pathway (Takahashi et al., 2004). The molecular changes induced by MCI-186 were associated with preservation of large motor neuron viability and improvement in neurological function after injury when compared to vehicle-treated animals. Taken together, these findings provide strong evidence that interventions which prevent DNA damage and/or increase expression/activity of DNA repair enzymes may provide neurological benefit following spinal cord injury.
DNA Damage in Traumatic Brain Injury and Cerebral Ischemia
Considerable evidence suggests that oxidative stress and resultant DNA damage are also important contributors to the pathophysiology of traumatic brain injury and cerebral ischemia. Using in situ hydroethidine oxidation to ethidium as an indicator of superoxide production, Lewén et al. reported increased oxidative stress following controlled cortical impact (CCI) in mice (Lewen et al., 2001). Superoxide production in this model was associated with increased oxidation of guanine demonstrated by the formation of 8-OxoG in injured animals. Interestingly, this study also reported reduced expression of APE indicating a potential deficiency in DNA damage and repair responses after brain insult. Increases in 8-OxoG have also been reproduced in other experimental models of brain injury and cerebral ischemia (Itoh et al., 2010; Lukic-Panin et al., 2010; Nito et al., 2011; Suganuma et al., 2010). In addition, DNA SSBs have been identified in a rat model of TBI using the DNA polymerase I-mediated biotin-dATP nick-translation (PANT) method beginning at 6 hrs. post-injury in several areas including the ipsilateral cortex, dentate gyrus, CA1, and CA3 regions of the hippocampus (Clark et al., 2001). Similar increases in SSBs have also been reported after transient middle cerebral artery occlusion (MCAO) in rats (Chen et al., 1997).
As is the case with SCI, a number of experimental therapies aimed at preventing oxidative stress and its downstream consequences such as DNA damage have shown particular promise in promoting neurological recovery in brain injury (reviewed in (Hall et al., 2010)). A thorough description of pre-clinical studies using antioxidant therapy in TBI and cerebral ischemia is beyond the scope of this review. As might be expected, significant overlap exists between the antioxidant agents used in TBI and cerebral ischemia and those used in experimental models of SCI. For example, recent evidence suggests that MCI-186 (Edaravone) also reduces oxidative stress-related events including formation of 8-OxoG and lipid peroxidation following TBI in rats (Itoh et al., 2010). Amelioration of oxidative events was associated with improved spatial memory performance on a Morris Water Maze (MWM) task and reduced apoptosis in neural cells. Similar neuroprotective effects for MCI-186 have also been reported in a weight-drop model of TBI in rats (Wang et al., 2011a). Because of its strong potential as a therapeutic agent, MCI-186 has received approval for use in patients with cerebral infarct in Japan. Although evidence for clinical efficacy of MCI-186 in cerebral ischemia is limited, clinical trial data appears at least somewhat promising (Feng et al., 2011). Administration of the immunosuppressant FK506 (Tacrolimus), which is currently in clinical use to prevent organ transplant rejection, has also been shown to prevent oxidative DNA damage and reduce neurological deficit following MCAO-induced cerebral ischemia (Nito et al., 2011). Also of particular interest in TBI is the steroid hormone progesterone (PROG). Like its counterpart estrogen (discussed above), PROG has multiple actions that may contribute to neuroprotection following CNS insult. PROG possesses antioxidant activity and has been shown to prevent lipid peroxidation in a rat model of TBI (Roof et al., 1997). To our knowledge, there is no direct evidence to show that PROG treatment also prevents oxidative damage to DNA in this condition. However, given the well-characterized actions of PROG against oxidative stress, it is likely that protection of DNA against ROS/RNS attack is also a consequence of administration of this steroid hormone. Phase II clinical trails in TBI patients have generated promising results suggesting PROG may have neurological benefit and larger, multi-center Phase III trials (ProTECT III; www.clinicaltrials.gov) are now underway (Wright et al., 2007).
It is important to acknowledge that the antioxidant and anti-inflammatory agents discussed thus far in this review have multiple actions that contribute to neuroprotection following acute CNS injury. Therefore, it is difficult to resolve the individual contribution of blockade of oxidative DNA damage to the overall neuroprotective effects of these drugs. Put another way: how do we know that prevention of DNA oxidation is truly involved in protection against CNS insult when compared to other antioxidant and anti-inflammatory actions (e.g. reduction of lipid peroxidation, protein oxidation, etc.)? More direct evidence of defining the contribution of oxidative DNA damage to acute neurodegeneration and its role as a therapeutic target is necessary to fully understand this issue.
Endogenous DNA Repair Systems in Neurons
As described above, deficiencies in the various DNA repair systems may result in neurodegenerative phenotypes (Biton et al., 2008; Jaarsma et al., 2011; Jeppesen et al., 2011; Kraemer et al., 2007; Rapin et al., 2000; Verhagen et al., 2012). However, the mechanisms by which oxidative DNA damage induces neuronal degeneration and how these effects may be reversed by DNA repair systems remains largely unknown. This is particularly important given that post-mitotic neurons are not readily replaced following irreversible damage. Recent studies have reported that cell cycle re-activation following intensive DNA damage leads to S-phase reentry of neuronal cells, which may promote DNA repair or induce apoptosis depending on the context of cellular insult (Kruman, 2004). Determining the roles and interactions between multiple DNA repair pathways following CNS insult is therefore of particular interest. However, endogenous DNA repair is complex and often involves overlapping mechanisms that are coordinated based on the type and severity of DNA damage (Marinoglou, 2012; Melis et al., 2012). The purpose of this section is to outline various systems responsible for repair of both SSBs (BER, NER, mismatch repair [MMR]) and DSBs (homologous recombination [HR] and nonhomologous end-joining [NHEJ]).
BER is the major DNA repair pathway responsible for maintaining genomic integrity in neurons following DNA SSBs through removal of damaged/oxidized bases initiated by a family of enzymes known as the DNA glycosylases (Swain and Rao, 2012). BER may be completed by one of two sub-pathways: short-patch BER that is capable of repairing only one nucleotide and long-patch BER which may replace between 2–13 nucleotides (Fortini and Dogliotti, 2007; Swain and Rao, 2012; Wilson and Bohr, 2007; Wilson and McNeill, 2007). Generally, activation of BER results in five sequential steps to repair DNA lesions: 1) excision of damaged bases, 2) cutting of the DNA backbone at the AP site 3) clean-up of the DNA terminal ends, 4) synthesis of replacement nucleotides and 5) sealing of the DNA nick (Swain and Rao, 2012; Wilson and McNeill, 2007). Expression of several essential enzymes comprising the BER machinery has recently been observed in the CNS including: DNA glycosylases which recognize and remove damaged bases to form AP sites for repair; AP endonuclease 1 (APE1) responsible for cleaving the remaining AP site; DNA polymerase β (POLβ) for nucleotide replacement; X-ray cross-complementing 1 (XRCC1) which acts as a scaffolding protein for the BER machinery; and DNA ligases to catalyze reformation of phosphodiester bonds (McMurray, 2005; Wilson and Bohr, 2007; Wilson and McNeill, 2007). Interestingly, recent studies also suggest that neuronal BER activity is reduced in an age-dependent manner which might be associated with increasing incidence of neurodegenerative disorders in aged individuals (Chen et al., 2002; Gredilla et al., 2010; Gredilla et al., 2012; Imam et al., 2006; Lovell et al., 2000; Wang et al., 2005). Cabelof et al. have further attributed these deficiencies in BER to age-dependent reductions in expression (at both the mRNA and protein levels) and activity of POLβ (Cabelof et al., 2002). Independent addition of uracil DNA-glycosylase (UDG), OGG1, APE1, POLβ or T(4) DNA ligase was not capable of restoring BER activity in neurons extracted from adult and old brains. However, a combination of POLβ and T(4) DNA ligase or a cocktail containing all of these enzymes significantly reduced loss of BER activity in aged neurons (Swain and Rao, 2012). Taken together, these findings suggest that deficiencies in both POLβ and DNA ligase activity may explain the loss of BER in the aging brain.
The NER pathway also plays an important role in maintenance of both DNA SSBs and neuronal fate. The NER system is comprised of over 30 proteins which act to recognize and remove damaged/oxidized nucleotides within DNA lesions (Cleaver et al., 2009; Nouspikel and Hanawalt, 2002). NER is divided into two distinct mechanisms including global genomic NER (GG-NER) which repairs damaged nucleotides from the entire genome and transcription-coupled NER (TC-NER) that removes nucleotide lesions from regions of DNA undergoing active transcription (Robu et al., 2013). Activation of TC-NER occurs as RNA polymerase II activity stalls at the site of the DNA lesion. In contrast, recognition of nucleotide damage by a variety of damage-sensing proteins including DNA-damage binding (DDB) proteins DDB1 and DDB2 and the XPC/RAD23b complex is responsible for initiation of GG-NER (Fei et al., 2011). Although these systems differ in the mechanisms by which they are activated, GG-NER and TC-NER utilize the same machinery for lesion incision, repair and ligation to repair neuronal DNA damage (Fishel et al., 2007). Accumulating evidence support the notion that defects in normal NER function may lead to severe neuronal dysfunction and neurodegenerative phenotypes associated with disorders such as XP, AT, trichothidystrophy (TTD) and cockayne syndrome (CS) as described above (Fishel et al., 2007; Jaarsma et al., 2011; Kraemer et al., 2007; Rapin et al., 2000).
MMR can recognize and repair mismatched nucleotides which are incorrectly incorporated into the DNA structure (Fishel et al., 2007). Nucleotide mismatch can occur for a number of reasons including erroneous incorporation of nucleotides by DNA polymerases and damage to nucleotides before their incorporation. Isolated adult rat neurons have been shown to possess the machinery necessary to correct G–T and G–U mismatches (Brooks et al., 1996). More recent studies have shown that several proteins involved in MMR are expressed in neuronal cells including MSH2, the MSH2–MSH6 complex, thymine DNA glycosylase (TDG) and MLH1 (Marietta et al., 1998). Interestingly, Francisconi et al. have shown that exposure of differentiated SH-SY5Y neuroblastoma cells to oxidative stress (H2O2) results in nuclear translocation and induction of MSH2 activity (Francisconi et al., 2005).
