Abstract
Background
Malaria parasites undergo complex developmental transitions within the mosquito vector. A commonly used laboratory model for studies of mosquito-malaria interaction is the rodent parasite, P. berghei. Anopheles funestus is a major malaria vector in sub-Saharan Africa but has received less attention than the sympatric species, Anopheles gambiae. The imminent completion of the A. funestus genome sequence will provide currently lacking molecular tools to describe malaria parasite interactions in this mosquito, but previous reports suggested that A. funestus is not permissive for P. berghei development.
Methods
An A. funestus population was generated in the laboratory by capturing female wild mosquitoes in Mali, allowing them to oviposit, and rearing the eggs to adults. These F1 progeny of wild mosquitoes were allowed to feed on mice infected with a fluorescent P. berghei strain. Fluorescence microscopy was used to track parasite development inside the mosquito, salivary gland sporozoites were tested for infectivity to mice, and parasite development in A. funestus was compared to A. gambiae.
Results
P. berghei oocysts were detectable on A. funestus midguts by 7 days post-infection. By 18–20 days post-infection, sporozoites had invaded the median and distal lateral lobes of the salivary glands, and hemocoel sporozoites were observed in the hemolymph. Mosquitoes were capable of infecting mice via bite, demonstrating that A. funestus supports the complete life cycle of P. berghei. In a random sample of wild mosquito genotypes, A. funestus prevalence of infection and the characteristics of parasite development were similar to that observed in A. gambiae-P. berghei infections.
Conclusions
The data presented in this study establish an experimental laboratory model for Plasmodium infection of A. funestus, an important vector of human malaria. Studying A. funestus-Plasmodium interactions is now feasible in a laboratory setting. This information lays the groundwork for exploitation of the awaited genome sequence of A. funestus.
Introduction
Close to half of the world's population is at risk of malaria infection [1], [2]. Attempts to curtail disease transmission have focused on the development of drugs to treat infected individuals, insecticide spraying to kill the mosquito vectors, and the use of physical barriers to prevent vector-human contact. Understanding the biology of mosquito-malaria interactions may aid in the development of a new generation of vector-based measures for malaria control.
In sub-Saharan Africa, where greater than 85% of malaria-associated mortality occurs [1], the major Plasmodium vectors are A. gambiae, A. arabiensis, A. funestus, A. nili, and A. moucheti, with heterogeneities in populations occurring both geographically and seasonally [3], [4]. To date, due to practical reasons such as extensive genome information and relative ease of colonization, most studies on mosquito-Plasmodium interactions have focused on the African mosquito, A. gambiae, and the Asian mosquito, A. stephensi. However, A. funestus is a major malaria vector in certain regions of Africa [3], plays a more prominent role than A. gambiae during the dry season [5], and in areas where it co-exists with A. gambiae it has been observed to have higher infection rates [6]. Thus, understanding the vector biology of A. funestus needs to be part of successful malaria control, but currently little is known about this species. Towards this end, we and colleagues recently determined and reported the complete transcriptome sequence of A. funestus using RNA-seq next-generation sequencing technology [7].
When studying mosquito-malaria interactions, model parasite systems are often used because of the ease of manipulation and the laboratory safety afforded by using parasites incapable of infecting humans. One model parasite commonly used is P. berghei, a rodent malaria species originally isolated from the salivary glands of A. dureni and whose vertebrate host in nature is the Central African tree rat, Thamnomys surdaster [8], [9]. P. berghei can be genetically manipulated, and marked transgenic parasites are easily visualized in mosquito and mammalian tissues [10]–[14]. To date, experimental infections have shown that P. berghei is capable of completing its life cycle in A. quadrimaculatus, A. freeborni, A. stephensi, A. annupiles, A. atroparvus, A. maculipennis, and A. gambiae [15]–[21]. A. albimanus, a major malaria vector in South America, is not an efficient laboratory vector of P. berghei [19], [22], and the African mosquito A. quadriannulatus Species A, a member of the A. gambiae species complex, also is not permissive for P. berghei development [23]. Ten other anopheline species have been described as being resistant to P. berghei, including the only published report using A. funestus, which states that P. berghei is unable to infect A. funestus [18], [20]. Here, we show for the first time that P. berghei can indeed infect and complete its life cycle in random natural genotypes of the important African malaria vector A. funestus, and that infection progression proceeds with similar kinetics and efficiency to that observed in A. gambiae.
Methods
Mosquitoes
Wild A. funestus females were collected indoors in the village of Niono, Mali, West Africa. No specific permits were required for the collection of mosquitoes. Mosquitoes were collected inside village houses by agreement of the residents. Because they were captured resting indoors, the captured females, morphologically identified as A. funestus sensu lato, had already mated and taken a bloodmeal in nature. Mosquitoes were housed in an environmental chamber at 26°C and 75% relative humidity. For each experiment approximately 50 wild-fed gravid females were allowed to oviposit collectively. The resulting eggs were grown to adult mosquitoes under standard insectary conditions, including larval food, as used for A. gambiae [12].
