Abstract
STUDY DESIGN
Case report.
BACKGROUND
Rehabilitation that includes progressive quadriceps strengthening after total knee arthroplasty (TKA) leads to superior outcomes. Though patients with TKA show marked functional improvement after outpatient physical therapy, they continue to adopt movement asymmetries characterized by reduced knee excursion on the operated limb and excessive loading on the contralateral limb. The purpose of this case report was to describe the functional and biomechanical improvements in a patient who, after TKA, participated in a novel physical therapy protocol that included retraining of symmetrical movement patterns.
CASE DESCRIPTION
A 57-year-old female with unilateral knee osteoarthritis was evaluated prior to TKA and at 3 and 10 weeks after surgery. Postoperative rehabilitation included progressive quadriceps strengthening and movement retraining that consisted of visual, verbal, and tactile feedback to promote symmetrical weight bearing during strengthening exercises and functional activities. Outcomes were compared to a historical cohort of patients with TKA.
OUTCOMES
Prior to TKA, the patient scored below average on all functional measures and walked with knee biomechanics that were abnormal and asymmetrical. After symmetry retraining, her knee motion and moments were restored to normal levels. The patient also walked with greater magnitude and more symmetrical knee excursion compared to a cohort of similar patients.
DISCUSSION
This case report describes the use of a novel rehabilitation protocol intended to improve walking biomechanics and functional outcomes after TKA. Restoration of symmetrical movement patterns could improve long-term outcomes of TKA. Further research is needed to evaluate the effectiveness and implementation of similar rehabilitation strategies in a wide range of patients after TKA.
Keywords: motion analysis, osteoarthritis, physical therapy, rehabilitation, total knee replacement
Total knee arthroplasty (TKA) reliably reduces the pain associated with end-stage knee osteoarthritis (OA); however, patients who elect to undergo TKA demonstrate persistent functional impairments and long-term functional ability that is lower than age-matched, healthy control subjects.14 Persistent movement abnormalities and postoperative quadriceps weakness of the operated limb, as well as a decline in strength of the nonoperated limb, may contribute to functional deficits that persist several years after surgery.3,9,10
Despite an annual incidence of more than 500 000 procedures, there are few published guidelines on outpatient rehabilitation after TKA. The National Institutes of Arthritis and Musculoskeletal and Skin Disease and the National Institutes of Health’s Office of Medical Applications Research convened a consensus development conference in 2003 to compile the scientific evidence surrounding TKA to enhance clinical decision making guidelines and patient clinical outcomes.11 Some of the primary conclusions from this consensus conference were that “the use of rehabilitation services was one of the most understudied aspects of the perioperative management of patients following total knee replacement” and that “there is no evidence supporting the generalized use of any specific preoperative or postoperative rehabilitation interventions.”11 Outpatient physical therapy after TKA differs by geographic region and surgeon and ranges from no treatment at all to structured and progressive rehabilitation that includes strengthening, manual therapy, and modalities to reduce pain and swelling.2,5,12
We have previously demonstrated that functional outcomes are dependent on the rehabilitation protocol utilized after TKA12 and outpatient physical therapy regimens that include progressive quadriceps strengthening produce outcomes that are superior to regimens that include only therapeutic exercises and activities focused on restoring ambulatory ability.12 Despite outcomes after progressive strengthening that approached the levels of healthy control subjects, many patients demonstrated persistent weakness in the operated limb and movement asymmetries during walking, rising from a chair, and stair climbing that favored the nonoperated limb.1,6,10,15 These asymmetrical movement patterns increased joint load on the nonoperated limb by increasing knee adduction moment and vertical ground reaction force, which may be underlying causes of the greater need for contralateral knee joint replacement after the initial TKA.1,7 Incidence of contralateral TKA is nearly 40% within 10 years of the index surgery, and even patients with no or minimal symptoms in the contralateral knee at baseline experience OA progression and require contralateral TKA within 5 years.13 In a sample of 60 patients who had primarily unilateral OA at baseline, the status of the nonoperated limb was the best predictor of functional performance 3 years after TKA.3 Outpatient physical therapy protocols that incorporate functional retraining to reduce the load on the operated limb, emphasize normal and symmetrical motion, and preserve the integrity of the nonoperated joint may therefore reduce the incidence of contralateral TKA and lead to improved long-term functional outcomes.
