Abstract
Aim
Determine the impact of backboard placement, torso weight and bed compression on chest compression (CC) depth feedback in simulated cardiac arrest patients.
Methods
Epochs of 50 high quality CCs with real-time feedback of sternum-to-spine compression depth were provided by a blinded BLS/ACLS/PALS certified provider on manikins of two torso weights (25 vs. 50 kg), using three bed surfaces (stretcher, Stryker hospital bed with Impression mattress, soft Total Care ICU bed), with/without a backboard (BB). Two BB sizes were tested (small: 60 cm × 50 cm; large: 89 cm × 50 cm) in vertical vs. horizontal orientation. Mattress displacement was measured using an accelerometer placed internally on the spine plate of the manikin. Mattress displacement of ≥5 mm was prospectively defined as the minimal clinically important difference.
Results
During CPR (CC depth: 51.8 ± 2.8 mm), BB use significantly reduced mattress displacement only for soft ICU beds. Mattress displacement was reduced (vs. no BB) for 25 kg torso weight: small BB12.3 mm (95%CI 11.9–12.6), horizontally oriented large BB 11.2 mm (95%CI 10.8–11.7), and vertically oriented large BB 12.2 mm (95%CI 11.8–12.6), and for 50 kg torso weight: small BB 7.4 mm (95%CI 7.1–7.8), horizontally oriented large BB 7.9 mm (95%CI 7.6–8.3), and vertically oriented large BB 6.2 mm (95%CI 5.8–6.5; all p < 0.001). BB size and orientation did not significantly affect mattress displacement. Lighter torso weight was associated with larger displacement in soft ICU beds without BB (difference: 6.9 mm, p < 0.001).
Conclusion
BB is important for CPR when performed on soft surfaces, such as ICU beds, especially when torso weight is light. BB may not be needed on stretchers, relatively firm hospital beds, or for patients with heavy torso weights.
Keywords: Backboard, CPR, Resuscitation, Child, Mattress, Displacement
1. Introduction
Best estimates suggest pediatric cardiac arrest occurs in about 16,000 children each year, with about half of cardiac arrests inhospital.1,2 High quality CPR has repeatedly been associated with improved patient outcomes.3–5
Chest compressions (CCs) provided for children during inhospital cardiac arrest are typically performed on soft surfaces such as ICU beds, and less frequently on firm hospital beds or firm transport stretchers.6,7 Traditionally, clinicians have placed a backboard under the patient to minimize the mattress displacement to provide more effective CC and decrease work of CC delivery. However, recently published evidence-based resuscitation guidelines recommend an optional use of backboards, due to a lack of evidence to support or refute backboard effectiveness to improve quality of CPR.8,9
Our previous study using forensic reconstruction techniques demonstrated substantial movement (displacement) in supporting systems (mattress and bed) during actual CCs. 7 However, very few studies evaluate the effectiveness of the backboard directly, and the results are inconclusive.10–17 An important reason the prior results are inconclusive is that the quality of CC is often not optimized in these experiments.11
CPR feedback and coaching devices to guide CC providers have become more available over the last a few years.18 However, devices that coach based upon sternal movement may overestimate the patient’s sternum-to-spine CC depth due to the mattress displacement, and potentially result in shallower CCs and worse patient outcomes.14 Smarter CPR feedback devices are on the horizon to correct those errors and minimize this overestimation by compensating for mattress displacement or accurately measuring actual sternum-to-spine CC depth. Therefore, we attempted to replicate high quality CPR with accurate 2010 guideline compliant sternum-to-spine depth feedback to evaluate the effectiveness of backboard use on a variety of hospital bed surfaces.
Our objective for this study was to evaluate the impact of backboard placement, torso weight, and bed/mattress displacement on anterior sternal movement based CC depth in simulated in-hospital cardiac arrest patients. We hypothesized that: (1) the backboard use would reduce displacement of the supporting system ≥ 5 mm (i.e., firm stretcher, hospital bed with firm mattress, soft ICU bed) and (2) the effectiveness of a backboard to reduce mattress displacement would be affected by bed surface stiffness, torso weight, and backboard orientation (horizontal vs. vertical).
2. Methods
The study protocol was approved by the institutional review board at The Children’s Hospital of Philadelphia.
2.1. Setting
Simulated CPR settings were generated controlling for (1) Manikin characteristics, (2) Torso weight, (3) bed surface stiffness, (4) backboard size, and (5) backboard orientation.
A Voice Advisory Manikin with Skill Reporter System (Laerdal, Wappinger Falls, NY, USA) was used as a testing manikin. The internal displacement sensor reported the manikin anterior sternum-to-spine compression depth for every CC. A Heart-start 4000 (Philips Medical Systems, Andover, MA, USA) monitor/defibrillator equipped with a force and displacement sensor (FDS) placed on top of the manikin’s sternum was used to collect total compression depth. The monitor/defibrillator records data on CC quality (CC rate/min, depth (mm), force (kg). Two different weights, cut to the shape of the manikin torso were placed underneath the manikin on the backboard to adjust the torso weight to 25 kg and 50 kg, representing a child and adult torso, respectively. Our previous studies have shown that the stiffness of the child and elderly adult chests during CPR are similar,19 thus justifying the use of the same manikin stiffness (i.e., spring stiffness) to represent elderly adult and child, and change only the manikin torso mass.