Parasites and infection
To determine the permissiveness of A. funestus to P. berghei infection, approximately 200 5–7 day old adult females (raised from wild larvae) were starved overnight and allowed to feed for 30 min on Swiss Webster mice with a parasitemia of approximately 10% and a gametocytemia of approximately 2%. Following blood feeding, unfed mosquitoes were removed and fed mosquitoes were maintained at 20.5°C and 75% relative humidity. Infections were done using the PbGFPCON transgenic strain of P. berghei that constitutively expresses green fluorescent protein (GFP) [10].
This study was carried out in strict accordance with the recommendations in the Guide for the Care and Use of Laboratory Animals of the National Institutes of Health. The protocol was approved by the Institutional Animal Care and Use Committee of the University of Minnesota (Permit Number: 1201A08951, NIH Animal Welfare Assurance number: A3456). All mosquito infections were performed by feeding on mice anesthetized with ketamine/xylazine, and all efforts were made to minimize suffering.
Parasite quantitation and statistical analysis
To qualitatively and quantitatively assess the permissiveness of A. funestus to P. berghei, intact mosquitoes and dissected mosquito tissues were examined at 7 days post-feeding to assay midgut stages of infection and at 18–20 days post-feeding to assay sporozoite migration and salivary gland invasion. Oocyst infection prevalence is defined as the percentage of mosquitoes that become infected with oocysts, and oocyst intensity is the mean and median number of oocysts in the midguts of infected mosquitoes [24].
The data presented in this study represent the results from two independent field collections and laboratory experiments. For comparison, parallel infections were carried out by feeding mosquitoes of the sympatric species, A. gambiae (G3 colony) on the same P. berghei-infected mice. A. gambiae were reared and maintained under the same conditions described for A. funestus.
Cell imaging
Visual observations were done under bright field illumination, differential-interference-contrast (DIC), and GFP epi-fluorescence using a Nikon Eclipse E600 upright microscope connected to a CoolSNAPES digital camera (Photometrics, Tucson, AZ). Digital images were taken using MetaVue Imaging Software (Universal Imaging Corporation, Downingtown, PA), bright field images HiGauss filtered using Image-Pro Plus (Media Cybernetics, Silver Spring, MD), and histogram stretches, stitching, and overlays done using Adobe Photoshop (Adobe Systems, San Jose, CA).
Results and Discussion
We used the F1 progeny of field-collected A. funestus females to assess whether P. berghei can complete its life cycle in this mosquito species, and we did not attempt to obtain further generations. Thus, the mosquitoes tested should represent an unbiased sample of random wild mosquito genotypes.
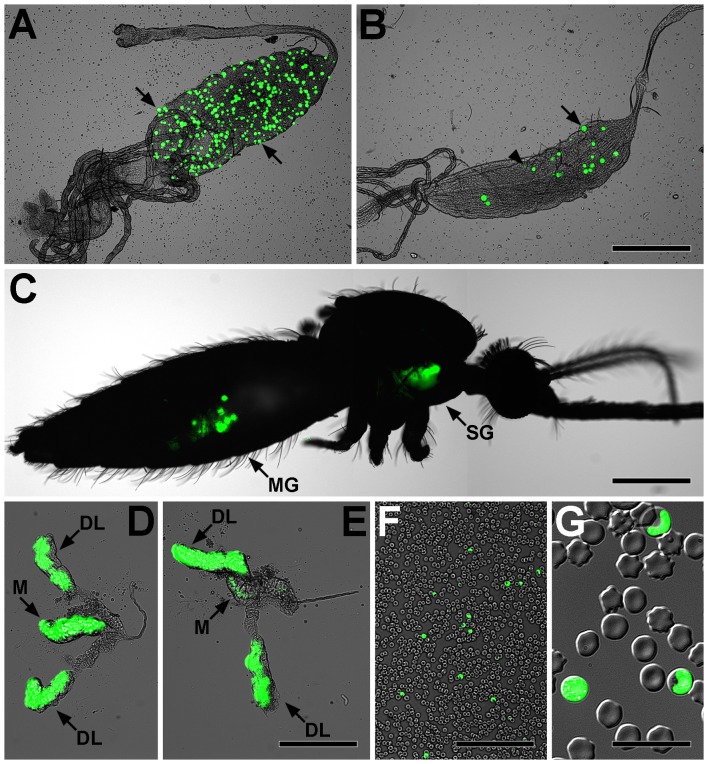
Following blood feeding on infected mice, numerous P. berghei oocysts were observed on A. funestus midguts as early as 7 days post-feeding, the earliest time point tested (Figure 1A). By 18–20 days post-infection, both midgut oocysts and salivary gland sporozoites were observed in dissected tissues (Figure 1B, D–E), and through the cuticle of live mosquitoes (Figure 1C). By this time several oocysts had ruptured, and 57% (9/17) of infected mosquitoes carried salivary gland sporozoites. In the hemocoel, migrating sporozoites were observed to flow with the hemolymph through the dorsal vessel in a manner similar to that recently reported in the A. gambiae-P. berghei system [12], [14]. Furthermore, sporozoites were also occasionally observed attached to the cuticle and in the appendages. When the salivary glands were closely examined, sporozoites were observed to preferentially invade the median and distal lateral lobes (Figure 1D–E). These observations are in agreement with reports in other mosquito species [25], [26], including the A. gambiae-P. berghei system [27].