To improve on traditional rehabilitation after TKA, we have developed a retraining program that includes biofeedback, with the intent to restore normal and symmetrical lower extremity joint motion during ambulation and dynamic functional activities. The purpose of this case report was to describe the functional and biomechanical improvements in a patient with severe end-stage knee OA who underwent unilateral TKA and participated in an outpatient physical therapy protocol that included progressive quadriceps strengthening, appropriate manual therapy, and biofeedback retraining.
CASE DESCRIPTION
Patient History
A 57-year-old female underwent unilateral tricompartmental TKA after a reported 3-year history of unilateral symptomatic OA in her left knee. Following TKA, the patient performed 2 weeks of home-care physical therapy before her initial outpatient physical therapy evaluation at the University of Delaware clinic. The patient’s past medical history was nonsignificant, but she reported a previous bunionectomy on the limb that underwent TKA that did not interfere with her functional performance. Prior to participation in the testing and intervention, the patient gave informed, written consent. The testing and intervention protocols were approved by the Human Subjects Review Board at the University of Delaware.
Evaluation
Evaluations were completed at 3 time points: (1) 1 week prior to TKA, (2) at the initial outpatient physical therapy session 3 weeks after TKA, and (3) at the last outpatient physical therapy appointment 10 weeks after TKA. The patient participated in functional testing on all 3 occasions, but motion analysis testing was only completed at the preoperative session and 10 weeks after TKA.
Functional testing consisted of a battery of clinical tests known collectively as the Delaware Osteoarthritis Profile.8 These functional tests included the following:
Timed up-and-go test. This test measured the time it took for the patient to rise from a standard-height chair (seat height, 46 cm), walk 3 m, and return to a seated position in the same chair. One practice test was performed, and the average of the 2 subsequent trials was recorded.
Stair-climbing test. This test measured the time it took the patient to ascend and descend 12 standard steps (18 cm in height and 28 cm in tread). A handrail was available during testing, although the patient was instructed to use the handrail only if required for safety. One practice test was performed, followed by 2 recorded trials. The stair-climbing test measures a higher level of function than the timed up-and-go test and therefore reduces the possibility of a ceiling effect.
Six-minute walk test. The patient was asked to cover as much distance as she could while walking on level ground for 6 minutes. The use of assistive devices was permitted.
Unilateral forefoot balance test. The patient was asked to stand on 1 limb for as long as she was able. The patient performed 3 trials on each limb until she lost balance or stood for 60 seconds. The average of the trials was recorded.
The patient also completed a number of self-report questionnaires, which included the following:
Knee Outcome Survey (KOS) activities of daily living scale. This subsection of the KOS contains 14 questions about an individual’s perception of his or her ability to perform activities of daily living.
Short Form-36 Health Survey (SF-36). The SF-36 is a reliable, internally consistent, and easy-to-administer questionnaire that has been repeatedly used as a generic health measure in patients with TKA and knee OA. This questionnaire includes 8 scales of differing domains of health, of which the physical functioning scale (PCS) and mental health scale (MCS) were calculated in this case report. The SF-36 is a norm-based test, with a score of 50 representing the national average.
Global rating scale. The patient rated her perception of knee functional ability on a scale of 0% to 100%, where 0% represents complete disability and 100% represents the level of knee function prior to the patient having any symptoms.
Knee Injury and Osteoarthritis Outcome Score. This is a valid, reliable, and responsive self-administered instrument designed to be used for patients with symptomatic OA. It consists of several subscales, including pain, other symptoms, function in daily living, function in sport and recreation, and knee-related quality of life.
Visual analog scale for pain. The patient rated her average and maximal pain over the past week for each knee on a 10-cm line with 1-cm intervals.
Clinical measures included the following:
Active and passive knee flexion and extension range of motion, measured with a standard long-arm goniometer. During extension measurement, the patient was positioned supine with her heel elevated on a block to ensure full knee extension. During flexion measurement, the patient was positioned supine and asked to draw her heel toward her buttocks.
Muscle strength. Quadriceps strength was measured using an isokinetic dynamometer (Kin-Com; Isokinetic International, East Ridge, TN). Isometric force output during active knee extension was measured with the knee at 75° of flexion. Force output was normalized to body mass index.
Anthropometric data. Height, weight, body mass index, and knee girth (circumference at the midpatella region) were collected at each session.
