Abstract
A high proportion of people with severe mental health problems are unemployed but would like to work. Individual Placement and Support (IPS) offers a promising approach to establishing people in paid employment. In a randomized controlled trial across six European countries, we investigated the economic case for IPS for people with severe mental health problems compared to standard vocational rehabilitation. Individuals (n=312) were randomized to receive either IPS or standard vocational services and followed for 18 months. Service use and outcome data were collected. Cost-effectiveness analysis was conducted with two primary outcomes: additional days worked in competitive settings and additional percentage of individuals who worked at least 1 day. Analyses distinguished country effects. A partial cost-benefit analysis was also conducted. IPS produced better outcomes than alternative vocational services at lower cost overall to the health and social care systems. This pattern also held in disaggregated analyses for five of the six European sites. The inclusion of imputed values for missing cost data supported these findings. IPS would be viewed as more cost-effective than standard vocational services. Further analysis demonstrated cost-benefit arguments for IPS. Compared to standard vocational rehabilitation services, IPS is, therefore, probably cost-saving and almost certainly more cost-effective as a way to help people with severe mental health problems into competitive employment.
Keywords: Supported employment, cost-effectiveness, severe mental illness, economics, work
People with severe mental illness face many challenges in securing paid work, and employment rates are low 1. Not surprisingly, many public and other bodies emphasize the need to target help on these individuals 2,3. As macroeconomic pressures mount and public budgets face substantial cuts, it becomes all the more pressing to know whether such help is cost-effective (do the outcomes justify the costs?) and to gauge its budget impact (what is the impact on overall expenditure?).
Individual Placement and Support (IPS) has emerged as an effective way to help many people with severe mental illness obtain competitive employment 4,5 and could potentially contribute to social and economic inclusion. A multisite randomized trial of IPS, conducted in six European cities (the EQOLISE study), was the first to examine directly the hypothesis that IPS would prove more effective than comparison services in Europe 6.
As in the United States 4, Canada 7, Australia 8, and Hong Kong 9, the study found that IPS participants were much more likely to work in competitive settings and worked more hours than individuals receiving comparison services. Recently, Bond et al 10 argued that the positive findings in support of IPS in the United States “may transport well into new settings as long as programs achieve high fidelity to the IPS model”. However, what are the economic consequences? In this study, we examined the cost-effectiveness, budget impact, and overall economic impact of IPS, using data from the EQOLISE trial.
Methods
Overall design of the EQOLISE study
In the EQOLISE trial, 312 individuals with severe mental illness (schizophrenia and schizophrenia-like disorders, bipolar disorder, or depression with psychotic features, using IDC-10 criteria) were randomly assigned to receive either IPS (n=156) or standard vocational services (n=156). The sample was drawn from six European cities: Groningen (Netherlands), London (UK), Rimini (Italy), Sofia (Bulgaria), Ulm-Günzburg (Germany), and Zurich (Switzerland). People who entered the trial had been ill and experiencing major difficulties accomplishing normal roles for at least 2 years and had not been employed for at least 1 year. They were followed for 18 months.
People assigned to the IPS group received IPS services with fidelity ratings ranging from good to fair (61 to 70 of 75, with a median of 65) 11. Comparison interventions, which were selected to represent the best typical vocational rehabilitation service in each city, followed the train-and-place approach and consisted of day treatment or, in the case of Ulm, residential care. Randomization was at the individual participant level and stratified using the minimization technique by center diagnosis and work history (more or less than 1 year of employment in a previous job). Further details are given elsewhere 6,12.
Economic evaluation
The economic evaluation was carried out from the perspective of the health and social care system: the costs of mental and physical health care, social care (including care accommodation), and vocational rehabilitation services were considered. The number of days worked in competitive settings, and the percentage of sample members who worked at least 1 day, served as measures of effectiveness for the cost-effectiveness analysis.
In addition, we were interested to examine whether IPS was cost-saving compared to vocational rehabilitation services (in the sense that it cost less to run), and whether it was cost-beneficial (in the sense that the outcomes achieved by IPS when expressed in monetary terms exceeded the costs, compared to vocational rehabilitation).
Measures
Vocational staff in each service kept track of each individual's work experience on an ongoing basis, noting which individuals worked for at least 1 day in competitive settings, and alerting research staff to any jobs that clients might obtain. Research staff then contacted individuals and administered a questionnaire, at the start and after the end of each job, ascertaining hours and days worked.
Data on individual characteristics, outcomes, and use of services were collected at baseline, and 6, 12, and 18 months later. A tailored version of the Client Socio-demographic and Service Receipt Inventory — European Version (CSSRI-EU) 13 was administered at each of these assessment points to collect individual-level data on socio-demographics, usual living situation, employment, income, use of health and social care services, and medication use over the previous 6 months.
