Anxiety disorders, among the most prevalent childhood psychiatric disorders, significantly impair current functioning and portend increased risk for various problems in adolescence and adulthood1,2. Therefore, studying risk factors is crucially important. One such risk factor is the child temperament of behavioral inhibition (BI). Children with this temperament are significantly more likely to develop anxiety disorders than children with other temperaments1.
Research on BI delineates how children shape and respond to their social environments. From infancy, children with BI display heightened reactions to novelty and heightened sensitivity to stimulus variations, and in toddlerhood, they withdraw from novel or unfamiliar social situations. As they recurrently withdraw, this tendency evolves to leave the inhibited child less assertive and more prone to rejection than their peers, catalyzing the growth of negative self-perceptions. Relative to their peers, behaviorally inhibited children experience more social rejection, interpret ambiguous social encounters as particularly rejecting, more vigorously tend to avoid social stressors, and more often respond to social rejection with attributions of internal failings and avoidant coping. BI, then, by shaping personal relationships across early and middle childhood, may set the stage for early adolescent social anxiety, which occurs at a time when peers become increasingly important3.
BI is only moderately stable4. This raises questions about factors that distinguish children with relatively high, stable levels of inhibition, and an associated elevated risk for anxiety, from those with either unstable or consistently low levels of inhibition. One critical factor appears to be attention biases towards threat4. Emerging data suggest that a bias to orient towards threats, a sign of vigilance, shapes the relation that BI shows over time with later anxiety disorders5. In the clinical anxiety literature, associations between such threat-related attention biases and various anxiety-related outcomes represents one of the most consistently observed findings. Relative to non-anxious individuals, anxious individuals tend to display greater vigilance towards threatening information during early, automatic stages of processing, as well as show greater difficulty in disengaging attention from threats once they have been engaged and more elaborately processed6.
Prior research has described a distributed neural circuit that is engaged when threats capture attention. This work relies on a task called the “dot-probe” paradigm, which quantifies the capacity of threat stimuli, such as angry faces, to divert attention from a simple motor task (See Figure 1). Biases in the engagement of this circuit are thought to account for the association between clinical anxiety and vigilance towards threat, as manifest behaviorally on the dot-probe task. Two key components of this circuit comprise the amygdala and the ventro-lateral prefrontal cortex (vlPFC)7. The amygdala is a structure centrally involved in salience detection and stimulus-reinforcement learning. Imaging work, both with clinically-anxious and with behaviorally inhibited subjects, has found amygdala hyperactivity to threat-relevant cues (e.g., angry faces), reflecting the enhanced salience of such cues. Considerable basic science work delineates the ways in which the amygdala and vlPFC support attention orienting, when individuals confront threats. This knowledge can be used to understand how individual differences in brain functions map onto individual differences in risk and clinical outcomes. The vlPFC is a region that adjusts attention so that goal-directed behavior can remain aligned with signals concerning the nature of threat-salience information. Individual differences in amygdala and vlPFC engagement in the context of attention orienting thereby reflect two fundamental processes linked to attention control. Amygdala response might reflect children’s immediate ascertainment of initial level of threat in the environment. vlPFC engagement might then reflect children’s response to such threats, in terms of the allocation of attention7
Figure 1.