Although, DNA DSB-induced biochemical alterations are not well characterized in neuronal cells, this type of DNA damage can have severe consequences following CNS injury leading to rapid induction of apoptosis in neurons (Lee and McKinnon, 2007). However, there are systems which act to repair DNA DSBs and have been shown to encourage neuronal survival in some contexts. The first of these systems, NHEJ, acts to directly ligate DNA DSBs without the need for a homologous template. NHEJ involves variety of repair enzymes and associated factors such as Ku70, Ku80, DNA ligase IV, XRCC4 and DNA-PKcs (Hefferin and Tomkinson, 2005). Mice deficient in NHEJ components demonstrate marked apoptosis during normal neuronal development (Sekiguchi et al., 1999). In addition, induction of Ku70 at the mRNA and protein levels has been noted in hippocampal CA1 neurons following transient global ischemia and was directly correlated with neuronal survival (Sugawara et al., 2001). It should be noted that another DSB repair mechanism, known as homologous recombination (HR) also exists, but very little is known about its involvement in neurons.
Transgenic Animal Models: Window to A Better Understanding the Role of DNA Damage in Acute CNS Insult?
Transgenic animal models have begun to provide stronger, more direct evidence suggesting that oxidative-stress induced DNA damage is a critical player in the pathophysiology of TBI and cerebral ischemia. Unfortunately, similar studies in SCI are still lacking. Liu et al. have investigated the role of OGG1, a glycosylase responsible for the excision of 8-OxoG as discussed previously, in biochemical and neurological outcomes following permanent MCAO in OGG1−/− mice (Liu et al., 2011). As expected, OGG1-deficient mice were found to have significantly reduced excision of 8-OxoG both under normal conditions and following ischemic stroke. Lack of OGG1 also resulted in increased oxidative modification of nucleotide bases after cerebral ischemia. Wild-type mice in this study demonstrated marked up-regulation of OGG1 after MCAO, suggesting that expression/activity of this enzyme represents a compensatory mechanism to prevent further cellular damage under ischemic conditions. In support of this hypothesis, cortical neurons cultured from OGG1-deficient mice were more susceptible to oxidative stress-induced cell death. Most importantly, OGG1−/− mice demonstrated significantly increased infarct volume and poorer locomotor performance on the rotarod test after cerebral ischemia when compared to their wild-type littermates. It should be noted, however, that OGG1-deficient animals also demonstrated poorer baseline rotarod performance.
A role for endonuclease VIII-like 1 (NEIL1), another DNA glycosylase that is capable of excising a number of oxidatively-modified nucleotide bases (e.g. 5-hydroxycytosine, thymine glycol, etc.), in cellular protection against cerebral ischemia has also been defined (Canugovi et al., 2012). NEIL1-null mice showed greater mortality, increased infarct area, and more severe neurological deficits following transient MCAO and reperfusion (MCAO/R) when compared to their wild-type littermates. Rotarod tests also demonstrated that NEIL1−/− mice experiencing cerebral ischemia had increased number of falls over the experimental period and reduced latency to first fall. Counts of TUNEL+ apoptotic cells were also significantly greater in the NEIL1-deficient animals, further confirming a role for DNA repair in cellular protection following CNS insult.
Tomasevic et al. have shown that at least one protein involved in the NER system plays a critical role in the extent of neurological dysfunction following TBI (Tomasevic et al., 2012). Mice deficient in the gene encoding XPA, which is also commonly mutated in individuals with XP, had significantly delayed locomotor recovery (measured by composite neurological score and rotarod) and impaired spatial memory (MWM task) following CCI injury when compared to XPA+/+ controls. However, it must be noted that these neurological deficits could not be attributed to differences in lesion volume, neurogenesis, damage to hippocampal regions, or cell loss between injured XPAdeficient and control animals. Given the previously described findings in OGG1 and NEIL1 knockout mice and the characteristic loss of neurons seen in individuals with XP, these discrepancies are difficult to explain. However, the authors provide a plausible explanation that, while changes in neural cell viability after TBI are similar between groups, there may be greater loss of normal function in these cells in XPA−/− mice contributing to the difference in behavioral outcomes.
Effects of DNA Damage on Neuronal Viability
DNA Damage Sensors and their Downstream Effectors: Phosphatidylinositol 3-kinase-like kinases
It is well known that excessive oxidative damage to DNA may overwhelm innate repair mechanisms and contribute to neuronal death in neurodegenerative conditions. Mechanisms by which oxidative DNA modifications result in neuronal degeneration remain a topic of considerable interest. The cell has developed a rather complex machinery to sense and respond to DNA damage. Among the sensors of DNA damage are specific members of the phosphatidylinositol 3-kinase-like kinase (PIKK) family of serine/threonine kinases including ATM, Ataxia-telangiectasia and Rad-3 related (ATR), and the DNA-dependent protein kinase catalytic subunit (DNA-PKcs). PIKKs respond to different forms of DNA damage to initiate downstream molecular cascades. For example, ATM and DNA-PKcs specifically respond to the presence of DNA DSBs, whereas ATR is activated by SSBs and replication fork stalling (Ditch and Paull, 2012). Although PIKK activation is intended to initiate the appropriate cellular machinery for repairing damaged DNA, it may also contribute to neurodegenerative changes by directly activating apoptotic signaling cascades. Contusion SCI in the rat has been reported to promote sustained up-regulation of both ATM and ATR up to 3 weeks after injury (Kotipatruni et al., 2011). In addition, increased DNA binding activity of the Ku70/80 heterodimer, a major activator of DNA-PKcs, has also been observed following ischemia-reperfusion injury in the rabbit spinal cord (Shackelford et al., 1999). Phosphorylation targets of PIKKs that may contribute to DNA damage-induced neuronal death include p53, checkpoint kinases (Chk1, Chk2), and H2AX. Although this review focuses on the mechanisms by which activation of PIKKs contributes to neurodegeneration, it should be noted that the physiologic function of these proteins in repairing DNA damage may also have neuroprotective effects. For example, hippocampal neurons cultured from mice lacking DNA-PK have enhanced sensitivity to a variety to cellular insults including direct DNA damage, amyloid β exposure, and glutamate excitotoxicity (Culmsee et al., 2001). Further investigation is needed to understand the mechanisms by which PIKKs control neuronal fate (i.e. engagement of protective DNA repair vs. apoptotic cell death) in the context of CNS insult.
p53 as a Downstream Target of PIKKs in Response to DNA Damage: Role in Induction of Apoptosis
Phosphorylation of serine residues in p53 by PIKKs has two important consequences: activation of p53 signaling and increased resistance of p53 to proteasomal degradation thereby enhancing its stability (Culmsee and Mattson, 2005). The case for involvement of p53 in neuronal apoptosis following genotypic stress is undeniable. Once activated, p53 enhances transcription of a number of genes involved in the process of programmed cell death including pro-apoptotic members of the Bcl-2 family (Bax, Bad, Bid, Noxa, Puma), apoptotic protease-activating factor 1 (APAF1; an essential mediator of apoptosome formation), and the apoptosis regulatory protein SIVA1 (Chatoo et al., 2011; Culmsee and Mattson, 2005). Interestingly, p53 also appears to have a variety of pro-oxidant activities in the CNS which may further exacerbate cellular injury associated with oxidative stress. In support of a role for p53 in cell death after CNS injury, increased levels of total p53 and phosphorylated p53 were noted in the contused rat spinal cord (Kotipatruni et al., 2011). These changes were associated with increased p53-mediated transcriptional activity and up-regulation of its downstream targets including Bax and Apaf1. p53 signaling in this study was also associated with elevation in classical markers of apoptosis such as increased numbers of TUNEL+ cells in the caudal penumbra and cleavage/activation of both caspase-3 and caspase-9. Similar studies using experimental models of TBI and cerebral ischemia have also described a role for neuronspecific induction of p53 activity in neuronal death (Plesnila et al., 2007; Yamaguchi et al., 2002). Recently, p53 has received attenuation as a therapeutic target in CNS injuries. Using pifithrin-α (PFT-α), a specific inhibitor of p53 transcriptional activity, Plesnila et al. demonstrated reduced lesion volume and improved neurological function (beamwalking and novel object recognition tasks) in a mouse model of CCI (Plesnila et al., 2007). Similar findings have also been reported in other experimental models of brain injury using both pharmacological and genetic approaches to reduce p53 activity (Leker et al., 2004; Nijboer et al., 2011; Yonekura et al., 2006). However, it should be noted that the role of p53 in the pathophysiology of CNS injuries is complex and remains to be fully characterized. A growing body of work suggests that p53 may also promote neuronal and axonal regeneration after cellular insult (Tedeschi and Di Giovanni, 2009). These differences may attributed to a variety of factors including the type of injury, severity of injury, time point at which p53 activity is examined, and involvement of other signaling pathways. Interestingly, recent studies have also defined a new role for p53 in initiating necrosis in the context of cerebral ischemia-reperfusion injury (Vaseva et al., 2012).
It should be noted that p53 activation is not unique to PIKKs as other signaling cascades known to contribute to neuronal death following CNS injury also enhance p53 activity. Of particular interest is the family of calcium-dependent neutral proteases known as calpains. Involvement of calpains has been reported in animal models of SCI, TBI, and ischemic stroke (Bartus et al., 1994; Sribnick et al., 2007; Yamada et al., 2012). Recent experimental evidence suggests that calpain may activate p53 following induction of direct DNA damage in primary cortical neurons in vitro (Sedarous et al., 2003). Pharmacological inhibition of calpain also prevented induction of p53 and protected against cell death following camptothecin exposure. Taken together, these findings suggest that calpain may also be a therapeutic target of interest to prevent pro-apoptotic activation of p53 in response to DNA damage.
Posttranslational regulation of p53 also plays important role in determining cell fate. For example, acetylation of p53 at Lys320 and Lys373 has been shown to enhance neurite outgrowth and neuronal maturation independently of cell survival. Acetylation of the same residues may also promote cell cycle arrest and apoptotic signaling depending on cellular context, especially when DNA repair systems are overwhelmed leading to cell death. Interestingly, ROS have also been shown to directly modulate the DNA binding capacity of p53 by oxidizing cysteine residues within the DNA binding domain leading to conformational changes. ROS-mediated alterations in p53 DNA binding may also have a significant impact on cell fate.