The costs of IPS and usual vocational services were calculated from information collected locally from these services in each site. To keep unit costs in line with costs estimated for other services, we applied UK unit costs to human resources. Other revenue and overhead costs were calculated on the basis of service-level data on the proportion of their total costs that were comprised of salary costs. We applied that same ratio to the salary costs we calculated for each service. Capital costs were excluded due to a lack of data across the six countries. Where relevant, costs were converted using purchasing power parities to 2003 prices (in British pounds). Total costs for each service were divided by the number of clients to derive average cost per client, adjusted to reflect an 18-month period. For sites with multiple IPS or other vocational services or sites that supplied data at multiple time points, we calculated costs per client for each service/time point and then took an average of these for each group.
Costs for other services were assigned by multiplying service use frequencies by unit costs. Unit costs for 2003 (when the trial began) were taken from the annual Personal Social Services Research Unit (PSSRU) volume for England 14. As other countries included in the study have no comparable sources of unit costs, and given the complications generated by using multiple cost bases, figures for England were used for all countries.
Analyses
Data were analyzed using SPSS for Windows Release 12.0.1 15 and STATA 8.2 16 and 10.1 17 for Windows. Individuals were analyzed in the group to which they were randomized regardless of the type or level of input received from IPS or other vocational services. Analyses were conducted for all six centers together, on the grounds of statistical power, with subsequent examination of center-specific results.
Costs were compared at each assessment point and as totals over the whole 18-month period and are reported as mean values with standard deviations. Mean differences and 95% confidence intervals were obtained by nonparametric bootstrap regressions (1000 repetitions), which included baseline costs as a covariate.
Some values for 18-month cost data had to be imputed because 83 clients had missing cost data at one or more of the three follow-up points. Missing 18-month costs were estimated using the multiple imputation procedure in Stata 10.1, which estimated a predictive model for costs based on costs at each time point, age, gender, country, and randomization group. Budget impact was assessed by making comparisons of total costs over 18 months, both with and without imputation for missing values.
Incremental cost-effectiveness ratios were computed for each cost-outcome combination that showed both higher costs and better outcomes. These were calculated as the mean cost difference between the IPS and vocational services over the 18-month follow-up period divided by the mean difference between the groups in the outcome measure over that same period.
To assess the impact of sampling uncertainty on the probability that IPS is cost-effective given varying levels of willingness to pay (λ) for an additional unit of effectiveness (an additional day of work, or an additional 1% of study participants who worked for at least 1 day), cost-effectiveness acceptability curves based on the net benefit approach were constructed 18. These were based on the usual formula (net benefit=λ E – C), where E is effectiveness (additional day of work or additional 1% of clients who worked for at least 1 day), C is cost, and λ is the willingness to pay for one additional unit of effect.
A series of net-benefit values were calculated for each individual for a range of λ values between £0 and £1000 (in £200 increments). After calculating net benefit for each individual for each value of λ, coefficients of differences in net benefit between groups were obtained through a series of bootstrapped linear regressions (1000 repetitions) of group upon net benefit. The resulting coefficients were examined to calculate the proportion of times that the IPS group had a greater net benefit than the comparison services group for each value of λ. Finally, these proportions were plotted to generate cost-effectiveness acceptability curves based on pooled and site-specific perspectives. Imputed values were used for these calculations.
For the (partial) cost-benefit analysis, we calculated the monetary value of days employed minus total costs (intervention plus other services used) for the IPS and vocational rehabilitation groups, and then compared them by regressing net benefit (per individual) on randomization allocation, adjusting for baseline costs. We used bootstrap regression. The monetary value attached to each day of employment was based on the standard assumption in economic analyses that the gross wage paid is an estimate of the social value of what is produced. The average gross rate of pay for someone who was previously supported by welfare benefits because of sickness or disability was calculated from UK data on destinations of benefit leavers and the wages they earned in 2003 19. This gives a gross average daily wage of £54.81, which was then applied to data collected in the trial on number of days worked. Note that this is a partial cost-benefit analysis, because we did not attach monetary values to any observed improvements in health or quality of life.
Results
Sample
The characteristics of the sample members at baseline have been reported elsewhere: there were no differences between the IPS and control groups on any of the baseline variables measured, including age, gender, education, living situation, immigrant status, lifetime hospital admissions, distribution of diagnoses, or work history during the previous 5 years 6.
Outcomes
As reported previously 6, the EQOLISE trial found that IPS was more effective than vocational services for every vocational outcome studied: 85 (55%) of the individuals assigned to IPS worked for at least 1 day during the 18-month follow-up period compared with 43 (28%) individuals assigned to vocational services. Individuals assigned to vocational services were significantly more likely to drop out of the service (45%) and to be readmitted to hospital (31%) than people in the IPS arm of the trial (13% and 20%, respectively). The trial also found that context was important, with local unemployment rates explaining a substantial proportion of the observed variation in IPS effectiveness.