Three different bed surfaces were used to evaluate the effect of backboard placement on displacement of the mattress during CCs: (1) firm stretcher: Steris Hausted Horizon (thickness 6 cm; Steris Corp, Mentor, OH); (2) firm hospital bed: Stryker bed with Impression mattress (thickness: 13 cm; Stryker Medical, Portage, MI, USA), and (3) standard soft ICU bed: Total Care Bed with a therapy mattress (thickness: 14 cm; Hill Rom Corp, Batesville, IN, USA). Two different size backboards were assessed: (1) small backboard (Small backboard: 59 cm × 50.5 cm × 1 cm, weight 3.5 kg) which is currently used in our hospital and (2) a large backboard (Large backboard: 88.7 cm × 50.5 cm × 1 cm, weight 5 kg).
2.2. Design
A single American Heart Association Basic Life Support, Advanced Cardiac Life Support, and Pediatric Advanced Life Support certified provider experienced in adult and pediatric resuscitation performed CCs. Real-time sternum-to-spine CC depth feedback from the Voice Advisory Manikin with Skill Reporter System was used to guide high quality 2010 guideline compliant CC. Chest compressions were targeted using real-time feedback to achieve 50 mm depth with a rate of 100/min and complete release between CCs. The provider was blinded to the presence, size and orientation of the backboard. Specifically, each backboard condition was prepared by separate investigators without the provider present, and the bed surface was covered by white sheets. The CC provider focused on the real-time feedback displayed on the computer screen that was at eye height level across the bed. Fifty consecutive CCs were performed in each setting. A step stool was utilized as needed to achieve real-time feedback-guided CC goals.
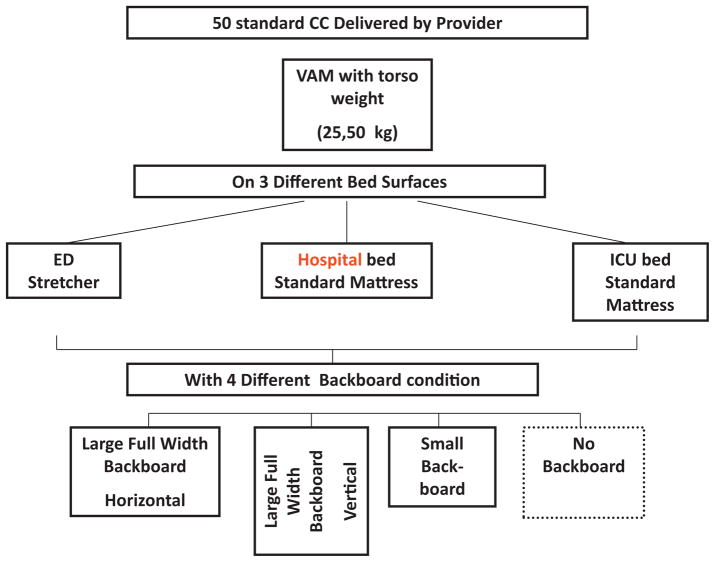
To evaluate the effect of backboard presence, size and orientation, a total of 24 conditions were evaluated based on the possible combinations of two different torso weights (25 and 50 kg), three bed types (firm stretcher, firm hospital bed, soft ICU bed), and four different backboard conditions (no backboard, small backboard, large backboard in horizontal position, large backboard in vertical position) [Fig. 1].
Fig. 1.
Study design CC denotes chest compressions. ED denotes Emergency Department. VAM: Voice Advisory Manikin (Laerdal, Wappinger Falls, NY, USA) Large backboard: 88.7 cm × 50.5 cm × 1 cm, weight 5 kg Small backboard: 59 cm × 50.5 cm × 1 cm, weight 3.5 kg ED Stretcher: Steris Hausted Horizon (Steris Corp, Mentor, OH, USA) Hospital bed: Stryker bed with Impression mattress (thickness: 13 cm) (Stryker Medical, Portage, MI Standard ICU bed: Total Care Bed with a therapy mattress (thickness: 14 cm) (Hill Rom Corp, Batesville, IN, USA).
2.3. Measurement
Mattress displacement was directly measured by an accelerometer placed on the spine plate inside the manikin torso. This method was previously published to measure the mattress displacement during simulated CCs.7 Our measurement of mattress displacement was performed by accelerometer-based measures with an error range of 3 mm.7,19–22 The mattress displacement for each CC was calculated by double integration from the accelerometer measurement. The CC depth measures were recorded and stored in the Heart-start 4000 defibrillator and Voice Advisory Manikin (VAM) with Skill Reporter System.
2.4. Statistical analysis
Our primary outcome measures are the difference in mattress displacement during CCs with or without backboards. The mattress displacement and chest compression data were extracted to an Excel spreadsheet (Microsoft Corp, Redmond, WA, USA). Summary data were reported as mean ± standard deviation (sd). An independent t-test was used for univariate analysis. The effect of backboard was reported as the reduction in mattress displacement. We prospectively defined ≥5 mm reduction in mattress displacement as a minimally clinically important difference from the existing literature.4,23 An estimated mean with 95% confidence interval (CI) was reported for the difference between testing conditions. A two-sided test with alpha = 0.05. STATA 11.0 (Stata Corporation, College Station, TX, USA) was used throughout.