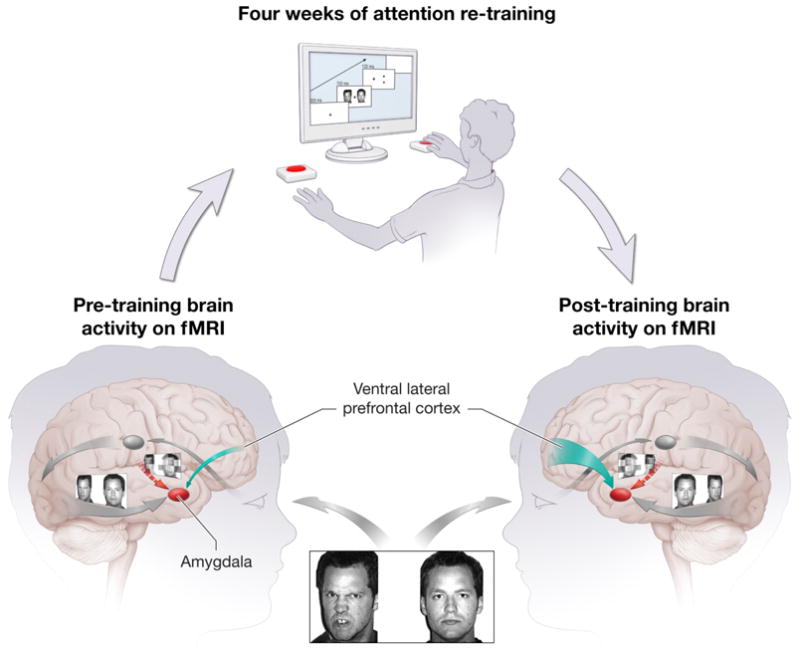
depicts expected re-training related changes in brain activity on fMRI. Before attention re-training, the left side of the figure depicts amygdala-ventral lateral prefrontal cortex (vlPFC) engagement on the dot-probe task. This shows that experimental events that elicit attention orienting, while viewing threat-neutral face pairs on the dot-probe task, engage the amygdala and vlPFC, with relatively weak vlPFC engagement, as indicated by a thin green arrow. Next, a subject undergoes four weeks of re-training with the dot-probe task, administered on a computer. The right side of the figure shows increased vlPFC engagement on the dot-prob task, with an increase in vlPFC function, as indicated by the thick green arrow
From this perspective, behaviorally inhibited children, as a group, may show a heightened tendency to respond immediately to threats in the environment, a response mediated by early amygdala engagement5. However, among this relatively large group of children, the subset who can successfully control attention, through compensatory engagement of the vlPFC, may face relatively low risk for adverse outcomes as well as less extreme attention biases, in terms of their behavior. Finally, the malleability of the immature fear circuit in infants and young children underscores the importance of studying these processes as they emerge over time. Thus, it may be easier to shape amygdala-vlPFC function and its effects on attention in relatively young as compared to older children. And, changes in attention early in the life of a child may have more opportunities to influence development and associated long-term risk, relative to changes in the older child.
Two recent studies from our group suggest that early attention biases to threat may indeed shape clinical outcomes over time. Both studies relied on variants of the same dot-probe task employed in imaging work on attention biases in clinical anxiety. In one study, using a longitudinal design, we examined BI in toddlerhood, attention biases during preschool, and preschool social withdrawal. Findings indicated that attention bias to threat moderated the outcome of early childhood BI, predicting preschool levels of social withdrawal8. In the second study, similar relationships were found among BI in toddlerhood, attention biases during adolescence, and adolescent social withdrawal. These data link attention with negative socio-emotional outcomes and the later emergence of clinical anxiety.
Recent work on attention bias has focused on novel intervention strategies9. Studies have attempted to train anxious subjects in such a way that they learn implicitly how to avoid threats and attend preferentially to neutral stimuli. These studies have used modifications of the very same dot-probe paradigm employed in imaging work on clinical anxiety and in the two studies described above concerning behavioral inhibition. Attention bias modification in clinically anxious and high-trait-anxiety adult populations appears to produce meaningful clinical benefits10. These findings have stimulated work in children, where two recent studies show that children respond similarly to adults when studied with attention-modification techniques. Such work has motivated a number of ongoing studies examining the utility of attention-bias-modification treatment for pediatric anxiety disorders9.
Clearly, work on attention-bias modification is important as a novel avenue for treating pediatric anxiety and for the clues that it provides concerning other therapeutic advances. Unlike treatments that arise through serendipitous clinical observation, attention-bias modification therapy is firmly grounded in cognitive neuroscience theory. Thus, by simultaneously examining the effects of such therapy on both clinical outcome and neural-circuitry function, this work directly generates insights into the neural mediators of successful treatment. These insights in turn can inform further advances in therapeutics7.
As noted above, threat-related attention biases reflect perturbations in a neural circuit connecting the amygdala to the vlPFC. At least some aspect of this perturbation occurs very rapidly when anxious children confront threats, more rapidly than can be described or, perhaps, even consciously perceived by the child. This rapidly-occurring perturbation involves dysfunctional connections between the vlPFC and the amygdala. Since this dysfunction cannot readily be perceived by the child, the child cannot easily discuss with a therapist at least some aspects of their attention dysfunction and its associated perturbation in vlPFC circuitry. Such discussions might occur during some forms of effective anxiety treatment, such as cognitive behavioral psychotherapy (CBT). Nevertheless, vlPFC activation does increase following CBT, though the mechanism for this change remains poorly-understood.