Costs
Inpatient costs for the IPS group, which were somewhat higher than those for the usual care group at baseline, declined much more than those for the usual care group over the first 6 months following randomization, so that adjusted inpatient costs over the first 6 months were significantly lower for IPS than for the usual care group (Table 1). However, the difference diminished over the subsequent 6 months, and these inpatient costs were virtually identical over the final 6 months. In contrast, outpatient service costs (adjusted for baseline outpatient costs) were greater for the IPS group over the final 6-month follow-up period, but the difference was small. Total costs over the first 6 months were lower for the IPS group by more than £2,700, but differences over the two subsequent 6-month periods were not significant.
Table 1.
Mean health and social care costs (£, 2003) for 6-month period at T0, T1, T2, and T3
| IPS | Vocational services | Difference between IPS and vocational servicesa | |||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|||||||
| Time | N | Mean | SD | Valid N | Mean | SD | Mean | 95% CI | |
| Accommodation | 0 | 156 | 822 | 4612 | 156 | 928 | 4801 | −107 | −1141, 946 |
| 1 | 141 | 531 | 1952 | 130 | 391 | 1389 | 146 | −222, 523 | |
| 2 | 133 | 499 | 1821 | 130 | 523 | 1977 | −23 | −479, 438 | |
| 3 | 132 | 536 | 1981 | 120 | 748 | 2165 | −206 | −715, 311 | |
| Inpatient services | 0 | 156 | 6034 | 10,575 | 156 | 5007 | 10,044 | 1027 | −1121, 3293 |
| 1 | 141 | 1861 | 6830 | 130 | 4056 | 9737 | −2580 | −4335, −717 | |
| 2 | 133 | 2499 | 7951 | 130 | 3222 | 8490 | −1253 | −3126, 696 | |
| 3 | 132 | 3441 | 10,915 | 120 | 3475 | 9176 | −606 | −2837, 1640 | |
| Outpatient services | 0 | 156 | 442 | 1415 | 156 | 269 | 1137 | 172 | −119, 423 |
| 1 | 141 | 296 | 1189 | 130 | 132 | 644 | 161 | −40, 396 | |
| 2 | 133 | 107 | 467 | 130 | 105 | 637 | 3 | −139, 128 | |
| 3 | 132 | 242 | 1314 | 120 | 41 | 183 | 199 | 18, 455 | |
| Community−based services | 0 | 156 | 512 | 1531 | 156 | 480 | 1388 | 32 | −273, 353 |
| 1 | 141 | 605 | 1475 | 130 | 626 | 1484 | 1 | −285, 286 | |
| 2 | 133 | 543 | 1546 | 130 | 544 | 1241 | 19 | −274, 348 | |
| 3 | 132 | 911 | 3006 | 120 | 498 | 1626 | 417 | −156, 1027 | |
| Community−based professions | 0 | 156 | 977 | 1437 | 156 | 811 | 1182 | 166 | −132, 467 |
| 1 | 141 | 835 | 1233 | 130 | 1198 | 2960 | −464 | −1036, 13 | |
| 2 | 133 | 1073 | 4435 | 130 | 706 | 1172 | 355 | −219, 1237 | |
| 3 | 132 | 834 | 1643 | 120 | 790 | 1352 | −11 | −377, 355 | |
| Medication | 0 | 156 | 483 | 490 | 156 | 502 | 596 | −19 | −144, 103 |
| 1 | 141 | 559 | 538 | 130 | 522 | 569 | 49 | −50, 156 | |
| 2 | 133 | 520 | 613 | 128 | 522 | 604 | 22 | −99, 155 | |
| 3 | 132 | 624 | 756 | 120 | 700 | 935 | −62 | −254, 117 | |
| Total (excl. intervention cost) | 0 | 156 | 9269 | 10,980 | 156 | 7998 | 10,991 | 1271 | −994, 3661 |
| 1 | 141 | 4688 | 7236 | 130 | 6926 | 10,417 | −2720 | −4624, −813 | |
| 2 | 133 | 5241 | 9428 | 128 | 5694 | 9460 | −960 | −3228, 1443 | |
| 3 | 132 | 6589 | 12,560 | 120 | 6253 | 9905 | −319 | −2781, 2336 | |
IPS – Individual Placement and Support
Based on bootstrapped linear regression of group upon cost (1000 repetitions)
T1, T2, and T3 mean differences are adjusted for baseline estimate of relevant cost component
The cost of the IPS intervention itself varied threefold across sites (being highest in Sofia and lowest in Ulm), while the costs of comparison interventions varied more than 10-fold (being highest in Zurich and lowest in Groningen; Table 2). Looking only at intervention costs, IPS was more expensive than comparison services in two of the sites, less expensive in the four others.
Table 2.