DNA Damage Sensors and their Downstream Effectors: Poly(ADP-ribose) polymerase-1
Poly(ADP-ribose) polymerase-1 (PARP-1) is another sensor of oxidative DNA damage which has been implicated in the pathophysiology of acute neurodegeneration. Although PARP-1 plays an important role in the physiological repair of DNA damage, massive activation of PARP-1 upon its binding to DNA SSBs formed under genotoxic stress (such as oxidative stress) is also known to initiate a number of downstream signaling events which may contribute to neuronal death. An important consequence is PARP-1-mediated cleavage of nicotinamide adenine dinucleotide (NAD+) to generate polymers of ADP-ribose (PAR) that act as a signal to other DNA repair proteins. NAD+ participates in the redox reactions underlying the oxidative phosphorylation pathway, and is thus essential for the formation of ATP under normal conditions. In the case of excessive DNA damage, PARP-1 becomes overactive and may exhaust NAD+, leading to mitochondrial dysfunction, depletion of energy stores, and eventual necrosis (Ha and Snyder, 1999). Increased formation of PAR (indicating PARP-1 activation) in an MCAO model of stroke was associated with a significant reduction in NAD+ levels in the injured hemisphere (Endres et al., 1997). In the same study, PARP−/− mice demonstrated both increased levels of NAD+ and reduced infarct volume following cerebral ischemia, indicating an important role for PARP-mediated depletion of cellular energy stores in neurodegeneration. In addition, exogenous administration of NAD+ appears to have neuroprotective effects in experimental models of CNS injury (Won et al., 2012; Ying et al., 2007). There remains considerable debate regarding the contribution of energy depletion to PARP-1-mediated cell death (Goto et al., 2002). Although the mechanisms of PARP-1-mediated necrosis have not been fully elucidated, it is important to note that there are several signaling pathways involved. Recent findings suggest that the step-wise activation of PARP-1, calpains (discussed above), and Bax may be required for necrosis induced by DNA damage in vitro (Moubarak et al., 2007). These findings further support the idea that calpain is an essential mediator of DNA damage-induced cellular death and may therefore represent a strong therapeutic target in CNS injury.
PARP-1 activity may also initiate neuron death through its effects on a mitochondrial protein known as apoptosis-inducing factor (AIF). PARP-1 activation in the context of DNA damage can result in the translocation of AIF from the mitochondria to the nucleus via binding of PAR to AIF (Wang et al., 2011b). Once inside the nucleus, AIF initiates caspase-independent cell death characterized by chromatin condensation and large DNA fragmentation (approximately 50 kilobases in size) which was subsequently termed parthanatos (Wang et al., 2009). Although not as well studied as the classical forms of cell death, experimental evidence indicates that parthanatos contributes to neuronal loss after cerebral ischemia and excitotoxic brain injury (Andrabi et al., 2011). Harlequin mice that express markedly reduced levels of AIF (80% reduction compared to wild-type) have also shown reduced infarct volume following transient cerebral ischemia when compared to C57BL/6 controls further generating interest in AIF as a therapeutic target for CNS insult (Culmsee et al., 2005).
The Telomeric Complex in Oxidative DNA Damage and Neurodegeneration
The Telomeric Complex as a Target for Oxidative DNA Damage
Telomeres consist of a series of non-coding, hexanucleotide repeats (TTAGGG) found at the end of linear chromosomes that serve to ensure genomic stability by preventing the loss of coding sequences during cell division. The telomeric complex also contains a number of auxillary proteins including the telomerase enzyme, telomere repeat binding factor 1 (TRF1), telomere repeat binding factor 2 (TRF2), and protection of telomeres 1 (POT1) that regulate telomere structure and dynamics and guard against recognition of chromosome ends as DNA DSBs (reviewed in (Giraud-Panis et al., 2010)). Telomerase, an enzyme consisting of a catalytic subunit known as telomerase reverse transcriptase (TERT) and an RNA template (telomerase RNA component; TERC), is responsible for maintaining telomere length by the addition of TTAGGG sequences to the chromosome end. Recent studies suggest that telomeres are preferential targets of DNA damage under oxidative and genotoxic conditions (Hewitt et al., 2012; Rhee et al., 2011). Recent studies have shown that telomerase and other telomere-associated proteins may have an important impact on neuronal viability. For example, TRF2 may prevent ATM-mediated initiation of oxidative DNA damage signaling (Denchi and de Lange, 2007) possibly by inhibiting autophosphorylation and subsequent activation of ATM (Karlseder et al., 2004). POT1, which maintains stability of telomeric ends, is also known to inhibit another DNA damage kinase ATR (Hockemeyer et al., 2005). Both ATM and ATR are known to initiate apoptotic neuronal death in the context of DNA damage through activation of p53. Chin et al. have demonstrated that p53 deletion inhibits the proapoptotic effects of telomere loss (Chin et al., 1999). Interestingly, recent studies also indicate that p53 is capable of inhibiting TRF2, resulting in subsequent ATM activation and establishing a positive feedback loop whereby p53 augments adverse responses to telomere uncapping and loss and further enhances widespread p53 activation (Horikawa et al., 2011). Together, these findings suggest that both the TRF2-ATM-p53 and POT1-ATR-p53 pathways are activated in response to DNA damage which occurs with telomere uncapping. Therefore, we propose that the telomeric complex may represent a novel therapeutic target downstream of both oxidative stress and DNA damage in the context of acute neurodegeneration.
Telomeres and Telomerase In Neurological and Neurodegenerative Disorders
Telomeres and telomerase have largely been investigated for their roles in cancer and cellular senescence in mitotic cells. However, recent studies have linked dysfunction of the telomeric complex to a variety of disease states. One such example is dyskeratosis congenita (DC) which results from inherited defects in several proteins involved in telomere maintenance (including TERT and TERC). DC is characterized by short telomeres, bone marrow failure, and increased cancer risk. In addition, neurological disturbances including learning difficulties, mental retardation, and microcephaly have also been reported in patients with DC (Nelson and Bertuch, 2012). A severe variant of DC known as Hoyeraal-Hreidarsson Syndrome (HHS) shares similar neurological features in addition to cerebellar hypoplasia. Similarly, transgenic animal models have shed light on the role of the telomeric complex in normal CNS function and development. Late-generation mice possessing a tamoxifen-inducible knock-in allele for TERT showed no detectable telomerase and demonstrated reduced brain weights, lower numbers of mature oligodendrocytes, and dysfunctional myelination (Jaskelioff et al., 2011). In addition, TERT−/− mice exhibit anxiety-like behavior and impaired olfactory function (Lee et al., 2010). It should also be noted that shortened leukocyte telomere length has been associated with neurodegenerative conditions in humans. Most interestingly, significantly shorter leukocyte telomere length was reported in patients with Alzheimer’s disease (AD) when compared to age-matched healthy controls (Thomas et al., 2008). However, it is unclear whether shortened telomere length was a cause or consequence of disease in this study since hippocampal cells derived from the AD brain showed significantly greater telomere length. Further investigation is needed to determine the role of telomere erosion in neurodegeneration.
Evidence for Telomerase as a Therapeutic Target in CNS Injury: In Vitro Studies
Although telomerase activity is considered to be absent (or at least undetectable) in post-mitotic neurons, expression of telomerase has been reported in multiple neuronal subtypes including rat spinal cord motor neurons and hippocampal neurons in vitro and cerebellar Purkinje neurons in vivo (Eitan et al., 2012a; Niu and Yip, 2011; Zhu et al., 2000). Mounting evidence suggests that telomerase, and especially its catalytic subunit TERT, may have anti-apoptotic activity in the face of neuronal insult which could be exploited as a therapeutic target in acute neurodegeneration. TERT overexpression in rat pheochromocytoma PC12 cells (used widely as an in vitro neuronal model) rendered these cells significantly more resistant to direct DNA damage by the topoisomerase inhibitors etoposide and camptothecin (Lu et al., 2001). Conversely, antisense knockdown of TERT in cultured hippocampal neurons increased their sensitivity to the same DNA damaging agents. Similar neuroprotective roles for TERT have also been described in in vitro models of oxidative stress and excitotoxicity (Fu et al., 1999; Kang et al., 2004).
The mechanisms by which telomerase exerts anti-apoptotic effects in neurons remain to be fully elucidated. Several studies suggest that the canonical function of telomerase in promoting genomic stability is required for its protective effects against neuronal insult. Using site-directed mutagenesis, Zhang et al. demonstrated that the reverse transcriptase domain of TERT is required for protection against both staurosporine- and camptothecin-induced apoptosis in HeLa cells (Zhang et al., 2003). Further evidence suggests that TERT may act via several mechanisms to suppress both the intrinsic and extrinsic pathways of apoptosis (reviewed in (Li et al., 2011)).
It should also be noted that non-canonical, extra-telomeric functions of telomerase may also contribute to cellular protection against oxidative damage. Under conditions of persistent hyperoxia or insult with hydrogen peroxide in MRC5 lung fibroblasts, Ahmed et al. reported that TERT does not combat against telomere shortening and is instead excluded from the nucleus (Ahmed et al., 2008). Extranuclear TERT co-localized with mitochondrial staining indicating mitochondrial translocation of this protein under oxidative conditions. In addition, overexpression of TERT (which remained excluded from the nucleus) resulted in significant preservation of mitochondrial DNA integrity and mitochondrial membrane potential. As expected, protection of mitochondria in these cells reduced their production of both superoxide and peroxide. However, this remains an area of considerable debate as other studies have suggested that mitochondrial translocation of TERT may contribute to both mitochondrial damage and apoptotic cell death in fibroblasts (Santos et al., 2006). Thus, further studies are needed to fully understand the role of mitochondria-localized TERT in cell death and particularly how this affects neuronal viability.
Evidence for Telomerase as a Therapeutic Target in CNS Injury: In Vivo Studies
The seminal finding that re-activation of telomerase could prevent degenerative changes in the brain (i.e. reduced brain weight, decreased number of mature oligodendrocytes, and dysmyelination discussed above) in late-generation mice with a tamoxifen-inducible knock-in allele for TERT has generated significant interest in telomerase as a therapeutic target for neurodegeneration (Jaskelioff et al., 2011). However, even before this development, experimental evidence suggested that telomerase activity protects against a variety of CNS insults. Kang et al. reported that transgenic mice engineered to overexpress TERT had significantly reduced infarct volume following permanent occlusion of the MCA (Kang et al., 2004). Interestingly, TERT mRNA levels were also significantly increased in the wild-type mouse brain in response to MCAO, suggesting that telomerase induction might represent an endogenous compensatory mechanism to protect against ischemic injury in the brain. Further studies have confirmed TERT up-regulation at the protein level in both neurons and astrocytes up to 96 hrs. after hypoxic-ischemic injury in the rat (Qu et al., 2011). Telomerase-mediated protection in this study was attributed in part to increases in cell cycle regulatory proteins (p15) and neurotrophin-3 in astrocytes. To our knowledge, it is unknown whether similar changes occur in telomerase expression and activity following SCI or TBI.