3. Results
A total of 24 conditions with 1191 CCs were analyzed. High quality CCs guided by real-time sternum-to-spine feedback were delivered with mean depth 51.8 ± 2.8 mm and mean force 42.8 ± 4.9 kg. Table 1 demonstrates the delivered CC force and sternum-to-spine depth as well as the measured mattress displacement under various conditions.
Table 1.
Chest compression force, Sternum-to-Spine depth, and mattress displacement.
| Surface/Bed | Torso weight | BB condition | Force (kg) | Sternum-to-Spine depth (mm) | Mattress displacement (mm) |
|---|---|---|---|---|---|
| Stretcher | 25 kg | No BB | 51.0 ± 1.8 | 52.9 ± 1.7 | 16.0 ± 1.0 |
| Standard BB | 48.7 ± 1.3 | 52.5 ± 1.4 | 11.2 ± 0.4 | ||
| Large BB Horizontal | 44.2 ± 2.1 | 52.9 ± 2.3 | 13.2 ± 0.8 | ||
| Large BB Vertical | 34.3 ± 1.7 | 52.9 ± 2.1 | 5.0 ± 0.5 | ||
| 50 kg | No BB | 48.6 ± 2.6 | 55.4 ± 2.4 | 10.8 ± 0.7 | |
| Standard BB | 46.8 ± 1.9 | 52.5 ± 2.3 | 11.3 ± 0.4 | ||
| Large BB Horizontal | 38.0 ± 2.4 | 55.0 ± 2.6 | 9.9 ± 0.5 | ||
| Large BB Vertical | 48.7 ± 2.5 | 52.1 ± 2.9 | 9.6 ± 0.4 | ||
| Hospital Bed | 25 kg | No BB | 36.7 ± 2.9 | 45.1 ± 2.2 | 13.0 ± 0.8 |
| Standard BB | 43.5 ± 1.7 | 51.1 ± 1.6 | 10.2 ± 0.5 | ||
| Large BB Horizontal | 35.4 ± 1.2 | 49.5 ± 1.4 | 11.8 ± 0.4 | ||
| Large BB Vertical | 46.6 ± 1.9 | 50.6 ± 1.8 | 11.1 ± 0.4 | ||
| 50 kg | No BB | 37.5 ± 1.4 | 52.6 ± 1.8 | 10.2 ± 0.7 | |
| Standard BB | 37.2 ± 2.5 | 50.7 ± 3.4 | 8.9 ± 0.7 | ||
| Large BB Horizontal | 44.3 ± 1.5 | 50.1 ± 1.5 | 11.3 ± 0.4 | ||
| Large BB Vertical | 44.0 ± 1.1 | 51.8 ± 1.3 | 9.4 ± 0.3 | ||
| ICU Bed | 25 kg | No BB | 38.2 ± 1.8 | 53.4 ± 1.8 | 28.4 ± 1.2 |
| Standard BB | 41.3 ± 1.1 | 49.7 ± 1.2 | 16.1 ± 0.6 | ||
| Large BB Horizontal | 43.2 ± 1.3 | 52.6 ± 1.5 | 17.2 ± 1.0 | ||
| Large BB Vertical | 44.6 ± 1.7 | 52.4 ± 1.8 | 16.2 ± 0.7 | ||
| 50 kg | No BB | 43.0 ± 1.4 | 51.2 ± 1.5 | 21.5 ± 1.0 | |
| Standard BB | 40.7 ± 2.2 | 50.5 ± 2.0 | 14.1 ± 0.9 | ||
| Large BB Horizontal | 44.6 ± 1.1 | 52.2 ± 1.5 | 13.6 ± 0.6 | ||
| Large BB Vertical | 45.4 ± 1.6 | 53.0 ± 1.7 | 15.3 ± 0.8 |
Mean ± standard deviation. Stretcher: Steris Hausted Horizon (Steris Corp, Mentor, OH, USA). Hospital Bed: Stryker bed with Impression mattress (thickness: 13 cm) (Stryker Medical, Portage, MI, USA). ICU Bed: Total Care Bed with a therapy mattress (thickness: 14 cm) (Hill Rom Corp, Batesville, IN, USA).
3.1. Effectiveness of backboard placement
Backboard use reduced the mattress displacement significantly (i.e. ≥5 mm) only in soft ICU beds for 25 kg and 50 kg torso weight and in the 25 kg patient on a firm stretcher (Table 2). Reduction in mattress displacement for the 25 kg torso weight on the soft ICU bed was 12.3 mm (95% CI 11.9–12.6 mm) with a small backboard, 11.2 mm (95% CI 10.8–11.7 mm) with a horizontally placed large backboard, and 12.2 mm (95% CI 11.8–12.6 mm) with a vertically placed large backboard (p < 0.001 for all comparisons). Reduction in mattress displacement for the 50 kg torso weight on the soft ICU bed was: small backboard 7.4 mm (95% CI 7.1–7.8 mm, p < 0.001), horizontally placed large backboard 7.9 mm (95% CI 7.6–8.3 mm, p < 0.001) and vertically placed large backboard 6.2 mm (95% CI 5.8–6.5 mm, p < 0.001). Reduction in mattress displacement for the 25 kg torso weight on the firm stretcher was 10.9 mm (95% CI 10.6–11.2 mm, p < 0.001) with the backboard placed vertically.
Table 2.