Costs of the IPS and vocational service interventions over 18 months, average per client (£, 2003)
| IPS | Vocational services | |
|---|---|---|
| London | 2086 | 3234 |
| Ulm | 1568 | 8586 |
| Rimini | 2467 | 9520 |
| Zurich | 1870 | 14,447 |
| Groningen | 1692 | 1385 |
| Sofia | 4757 | 1567 |
IPS – Individual Placement and Support
Table 3 presents costs summed over 18 months, distinguishing between intervention and other costs (aggregated), with and without imputations for missing values. It also presents total costs (including imputations) by site. Averaged across sites, IPS services cost £4022 less than other vocational services. Total per person costs over 18 months (adjusted for baseline) were significantly lower — by about one-third — for the IPS group. Including imputations for missing values confirmed this. Total adjusted costs were lower for the IPS group at five out of six sites (the exception being Groningen), with differences for London, Ulm, and Zurich reaching statistical significance.
Table 3.
Intervention costs and total 18-month costs (£, 2003)
| IPS | Vocational services | Difference between IPS and vocational servicesa | ||||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|
||||||
| N | Mean | SD | N | Mean | SD | Mean | 95% CI | |
| Intervention (IPS/vocational services) | 156 | 2424 | 1110 | 156 | 6446 | 4816 | −4022 | −4791, −3239 |
| Overall | ||||||||
| Excluding intervention cost | ||||||||
| Available cases | 120 | 15,490 | 20,329 | 109 | 19,488 | 25,855 | −5233 | −10,855, 20 |
| Imputed | 156 | 16,453 | 22,514 | 156 | 18,999 | 23,541 | −3845 | −7854, 862 |
| Including intervention cost | ||||||||
| Available cases | 120 | 17,814 | 20,201 | 109 | 26,206 | 27,076 | −9616 | −15,544, −4262 |
| Imputed | 156 | 18,877 | 22,372 | 156 | 25,445 | 24,856 | −7880 | −12,249, −3151 |
| Site−specific | ||||||||
| Including intervention cost and based on imputed data | ||||||||
| London | 25 | 7414 | 5232 | 25 | 10,985 | 8929 | −3769 | −7654, −240 |
| Ulm | 26 | 18,442 | 17,832 | 26 | 33,414 | 24,275 | −14,057 | −24,875, −3468 |
| Rimini | 26 | 32,194 | 39,256 | 26 | 36,480 | 35,195 | −10,261 | −20,038, 601 |
| Zurich | 26 | 20,483 | 15,908 | 26 | 36,133 | 22,691 | −17,944 | −28,956, −8545 |
| Groningen | 26 | 22,469 | 23,388 | 26 | 22,209 | 24,912 | 233 | −13,495, 14,171 |
| Sofia | 27 | 12,079 | 5870 | 27 | 13,359 | 9865 | −2026 | −6684, 2081 |
IPS – Individual Placement and Support
Based on bootstrapped linear regression of group upon cost (1000 repetitions) T1, T2, and T3 mean differences are adjusted for baseline estimate of relevant cost component
Eighty-three cases had missing cost data at one or more of the three time points
Cost-effectiveness
Incremental cost-effectiveness ratios were computed for each of the two outcomes in turn, first for the whole sample and then for each of the six sites (Table 4). At the five sites where overall costs were lower, IPS dominated the control condition: i.e., it was both more effective (on both outcome measures) and less costly. At the Groningen site, spending an additional £30 per person over 18 months by switching from usual vocational services to IPS resulted in an additional 1% of individuals working at least 1 day in a competitive setting; £10 per person “purchased” an additional day of work. It may be noted, however, that the difference of 24.2 days worked was large in relation to the difference of 7.7% in the proportion of people who worked at least 1 day, because one individual in the IPS service worked 456 days over the 18-month period. If this person was excluded from the analyses, the difference in days worked fell to 8.3; after this exclusion, £28 would be needed to achieve one additional day of work.
Table 4.
Incremental cost-effectiveness ratios for IPS versus vocational services (based on total 18-month costs)
| Cost perspective | Additional cost per additional 1% of people working at least 1 day | Additional cost per additional day worked |
|---|---|---|
| Overall—available cases | IPS dominates | IPS dominates |
| Overall—imputed costs | IPS dominates | IPS dominates |
| London—imputed costs | IPS dominates | IPS dominates |
| Ulm—imputed costs | IPS dominates | IPS dominates |
| Rimini—imputed costs | IPS dominates | IPS dominates |
| Zurich—imputed costs | IPS dominates | IPS dominates |
| Groningen—imputed costs | £233 / 7.7%=£30 | £233 / 24.2 days=£10 |
| Sofia—imputed costs | IPS dominates | IPS dominates |
IPS – Individual Placement and Support
Cost-effectiveness acceptability curves illustrate the probability that IPS is cost-effective in comparison with vocational services as a function of the amount a decision maker is willing to pay for an additional 1% of clients working for at least 1 day over the 18-month period or for an additional day of work (Figures 1 and 2, respectively). This probability was nearly equal to 1 in each case, for willingness-to-pay thresholds ranging from 0 to £1000. Inclusion or noninclusion of imputed values for missing data made no material difference to the result.
Figure 1.
Probability that Individual Placement and Support is cost-effective compared with vocational services for a range of values of willingness to pay for an additional 1% in people working at least 1 day
Figure 2.