Figure 1. Light and GFP epi-fluorescence microscopy show fluorescent Plasmodium berghei parasites developing in Anopheles funestus mosquitoes and murine erythrocytes.
A. A. funestus midgut with greater than 300 P. berghei oocysts (e.g., arrows) at 7 days post-infection. B. A. funestus midgut showing normal oocysts (e.g., arrow) and oocysts that have recently undergone rupture (e.g., arrowhead) at 20 days post-infection. C. Imaging of fluorescent parasites through the cuticle of a live A. funestus showing parasite development in the midgut (MG) and salivary glands (SG). Note that tissues presented in panels B, D, and E originated from this mosquito. D–E. A. funestus salivary glands showing that sporozoites preferentially invade the median (M) and distal lateral (DL) lobes. F–G. Blood smear from a mouse exposed to P. berghei via mosquito bite showing infected erythrocytes, indicating that A. funestus salivary gland sporozoites are infective to the vertebrate host and that the parasite can complete its life cycle inside the insect vector. Bars: A–C = 500 µm; D–E = 200 µm; F = 100 µm; G = 20 µm.
To test the infectivity of A. funestus salivary gland sporozoites to mice, 15 infected mosquitoes (19 days post-P. berghei infection) were fed on two normal mice. One mouse became infected as determined by the visualization of blood stage parasites at 7 days post-mosquito bite (Figure 1F–G). These experiments indicate that P. berghei is capable of completing its life cycle in A. funestus.
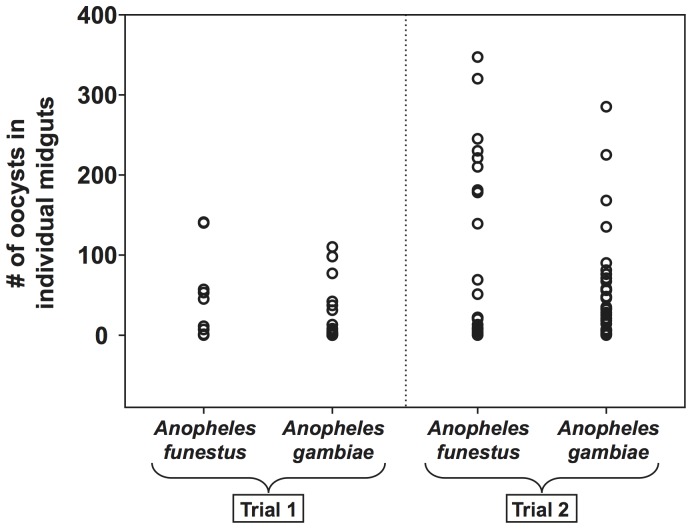
To compare parasite development in A. funestus versus A. gambiae, parallel infections were tracked for the first 7 days post-infection (Figure 2). In the first trial, A. funestus prevalence of infection, as determined by the presence of fluorescent P. berghei oocysts on the midguts of individual mosquitoes, was 62.5% (10/16) and median oocyst intensity was 28 (mean = 47; range = 1–141). In a parallel infection using A. gambiae, prevalence of infection was 56% (20/36) and median oocyst intensity was 4 (mean = 23; range = 1–110). The second trial yielded a similar comparison: A. funestus prevalence of infection was 95% (19/20) as compared to 97% (29/30) for A. gambiae, and median oocyst intensity was 69 (mean = 120; range = 1–347) for A. funestus and 35 (mean = 56; range = 1–285) for A. gambiae. Overall, P. berghei infection prevalence was equivalent in the two mosquito species. Although both trials showed a trend for higher oocyst intensities in A. funestus, the difference was not statistically significant (Mann-Whitney P>0.05). However, due to the negative binomial distribution of oocysts in infected midguts [28], [29], large sample sizes would be necessary to yield statistically significant estimates of mean infection intensity.
Figure 2. Anopheles funestus and Anopheles gambiae mosquitoes display equivalent susceptibility to Plasmodium berghei infection.