Also of note is a recent report demonstrating beneficial effects of pharmacological telomerase stimulation in NMDA-mediated excitotoxicity and in the SOD1 transgenic mouse model of amyotrophic lateral sclerosis (ALS) (Eitan et al., 2012b). In this study, the authors used AGS-499, a novel triaryl compound to induce expression and activity of telomerase in various regions of the CNS including the forebrain, brainstem, and spinal cord in a dose-dependent manner. Pre-administration AGS-499 increased overall survival and ameliorated neurological deficits in CD-1 mice exposed to NMDA. Similarly, AGS-499 treatment at the onset of symptoms in SOD1 transgenic mice significantly delayed disease progression and development of locomotor deficits. The protective effects of AGS-499 also lead to significant improvement in spinal cord motor neuron viability; AGS-499 SOD1 mice had 60% greater motor neuron survival when compared to vehicle-treated animals at the same age. This is of particular interest in SCI where death of motor neurons is a significant contributor to neurological deficits including paralysis. Taken together, these findings suggest that telomerase and other components of the telomeric complex may represent novel therapeutic targets to promote neuronal survival and improved outcomes after acute CNS injury. However, it should be noted that telomerase (and TERT in particular) is expressed at either very low or nondetectable levels in mature neurons. Therefore, there remain a number of concerns regarding whether telomerase reactivation is an appropriate strategy to attenuate CNS injury. In particular, it will be of utmost importance to characterize the effects of telomerase reactivation on glial populations (astrocytes, microglia, oligodendrocytes) and other mitotic support cells within the CNS. Future studies should be aimed at addressing these important questions.
Conclusion
Oxidative stress is a major contributor to the pathophysiology of CNS injuries including SCI, TBI, and cerebral ischemia. Oxidative damage in the CNS occurs in many forms including lipid peroxidation, protein oxidation, and DNA damage. Effects of excessive ROS/RNS production on DNA include oxidative base lesions, DNA single strand breaks, and double strand breaks. When left unrepaired, oxidative DNA damage can initiate a number of downstream events that contribute to neuronal death in CNS injury including p53 activation, PARP-1 signaling, and cell cycle re-entry. Mounting evidence suggests that DNA damage may represent a viable therapeutic target to ameliorate both neuronal death and neurological deficits associated with these conditions. In addition, recent evidence suggests that the telomere and its associated proteins (e.g. telomerase) may regulate the neuronal response to oxidative stress and DNA. We therefore propose in this review that the telomeric complex may represent a novel means to promote neuroprotection in the injured brain and spinal cord. Exciting work remains to be done in both the fields of DNA damage and telomere dynamics as they relate to acute CNS injuries and neurodegeneration.
Research Highlights.
Oxidative stress is a major contributor to acute CNS injury and disease.
A major consequence of excessive ROS/RNS production is DNA damage.
Unrepaired DNA damage initiates signaling cascades for neuron death.
The telomeric complex may modulate the pro-apoptotic response to DNA damage.
DNA damage and telomerase remain strong candidates for therapy in CNS injury.
Acknowledgements
The authors would like to thank Dr. Supriti Samantaray for her helpful comments and critical revision of this manuscript. Support for this work was provided by the National Institutes of Health (NIH) / National Institute of Neurological Disorders and Stroke (NINDS): (NS-31622, NS-62327) and the State of South Carolina Spinal Cord Injury Research Fund.
Abbreviations
- MDA
malondialdehyde
- 4-HNE
4-hydroxynonenal
- EAE
experimental allergic encephalomyelitis
- MS
mutiple sclerosis
- SSB
single strand break
- DSB
double strand break
- 8-OxoG
8-hydroxyguanosine
- 8-NO(2)-G
8-nitroguanine
- AP
apurinic/apyrmidinic
- OGG1
8-oxoguanine DNA glycosylase
- XP
xeroderma pigmentosum
- ATM
ataxia-telangiectasia mutated
- MP
methylprednisolone
- BBB
Basso Beattie Bresnahan
- APE
apurinic/apyrimidinic endonuclease
- PANT
DNA polymerase I-mediated biotin-dATP nick-translation
- PROG
progesterone
- NEIL1
endonuclease VIII-like 1
- PIKK
phosphatidylinositol 3-kinase like kinase
- DNA-PKcs
DNA-dependent protein kinase catalytic subunit
- Chk
checkpoint kinase
- APAF1
apoptotic protease-activating factor 1
- PFT-α
pifithrin-α
- PARP-1
Poly (ADP-ribose) polymerase-1
- NAD
nicotinamide adenine dinucleotide
- AIF
apoptosis-inducing factor
- CCI
controlled cortical impact
- TRF
telomere repeat binding factor
- POT1
protection of telomeres 1
- TERT
telomerase reverse transcriptase
- TERC
telomerase RNA component
- DC
dyskeratosis congenita
- HHS
Hoyeraal-Hreidarsson Syndrome
- SOD1
superoxide dismutase 1
- ALS
amyotrophic lateral sclerosis
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Joshua A. Smith, Email: smijo@musc.edu.
Sookyoung Park, Email: parsoo@musc.edu.
James S. Krause, Email: krause@musc.edu.
Naren L. Banik, Email: baniknl@musc.edu.
References
- Ahmed S, Passos JF, Birket MJ, Beckmann T, Brings S, Peters H, Birch-Machin MA, von Zglinicki T, Saretzki G. Telomerase does not counteract telomere shortening but protects mitochondrial function under oxidative stress. J Cell Sci. 2008;121:1046–1053. doi: 10.1242/jcs.019372. [DOI] [PubMed] [Google Scholar]
- Andrabi SA, Kang HC, Haince JF, Lee YI, Zhang J, Chi Z, West AB, Koehler RC, Poirier GG, Dawson TM, Dawson VL. Iduna protects the brain from glutamate excitotoxicity and stroke by interfering with poly(ADP-ribose) polymer-induced cell death. Nat Med. 2011;17:692–699. doi: 10.1038/nm.2387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ansari MA, Roberts KN, Scheff SW. Oxidative stress and modification of synaptic proteins in hippocampus after traumatic brain injury. Free Radic Biol Med. 2008;45:443–452. doi: 10.1016/j.freeradbiomed.2008.04.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bao F, Chen Y, Dekaban GA, Weaver LC. An anti-CD11d integrin antibody reduces cyclooxygenase-2 expression and protein and DNA oxidation after spinal cord injury in rats. J Neurochem. 2004;90:1194–1204. doi: 10.1111/j.1471-4159.2004.02580.x. [DOI] [PubMed] [Google Scholar]
- Bartus RT, Hayward NJ, Elliott PJ, Sawyer SD, Baker KL, Dean RL, Akiyama A, Straub JA, Harbeson SL, Li Z, et al. Calpain inhibitor AK295 protects neurons from focal brain ischemia. Effects of postocclusion intra-arterial administration. Stroke. 1994;25:2265–2270. doi: 10.1161/01.str.25.11.2265. [DOI] [PubMed] [Google Scholar]
- Berlett BS, Stadtman ER. Protein oxidation in aging, disease, and oxidative stress. J Biol Chem. 1997;272:20313–20316. doi: 10.1074/jbc.272.33.20313. [DOI] [PubMed] [Google Scholar]
- Biton S, Barzilai A, Shiloh Y. The neurological phenotype of ataxia-telangiectasia: solving a persistent puzzle. DNA Repair (Amst) 2008;7:1028–1038. doi: 10.1016/j.dnarep.2008.03.006. [DOI] [PubMed] [Google Scholar]
- Bracken MB, Shepard MJ, Collins WF, Holford TR, Young W, Baskin DS, Eisenberg HM, Flamm E, Leo-Summers L, Maroon J, et al. A randomized, controlled trial of methylprednisolone or naloxone in the treatment of acute spinal-cord injury. Results of the Second National Acute Spinal Cord Injury Study. N Engl J Med. 1990;322:1405–1411. doi: 10.1056/NEJM199005173222001. [DOI] [PubMed] [Google Scholar]
- Bracken MB, Shepard MJ, Holford TR, Leo-Summers L, Aldrich EF, Fazl M, Fehlings M, Herr DL, Hitchon PW, Marshall LF, Nockels RP, Pascale V, Perot PL, Jr, Piepmeier J, Sonntag VK, Wagner F, Wilberger JE, Winn HR, Young W. Administration of methylprednisolone for 24 or 48 hours or tirilazad mesylate for 48 hours in the treatment of acute spinal cord injury. Results of the Third National Acute Spinal Cord Injury Randomized Controlled Trial. National Acute Spinal Cord Injury Study. JAMA. 1997;277:1597–1604. [PubMed] [Google Scholar]
- Brooks PJ, Marietta C, Goldman D. DNA mismatch repair and DNA methylation in adult brain neurons. J Neurosci. 1996;16:939–945. doi: 10.1523/JNEUROSCI.16-03-00939.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruner SD, Norman DP, Verdine GL. Structural basis for recognition and repair of the endogenous mutagen 8-oxoguanine in DNA. Nature. 2000;403:859–866. doi: 10.1038/35002510. [DOI] [PubMed] [Google Scholar]