Probability that Individual Placement and Support is cost-effective compared with vocational services for a range of values of willingness to pay for an additional day of work
Cost-effectiveness acceptability curves were plotted for each site for the outcome measuring “additional 1% of clients working” (Figure 3). With the smaller sample sizes involved, Zurich, Ulm, London, and Rimini showed the highest probabilities that IPS is cost-effective. Sofia followed closely. Groningen showed the lowest level, and IPS and vocational services would generally be interpreted from this evidence to be equivalent in that site. As a sensitivity analysis, the willingness to pay for an additional 1% of clients working at the Groningen site was increased to £5,000 and £10,000. The probability of cost-effectiveness still only reached 0.545 at the £10,000 threshold.
Figure 3.
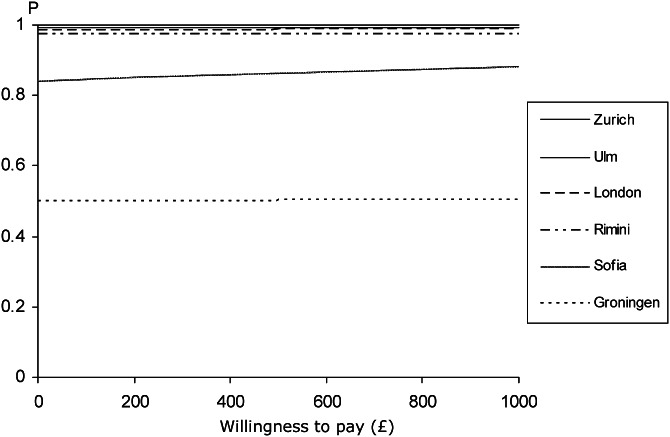
Probability (by site) that Individual Placement and Support is cost-effective compared with vocational services for a range of values of willingness to pay for an additional 1% in people working for at least 1 day
Cost benefit
The difference between the cost of the intervention and the value of employment achieved (days worked, valued at the expected gross wage in the UK for someone moving into employment following welfare benefits support because of sickness or disability) averaged −£9,440 for individuals in the IPS group and −£25,151 for individuals in the vocational rehabilitation group. These negative signs indicate that the costs of intervention and support exceeded the monetary value of the employment gained. To compare between the two groups, bootstrap regression (1000 replications) was used to adjust for baseline costs (to be consistent with our other analyses) and revealed a difference in net benefit of +£17,005 in favour of IPS. In other words, this (partial) cost-benefit analysis shows that IPS represents a more efficient use of resources than its comparator.
Discussion
Employment is a major contributor to an individual's economic status, social position, and quality of life. Unfortunately, people with severe mental illness have high rates of unemployment. For example, a five-country European study found less than a quarter of people with schizophrenia were in paid employment, the proportion being as low as 5% in London 20. The economic and social impacts of employment difficulties are enormous. For individuals, it can mean long-term reliance on state welfare benefits, insecure low-paid work, and a disability trap that makes it hard to escape 21. For the broader society, the impacts are the risk of an almost permanently marginalized, socially excluded group of people 21, and high costs: productivity losses because of unemployment or absenteeism account for a large proportion of the overall cost of schizophrenia across many countries 22.
Public policies across much of the world emphasize the importance of promoting employment opportunities for disadvantaged groups, including people with chronic disabilities and health problems 2,3. Although that policy attention has tended to focus more on people with common mental disorders, various attempts have been made to improve access to employment for people with severe mental health problems. These include the development of sheltered work settings, clubhouse models and social firms, and, more recently, integration into competitive work settings without prior preparatory steps, following the IPS approach. IPS seeks to place people in open paid employment, providing them with intensive and ongoing support. The approach has an encouraging track record in a number of US sites, and is beginning to be explored elsewhere. This wider exploration is needed because, for example, European health systems, benefits systems and labour markets differ in important ways from those in the United States.
In this multicenter European trial of supported employment, IPS was found to dominate alternative vocational services against which it was matched, producing better outcomes in terms of both the proportion of people who worked for at least 1 day and the number of days they worked at lower cost overall to the government provider of health and social care services. This pattern held at five of the six European centers, Groningen being the exception. With the inclusion of imputed values, the difference was maintained. An analysis of uncertainty using cost-effectiveness acceptability curves yields a consistent overall view of the findings in that, whether imputed values are used or not, IPS is almost certain to be viewed as more cost-effective than standard vocational services even if the decision maker is not willing to pay anything for an additional 1% of clients working at least 1 day or for an additional day of work. That IPS would yield better competitive employment outcomes than comparison vocational services in Europe should not be surprising, given that IPS has consistently done so almost everywhere it has been tested, whether in the United States, Canada, Australia, or Hong Kong 10. An exception is the Supported Work And Needs (SWAN) study 23, although concerns have been expressed about the fidelity of the IPS service delivered 24.