Prior to and 10 weeks after TKA, the patient’s walking was assessed using a 3-dimensional, 8-camera motion analysis system (Vicon Motion Systems, Oxford, UK). Retroreflective markers were placed bilaterally over the iliac crest, greater trochanter, lateral femoral epicondyles, lateral malleoli, upper and lower calcanei, and the lateral aspect of the fifth metatarsal. A cluster of 4 markers fixed to rigid thermoplastic shells was placed bilaterally over the lateral aspect of the shin and thigh, and a single shell was placed over the sacrum. Double-sided tape and elastic wraps (SuperWrap; Fabrifoam, Exton, PA) were used to affix all markers and shells to the patient’s skin. The patient was asked to walk at her own comfortable pace along a 10-m walkway. Two force plates embedded in the walkway recorded ground reaction force data during stance for each limb. Marker trajectories were low-pass filtered at 6 Hz, and forceplate data were low-pass filtered at 40 Hz. Ground reaction force data were normalized to body mass. Rigid body analysis and Euler angles were used to calculate joint angles. Joint moments were calculated via inverse dynamics and were expressed as net external moments normalized to body mass and height (Visual3D, Version 3.77; C-Motion, Inc, Germantown, MD). All data were time normalized to 100% of the gait cycle. Peak knee angles and knee, ankle, and hip moments were averaged across 6 walking trials. A ratio of symmetry was calculated for knee flexion excursion and knee extension excursion by dividing the peak of the operated limb by the peak of the nonoperated limb, where 1 represented complete symmetry between limbs. At the postoperative assessment, the patient was asked to walk at a similar speed to her preoperative pace.
Our patient’s functional and clinical status, as determined from the Delaware Osteoarthritis Profile, was compared to a historical group of 198 patients who had previously undergone progressive strengthening rehabilitation at our facility after TKA. Patients in this cohort were part of a larger clinical trial investigating the effects of neuromuscular electrical stimulation on the quadriceps as an adjunct to a progressive quadriceps strengthening and comprehensive rehabilitation program.12 Lower extremity kinetics and kinematics were compared to 4 subjects from this historical control group whose gaits were assessed at discharge from physical therapy. Qualitative comparisons were made between the outcomes from the current patient and those of the historical group.
Intervention
The patient attended physical therapy 2 to 3 times per week for 7 weeks (total of 17 visits). The intervention protocol consisted of 2 main components: (1) progressive strengthening exercises aimed at maximizing range of motion and quadriceps strength,12 and (2) biofeedback during functional activities aimed at improving normal movement patterns through restoration of symmetry between limbs (APPENDIX). The progressive strengthening protocol has been previously described, but consisted of non–weight-bearing and weight-bearing quadriceps strengthening exercises that were progressed in a standardized fashion as the patient met clinical milestones.12,17 Retraining via biofeedback consisted of several exercises, including weight-bearing strengthening on the SymSlide (Custom-KYnetics, Versailles, KY), a leg press device that monitors the magnitude of force through each limb (FIGURE 1A). When the force is equal between both limbs, a visual tracing displayed on a video monitor remains in the center of the screen. When the force is unequally distributed between limbs, the tracing moves toward the side of the screen corresponding to the lower extremity that is applying more force. The individual is instructed to keep the tracing within a predefined window on the monitor, the width of which can be reduced as the individual progresses (FIGURE 1B). Therapeutic exercises (eg, wall slides) and functional tasks (eg, sit-to-stand) were performed with visual feedback that encouraged symmetrical joint loading (FIGURE 2A). Patients stood on a Wii Balance Board (Nintendo of America Inc, Redmond, WA), while a custom-written software program on a laptop computer displayed the relative weight distribution between the left and right limbs. The digital signal from the Wii Balance Board was obtained via a Bluetooth connection. The visual display consisted of cylinders that filled or emptied according to the percentage of weight distributed to each limb (FIGURE 2B). Additional biofeedback on symmetrical weight bearing was provided by verbal and tactile cues from the therapist, and visual feedback was provided by a mirror during functional activities such as overground ambulation, walking on a treadmill, and stair climbing. The patient was progressed through more challenging tasks as clinical milestones were met. Details of the biofeedback protocol are provided in the APPENDIX. The patient’s home exercise program included strengthening exercises only, consistent with the programs prescribed to the historical control group.
FIGURE 1.