- Cabelof DC, Raffoul JJ, Yanamadala S, Ganir C, Guo Z, Heydari AR. Attenuation of DNA polymerase beta-dependent base excision repair and increased DMS-induced mutagenicity in aged mice. Mutat Res. 2002;500:135–145. doi: 10.1016/s0027-5107(02)00003-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Canugovi C, Yoon JS, Feldman NH, Croteau DL, Mattson MP, Bohr VA. Endonuclease VIII-like 1 (NEIL1) promotes short-term spatial memory retention and protects from ischemic stroke-induced brain dysfunction and death in mice. Proc Natl Acad Sci U S A. 2012;109:14948–14953. doi: 10.1073/pnas.1204156109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Catala A. Lipid peroxidation of membrane phospholipids in the vertebrate retina. Front Biosci (Schol Ed) 2011;3:52–60. doi: 10.2741/s131. [DOI] [PubMed] [Google Scholar]
- Catala A. Lipid peroxidation modifies the picture of membranes from the "Fluid Mosaic Model" to the "Lipid Whisker Model". Biochimie. 2012;94:101–109. doi: 10.1016/j.biochi.2011.09.025. [DOI] [PubMed] [Google Scholar]
- Chatoo W, Abdouh M, Bernier G. p53 pro-oxidant activity in the central nervous system: implication in aging and neurodegenerative diseases. Antioxid Redox Signal. 2011;15:1729–1737. doi: 10.1089/ars.2010.3610. [DOI] [PubMed] [Google Scholar]
- Chen D, Cao G, Hastings T, Feng Y, Pei W, O'Horo C, Chen J. Age-dependent decline of DNA repair activity for oxidative lesions in rat brain mitochondria. J Neurochem. 2002;81:1273–1284. doi: 10.1046/j.1471-4159.2002.00916.x. [DOI] [PubMed] [Google Scholar]
- Chen J, Jin K, Chen M, Pei W, Kawaguchi K, Greenberg DA, Simon RP. Early detection of DNA strand breaks in the brain after transient focal ischemia: implications for the role of DNA damage in apoptosis and neuronal cell death. J Neurochem. 1997;69:232–245. doi: 10.1046/j.1471-4159.1997.69010232.x. [DOI] [PubMed] [Google Scholar]
- Chin L, Artandi SE, Shen Q, Tam A, Lee SL, Gottlieb GJ, Greider CW, DePinho RA. p53 deficiency rescues the adverse effects of telomere loss and cooperates with telomere dysfunction to accelerate carcinogenesis. Cell. 1999;97:527–538. doi: 10.1016/s0092-8674(00)80762-x. [DOI] [PubMed] [Google Scholar]
- Clark RSB, Chen M, Kochanek PM, Watkins SC, Jin KL, Draviam R, Nathaniel PD, Pinto R, Marion DW, Graham SH. Detection of single- and double-strand DNA breaks after traumatic brain injury in rats: comparison of in situ labeling techniques using DNA polymerase I, the Klenow fragment of DNA polymerase I, and terminal deoxynucleotidyl transferase. J Neurotrauma. 2001;18:675–689. doi: 10.1089/089771501750357627. [DOI] [PubMed] [Google Scholar]
- Cleaver JE, Lam ET, Revet I. Disorders of nucleotide excision repair: the genetic and molecular basis of heterogeneity. Nat Rev Genet. 2009;10:756–768. doi: 10.1038/nrg2663. [DOI] [PubMed] [Google Scholar]
- Cooke MS, Evans MD, Dizdaroglu M, Lunec J. Oxidative DNA damage: mechanisms, mutation, and disease. FASEB J. 2003;17:1195–1214. doi: 10.1096/fj.02-0752rev. [DOI] [PubMed] [Google Scholar]
- Culmsee C, Bondada S, Mattson MP. Hippocampal neurons of mice deficient in DNA-dependent protein kinase exhibit increased vulnerability to DNA damage, oxidative stress and excitotoxicity. Brain Res Mol Brain Res. 2001;87:257–262. doi: 10.1016/s0169-328x(01)00008-0. [DOI] [PubMed] [Google Scholar]
- Culmsee C, Mattson MP. p53 in neuronal apoptosis. Biochem Biophys Res Commun. 2005;331:761–777. doi: 10.1016/j.bbrc.2005.03.149. [DOI] [PubMed] [Google Scholar]
- Culmsee C, Zhu C, Landshamer S, Becattini B, Wagner E, Pellecchia M, Blomgren K, Plesnila N. Apoptosis-inducing factor triggered by poly(ADP-ribose) polymerase and Bid mediates neuronal cell death after oxygen-glucose deprivation and focal cerebral ischemia. J Neurosci. 2005;25:10262–10272. doi: 10.1523/JNEUROSCI.2818-05.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dagci T, Armagan G, Konyalioglu S, Yalcin A. Alterations in the expression of the apurinic/apyrimidinic endonuclease-1/redox factor-1 (APE/ref-1) and DNA damage in the caudal region of acute and chronic spinal cord injured rats treated by embryonic neural stem cells. Physiol Res. 2009;58:427–434. doi: 10.33549/physiolres.931388. [DOI] [PubMed] [Google Scholar]
- Dedon PC. The chemical toxicology of 2-deoxyribose oxidation in DNA. Chem Res Toxicol. 2008;21:206–219. doi: 10.1021/tx700283c. [DOI] [PubMed] [Google Scholar]
- Demple B, DeMott MS. Dynamics and diversions in base excision DNA repair of oxidized abasic lesions. Oncogene. 2002;21:8926–8934. doi: 10.1038/sj.onc.1206178. [DOI] [PubMed] [Google Scholar]
- Denchi EL, de Lange T. Protection of telomeres through independent control of ATM and ATR by TRF2 and POT1. Nature. 2007;448:1068–1071. doi: 10.1038/nature06065. [DOI] [PubMed] [Google Scholar]
- Ditch S, Paull TT. The ATM protein kinase and cellular redox signaling: beyond the DNA damage response. Trends Biochem Sci. 2012;37:15–22. doi: 10.1016/j.tibs.2011.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dizdaroglu M, Jaruga P. Mechanisms of free radical-induced damage to DNA. Free Radic Res. 2012;46:382–419. doi: 10.3109/10715762.2011.653969. [DOI] [PubMed] [Google Scholar]
- Duffy S, So A, Murphy TH. Activation of endogenous antioxidant defenses in neuronal cells prevents free radical-mediated damage. J Neurochem. 1998;71:69–77. doi: 10.1046/j.1471-4159.1998.71010069.x. [DOI] [PubMed] [Google Scholar]
- Eitan E, Tichon A, Daniel G, Priel E. Telomerase expression in adult and old mouse Purkinje neurons. Rejuvenation Res. 2012a;15:206–209. doi: 10.1089/rej.2011.1285. [DOI] [PubMed] [Google Scholar]
- Eitan E, Tichon A, Gazit A, Gitler D, Slavin S, Priel E. Novel telomerase-increasing compound in mouse brain delays the onset of amyotrophic lateral sclerosis. EMBO Mol Med. 2012b;4:313–329. doi: 10.1002/emmm.201200212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Endres M, Wang ZQ, Namura S, Waeber C, Moskowitz MA. Ischemic brain injury is mediated by the activation of poly(ADP-ribose)polymerase. J Cereb Blood Flow Metab. 1997;17:1143–1151. doi: 10.1097/00004647-199711000-00002. [DOI] [PubMed] [Google Scholar]
- Fei J, Kaczmarek N, Luch A, Glas A, Carell T, Naegeli H. Regulation of nucleotide excision repair by UV-DDB: prioritization of damage recognition to internucleosomal DNA. PLoS Biol. 2011;9:e1001183. doi: 10.1371/journal.pbio.1001183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feng S, Yang Q, Liu M, Li W, Yuan W, Zhang S, Wu B, Li J. Edaravone for acute ischaemic stroke. Cochrane Database Syst Rev. 2011 doi: 10.1002/14651858.CD007230.pub2. CD007230. [DOI] [PubMed] [Google Scholar]
- Fishel ML, Vasko MR, Kelley MR. DNA repair in neurons: so if they don't divide what's to repair? Mutat Res. 2007;614:24–36. doi: 10.1016/j.mrfmmm.2006.06.007. [DOI] [PubMed] [Google Scholar]
- Fortini P, Dogliotti E. Base damage and single-strand break repair: mechanisms and functional significance of short- and long-patch repair subpathways. DNA Repair (Amst) 2007;6:398–409. doi: 10.1016/j.dnarep.2006.10.008. [DOI] [PubMed] [Google Scholar]
- Francisconi S, Codenotti M, Ferrari-Toninelli G, Uberti D, Memo M. Preservation of DNA integrity and neuronal degeneration. Brain Res Brain Res Rev. 2005;48:347–351. doi: 10.1016/j.brainresrev.2004.12.023. [DOI] [PubMed] [Google Scholar]
- Fu W, Begley JG, Killen MW, Mattson MP. Anti-apoptotic role of telomerase in pheochromocytoma cells. J Biol Chem. 1999;274:7264–7271. doi: 10.1074/jbc.274.11.7264. [DOI] [PubMed] [Google Scholar]
- Giraud-Panis MJ, Pisano S, Poulet A, Le Du MH, Gilson E. Structural identity of telomeric complexes. FEBS Lett. 2010;584:3785–3799. doi: 10.1016/j.febslet.2010.08.004. [DOI] [PubMed] [Google Scholar]
- Goto S, Xue R, Sugo N, Sawada M, Blizzard KK, Poitras MF, Johns DC, Dawson TM, Dawson VL, Crain BJ, Traystman RJ, Mori S, Hurn PD. Poly(ADP-ribose) polymerase impairs early and long-term experimental stroke recovery. Stroke. 2002;33:1101–1106. doi: 10.1161/01.str.0000014203.65693.1e. [DOI] [PubMed] [Google Scholar]
- Gredilla R, Garm C, Holm R, Bohr VA, Stevnsner T. Differential age-related changes in mitochondrial DNA repair activities in mouse brain regions. Neurobiol Aging. 2010;31:993–1002. doi: 10.1016/j.neurobiolaging.2008.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gredilla R, Weissman L, Yang JL, Bohr VA, Stevnsner T. Mitochondrial base excision repair in mouse synaptosomes during normal aging and in a model of Alzheimer's disease. Neurobiol Aging. 2012;33:694–707. doi: 10.1016/j.neurobiolaging.2010.06.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gris D, Marsh DR, Oatway MA, Chen Y, Hamilton EF, Dekaban GA, Weaver LC. Transient blockade of the CD11d/CD18 integrin reduces secondary damage after spinal cord injury, improving sensory, autonomic, and motor function. J Neurosci. 2004;24:4043–4051. doi: 10.1523/JNEUROSCI.5343-03.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ha HC, Snyder SH. Poly(ADP-ribose) polymerase is a mediator of necrotic cell death by ATP depletion. Proc Natl Acad Sci U S A. 1999;96:13978–13982. doi: 10.1073/pnas.96.24.13978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall ED. Antioxidant therapies for acute spinal cord injury. Neurotherapeutics. 2011;8:152–167. doi: 10.1007/s13311-011-0026-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall ED, Detloff MR, Johnson K, Kupina NC. Peroxynitrite-mediated protein nitration and lipid peroxidation in a mouse model of traumatic brain injury. J Neurotrauma. 2004;21:9–20. doi: 10.1089/089771504772695904. [DOI] [PubMed] [Google Scholar]