There are few cost-effectiveness results to frame the findings of the present study. Only three previous trials of IPS appear to have reported cost-effectiveness results, and cost-benefit results are even rarer. Comparing IPS with an enhanced vocational rehabilitation program in inner-city Washington, Dixon et al 25 estimated that IPS allowed clients to achieve additional hours of competitive work at an average cost of $13 per hour or $283 per additional week of competitive work (counting direct mental health costs). The SWAN trial found that, although the intervention cost only £296 per client, control group participants who were admitted to hospital had longer stays, so that total costs were £2176 higher on average for control group clients. The intervention was thus cost-effective (lower costs with similar effectiveness), but the saving in hospitalization seems unlikely to be attributable to the intervention, which had a very low intensity 23,26. Applying a cost-benefit framework to the New Hampshire trial of IPS, Clark et al 27 estimated a marginally higher benefit–cost ratio for IPS than for group skills training, from the perspectives of society as a whole (2.18 vs. 2.07) as well as from the perspective of government (1.74 vs. 1.39). Here both interventions were associated with significant, and nearly identical, reductions in costs of hospitalization.
The difference in the present study is partly attributable to IPS itself being less costly than comparison services: it cost less than comparison services in four sites. It is also attributable to lower inpatient costs — unlike the finding in the Washington trial. Among the five quasi-experimental studies that have looked for an association between hospital admissions (or hospital inpatient days) and being in IPS, three report no evidence of an association 28–30, whereas two others report fewer admissions for the IPS group 31–33. In one case, however, fewer admissions were found only among people with higher outpatient mental health service use 32.
There are a number of reasons why IPS might reduce hospital use. Vocational advisors may happen to observe, for example, signs that their client is on the way to a crisis and alert his or her clinicians. Their relationship with a client may in and of itself have a therapeutic effect. Clients who do begin to work may experience an improvement in symptoms and self-esteem 34,35, which might in turn reduce hospitalizations. Studies that have considered the effects of working on overall treatment costs do suggest that, in clients who enter into work (which IPS facilitates but does not guarantee), there are reductions in treatment costs 36–38, and these are largely influenced by inpatient use.
In the present study, inpatient hospital use for the IPS group was reduced significantly only during the first 6 months; the difference essentially disappeared by the end of the follow-up period. Further analyses (not reported here) indicated considerable variability in the difference in inpatient costs between IPS and comparison groups across sites and over time. Indeed, both fixed effects and random effects regressions of inpatient costs over time, service and the interaction between the two, indicated an overall downward trend in hospitalization costs, but no difference in trend between IPS and usual services (p=0.34 and 0.44, respectively). The observed difference at 6 months could therefore be attributable to chance. In only one of the six sites (Groningen) did IPS generate numerically higher costs than the comparison intervention (but the difference was not significant). This was the site where IPS was implemented in the least effective way compared with usual services: it appears to represent an atypical experience.
Variations in vocational service costs across sites also bear comment. Not surprisingly, given the heterogeneity in traditional vocational services, the cost of comparison services varied widely across sites. The considerable (threefold) variation in costs of IPS services was more surprising, because the same unit costs were used to calculate those costs across sites, and because all sites achieved good or fair levels of fidelity to the IPS model 6. Differences in infrastructure may account for some of the variability in IPS intervention costs.
The cost-effectiveness analysis was conducted from the perspective of the health care system, with costs measuring only health and social care inputs. Although effectiveness was gauged in terms of employment gained, this is a valid aim for community mental health services. When we turned to the cost-benefit arguments, we attached an estimate of the societal value of the employment gained but we did not attempt to attach monetary values to any other clinical or quality of life gains. Even so, this partial analysis demonstrated the broader social value of the IPS approach.
Limited sample size for the cost analysis is a limitation of the study, although one that is difficult to avoid given the complexity (and cost) of conducting studies such as this. The use of UK unit costs for all study sites may also be viewed as a limitation of the study, but this could not be avoided given the absence of country-specific information to compute valid and comparable unit costs in all sites. Moreover, using country-specific unit costs introduces further extraneous variation that would have to have been adjusted for in the analyses. In fact, unit costs for health services and social care are largely driven by local wage rates. Lower wage rates in some sites, such as Sofia, would tend to reduce all unit costs more or less proportionately, so that it is unlikely that the observed differences in cost between IPS and comparison services would alter very much in magnitude. Another limitation is that it was not possible to take into account changes in the cost of welfare benefits linked to unemployment benefits or changes in income tax contributions. For a cost-effectiveness analysis, these would be irrelevant as they are transfer payments, but they would be of interest to government that has to fund them.
When public bodies seek to introduce policies to improve employment rates among people with mental health needs, they do not tend to devote much attention to people with the most severe needs. This may be because of the comparatively small numbers of people involved, and perhaps because policy-makers do not believe much can be done at an affordable cost. However, this six-country European study paints a rosier picture.
This is not merely a case of helping people move from unemployment to employment, fundamentally important though that is, but of addressing needs of people facing long-term disadvantage. Employment is both a source of income and independence and a major contributor to social inclusion, self-determination, and recovery. IPS appears to provide an effective and cost-effective means of helping many people with a serious mental illness to come closer to achieving their employment goals.