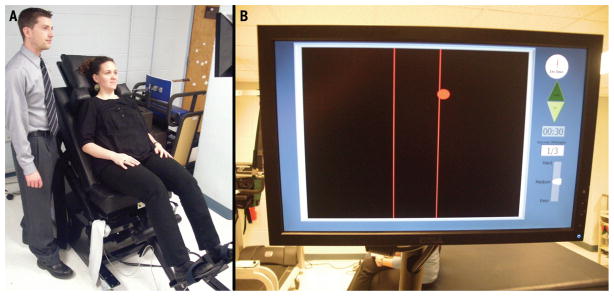
The SymSlide provides visual feedback on weight distribution during closed-chain knee exercises (A). To increase resistance on the SymSlide, the angle of inclination of the sled portion can be increased. In this case, the patient is putting more force through the right foot, as demonstrated by the ball drifting toward the right side of the target area (B).
FIGURE 2.
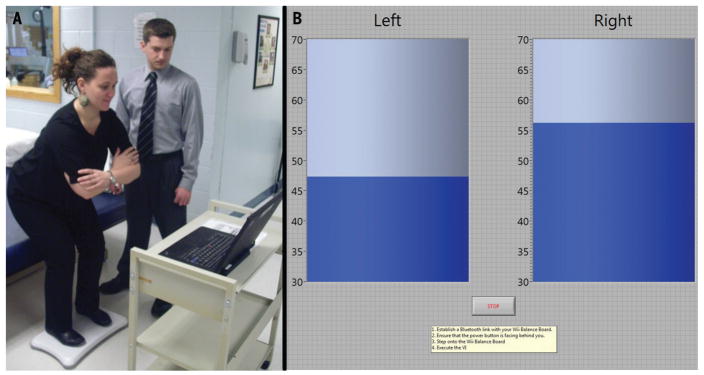
The patient is provided with visual feedback on weight distribution between limbs during sit-to-stand functional retraining exercises (A). In this case, the patient’s weight is shifted over her right limb during the movement (B).
OUTCOMES
At her testing session prior to surgery and at the initial physical therapy evaluation 3 weeks after TKA, the patient was substantially more impaired than the historical cohort of patients with TKA at the same time points for all performance and self-report questionnaires, with the exception of knee flexion range of motion and the global rating scale (TABLE). By the time of discharge from physical therapy, the patient had improved by 65% on the KOS activities of daily living, 3 points on the Knee Injury and Osteoarthritis Outcome Score pain, and 40% on the global rating scale, compared to her initial physical therapy evaluation. At discharge, her self-reported scores exceeded her preoperative evaluations and were substantially greater than scores from the historical cohort of patients with TKA treated at our facility. The patient demonstrated a 4.7-second improvement on the timed up-and-go test and a 23.3-second improvement on the stair-climbing test. She also walked 194 m farther on the six-minute walk test and improved by 13.1 seconds on the unilateral forefoot balance test, compared to scores at her initial physical therapy visit. Her performance-based scores were substantially better than her preoperative scores and were comparable to the average from the historical cohort of patients with TKA.
TABLE 1.
The Patient’s Functional Characteristics at All 3 Time Points
| Pre-TKA
|
Initial Physical Therapy Evaluation: 3 wk Post-TKA
|
10 wk Post-TKA
|
||||
|---|---|---|---|---|---|---|
| Case Report | Historical Cohort* | Case Report | Historical Cohort* | Case Report | Historical Cohort* | |
| Knee Outcome Survey activities of daily living, % | 37.1 | 50.3 ± 17.4 | 32.9 | 55.9 ± 13.6 | 98.6 | 79.0 ± 12.4 |
| Knee Outcome Survey pain, 0–5 | 2 | 2.9 ± 1.0 | 3 | 2.5 ± 1.0 | 0 | 1.2 ± 1.0 |
| Global rating scale, % | 65.0 | 54.9 ± 21.1 | 60.0 | 54.5 ± 19.1 | 100.0 | 73.5 ± 12.1 |
| Timed up-and-go, s | 11.1 | 10.2 ± 2.8 | 14.3 | 11.9 ± 3.5 | 9.6 | 8.3 ± 1.9 |
| Stair-climbing test, s | 23.4 | 20.3 ± 9.5 | 36.4 | 26.8 ± 12.2 | 13.1 | 13.8 ± 15.1 |
| Six-minute walk, m | 439.5 | 453.2 ± 125.0 | 327 | 402.0 ± 102.7 | 520.9 | 528.2 ± 109.2 |
| Unilateral balance test, operated limb, s | 13.5 | 20.1 ± 20.9 | 3.2 | 19.4 ± 19.9 | 16.3 | 29.6 ± 23.6 |
| Unilateral balance test, contralateral limb, s | 13.4 | 24.0 ± 22.6 | 38.9 | 25.8 ± 22.9 | 20.4 | 31.3 ± 23.1 |
| Passive knee flexion range, deg | 135 | 118 ± 14 | 95 | 98 ± 15 | 123 | 115 ± 11 |
| Quadriceps strength operated limb, N/BMI | 11.4 | 18.7 ± 7.5 | 3.9 | 10.0 ± 4.3 | 12.3 | 17.0 ± 6.7 |
| Quadriceps strength contralateral limb, N/BMI | 13.1 | 22.9 ± 9.1 | 15.5 | 23.5 ± 8.6 | 16.1 | 23.8 ± 6.4 |
Abbreviation: BMI, body mass index (kg/m2); TKA, total knee arthroplasty
Data for the historical cohort of patients (n = 198) are mean ± SD.