- Hall ED, Vaishnav RA, Mustafa AG. Antioxidant therapies for traumatic brain injury. Neurotherapeutics. 2010;7:51–61. doi: 10.1016/j.nurt.2009.10.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamann K, Durkes A, Ouyang H, Uchida K, Pond A, Shi R. Critical role of acrolein in secondary injury following ex vivo spinal cord trauma. J Neurochem. 2008;107:712–721. doi: 10.1111/j.1471-4159.2008.05622.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hazra TK, Hill JW, Izumi T, Mitra S. Multiple DNA glycosylases for repair of 8-oxoguanine and their potential in vivo functions. Prog Nucleic Acid Res Mol Biol. 2001;68:193–205. doi: 10.1016/s0079-6603(01)68100-5. [DOI] [PubMed] [Google Scholar]
- Hefferin ML, Tomkinson AE. Mechanism of DNA double-strand break repair by non-homologous end joining. DNA Repair (Amst) 2005;4:639–648. doi: 10.1016/j.dnarep.2004.12.005. [DOI] [PubMed] [Google Scholar]
- Hegde ML, Hazra TK, Mitra S. Early steps in the DNA base excision/single-strand interruption repair pathway in mammalian cells. Cell Res. 2008;18:27–47. doi: 10.1038/cr.2008.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hewitt G, Jurk D, Marques FD, Correia-Melo C, Hardy T, Gackowska A, Anderson R, Taschuk M, Mann J, Passos JF. Telomeres are favoured targets of a persistent DNA damage response in ageing and stress-induced senescence. Nat Commun. 2012;3:708. doi: 10.1038/ncomms1708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hockemeyer D, Sfeir AJ, Shay JW, Wright WE, de Lange T. POT1 protects telomeres from a transient DNA damage response and determines how human chromosomes end. EMBO J. 2005;24:2667–2678. doi: 10.1038/sj.emboj.7600733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horikawa I, Fujita K, Harris CC. p53 governs telomere regulation feedback too, via TRF2. Aging (Albany NY) 2011;3:26–32. doi: 10.18632/aging.100271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu BR, Martone ME, Jones YZ, Liu CL. Protein aggregation after transient cerebral ischemia. J Neurosci. 2000;20:3191–3199. doi: 10.1523/JNEUROSCI.20-09-03191.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang WL, King VR, Curran OE, Dyall SC, Ward RE, Lal N, Priestley JV, Michael-Titus AT. A combination of intravenous and dietary docosahexaenoic acid significantly improves outcome after spinal cord injury. Brain. 2007;130:3004–3019. doi: 10.1093/brain/awm223. [DOI] [PubMed] [Google Scholar]
- Imam SZ, Karahalil B, Hogue BA, Souza-Pinto NC, Bohr VA. Mitochondrial and nuclear DNA-repair capacity of various brain regions in mouse is altered in an age-dependent manner. Neurobiol Aging. 2006;27:1129–1136. doi: 10.1016/j.neurobiolaging.2005.06.002. [DOI] [PubMed] [Google Scholar]
- Inci S, Ozcan OE, Kilinc K. Time-level relationship for lipid peroxidation and the protective effect of alpha-tocopherol in experimental mild and severe brain injury. Neurosurgery. 1998;43:330–335. doi: 10.1097/00006123-199808000-00095. discussion 335–336. [DOI] [PubMed] [Google Scholar]
- Itoh T, Satou T, Nishida S, Tsubaki M, Imano M, Hashimoto S, Ito H. Edaravone protects against apoptotic neuronal cell death and improves cerebral function after traumatic brain injury in rats. Neurochem Res. 2010;35:348–355. doi: 10.1007/s11064-009-0061-2. [DOI] [PubMed] [Google Scholar]
- Jaarsma D, van der Pluijm I, de Waard MC, Haasdijk ED, Brandt R, Vermeij M, Rijksen Y, Maas A, van Steeg H, Hoeijmakers JH, van der Horst GT. Age-related neuronal degeneration: complementary roles of nucleotide excision repair and transcription-coupled repair in preventing neuropathology. PLoS Genet. 2011;7:e1002405. doi: 10.1371/journal.pgen.1002405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaskelioff M, Muller FL, Paik JH, Thomas E, Jiang S, Adams AC, Sahin E, Kost-Alimova M, Protopopov A, Cadinanos J, Horner JW, Maratos-Flier E, Depinho RA. Telomerase reactivation reverses tissue degeneration in aged telomerase-deficient mice. Nature. 2011;469:102–106. doi: 10.1038/nature09603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeppesen DK, Bohr VA, Stevnsner T. DNA repair deficiency in neurodegeneration. Prog Neurobiol. 2011;94:166–200. doi: 10.1016/j.pneurobio.2011.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jia Z, Zhu H, Li J, Wang X, Misra H, Li Y. Oxidative stress in spinal cord injury and antioxidant-based intervention. Spinal Cord. 2012;50:264–274. doi: 10.1038/sc.2011.111. [DOI] [PubMed] [Google Scholar]
- Jia Z, Zhu H, Vitto MJ, Misra BR, Li Y, Misra HP. Alpha-lipoic acid potently inhibits peroxynitrite-mediated DNA strand breakage and hydroxyl radical formation: implications for the neuroprotective effects of alpha-lipoic acid. Mol Cell Biochem. 2009;323:131–138. doi: 10.1007/s11010-008-9971-6. [DOI] [PubMed] [Google Scholar]
- Jin Y, McEwen ML, Nottingham SA, Maragos WF, Dragicevic NB, Sullivan PG, Springer JE. The mitochondrial uncoupling agent 2,4-dinitrophenol improves mitochondrial function, attenuates oxidative damage, and increases white matter sparing in the contused spinal cord. J Neurotrauma. 2004;21:1396–1404. doi: 10.1089/neu.2004.21.1396. [DOI] [PubMed] [Google Scholar]
- Kang HJ, Choi YS, Hong SB, Kim KW, Woo RS, Won SJ, Kim EJ, Jeon HK, Jo SY, Kim TK, Bachoo R, Reynolds IJ, Gwag BJ, Lee HW. Ectopic expression of the catalytic subunit of telomerase protects against brain injury resulting from ischemia and NMDA-induced neurotoxicity. J Neurosci. 2004;24:1280–1287. doi: 10.1523/JNEUROSCI.4082-03.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karlseder J, Hoke K, Mirzoeva OK, Bakkenist C, Kastan MB, Petrini JH, de Lange T. The telomeric protein TRF2 binds the ATM kinase and can inhibit the ATM-dependent DNA damage response. PLoS Biol. 2004;2:E240. doi: 10.1371/journal.pbio.0020240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kassubek J, Sperfeld AD, Pinkhardt EH, Unrath A, Muller HP, Scharffetter-Kochanek K, Ludolph AC, Berneburg M. The cerebro-morphological fingerprint of a progeroid syndrome: white matter changes correlate with neurological symptoms in xeroderma pigmentosum. PLoS One. 2012;7:e30926. doi: 10.1371/journal.pone.0030926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kotipatruni RR, Dasari VR, Veeravalli KK, Dinh DH, Fassett D, Rao JS. p53- and Bax-mediated apoptosis in injured rat spinal cord. Neurochem Res. 2011;36:2063–2074. doi: 10.1007/s11064-011-0530-2. [DOI] [PubMed] [Google Scholar]
- Kraemer KH, Patronas NJ, Schiffmann R, Brooks BP, Tamura D, DiGiovanna JJ. Xeroderma pigmentosum, trichothiodystrophy and Cockayne syndrome: a complex genotype-phenotype relationship. Neuroscience. 2007;145:1388–1396. doi: 10.1016/j.neuroscience.2006.12.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kruman II. Why do neurons enter the cell cycle? Cell Cycle. 2004;3:769–773. [PubMed] [Google Scholar]
- Lee J, Jo YS, Sung YH, Hwang IK, Kim H, Kim SY, Yi SS, Choi JS, Sun W, Seong JK, Lee HW. Telomerase deficiency affects normal brain functions in mice. Neurochem Res. 2010;35:211–218. doi: 10.1007/s11064-009-0044-3. [DOI] [PubMed] [Google Scholar]
- Lee Y, McKinnon PJ. Responding to DNA double strand breaks in the nervous system. Neuroscience. 2007;145:1365–1374. doi: 10.1016/j.neuroscience.2006.07.026. [DOI] [PubMed] [Google Scholar]
- Leker RR, Aharonowiz M, Greig NH, Ovadia H. The role of p53-induced apoptosis in cerebral ischemia: effects of the p53 inhibitor pifithrin alpha. Exp Neurol. 2004;187:478–486. doi: 10.1016/j.expneurol.2004.01.030. [DOI] [PubMed] [Google Scholar]
- Lewen A, Sugawara T, Gasche Y, Fujimura M, Chan PH. Oxidative cellular damage and the reduction of APE/Ref-1 expression after experimental traumatic brain injury. Neurobiol Dis. 2001;8:380–390. doi: 10.1006/nbdi.2001.0396. [DOI] [PubMed] [Google Scholar]
- Li J, Tang B, Qu Y, Mu D. Telomerase reverse transcriptase: a novel neuroprotective mechanism involved in neonatal hypoxic-ischemic brain injury. Int J Dev Neurosci. 2011;29:867–872. doi: 10.1016/j.ijdevneu.2011.07.010. [DOI] [PubMed] [Google Scholar]
- Lin R, Roseborough G, Dong Y, Williams GM, Wei C. DNA damage and repair system in spinal cord ischemia. J Vasc Surg. 2003;37:847–858. doi: 10.1067/mva.2003.150. [DOI] [PubMed] [Google Scholar]
- Lin Y, Vreman HJ, Wong RJ, Tjoa T, Yamauchi T, Noble-Haeusslein LJ. Heme oxygenase-1 stabilizes the blood-spinal cord barrier and limits oxidative stress and white matter damage in the acutely injured murine spinal cord. J Cereb Blood Flow Metab. 2007;27:1010–1021. doi: 10.1038/sj.jcbfm.9600412. [DOI] [PubMed] [Google Scholar]