Mattress displacement during CPR (mm).
| Surface/bed | Torso weight (kg) | No BB (mm ± SD) | Decrease in mattress displacement compared to No BB (mm, 95%CI)
|
||
|---|---|---|---|---|---|
| Standard BB | Large BB Horizontal | Large BB Vertical | |||
| Stretcher | 25 | 16.0 ± 1.0 | 4.7 (4.4, 5.0) | 2.8 (2.4, 3.1) | 10.9 (10.6, 11.2)* |
| Stretcher | 50 | 10.8 ± 0.7 | −0.4 (−0.7, −0.2) | 1.0 (0.7, 1.2) | 1.2 (1.0, 1.4) |
| Hosp Bed | 25 | 13.0 ± 0.8 | 2.9 (2.6, 3.1) | 1.2 (1.0, 1.5) | 1.9 (1.7, 2.2) |
| Hosp Bed | 50 | 10.2 ± 0.7 | 1.3 (1.0, 1.6) | −1.1 (−0.9, −1.3) | 0.8 (0.6, 1.0) |
| ICU Bed | 25 | 28.4 ± 1.2 | 12.3 (11.9, 12.6)* | 11.2 (10.8, 11.7)* | 12.2 (11.8, 12.6)* |
| ICU Bed | 50 | 21.5 ± 1.0 | 7.4 (7.1, 7.8)* | 7.9 (7.6, 8.3)* | 6.2 (5.8, 6.5)* |
CI denotes confidence interval. Stretcher: Steris Hausted Horizon (Steris Corp, Mentor, OH, USA) Hosp Bed: Stryker bed with Impression mattress (thickness: 13 cm) (Stryker Medical, Portage, MI, USA) ICU Bed: Total Care Bed with a therapy mattress (thickness: 14 cm) (Hill Rom Corp, Batesville, IN, USA).
p < 0.05 for >5 mm difference compared to no backboard.
3.2. Effect of backboard size and orientation
The size and orientation of backboard did not significantly affect mattress displacement except in the condition utilizing a vertically placed large backboard on a firm stretcher with 25 kg torso weight (difference between small vs. vertically placed backboard, 6.2 mm [95% CI 6.0–6.4 mm, p < 0.001], between horizontally placed large backboard vs. vertically placed large backboard, 8.2 mm [95% CI 7.8–8.4 mm, p < 0.001]). The difference was not significant for the 50 kg torso weight (difference between small vs. vertically placed large backboard, 1.6 mm [95% CI 1.5–1.8 mm, p > 0.99], between horizontally placed large backboard vs. vertically placed large backboard, 0.2 mm [95% CI 0.0–0.4 mm, p > 0.99]).
3.3. Effect of torso weight
Overall, lighter torso weight (25 kg) was associated with larger mattress displacement in all bed/backboard conditions. This, however, became significant only in CCs delivered on a soft ICU bed without backboard (difference 6.9 mm, 95% CI: 6.4–7.3 mm, p < 0.001).
4. Discussion
Use of a backboard during in-hospital CPR is traditionally recommended to improve the quality of CC depth. 24 However, few studies have evaluated the effect of the backboard size and orientation, and the results are conflicting, which led to an inconclusive statement in the current resuscitation consensus and guidelines.8,9 In this study, we evaluated the effectiveness of various backboards to decrease the mattress displacement under realistic and varying realistic clinical conditions. Real-time sternum-to-spine depth feedback to the CPR provider was used to maintain high quality CC, regardless of bed surface. In order to avoid “statistically significant but not clinically important” results, we a priori defined the minimal clinically important difference in mattress displacement as ≥5 mm, based on previous clinical investigations (i.e., how much depth loss in the mattress would affect patient outcome).4,23
Our study results were somewhat surprising. Use of backboards did not significantly reduce the mattress displacement during CPR on firm stretchers or firm standard hospital beds, except on a stretcher with a lightly weighted torso when the large backboard was oriented vertically. On soft ICU beds, however, the backboard induced reduction in mattress displacement was >5 mm in all conditions, and ≥10 mm when the torso weight was light (25 kg). This suggests that backboards should be used for CPR events in pediatric and adult ICUs where the majority of patients are in soft ICU beds. The finding is intuitive if we acknowledge that lighter torso weights sink less into soft bed mattresses and thus have more potential for mattress displacement during CCs. Heavier torso weights cause the torso to sink into the mattress even when the CC force is released completely (i.e. no leaning), therefore leaving less potential for mattress displacement during chest compression.
Compared to our previously reported clinical study in older children on similar mattress surfaces and backboard positions, our study demonstrated a larger bed surface displacement.7 This difference is likely due to deeper sternum-to-spine CC depth targets with new 2010 International Liaison Committee on Resuscitation (ILCOR) guidelines (increasing from ≥38 mm to >50 mm), and delivery of more forceful CC.
Boe and Babbs previously evaluated the effect of the bed surface and backboard use applying a sophisticated mathematical model.25 In their study, the force of compression was held constant at 400 Newton (40.8 kg), described as a constant peak force technique. Interestingly, our findings of the 20% increase in total compression when a backboard is not placed are similar to the 15% decrease in sternum-to-spine compression distance that was reported by Boe and Babbs on a typical stiff hospital mattress without a backboard.