As shown in Figure 1, attention bias training may more directly shape vlPFC function and associated deficits in attention than CBT. Such training may operate similarly to other forms of training that allow people to master complex, rapidly-deployable motor tasks, like driving a car or hitting a baseball. Thus, much as one must directly practice driving or hitting to truly master the skill, the shaping of attention may benefit from recurrent, direct practice in the controlling of attention, as occurs in attention-bias training. Learning to drive requires both discussions about “rules-of-the-road” and practice in driving. The controlling of attention might require such discussions, as in CBT, as well as practice, as in attention-bias training.
The present paper reviews the link between BI and clinical anxiety disorder while considering the role of attention biases and the associated underlying neural circuitry involved in this link. To fully understand the developmental trajectories that lead to anxiety disorders in behaviorally inhibited children it is important to examine exactly how attention bias to threat develops over early childhood and exacerbate social withdrawal in these children. Finally, this paper introduces innovative methods which have turned the causal relation between attention and anxiety on its head, by training attention and in doing so reducing anxiety.
Acknowledgments
Support for this paper was provided in part by grants to NAF from NICHD (R37HD17899) and NIMH (MH074454)
Contributor Information
Nathan A. Fox, University of Maryland
Daniel S. Pine, National Institute of Mental Health
References
- 1.Perez-Edgar K, Fox NA. Temperament and anxiety disorders. Child and Adolescent Psychiatric Clinics. 2005;14:681–706. doi: 10.1016/j.chc.2005.05.008. [DOI] [PubMed] [Google Scholar]
- 2.Pine DS. Research review: A neuroscience framework for pediatric anxiety disorders. J Child Psych and Psychiatry. 2007;48:631–638. doi: 10.1111/j.1469-7610.2007.01751.x. [DOI] [PubMed] [Google Scholar]
- 3.Fox NA, Henderson HA, Marshall PJ, Nichols KE, Ghera MM. Behavioral inhibition: Linking biology and behavior within a developmental framework. Ann Rev Psych. 2005;56:235–262. doi: 10.1146/annurev.psych.55.090902.141532. [DOI] [PubMed] [Google Scholar]
- 4.Degnan KA, Fox NA. Behavioral inhibition and anxiety disorders: multiple levels of a resilience process. Develop Psychopath. 2007;19:729–746. doi: 10.1017/S0954579407000363. [DOI] [PubMed] [Google Scholar]
- 5.Fox NA, Hane AA, Pine DS. Plasticity for affective neurocircuitry: How the environment affects gene expression. Curr Dir Psych Sci. 2007;16:1–5. [Google Scholar]
- 6.Bar-Haim Y, Lamy D, Pergamin L, Bakermans-Kranenburg M, van IJzendoorn M. Threat-related attentional bias in anxious and nonanxious individuals: A meta-analytic study. Psych Bull. 2007;133:1–24. doi: 10.1037/0033-2909.133.1.1. [DOI] [PubMed] [Google Scholar]
- 7.Pine DS, Helfinstein SM, Bar-Haim Y, Nelson E, Fox NA. Challenges in Developing Novel Treatments for Childhood Disorders: Lessons from Research on Anxiety. Neuropsychopharm Rev. 2008:1–16. doi: 10.1038/npp.2008.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pérez-Edgar K, Reeb-Sutherland BC, McDermott JM, White LK, Henderson HA, Degnan KA, Hane AA, Pine DS, Fox NA. Attention bias to threat link behavioral inhibition to social withdrawal over time in very young children. J Abn Ch Psych. 2011;39:885–895. doi: 10.1007/s10802-011-9495-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bar-Haim Y. Research review: Attention bias modification (ABM): a novel treatment for anxiety disorders. J Child Psycho Psychiatry. 2010;52:859–870. doi: 10.1111/j.1469-7610.2010.02251.x. [DOI] [PubMed] [Google Scholar]
- 10.Hakamata Y, Lissek S, Bar-Haim Y, Britton JC, Fox NA, Leibenluft E, Ernst M, Pine DS. Attention bias modification treatment: A meta-analysis toward the establishment of novel treatment for anxiety. Biol Psychiat. 2010;68:982–990. doi: 10.1016/j.biopsych.2010.07.021. [DOI] [PMC free article] [PubMed] [Google Scholar]