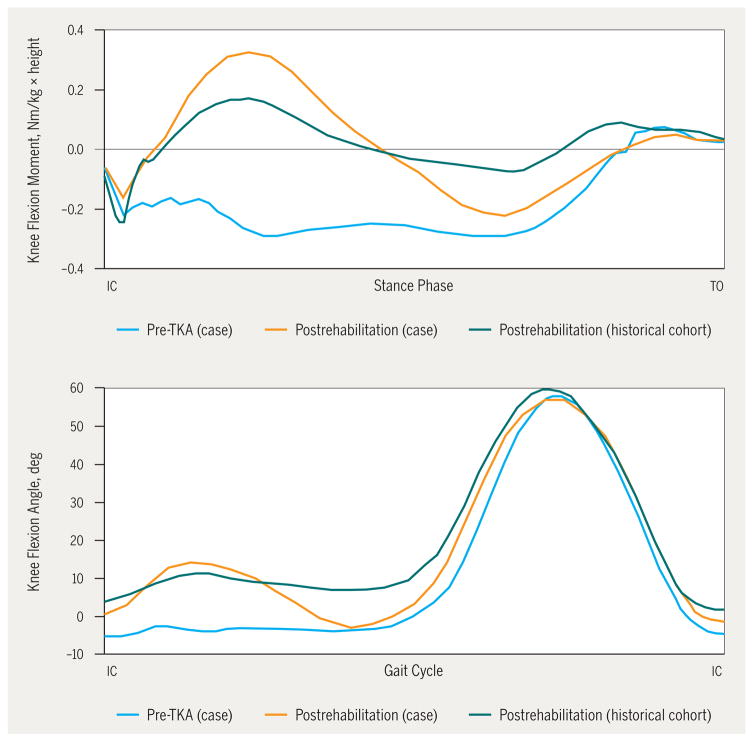
Prior to her TKA, the patient ambulated without any knee flexion excursion during loading response and demonstrated an abnormal knee flexion moment that was typical of a quadriceps avoidance or stiff-legged gait pattern common in patients with knee OA.4 Ten weeks after TKA, the patient demonstrated a restoration of normal and symmetrical knee motion (FIGURE 3), which improved to a greater extent than the average of a comparative group of subjects who received progressive strengthening but did not participate in the biofeedback protocol (FIGURE 3). At discharge from physical therapy, knee flexion excursion in the operated limb of this patient was 13.7°, compared to 7.3° for the historical control group. The ratio of knee flexion excursion (measured from heel strike to peak knee flexion) between the operated and nonoperated limbs was 0.9 for our patient and 0.5 for the patients with TKA who did not receive biofeedback training as part of postoperative rehabilitation. Similarly, the ratio of knee extension excursion (measured from peak knee flexion to peak knee extension) between limbs was 1.0 for our patient and 0.7 for the patients with TKA who did not receive biofeedback training.
FIGURE 3.
The patient who participated in biofeedback retraining (case) showed improvement in knee kinetics during stance (top) and knee flexion excursion during loading response (bottom). Her values after biofeedback retraining were greater than the comparative group of 4 individuals with total knee arthroplasty who were treated with a progressive strengthening program (historical cohort). Abbreviations: IC, initial contact; TO, toe-off.
Prior to TKA, our patient walked with peak knee adduction moments of 0.21 N/kg for the operated limb and 0.18 N/kg for the nonoperated limb. At 10 weeks post-TKA, the adduction moments were reduced to 0.19 N/kg for the operated limb and 0.11 N/kg for the nonoperated limb.