Our study results are different from other published studies, and fill in gaps that will inform future guidelines (see Table 3). One previous study with a similar design (targeting an internal sternum-to-spine compression depth) demonstrated a much larger effect of backboard presence to reduce CPR provider’s hand movement (i.e., to reduce mattress displacement).15 Reduction of mattress displacement at 50 mm CC depth target was approximately 45 mm. This study, however, did not add weight to the torso when CCs were provided without the backboard, which explains this large mattress displacement. Furthermore, torso weight was added only when CC were performed on the backboard. This probably led to an overestimation of the backboard effectiveness.
Table 3.
Key studies reporting backboard effectiveness.
| Author Year | Study design | Backboard condition | Bed condition | Torso weight | Quality of CC (Sternum-to-spine depth) | Measures | Result | Conclusion | Difference from current study |
|---|---|---|---|---|---|---|---|---|---|
| Babbs 199925 | Mathematical model of patient-bed mechanics (a) constant peak-displacement technique (target at a constant sternum movement) and (b) constant peak-force technique (target at a constant CC force) Mechanical compression |
With/Without BB Size: 30 cm × 44 cm | 2 hospital beds × 2 mattress types | Varied (53–110 kg) | Not applicable (mathematical model) | Mechanical elements of support system with/without BB | BB increased overall stiffness and damping of bed-mattress combination | BB and constant force method should be used for CPR | Mathematical model Single BB size No actual CC depth measured Stretcher not evaluated |
| Tweed 200112 | Randomized cross-over trial with various support surfaces (floor, foam, overlay with/without inflation, alternating pressure with/without inflation, low-air-loss with/without inflation) 4 BLS providers without feedback system Unblinded |
No BB used | Various surfaces floor foam overlay with/without inflation alternating pressure with/without inflation low-air-loss with/without inflation | 40 kg | 33–42 mm | Sternum-to- spine depth | Soft surfaces were associated with shallower CC depth | Soft surfaces were associated with shallower CC depth | BB not used Unblinded No feedback system used Quality of CC poor even based on 2005 ILCOR guidelines |
| Perkins 200611 | Randomized cross-over trial with or without BB 20 medical students with BLS instructor status No feedback system Unblinded |
With/Without BB Size: not reported | Standard hospital bed with foam mattress on top | Not reported | 29 mm without BB 31 mm with BB |
Sternum-to- spine depth | BB did not increase CC depth | BB did not increase depth when CCs are shallow | Unblinded Quality of CC poor even based on 2005 ILCOR guidelines Single bed condition |
| Andersen 200710 | Randomized cross-over trial with or without BB 23 hospital orderlies No feedback system Blinded |
With/Without BB Size: 44 cm × 58 cm × 1 cm | Hospital bed with foam mattress on top | Not reported | 43 mm without BB 48 mm with BB |
Sternum-to-spine depth | BB increased the depth by 5 mm Proportion of CC with depth > 40 mm: 92% with BB, 69% without BB | BB is recommended on hospital beds | Quality of CC shallow due to old (2005) ILCOR guidelines Single bed condition |
| Noorder-graaf 200915 | CC with targeted sternum-to-spine depth at 30, 40, 50, 60 mm A provider with potentiometer feedback of sternum-to-spine depth |
With/Without BB Size: 80 cm × 30 cm | Three hospital beds (foam and air mattress) and stretcher | 20 kg, 40 kg (no weight when no BB used) | Standardized at 30, 40, 50, 60 mm with error ±2 mm | Net movement of sternal surface | BB decreased net sternal movement by 45 mm without weight, 41 mm with 20 kg, 40 mm with 40 kg weight on soft bed at 50 mm target sternum-to-spine depth | BB is recommended to reduce hand movement and work by CPR providers | No BB orientation evaluated Single BB size No weight added when BB was not used |
| Perkins 200914 | CC with targeted depth with two feedback systems: Sternal accelerometer model Sternum-to-spine depth model A provider with feedback Unblinded |
3 BB conditions: no BB Narrow 45.7 cm × 182.6 cm × 3.7 cm Wide 63.5 cm × 150.9 cm × 0.4 cm |
3 surfaces Floor Foam on a bed Inflatable mattress on bed |
70 kg | Shallow CC with sternal accelerometer feedback (26–32 mm on mattress) Deep CC with sternum-to-spine depth feedback (40–50 mm) |
Sternum-to- spine depth for Sternal accelerometer feedback model % mattress compression of total compression for Sternum-to- spine depth model | BB increased CC depth (Narrow: 1.9 mm, wide: 2.6 mm) in Sternal accelerometer feedback model BB decreased % mattress compression to total (narrow: 4.7%, wide: 6.6%) in sternum-to-spine feedback model |
BB reduces the amount of mattress compression and work from CPR provider | Quality of CC shallow due to old (2005) ILCOR guidelines Unblinded Heavier torso weight used |
| Jantti 200927 | CC without feedback under two conditions: floor vs. hospital bed without BB Experienced ICU Nurses Unblinded Provider kneeled next to torso No feedback system |
No BB | 2 surfaces (floor, standard hospital bed) with 10 cm foam mattress | 21 kg | Floor: 45 mm Hospital bed: 43 mm |
Sternum-to- spine depth | No difference in CC depth between two conditions CC depth decline overtime did not vary among two conditions | When experienced CPR provider perform CCs, no difference in CC depths | No BB Quality of CC shallow due to old (2005) ILCOR guidelines Unblinded No Torso weight |