Acknowledgments
This study was supported by a grant from the European Commission, Quality of Life and Management of Living Resources Programme, QLRT 2001-00683. Thanks are due to G. McHugo for methodological advice, to D.R. Becker for training the IPS Workers, and to the IPS workers themselves: A. Lewis (London), W. Dorn and E. Marishka (Ulm), D. Piegari (Rimini), B. Bartsch and P. Meyer (Zurich), A. Mieke Epema, L. Jansen and B. Hummel (Groningen), P. Karaginev (Sofia). The authors also thank J.L. Fernandez (London School of Economics) for comments on an earlier draft.
References
- 1.Marwaha S, Johnson S, Bebbington P, et al. Rates and correlates of employment in people with schizophrenia in the UK, France and Germany. Br J Psychiatry. 2007;191:30–7. doi: 10.1192/bjp.bp.105.020982. [DOI] [PubMed] [Google Scholar]
- 2.Department of Health. No health without mental health: a cross-government mental health outcomes strategy for people of all ages. London: Department of Health; 2011. [Google Scholar]
- 3.European Commission. Improving the mental health of the population: towards a strategy on mental health for the European Union. Brussels: Commission of the European Union, 2005; [Google Scholar]
- 4.Bond GR, Drake RE, Becker DR. An update on randomised controlled trials of evidence-based supported employment. Psychiatr Rehabil J. 2008;31:280–90. doi: 10.2975/31.4.2008.280.290. [DOI] [PubMed] [Google Scholar]
- 5.Corrigan PW, Mueser KT, Bond GR, et al. Principles and practice of psychiatric rehabilitation: an empirical approach. New York: Guilford; 2008. [Google Scholar]
- 6.Burns T, Catty J, Becker T, et al. The effectiveness of supported employment for people with severe mental illness: a randomised controlled trial. Lancet. 2007;370:1146–52. doi: 10.1016/S0140-6736(07)61516-5. [DOI] [PubMed] [Google Scholar]
- 7.Latimer E, Lecomte T, Becker D, et al. Generalisability of the individual placement and support model of supported employment: results of a Canadian randomised controlled trial. Br J Psychiatry. 2006;189:65–73. doi: 10.1192/bjp.bp.105.012641. [DOI] [PubMed] [Google Scholar]
- 8.Killackey E, Jackson HJ, McGorry PD. Vocational intervention in first-episode psychosis: individual placement and support v. treatment as usual. Br J Psychiatry. 2008;193:114–20. doi: 10.1192/bjp.bp.107.043109. [DOI] [PubMed] [Google Scholar]
- 9.Wong K, Chiu R, Tang B, et al. A randomised controlled trial of a supported employment program for persons with long-term mental illness in Hong Kong. Psychiatr Serv. 2008;59:84–90. doi: 10.1176/ps.2008.59.1.84. [DOI] [PubMed] [Google Scholar]
- 10.Bond GR, Drake RE, Becker DR. Generalizability of the Individual Placement and Support (IPS) model of supported employment outside the US. World Psychiatry. 2012;11:32–9. doi: 10.1016/j.wpsyc.2012.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bond GR, Becker DR, Drake RE, et al. A fidelity scale for the Individual Placement and Support model of supported employment. Rehabil Couns Bull. 1997;40:265–84. [Google Scholar]
- 12.Catty J, Lissouba P, White S, et al. Predictors of employment for people with severe mental illness: results of an international six-centre randomised controlled trial. Br J Psychiatry. 2008;192:224–31. doi: 10.1192/bjp.bp.107.041475. [DOI] [PubMed] [Google Scholar]
- 13.Chisholm D, Knapp M, Knudsen HC, et al. Client Socio-demographic and Service Receipt Inventory — EU version: development of an instrument for international research. Br J Psychiatry. 2000;177(Suppl. 39):28–33. doi: 10.1192/bjp.177.39.s28. [DOI] [PubMed] [Google Scholar]
- 14.Curtis L, Netten A. Unit Costs of Health and Social Care 2003. Canterbury: PSSRU, University of Kent; 2003. [Google Scholar]
- 15.SPSS Inc. SPSS for Windows Release 12.0.1. SPSS Inc; 1989. -2001. [Google Scholar]
- 16.StataCorp LP. STATA 8.2 for Windows. StataCorp LP; 1985. -2004. [Google Scholar]
- 17.StataCorp LP. STATA 10.1 for Windows. StataCorp LP; 1985. -2009. [Google Scholar]
- 18.van Hout BA, Al MJ, Gordon GS, et al. Costs, effects and C/E-ratios alongside a clinical trial. Health Econ. 1994;3:309–19. doi: 10.1002/hec.4730030505. [DOI] [PubMed] [Google Scholar]
- 19.Bowling J, Coleman N, Wapshott J, et al. Destinations of benefit leavers. London: Department for Work and Pensions; 2004. [Google Scholar]