- Liu D, Croteau DL, Souza-Pinto N, Pitta M, Tian J, Wu C, Jiang H, Mustafa K, Keijzers G, Bohr VA, Mattson MP. Evidence that OGG1 glycosylase protects neurons against oxidative DNA damage and cell death under ischemic conditions. J Cereb Blood Flow Metab. 2011;31:680–692. doi: 10.1038/jcbfm.2010.147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lovell MA, Xie C, Markesbery WR. Decreased base excision repair and increased helicase activity in Alzheimer's disease brain. Brain Res. 2000;855:116–123. doi: 10.1016/s0006-8993(99)02335-5. [DOI] [PubMed] [Google Scholar]
- Lu C, Fu W, Mattson MP. Telomerase protects developing neurons against DNA damage-induced cell death. Brain Res Dev Brain Res. 2001;131:167–171. doi: 10.1016/s0165-3806(01)00237-1. [DOI] [PubMed] [Google Scholar]
- Lukic-Panin V, Deguchi K, Yamashita T, Shang J, Zhang X, Tian F, Liu N, Kawai H, Matsuura T, Abe K. Free radical scavenger edaravone administration protects against tissue plasminogen activator induced oxidative stress and blood brain barrier damage. Curr Neurovasc Res. 2010;7:319–329. doi: 10.2174/156720210793180747. [DOI] [PubMed] [Google Scholar]
- Marietta C, Palombo F, Gallinari P, Jiricny J, Brooks PJ. Expression of long-patch and short-patch DNA mismatch repair proteins in the embryonic and adult mammalian brain. Brain Res Mol Brain Res. 1998;53:317–320. doi: 10.1016/s0169-328x(97)00311-2. [DOI] [PubMed] [Google Scholar]
- Marinoglou K. The role of the DNA damage response kinase ataxia telangiectasia mutated in neuroprotection. Yale J Biol Med. 2012;85:469–480. [PMC free article] [PubMed] [Google Scholar]
- Martin LJ, Liu Z. Injury-induced spinal motor neuron apoptosis is preceded by DNA single-strand breaks and is p53- and Bax-dependent. J Neurobiol. 2002;50:181–197. doi: 10.1002/neu.10026. [DOI] [PubMed] [Google Scholar]
- McMurray CT. To die or not to die: DNA repair in neurons. Mutat Res. 2005;577:260–274. doi: 10.1016/j.mrfmmm.2005.03.006. [DOI] [PubMed] [Google Scholar]
- Medalha CC, Polesel FS, da Silva VH, Martins RA, Pozzi R, Ribeiro DA. Acute spinal cord injury induces genetic damage in multiple organs of rats. Cell Mol Neurobiol. 2012;32:949–952. doi: 10.1007/s10571-012-9825-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melis JP, van Steeg H, Luijten M. Oxidative DNA Damage and Nucleotide Excision Repair. Antioxid Redox Signal. 2012 doi: 10.1089/ars.2012.5036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moubarak RS, Yuste VJ, Artus C, Bouharrour A, Greer PA, Menissier-de Murcia J, Susin SA. Sequential activation of poly(ADP-ribose) polymerase 1, calpains, and Bax is essential in apoptosis-inducing factor-mediated programmed necrosis. Mol Cell Biol. 2007;27:4844–4862. doi: 10.1128/MCB.02141-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakamura J, Swenberg JA. Endogenous apurinic/apyrimidinic sites in genomic DNA of mammalian tissues. Cancer Res. 1999;59:2522–2526. [PubMed] [Google Scholar]
- Nelson ND, Bertuch AA. Dyskeratosis congenita as a disorder of telomere maintenance. Mutat Res. 2012;730:43–51. doi: 10.1016/j.mrfmmm.2011.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nijboer CH, Heijnen CJ, van der Kooij MA, Zijlstra J, van Velthoven CT, Culmsee C, van Bel F, Hagberg H, Kavelaars A. Targeting the p53 pathway to protect the neonatal ischemic brain. Ann Neurol. 2011;70:255–264. doi: 10.1002/ana.22413. [DOI] [PubMed] [Google Scholar]
- Nito C, Ueda M, Inaba T, Katsura K, Katayama Y. FK506 ameliorates oxidative damage and protects rat brain following transient focal cerebral ischemia. Neurol Res. 2011;33:881–889. doi: 10.1179/1743132811Y.0000000019. [DOI] [PubMed] [Google Scholar]
- Niu C, Yip HK. Neuroprotective signaling mechanisms of telomerase are regulated by brain-derived neurotrophic factor in rat spinal cord motor neurons. J Neuropathol Exp Neurol. 2011;70:634–652. doi: 10.1097/NEN.0b013e318222b97b. [DOI] [PubMed] [Google Scholar]
- Nouspikel T, Hanawalt PC. DNA repair in terminally differentiated cells. DNA Repair (Amst) 2002;1:59–75. doi: 10.1016/s1568-7864(01)00005-2. [DOI] [PubMed] [Google Scholar]
- Otterlei M, Kavli B, Standal R, Skjelbred C, Bharati S, Krokan HE. Repair of chromosomal abasic sites in vivo involves at least three different repair pathways. EMBO J. 2000;19:5542–5551. doi: 10.1093/emboj/19.20.5542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plesnila N, von Baumgarten L, Retiounskaia M, Engel D, Ardeshiri A, Zimmermann R, Hoffmann F, Landshamer S, Wagner E, Culmsee C. Delayed neuronal death after brain trauma involves p53-dependent inhibition of NF-kappaB transcriptional activity. Cell Death Differ. 2007;14:1529–1541. doi: 10.1038/sj.cdd.4402159. [DOI] [PubMed] [Google Scholar]
- Pommier Y, Redon C, Rao VA, Seiler JA, Sordet O, Takemura H, Antony S, Meng L, Liao Z, Kohlhagen G, Zhang H, Kohn KW. Repair of and checkpoint response to topoisomerase I-mediated DNA damage. Mutat Res. 2003;532:173–203. doi: 10.1016/j.mrfmmm.2003.08.016. [DOI] [PubMed] [Google Scholar]
- Qu Y, Duan Z, Zhao F, Wei D, Zhang J, Tang B, Li J, Yang C, Mu D. Telomerase reverse transcriptase upregulation attenuates astrocyte proliferation and promotes neuronal survival in the hypoxic-ischemic rat brain. Stroke. 2011;42:3542–3550. doi: 10.1161/STROKEAHA.111.626325. [DOI] [PubMed] [Google Scholar]
- Radak Z, Zhao Z, Goto S, Koltai E. Age-associated neurodegeneration and oxidative damage to lipids, proteins and DNA. Mol Aspects Med. 2011;32:305–315. doi: 10.1016/j.mam.2011.10.010. [DOI] [PubMed] [Google Scholar]
- Rajdev S, Hara K, Kokubo Y, Mestril R, Dillmann W, Weinstein PR, Sharp FR. Mice overexpressing rat heat shock protein 70 are protected against cerebral infarction. Ann Neurol. 2000;47:782–791. [PubMed] [Google Scholar]
- Rapin I, Lindenbaum Y, Dickson DW, Kraemer KH, Robbins JH. Cockayne syndrome and xeroderma pigmentosum. Neurology. 2000;55:1442–1449. doi: 10.1212/wnl.55.10.1442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhee DB, Ghosh A, Lu J, Bohr VA, Liu Y. Factors that influence telomeric oxidative base damage and repair by DNA glycosylase OGG1. DNA Repair (Amst) 2011;10:34–44. doi: 10.1016/j.dnarep.2010.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robu M, Shah RG, Petitclerc N, Brind'amour J, Kandan-Kulangara F, Shah GM. Role of poly(ADP-ribose) polymerase-1 in the removal of UV-induced DNA lesions by nucleotide excision repair. Proc Natl Acad Sci U S A. 2013;110:1658–1663. doi: 10.1073/pnas.1209507110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roof RL, Hoffman SW, Stein DG. Progesterone protects against lipid peroxidation following traumatic brain injury in rats. Mol Chem Neuropathol. 1997;31:1–11. doi: 10.1007/BF02815156. [DOI] [PubMed] [Google Scholar]
- Samantaray S, Smith JA, Das A, Matzelle DD, Varma AK, Ray SK, Banik NL. Low dose estrogen prevents neuronal degeneration and microglial reactivity in an acute model of spinal cord injury: effect of dosing, route of administration, and therapy delay. Neurochem Res. 2011;36:1809–1816. doi: 10.1007/s11064-011-0498-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Samantaray S, Sribnick EA, Das A, Knaryan VH, Matzelle DD, Yallapragada AV, Reiter RJ, Ray SK, Banik NL. Melatonin attenuates calpain upregulation, axonal damage and neuronal death in spinal cord injury in rats. J Pineal Res. 2008;44:348–357. doi: 10.1111/j.1600-079X.2007.00534.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santos JH, Meyer JN, Van Houten B. Mitochondrial localization of telomerase as a determinant for hydrogen peroxide-induced mitochondrial DNA damage and apoptosis. Hum Mol Genet. 2006;15:1757–1768. doi: 10.1093/hmg/ddl098. [DOI] [PubMed] [Google Scholar]
- Sedarous M, Keramaris E, O'Hare M, Melloni E, Slack RS, Elce JS, Greer PA, Park DS. Calpains mediate p53 activation and neuronal death evoked by DNA damage. J Biol Chem. 2003;278:26031–26038. doi: 10.1074/jbc.M302833200. [DOI] [PubMed] [Google Scholar]
- Sekiguchi JM, Gao Y, Gu Y, Frank K, Sun Y, Chaudhuri J, Zhu C, Cheng HL, Manis J, Ferguson D, Davidson L, Greenberg ME, Alt FW. Nonhomologous end-joining proteins are required for V(D)J recombination, normal growth, and neurogenesis. Cold Spring Harb Symp Quant Biol. 1999;64:169–181. doi: 10.1101/sqb.1999.64.169. [DOI] [PubMed] [Google Scholar]
- Seligman ML, Flamm ES, Goldstein BD, Poser RG, Demopoulos HB, Ransohoff J. Spectrofluorescent detection of malonaldehyde as a measure of lipid free radical damage in response to ethanol potentiation of spinal cord trauma. Lipids. 1977;12:945–950. doi: 10.1007/BF02533316. [DOI] [PubMed] [Google Scholar]
- Shackelford DA, Tobaru T, Zhang S, Zivin JA. Changes in expression of the DNA repair protein complex DNA-dependent protein kinase after ischemia and reperfusion. J Neurosci. 1999;19:4727–4738. doi: 10.1523/JNEUROSCI.19-12-04727.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smerjac SM, Bizzozero OA. Cytoskeletal protein carbonylation and degradation in experimental autoimmune encephalomyelitis. J Neurochem. 2008;105:763–772. doi: 10.1111/j.1471-4159.2007.05178.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sribnick EA, Matzelle DD, Banik NL, Ray SK. Direct evidence for calpain involvement in apoptotic death of neurons in spinal cord injury in rats and neuroprotection with calpain inhibitor. Neurochem Res. 2007;32:2210–2216. doi: 10.1007/s11064-007-9433-7. [DOI] [PubMed] [Google Scholar]