| Cloete 201116 | CC with targeted sternal movement at 50 mm at various BB conditions Mechanical compression |
6 BB conditions: no BB large BB 86 cm × 56 cm × 1.2 cm small BB 56 cm × 43 cm × 1.1 cm 2 BB orientations: long and lateral |
2 mattresses | 75 kg | 20–29 mm without BB 31–47 mm with BB |
Sternum-to-spine depth | BB increased CC depth by at least 10 mm Large BB is more effective to increase CC depth compared to small BB (difference: 1–15 mm) BB orientation effect was small (1–3 mm) |
When net sternal movement is constant, BB increase sternum-to-spine depth Large BB is more effective Effect of BB orientation variable |
Quality of CC shallow due to study design (net sternal depth targeted at 50 mm) |
| Sato 201117 | CCs on operating table with or without BB Unblinded Physicians providers with some CPR experience No feedback system |
BB: 1 cm thickness | 1 surface operating bed with 6 cm thickness mattress | No torso weight | 49 mm without BB 54 mm with BB |
Sternum-to- spine depth | BB increased CC depth by 5 mm, also increased proportion of CCs with depth>50 mm (54% to 82%) | BB increase the CC depth and proportion of CCs with depth>50 mm | No torso weight A single bed condition Unblinded No feedback system |
| Nishisaki 2012 (Current Study) | CC with targeted sternum-to-spine depth at 50 mm, with or without BB Single with BLS/PALS/ACLS Feedback with sternum-to-spine depth Blinded 5 mm as minimally clinically important difference |
4 BB conditions No BB Large horizontal Large vertical Small Large BB: 88.7 cm × 50.5 cm × 1 cm Small BB: 59 cm × 50.5 cm × 1 cm |
3 surfaces Stretcher Hospital bed ICU bed |
25 kg, 50 kg | Standardized at 50 mm (measured 52 mm) | Movement of supporting surface | BB reduced mattress displacement only in soft ICU bed Reduction of mattress displacement: 11–12 mm in 25 kg Torso, 6–7 mm in 50 kg Torso) BB size and orientation did not affect mattress displacement | BB should be used for CCs on light torso weight on soft surfaces BBs may not be needed for large torso weight on firm support (stretcher, hospital bed) | Not applicable |
CC denotes chest compressions. BB denotes backboard. ILCOR denotes International Liaison Committee on Resuscitation.
Perkins et al. reported the effectiveness of a backboard to reduce soft and hard hospital mattress displacement, using a model with CC feedback based on sternum-to-spine compression depth, similar to what we used in our study.14 While mattress displacement accounted for up to 40% of overall sternum movement, their narrow backboard (45.7 cm × 182.6 cm × 3.7 cm) reduced this by 4.7% (95% CI 1.4–8.1%, p < 0.007) and their wide backboard (63.5 cm × 150.9 cm × 0.4 cm) reduced this by 6.6% (95% CI: 3.4–10.0%, p < 0.0001). They concluded that backboard use reduces the mattress compression and therefore the amount of work required from the CPR provider.
They also studied the effect of backboard use on CC depth with a similar VAM on their standard soft hospital bed with foam mattress on top.11 Twenty second-year medical student basic life support instructors were randomized to perform CC guided by a sternum-to-spine depth Voice Advisory Manikin with or without a backboard. Overall CC depth did not meet the current ILCOR guidelines, and they did not find differences between CC with and without backboard (29 ± 7 mm vs. 30 ± 10 mm, p = N.S.). Shallow CC depth performed in this study likely precludes conclusions regarding the effect of the backboard when high quality CPR guided to a 2010 guideline CC depth of >50 mm is provided.
Anderson et al. studied the effect of backboard presence on CC depth using adult manikins on a firm hospital bed without adjustment for a torso weight.10 Twenty-three members of their hospital cardiac arrest team were randomized to perform CPR with or without a small backboard (44 cm × 58 cm) similar to our currently studied small backboard. Subjects were trained and updated on ILCOR 2005 guidelines. They reported the use of backboard improved internal sternum-to-spine measured CC depth from 43 mm to 48 mm (p < 0.0001). This study was conducted without a feedback system and subjects were not blinded to the presence of backboard. A similar result was reported when CC were performed on a CPR manikin on a firm operating room bed with a pressure reduction mattress added on top.17 Our study was different from those studies, quantifying mattress displacement during CCs coached to the deeper 2010 Guideline depth (>50 mm). This suggests that use of an externally placed sternal accelerometer device could potentially underestimate actual sternum-to-spine CC depth and potentially misguide rescuers to achieve shallower CC depth.7,14
Our study did not show completely consistent results regarding the impact of size and orientation of the backboard on mattress displacement. Comparison to a recent prior study16 is difficult, since their study used a target cylinder movement (a net sternal movement) of 50 mm, not the actual sternum-to-spine CC depth of >50 mm, resulting in variable compression force delivery. They reported more sternum-to-spine displacement (i.e. less mattress displacement) when a larger (86 cm × 50 cm) vs. smaller (56 cm × 43 cm) backboard was used on a soft mattress (44 mm vs. 30 mm, p < 0.001). As in our study, this difference was not observed on a harder mattress. They also reported an inconsistent result regarding the effect of horizontal vs. vertical backboard orientation, similar to what we observed in our current study.