- 20.Knapp M, Chisholm D, Leese M, et al. Comparing patterns and costs of schizophrenia care in five European countries: the EPSILON study. Acta Psychiatr Scand. 2002;105:42–54. doi: 10.1034/j.1600-0447.2002._10310.x. [DOI] [PubMed] [Google Scholar]
- 21.Drake RE, Bond G, Thornicroft G, et al. Mental health disability: an international perspective. J Disability Policy Studies. (in press) [Google Scholar]
- 22.Knapp M, Mangalore R, Simon J. The global costs of schizophrenia. Schizophr Bull. 2004;30:279–93. doi: 10.1093/oxfordjournals.schbul.a007078. [DOI] [PubMed] [Google Scholar]
- 23.Howard L, Heslin M, Leese M, et al. Supported employment: randomised controlled trial. Br J Psychiatry. 2010;196:404–11. doi: 10.1192/bjp.bp.108.061465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Latimer E. An effective intervention delivered at sub-therapeutic dose becomes an ineffective intervention. Br J Psychiatry. 2010;196:341–2. doi: 10.1192/bjp.bp.109.073338. [DOI] [PubMed] [Google Scholar]
- 25.Dixon L, Hoch JS, Clark R, et al. Cost-effectiveness of two vocational rehabilitation programs for persons with severe mental illness. Psychiatr Serv. 2002;53:1118–24. doi: 10.1176/appi.ps.53.9.1118. [DOI] [PubMed] [Google Scholar]
- 26.Heslin M, Howard L, Leese M, et al. Randomised controlled trial of supported employment in England: 2 year follow-up of the Supported Work And Needs (SWAN) study. World Psychiatry. 2011;10:132–7. doi: 10.1002/j.2051-5545.2011.tb00035.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Clark RE, Xie H, Becker DR, et al. Benefits and costs of supported employment from three perspectives. J Behav Health Serv Res. 1998;25:22–34. doi: 10.1007/BF02287497. [DOI] [PubMed] [Google Scholar]
- 28.Bailey E, Ricketts S, Becker D, et al. Do long-term day treatment clients benefit from supported employment? Psychiatr Rehab J. 1998;22:24–9. [Google Scholar]
- 29.Becker DR, Bond GR, McCarthy D, et al. Converting day treatment centers to supported employment programs in Rhode Island. Psychiatr Serv. 2001;52:351–7. doi: 10.1176/appi.ps.52.3.351. [DOI] [PubMed] [Google Scholar]
- 30.Clark RE, Bush PW, Becker DR, et al. A cost-effectiveness comparison of supported employment and rehabilitative day treatment. Admin Policy Ment Health. 1996;24:63–77. [Google Scholar]
- 31.Drake RE, Becker DR, Biesanz JC, et al. Rehabilitative day treatment vs. supported employment: I. Vocational outcomes. Commun Ment Health J. 1994;30:519–31. doi: 10.1007/BF02189068. [DOI] [PubMed] [Google Scholar]
- 32.Drake R, Becker D, Biesanz JC, et al. Day treatment vs supported employment for persons with severe mental illness: a replication study. Psychiatr Serv. 1996;47:1125–7. doi: 10.1176/ps.47.10.1125. [DOI] [PubMed] [Google Scholar]
- 33.Henry AD, Lucca AM, Banks S, et al. Inpatient hospitalisations and emergency service visits among participants in an Individual Placement and Support (IPS) model program. Ment Health Serv Res. 2004;6:227–37. doi: 10.1023/b:mhsr.0000044748.24924.a0. [DOI] [PubMed] [Google Scholar]
- 34.Bond G, Resnick S, Drake R, et al. Does competitive employment improve nonvocational outcomes for people with severe mental illness? J Consult Clin Psychol. 2001;69:489–501. doi: 10.1037//0022-006x.69.3.489. [DOI] [PubMed] [Google Scholar]
- 35.Mueser KT, Becker DR, Torrey WC, et al. Work and non-vocational domains of functioning in persons with severe mental illness: a longitudinal analysis. J Nerv Ment Dis. 1997;185:419–26. doi: 10.1097/00005053-199707000-00001. [DOI] [PubMed] [Google Scholar]
- 36.Bush P, Drake R, Xie H, et al. The long term impact of employment on mental health service use and costs for persons with severe mental illness. Psychiatr Serv. 2009;60:1024–31. doi: 10.1176/ps.2009.60.8.1024. [DOI] [PubMed] [Google Scholar]
- 37.Perkins DV, Born DL, Raines JA, et al. Program evaluation from an ecological perspective: supported employment services for persons with serious psychiatric disabilities. Psychiatr Rehabil J. 2005;28:217–24. doi: 10.2975/28.2005.217.224. [DOI] [PubMed] [Google Scholar]
- 38.Schneider J, Boyce M, Johnson R, et al. Impact of supported employment on service costs and income of people with mental health needs. J Ment Health. 2009;18:533–42. [Google Scholar]