DISCUSSION
At the conclusion of a 7-week outpatient physical therapy program that included biofeedback on symmetry of movement patterns in addition to progressive strengthening, the patient demonstrated functional outcomes that were comparable to historical values and approached the levels of healthy age-matched controls.12 In addition to marked improvement in function, strength, and range of motion, the patient also demonstrated restoration of normal and symmetrical movement patterns in the sagittal plane during overground walking. The magnitude and symmetry of her knee joint excursions and sagittal plane joint moments were superior to those in the group of 4 individuals who underwent TKA but did not receive biofeedback for retraining of symmetry during outpatient rehabilitation. This case report provides promising preliminary information on how a rehabilitation program that focused on improving strength and promoting more symmetrical movement patterns during daily functional activities led to more normal gait biomechanics after TKA.
Long-term outcomes after TKA depend on the function of the contralateral limb,2 and even patients who are asymptomatic at baseline may eventually require contralateral TKA to manage progressive symptomatic OA of the nonoperated limb. The knee adduction moment is the best predictor of future progression of knee OA, so this biomechanical variable in the nonoperated limb may serve as an important marker of long-term functional ability after TKA. Patients with greater knee adduction moments in the nonoperated limb are at the highest risk for disease progression in the contralateral joint. Therefore, rehabilitation protocols that reduce this variable are important to include in postoperative care. Restoration of quadriceps strength symmetry has been shown to explain only a small percentage of the difference in adduction moments between limbs, and most assessments show an increased knee adduction moment in the contralateral limb, despite the absence of large strength differences.10,14 In contrast, our patient had a knee adduction moment in the contralateral limb that was less than that of the operated limb; knee adduction moments in both limbs were reduced in comparison to preoperative values. Therefore, the biofeedback retraining program in this study may be an adjunct to traditional rehabilitation and could reduce abnormal joint loading or knee adduction moment in the nonoperated limb.
Prior to TKA, our patient had quadriceps strength that was only two-thirds of the average of our historical sample. Her movement patterns with the operated limb were reflective of this considerable quadriceps weakness, and her gait was characterized by a lack of knee flexion and the absence of a knee flexion moment during loading. This pattern is typical of patients with end-stage knee OA and has been historically referred to as a quadriceps-avoidance gait pattern.4,16 Knee flex-ion during loading response is important for absorbing the impact of the body after initial contact; the absence of knee flexion during this phase requires compensation from other ipsilateral lower-limb joints.16 If the patient is not able to compensate, then he or she may experience an increase in the magnitude and rate of ipsilateral axial joint compression. Improving symmetry after TKA may, therefore, have implications for the operated limb as well as the nonoperated limb. At the conclusion of the 7-week program, our patient not only walked with greater knee flexion excursion and an improved knee flexor moment during loading, which is more typical of normal gait, but also adopted these characteristics to a greater extent than the standard-care TKA group. Furthermore, knee flexion and extension excursion were restored to levels that were more symmetrical than those of patients without biofeedback retraining. These findings suggest that appropriate rehabilitation can positively alter joint biomechanics in a way that may contribute to the integrity of the prosthesis and ipsilateral joints.
Several limitations must be considered when interpreting these findings. First, the data provided are limited to only 10 weeks of follow-up after TKA. Although this was the first patient to complete the protocol and her results were promising, a larger group of patients must be followed for a longer period to make conclusive statements about the long-term benefit of this program for function and joint preservation of the nonoperated limb. In addition, this study protocol required an additional 30 minutes of treatment time at each visit, which may be an unreasonable burden on clinical therapy resources. Although commercially available, the equipment used to provide biofeedback during rehabilitation may limit the ability of some clinics to implement this protocol. Further work is needed to evaluate whether similar movement patterns can be achieved with a condensed rehabilitation protocol and whether some components of the rehabilitation protocol can be completed at home or in an unsupervised environment. This program will continue to be refined after feedback from clinicians and the functional and biomechanical results from a larger sample of patients.