5. Limitations
Our results should be interpreted with caution. We acknowledge that our study manikin chest may have different stiffness properties compared to actual humans. This might have led to more forceful CC to achieve the target depth. However, based on recent chest stiffness analyses during real CPR in humans, 43 kg of compression force applied in this study is a reasonable range to achieve a target 50 mm depth.20,21,26 We also acknowledge that the horizontally placed large backboard on a stretcher might have less contact to the bed than the surface of the backboard due to the narrow width of the stretcher. In addition, the CC provider could occasionally ‘guess’ the backboard condition in our experiment, especially for a horizontally placed large backboard. However, as CCs were tightly guided by the sternum-to-spine feedback system and the provided CCs consistently met the preset target, this should not have affected our outcome measures. Despite these limitations, our study provides quantitative data about the impact of backboard placement, torso weight, and bed compression on anterior sternal movement based feedback for CC depth in simulated in-hospital cardiac arrest patients.
6. Conclusions
Backboards should be used for CPR when performed on soft surfaces, such as ICU beds. Backboards may not be needed for CPR on firm stretchers, firm hospital beds, or for patients with heavy torso weights. We evaluated the effect of the backboard presence, size and the orientation in a quantitative manner under various conditions that mimic common clinical situations. We prospectively defined an evidence-based minimally clinically important difference. On soft ICU beds, backboard use was associated with a decrease in mattress displacement as compared to no backboard use. Backboard size and orientation (horizontal vs. vertical) did not have a consistent effect on mattress displacement. Lighter torso weights were associated with larger mattress displacements on soft ICU beds. Future studies should measure the reduction of work and fatigue of CPR providers when backboards are used on soft surfaces, and adequately deep sternum-to-spine high quality CCs are provided.
Acknowledgments
Funding
Laerdal Foundation for Acute Care Medicine and Endowed Chair of Critical Care Medicine at the Children’s Hospital of Philadelphia.
Funding provided by the Endowed Chair of Critical Care Medicine at the Children’s Hospital of Philadelphia and Laerdal Foundation for Acute Care Medicine. We thank Stephanie Tuttle, MBA for her administrative support, Larissa Hutchins APN, RN for arranging beds for testing. Blue Bell Bio-medical, Van Wert, OH supplied the large backboard.
Footnotes
A Spanish translated version of the summary of this article appears as Appendix in the final online version at doi:10.1016/j.resuscitation.2012.01.016.
Conflicts of interest
The authors acknowledge the following potential conflicts of interest. Akira Nishisaki, Dana Niles, Robert Sutton, Matthew R. Maltese and Vinay Nadkarni receive unrestricted research grant support from the Laerdal Foundation for Acute Care Medicine. Robert Sutton is supported through a career development award from the Eunice Kennedy Shriver National Institute of Child Health & Human Development (K23HD062629).
References
- 1.Atkins DL, Everson-Stewart S, Sears GK, et al. Resuscitation Outcomes Consortium Investigators. Epidemiology and outcomes from out-of-hospital cardiac arrest in children: the Resuscitation Outcomes Consortium Epistry-Cardiac Arrest. Circulation. 2009;119:1484–91. doi: 10.1161/CIRCULATIONAHA.108.802678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Topjian AA, Nadkarni VM, Berg RA. Cardiopulmonary resuscitation in children. Curr Opin Crit Care. 2009;15:203–8. doi: 10.1097/mcc.0b013e32832931e1. [DOI] [PubMed] [Google Scholar]
- 3.Abella BS, Sandbo N, Vassilatos P, et al. Chest compression rates during cardiopulmonary resuscitation are suboptimal: a prospective study during inhospital cardiac arrest. Circulation. 2005;111:428–34. doi: 10.1161/01.CIR.0000153811.84257.59. [DOI] [PubMed] [Google Scholar]
- 4.Edelson DP, Abella BS, Kramer-Johansen J, et al. Effects of compression depth and pre-shock pauses predict defibrillation failure during cardiac arrest. Resuscitation. 2006;71:137–45. doi: 10.1016/j.resuscitation.2006.04.008. [DOI] [PubMed] [Google Scholar]
- 5.Kramer-Johansen J, Myklebust H, Wik L, et al. Quality of out-of-hospital cardiopulmonary resuscitation with real time automated feedback: a prospective interventional study. Resuscitation. 2006;71:283–92. doi: 10.1016/j.resuscitation.2006.05.011. [DOI] [PubMed] [Google Scholar]
- 6.Niles D, Nysaether J, Sutton R, et al. Leaning is common during in-hospital pediatric CPR, and decreased with automated corrective feedback. Resuscitation. 2009;80:553–7. doi: 10.1016/j.resuscitation.2009.02.012. [DOI] [PubMed] [Google Scholar]
- 7.Nishisaki A, Nysaether J, Sutton R, et al. Effect of mattress deflection on CPR quality assessment for older children and adolescents. Resuscitation. 2009;80:540–5. doi: 10.1016/j.resuscitation.2009.02.006. [DOI] [PubMed] [Google Scholar]