- Sribnick EA, Matzelle DD, Ray SK, Banik NL. Estrogen treatment of spinal cord injury attenuates calpain activation and apoptosis. J Neurosci Res. 2006;84:1064–1075. doi: 10.1002/jnr.21016. [DOI] [PubMed] [Google Scholar]
- Sribnick EA, Samantaray S, Das A, Smith J, Matzelle DD, Ray SK, Banik NL. Postinjury estrogen treatment of chronic spinal cord injury improves locomotor function in rats. J Neurosci Res. 2010;88:1738–1750. doi: 10.1002/jnr.22337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suberviola B, Gonzalez-Castro A, Llorca J, Ortiz-Melon F, Minambres E. Early complications of high-dose methylprednisolone in acute spinal cord injury patients. Injury. 2008;39:748–752. doi: 10.1016/j.injury.2007.12.005. [DOI] [PubMed] [Google Scholar]
- Suemori S, Shimazawa M, Kawase K, Satoh M, Nagase H, Yamamoto T, Hara H. Metallothionein, an endogenous antioxidant, protects against retinal neuron damage in mice. Invest Ophthalmol Vis Sci. 2006;47:3975–3982. doi: 10.1167/iovs.06-0275. [DOI] [PubMed] [Google Scholar]
- Suganuma H, Arai Y, Kitamura Y, Hayashi M, Okumura A, Shimizu T. Maternal docosahexaenoic acid-enriched diet prevents neonatal brain injury. Neuropathology. 2010;30:597–605. doi: 10.1111/j.1440-1789.2010.01114.x. [DOI] [PubMed] [Google Scholar]
- Sugawara T, Noshita N, Lewen A, Kim GW, Chan PH. Neuronal expression of the DNA repair protein Ku 70 after ischemic preconditioning corresponds to tolerance to global cerebral ischemia. Stroke. 2001;32:2388–2393. doi: 10.1161/hs1001.097109. [DOI] [PubMed] [Google Scholar]
- Swain U, Rao KS. Age-dependent decline of DNA base excision repair activity in rat cortical neurons. Mech Ageing Dev. 2012;133:186–194. doi: 10.1016/j.mad.2012.01.001. [DOI] [PubMed] [Google Scholar]
- Takahashi G, Sakurai M, Abe K, Itoyama Y, Tabayashi K. MCI-186 reduces oxidative cellular damage and increases DNA repair function in the rabbit spinal cord after transient ischemia. Ann Thorac Surg. 2004;78:602–607. doi: 10.1016/j.athoracsur.2004.02.133. [DOI] [PubMed] [Google Scholar]
- Tedeschi A, Di Giovanni S. The non-apoptotic role of p53 in neuronal biology: enlightening the dark side of the moon. EMBO Rep. 2009;10:576–583. doi: 10.1038/embor.2009.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas P, NJ OC, Fenech M. Telomere length in white blood cells, buccal cells and brain tissue and its variation with ageing and Alzheimer's disease. Mech Ageing Dev. 2008;129:183–190. doi: 10.1016/j.mad.2007.12.004. [DOI] [PubMed] [Google Scholar]
- Tomasevic G, Laurer HL, Mattiasson G, van Steeg H, Wieloch T, McIntosh TK. Delayed neuromotor recovery and increased memory acquisition dysfunction following experimental brain trauma in mice lacking the DNA repair gene XPA. J Neurosurg. 2012;116:1368–1378. doi: 10.3171/2012.2.JNS11888. [DOI] [PubMed] [Google Scholar]
- Vaseva AV, Marchenko ND, Ji K, Tsirka SE, Holzmann S, Moll UM. p53 opens the mitochondrial permeability transition pore to trigger necrosis. Cell. 2012;149:1536–1548. doi: 10.1016/j.cell.2012.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vatassery GT. Vitamin E and other endogenous antioxidants in the central nervous system. Geriatrics. 1998;53(Suppl 1):S25–S27. [PubMed] [Google Scholar]
- Verhagen MM, Martin JJ, van Deuren M, Ceuterick-de Groote C, Weemaes CM, Kremer BH, Taylor MA, Willemsen MA, Lammens M. Neuropathology in classical and variant ataxia-telangiectasia. Neuropathology. 2012;32:234–244. doi: 10.1111/j.1440-1789.2011.01263.x. [DOI] [PubMed] [Google Scholar]
- Wang GH, Jiang ZL, Li YC, Li X, Shi H, Gao YQ, Vosler PS, Chen J. Free-radical scavenger edaravone treatment confers neuroprotection against traumatic brain injury in rats. J Neurotrauma. 2011a;28:2123–2134. doi: 10.1089/neu.2011.1939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang J, Xiong S, Xie C, Markesbery WR, Lovell MA. Increased oxidative damage in nuclear and mitochondrial DNA in Alzheimer's disease. J Neurochem. 2005;93:953–962. doi: 10.1111/j.1471-4159.2005.03053.x. [DOI] [PubMed] [Google Scholar]
- Wang Y, Dawson VL, Dawson TM. Poly(ADP-ribose) signals to mitochondrial AIF: a key event in parthanatos. Exp Neurol. 2009;218:193–202. doi: 10.1016/j.expneurol.2009.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y, Kim NS, Haince JF, Kang HC, David KK, Andrabi SA, Poirier GG, Dawson VL, Dawson TM. Poly(ADP-ribose) (PAR) binding to apoptosis-inducing factor is critical for PAR polymerase-1-dependent cell death (parthanatos) Sci Signal. 2011b;4:ra20. doi: 10.1126/scisignal.2000902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson DM, 3rd, Bohr VA. The mechanics of base excision repair, and its relationship to aging and disease. DNA Repair (Amst) 2007;6:544–559. doi: 10.1016/j.dnarep.2006.10.017. [DOI] [PubMed] [Google Scholar]
- Wilson DM, 3rd, McNeill DR. Base excision repair and the central nervous system. Neuroscience. 2007;145:1187–1200. doi: 10.1016/j.neuroscience.2006.07.011. [DOI] [PubMed] [Google Scholar]
- Wilson DM, 3rd, Sofinowski TM, McNeill DR. Repair mechanisms for oxidative DNA damage. Front Biosci. 2003;8:d963–d981. doi: 10.2741/1109. [DOI] [PubMed] [Google Scholar]
- Won SJ, Choi BY, Yoo BH, Sohn M, Ying W, Swanson RA, Suh SW. Prevention of traumatic brain injury-induced neuron death by intranasal delivery of nicotinamide adenine dinucleotide. J Neurotrauma. 2012;29:1401–1409. doi: 10.1089/neu.2011.2228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright DW, Kellermann AL, Hertzberg VS, Clark PL, Frankel M, Goldstein FC, Salomone JP, Dent LL, Harris OA, Ander DS, Lowery DW, Patel MM, Denson DD, Gordon AB, Wald MM, Gupta S, Hoffman SW, Stein DG. ProTECT: a randomized clinical trial of progesterone for acute traumatic brain injury. Ann Emerg Med. 2007;49:391–402. 402 e391–402 392. doi: 10.1016/j.annemergmed.2006.07.932. [DOI] [PubMed] [Google Scholar]
- Xiong Y, Rabchevsky AG, Hall ED. Role of peroxynitrite in secondary oxidative damage after spinal cord injury. J Neurochem. 2007;100:639–649. doi: 10.1111/j.1471-4159.2006.04312.x. [DOI] [PubMed] [Google Scholar]
- Yamada KH, Kozlowski DA, Seidl SE, Lance S, Wieschhaus AJ, Sundivakkam P, Tiruppathi C, Chishti I, Herman IM, Kuchay SM, Chishti AH. Targeted gene inactivation of calpain-1 suppresses cortical degeneration due to traumatic brain injury and neuronal apoptosis induced by oxidative stress. J Biol Chem. 2012;287:13182–13193. doi: 10.1074/jbc.M111.302612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yamaguchi A, Taniguchi M, Hori O, Ogawa S, Tojo N, Matsuoka N, Miyake S, Kasai K, Sugimoto H, Tamatani M, Yamashita T, Tohyama M. Peg3/Pw1 is involved in p53-mediated cell death pathway in brain ischemia/hypoxia. J Biol Chem. 2002;277:623–629. doi: 10.1074/jbc.M107435200. [DOI] [PubMed] [Google Scholar]
- Yermilov V, Rubio J, Ohshima H. Formation of 8-nitroguanine in DNA treated with peroxynitrite in vitro and its rapid removal from DNA by depurination. FEBS Lett. 1995;376:207–210. doi: 10.1016/0014-5793(95)01281-6. [DOI] [PubMed] [Google Scholar]
- Ying W, Wei G, Wang D, Wang Q, Tang X, Shi J, Zhang P, Lu H. Intranasal administration with NAD+ profoundly decreases brain injury in a rat model of transient focal ischemia. Front Biosci. 2007;12:2728–2734. doi: 10.2741/2267. [DOI] [PubMed] [Google Scholar]
- Yonekura I, Takai K, Asai A, Kawahara N, Kirino T. p53 potentiates hippocampal neuronal death caused by global ischemia. J Cereb Blood Flow Metab. 2006;26:1332–1340. doi: 10.1038/sj.jcbfm.9600293. [DOI] [PubMed] [Google Scholar]
- Yune TY, Kim SJ, Lee SM, Lee YK, Oh YJ, Kim YC, Markelonis GJ, Oh TH. Systemic administration of 17beta-estradiol reduces apoptotic cell death and improves functional recovery following traumatic spinal cord injury in rats. J Neurotrauma. 2004;21:293–306. doi: 10.1089/089771504322972086. [DOI] [PubMed] [Google Scholar]
- Zhang P, Chan SL, Fu W, Mendoza M, Mattson MP. TERT suppresses apoptotis at a premitochondrial step by a mechanism requiring reverse transcriptase activity and 14-3-3 protein-binding ability. FASEB J. 2003;17:767–769. doi: 10.1096/fj.02-0603fje. [DOI] [PubMed] [Google Scholar]
- Zhao L, Xu X, Zhu J, Chen J. Immunohistochemical research on brain stem injury: expression of heat shock protein 70 in rat brain after traumatic brain stem injury. Fa Yi Xue Za Zhi. 1998;14:135–137. 190. [PubMed] [Google Scholar]
- Zhu H, Fu W, Mattson MP. The catalytic subunit of telomerase protects neurons against amyloid beta-peptide-induced apoptosis. J Neurochem. 2000;75:117–124. doi: 10.1046/j.1471-4159.2000.0750117.x. [DOI] [PubMed] [Google Scholar]