In summary, after completing a postoperative rehabilitation protocol that focused on retraining symmetrical movement patterns and progressive strengthening, the patient in this case report walked with knee biomechanics that more closely resembled normal gait compared to a group of patients who underwent a more traditional rehabilitation program. Our patient walked with greater symmetry between limbs and reduced excessive loads on the nonoperated limb, thereby avoiding reliance on other joints of the lower limb during dynamic activities. This protocol did not have any negative implications for functional performance, strength, or range of motion, and future research that fully evaluates biofeedback retraining as an adjunct to traditional rehabilitation may provide clinicians with an optimal rehabilitation strategy to manage persistent impairments after TKA. This rehabilitation strategy offers a novel method of providing visual feedback to the patient during functional and strengthening exercises. Although we report the potential benefits of this protocol for a patient after TKA, it is possible that similar strategies may be beneficial for patients being treated for a wide variety of orthopaedic and neurological disorders for which functional impairments can be attributed to asymmetrical movement patterns.
Acknowledgments
This study was completed with the assistance of funding from the National Institutes of Health P20RR16458 grant. This study was approved by the University of Delaware’s Human Subjects Review Board.
APPENDIX
INTERVENTION PROTOCOL
Stage 1 (Typically Visits 1–6, Weeks 3–6 Post-TKA)
| Focus of Treatment | Treatment | Milestones |
|---|---|---|
| ROM |
|
|
| NMES |
|
|
| Volitional strength |
|
|
| Gait retraining |
|
|
| SymSlide | Exercise 1: Targets. Patient uses body weight to move a ball on the screen into a box
|
|
| Standing balance |
|
|
Stage 2 (Typically Visits 7–12, Weeks 5–8 Post-TKA)
| Focus of Treatment | Treatment | Milestones |
|---|---|---|
| ROM |
|
Consistent with carryover of AROM 0° to greater than 115° |
| NMES |
|
|
| Volitional strength |
|
|
| Gait retraining |
|
|
| Sit-to-stand |
|
|
| Squats on balance board |
|
|
| Stair ascent |
|
|
| Stair descent |
|
|
Stage 3 (Typically Visits 13–18; Weeks 7–10 Post-TKA)
| Focus of Treatment | Treatment | Milestones |
|---|---|---|
| ROM |
|
|
| NMES |
|
|
| Volitional strength |
|
|
| Sit-to-stand |
|
|
| Stair ascent |
|
|
| Stair descent |
|
|
Abbreviations: AROM, active range of motion; MVIC, maximum voluntary isometric contraction; NMES, neuromuscular electrical stimulation; PROM, passive range of motion; RM, repetition maximum; ROM, range of motion; SAQ, short-arc quads; SLR, straight leg raise; TKA, total knee arthroplasty.
Notes:
Pain and swelling: ice, compression, and elevation daily after exercises.
Incision mobility: soft tissue mobilizations to entire length of incision, with greater emphasis on the distal third of incision until incision moves freely over subcutaneous tissue.
Vital signs: monitored during each session.
NMES protocol guidelines: electrodes placed over proximal lateral quadriceps and distal medial quadriceps. Parameters: 2500 Hz; 75 bursts; 2-second ramp; 12 seconds on, 50 seconds off; intensity to maximum tolerable or at least 30% of the MVIC; 10 contractions per session; 3 sessions per week until quadriceps strength MVIC is 70% of uninvolved limb. Performed isometrically at 60° of knee flexion.
References
- 1.Alnahdi AH, Zeni JA, Snyder-Mackler L. Gait after unilateral total knee arthroplasty: frontal plane analysis. J Orthop Res. 2011;29:647–652. doi: 10.1002/jor.21323. http://dx.doi.org/10.1002/jor.21323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Coulter CL, Weber JM, Scarvell JM. Group physiotherapy provides similar outcomes for participants after joint replacement surgery as 1-to-1 physiotherapy: a sequential cohort study. Arch Phys Med Rehabil. 2009;90:1727–1733. doi: 10.1016/j.apmr.2009.04.019. http://dx.doi.org/10.1016/j.apmr.2009.04.019. [DOI] [PubMed] [Google Scholar]