- 8.Berg RA, Hemphill R, Abella BS, et al. Part 5: adult basic life support: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010;122:S685–705. doi: 10.1161/CIRCULATIONAHA.110.970939. [DOI] [PubMed] [Google Scholar]
- 9.Berg MD, Schexnayder SM, Chameides L, et al. Part 13: pediatric basic life support: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010;122:S862–75. doi: 10.1161/CIRCULATIONAHA.110.971085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Andersen LØ, Isbye DL, Rasmussen LS. Increasing compression depth during manikin CPR using a simple backboard. Acta Anaesthesiol Scand. 2007;51:747–50. doi: 10.1111/j.1399-6576.2007.01304.x. [DOI] [PubMed] [Google Scholar]
- 11.Perkins GD, Smith CM, Augre C, et al. Effects of a backboard, bed height, and operator position on compression depth during simulated resuscitation. Intensive Care Med. 2006;32:1632–5. doi: 10.1007/s00134-006-0273-8. [DOI] [PubMed] [Google Scholar]
- 12.Tweed M, Tweed C, Perkins GD. The effect of differing support surfaces on the efficacy of chest compressions using a resuscitation manikin model. Resuscitation. 2001;51:179–83. doi: 10.1016/s0300-9572(01)00404-x. [DOI] [PubMed] [Google Scholar]
- 13.Perkins GD, Benny R, Giles S, Gao F, Tweed MJ. Do different mattresses affect the quality of cardiopulmonary resuscitation? Intensive Care Med. 2003;29:2330–5. doi: 10.1007/s00134-003-2014-6. [DOI] [PubMed] [Google Scholar]
- 14.Perkins GD, Smith S, McCulloch R, Davies R. Compression feedback devices may under-estimate chest compression depth when performed on a bed. Resuscitation. 2009;80:79–82. doi: 10.1016/j.resuscitation.2008.08.011. [DOI] [PubMed] [Google Scholar]
- 15.Noordergraaf GJ, Paulussen IW, Venema A, et al. The impact of compliant surfaces on in-hospital chest compressions: effects of common mattresses and a backboard. Resuscitation. 2009;80:546–52. doi: 10.1016/j.resuscitation.2009.03.023. [DOI] [PubMed] [Google Scholar]
- 16.Cloete G, Dellimore KH, Scheffer C, Smuts MS, Wallis LA. The impact of backboard size and orientation on sternum-to-spine compression depth and compression stiffness in a manikin study of CPR using two mattress types. Resuscitation. 2011;82:1064–70. doi: 10.1016/j.resuscitation.2011.04.003. [DOI] [PubMed] [Google Scholar]
- 17.Sato H, Komasawa N, Ueki R, et al. Backboard insertion in the operating table increases chest compression depth: a manikin study. J Anesth. 2011 doi: 10.1007/s00540-011-1196-2. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 18.Dine CJ, Gersh RE, Leary M, Riegel BJ, Bellini LM, Abella BS. Improving cardiopulmonary resuscitation quality and resuscitation training by combining audiovisual feedback and debriefing. Crit Care Med. 2008;36:2817–22. doi: 10.1097/CCM.0b013e318186fe37. [DOI] [PubMed] [Google Scholar]
- 19.Maltese MR, Castner T, Niles D, et al. Methods for determining pediatric thoracic force-deflection characteristics from cardiopulmonary resuscitation. Stapp Car Crash J. 2008;52:83–105. doi: 10.4271/2008-22-0004. [DOI] [PubMed] [Google Scholar]
- 20.Maltese MR, Arbogast KB, Nadkarni V, et al. Incorporation of CPR Data into ATD Chest Impact Response Requirements. Ann Adv Automot Med. 2010;54:79–88. [PMC free article] [PubMed] [Google Scholar]
- 21.Arbogast K, Maltese M, Nadkarni V, Steen P, Nysaether J. Anterior-posterior force deflection characteristics measured during cardiopulmonary resuscitation: comparison to post-mortem human subject data. Stapp Car Crash J. 2006;50:131–45. doi: 10.4271/2006-22-0006. [DOI] [PubMed] [Google Scholar]
- 22.Aase SO, Myklebust H. Compression depth estimation for CPR quality assessment using DSP on accelerometer signals. IEEE Trans Biomed Eng. 2002;49:263–8. doi: 10.1109/10.983461. [DOI] [PubMed] [Google Scholar]
- 23.Sutton RM, Nishisaki A, Niles DE, et al. Deep chest compressions ≤ than 50 mm improve hemodynamic outcomes during actual pediatric and adolescent arrest. Crit Care Med. 2010;38:453. [Google Scholar]
- 24.2005 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care, Part 4: Adult Basic Life Support. Circulation. 2005;112:IV-19–34. doi: 10.1161/CIRCULATIONAHA.105.166550. [DOI] [PubMed] [Google Scholar]
- 25.Boe JM, Babbs CF. Mechanics of cardiopulmonary resuscitation performed with the patient on a soft bed vs a hard surface. Acad Emerg Med. 1999;6:754–7. doi: 10.1111/j.1553-2712.1999.tb00449.x. [DOI] [PubMed] [Google Scholar]
- 26.Tomlinson AE, Nysaether J, Kramer-Johansen J, Steen PA, Dorph E. Compression force–depth relationship during out-of-hospital cardiopulmonary resuscitation. Resuscitation. 2007;72:364–70. doi: 10.1016/j.resuscitation.2006.07.017. [DOI] [PubMed] [Google Scholar]
- 27.Jäntti H, Silfvast T, Turpeinen A, Kiviniemi V, Uusaro A. Quality of cardiopulmonary resuscitation on manikins: on the floor and in the bed. Acta Anaesthesiol Scand. 2009;53:1131–7. doi: 10.1111/j.1399-6576.2009.01966.x. [DOI] [PubMed] [Google Scholar]