- 3.Farquhar S, Snyder-Mackler L. The Chitranjan Ranawat Award: The nonoperated knee predicts function 3 years after unilateral total knee arthroplasty. Clin Orthop Relat Res. 2009;468:37–44. doi: 10.1007/s11999-009-0892-9. http://dx.doi.org/10.1007/s11999-009-0892-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fisher NM, Pendergast DR. Reduced muscle function in patients with osteoarthritis. Scand J Rehabil Med. 1997;29:213–221. [PubMed] [Google Scholar]
- 5.Kauppila AM, Kyllonen E, Ohtonen P, et al. Multidisciplinary rehabilitation after primary total knee arthroplasty: a randomized controlled study of its effects on functional capacity and quality of life. Clin Rehabil. 2010;24:398–411. doi: 10.1177/0269215509346089. http://dx.doi.org/10.1177/0269215509346089. [DOI] [PubMed] [Google Scholar]
- 6.Mandeville D, Osternig LR, Chou LS. The effect of total knee replacement on dynamic support of the body during walking and stair ascent. Clin Biomech (Bristol, Avon) 2007;22:787–794. doi: 10.1016/j.clinbiomech.2007.04.002. http://dx.doi.org/10.1016/j.clinbiomech.2007.04.002. [DOI] [PubMed] [Google Scholar]
- 7.Milner CE, O’Bryan ME. Bilateral frontal plane mechanics after unilateral total knee arthroplasty. Arch Phys Med Rehabil. 2008;89:1965–1969. doi: 10.1016/j.apmr.2008.02.034. http://dx.doi.org/10.1016/j.apmr.2008.02.034. [DOI] [PubMed] [Google Scholar]
- 8.Mizner RL, Petterson SC, Clements KE, Zeni JA, Jr, Irrgang JJ, Snyder-Mackler L. Measuring functional improvement after total knee arthroplasty requires both performance-based and patient-report assessments: a longitudinal analysis of outcomes. J Arthroplasty. 2010;26:728–737. doi: 10.1016/j.arth.2010.06.004. http://dx.doi.org/10.1016/j.arth.2010.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mizner RL, Petterson SC, Snyder-Mackler L. Quadriceps strength and the time course of functional recovery after total knee arthroplasty. J Orthop Sports Phys Ther. 2005;35:424–436. doi: 10.2519/jospt.2005.35.7.424. http://dx.doi.org/10.2519/jospt.2005.2036. [DOI] [PubMed] [Google Scholar]
- 10.Mizner RL, Snyder-Mackler L. Altered loading during walking and sit-to-stand is affected by quadriceps weakness after total knee arthroplasty. J Orthop Res. 2005;23:1083–1090. doi: 10.1016/j.orthres.2005.01.021. http://dx.doi.org/10.1016/j.orthres.2005.01.021. [DOI] [PubMed] [Google Scholar]
- 11.National Institutes of Health. NIH Consensus Statement on total knee replacement. NIH Consens State Sci Statements. 2003;20:1–34. [PubMed] [Google Scholar]
- 12.Petterson SC, Mizner RL, Stevens JE, et al. Improved function from progressive strengthening interventions after total knee arthroplasty: a randomized clinical trial with an imbedded prospective cohort. Arthritis Rheum. 2009;61:174–183. doi: 10.1002/art.24167. http://dx.doi.org/10.1002/art.24167. [DOI] [PubMed] [Google Scholar]
- 13.Ritter MA, Carr KD, Keating EM, Faris PM. Long-term outcomes of contralateral knees after unilateral total knee arthroplasty for osteoarthritis. J Arthroplasty. 1994;9:347–349. doi: 10.1016/0883-5403(94)90043-4. [DOI] [PubMed] [Google Scholar]
- 14.Walsh M, Woodhouse LJ, Thomas SG, Finch E. Physical impairments and functional limitations: a comparison of individuals 1 year after total knee arthroplasty with control subjects. Phys Ther. 1998;78:248–258. doi: 10.1093/ptj/78.3.248. [DOI] [PubMed] [Google Scholar]
- 15.Yoshida Y, Mizner RL, Ramsey DK, Snyder-Mackler L. Examining outcomes from total knee arthroplasty and the relationship between quadriceps strength and knee function over time. Clin Biomech (Bristol, Avon) 2008;23:320–328. doi: 10.1016/j.clinbiomech.2007.10.008. http://dx.doi.org/10.1016/j.clinbiomech.2007.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zeni JA, Jr, Higginson JS. Differences in gait parameters between healthy subjects and persons with moderate and severe knee osteoarthritis: a result of altered walking speed? Clin Biomech (Bristol, Avon) 2009;24:372–378. doi: 10.1016/j.clinbiomech.2009.02.001. http://dx.doi.org/10.1016/j.clinbiomech.2009.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zeni JA, Jr, Snyder-Mackler L. Early postoperative measures predict 1- and 2-year outcomes after unilateral total knee arthroplasty: importance of contralateral limb strength. Phys Ther. 2010;90:43–54. doi: 10.2522/ptj.20090089. http://dx.doi.org/10.2522/ptj.20090089. [DOI] [PMC free article] [PubMed] [Google Scholar]