A. gambiae and A. funestus mosquitoes were fed on the same infected P. berghei-infected mouse in two replicate experiments, and midgut oocyst infections were quantified at 7 days post-infection. Each circle represents the number of midgut oocysts in an individual mosquito.
Conclusions
This study demonstrates that P. berghei can complete its life cycle in A. funestus. Several hurdles remain to be overcome before unraveling the molecular interactions between Plasmodium parasites and A. funestus, including the lack of available diverse and robust laboratory colonies. Nevertheless, the data presented in this study, together with the understanding that A. funestus is a major vector of human malaria, illustrate that, once the reference genome sequence of A. funestus is available, studying A. funestus-Plasmodium interactions is feasible and warranted in a laboratory setting.
Funding Statement
This work was funded in part by National Institutes of Health/National Institute of Allergy and Infectious Diseases (NIH/NIAID) R01AI042361 and AI073685 to KDV and NIH/NIAID F32AI065075 to JFH. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Breman JG, Alilio MS, Mills A (2004) Conquering the intolerable burden of malaria: what's new, what's needed: a summary. Am J Trop Med Hyg 71: 1–15. [PubMed] [Google Scholar]
- 2. Hay SI, Guerra CA, Tatem AJ, Noor AM, Snow RW (2004) The global distribution and population at risk of malaria: past, present, and future. Lancet Infect Dis 4: 327–336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Cohuet A, Simard F, Wondji CS, Antonio-Nkondjio C, Awono-Ambene P, et al. (2004) High malaria transmission intensity due to Anopheles funestus (Diptera: Culicidae) in a village of savannah-forest transition area in Cameroon. J Med Entomol 41: 901–905. [DOI] [PubMed] [Google Scholar]
- 4. Sinka ME, Bangs MJ, Manguin S, Rubio-Palis Y, Chareonviriyaphap T, et al. (2012) A global map of dominant malaria vectors. Parasites & vectors 5: 69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Nkuo-Akenji T, Ntonifor NN, Ndukum MB, Abongwa EL, Nkwescheu A, et al. (2006) Environmental factors affecting malaria parasite prevalence in rural Bolifamba, South- West Cameroon. Afr J Health Sci 13: 40–46. [DOI] [PubMed] [Google Scholar]
- 6. Bigoga JD, Manga L, Titanji VP, Coetzee M, Leke RG (2007) Malaria vectors and transmission dynamics in coastal south-western Cameroon. Malar J 6: 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Crawford JE, Guelbeogo WM, Sanou A, Traore A, Vernick KD, et al. (2010) De novo transcriptome sequencing in Anopheles funestus using Illumina RNA-seq technology. PloS one 5: e14202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Vincke IH (1954) Natural history of Plasmodium berghei . Indian J Malariol 8: 245–256. [PubMed] [Google Scholar]
- 9. Vincke IH, Lips M (1948) Un nouveau Plasmodium d'un rongeur sauvage du Congo: Plasmodium berghei n.sp. Ann Soc Belge Med Trop 28: 97–104. [PubMed] [Google Scholar]
- 10. Franke-Fayard B, Trueman H, Ramesar J, Mendoza J, van der Keur M, et al. (2004) A Plasmodium berghei reference line that constitutively expresses GFP at a high level throughout the complete life cycle. Mol Biochem Parasitol 137: 23–33. [DOI] [PubMed] [Google Scholar]
- 11. Frevert U, Engelmann S, Zougbede S, Stange J, Ng B, et al. (2005) Intravital observation of Plasmodium berghei sporozoite infection of the liver. PLoS Biol 3: e192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Hillyer JF, Barreau C, Vernick KD (2007) Efficiency of salivary gland invasion by malaria sporozoites is controlled by rapid sporozoite destruction in the mosquito haemocoel. Int J Parasitol 37: 673–681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Jin Y, Kebaier C, Vanderberg J (2007) Direct microscopic quantification of dynamics of Plasmodium berghei sporozoite transmission from mosquitoes to mice. Infect Immun 75: 5532–5539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. King JG, Hillyer JF (2012) Infection-Induced Interaction between the Mosquito Circulatory and Immune Systems. PLoS Pathog 8: e1003058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Alavi Y, Arai M, Mendoza J, Tufet-Bayona M, Sinha R, et al. (2003) The dynamics of interactions between Plasmodium and the mosquito: a study of the infectivity of Plasmodium berghei and Plasmodium gallinaceum, and their transmission by Anopheles stephensi, Anopheles gambiae and Aedes aegypti . Int J Parasitol 33: 933–943. [DOI] [PubMed] [Google Scholar]
- 16. Bray RS (1954) The mosquito transmission of Plasmodium berghei . Indian J Malariol 8: 263–274. [PubMed] [Google Scholar]
- 17. Kalucy EC, McMillan B (1970) Transmission of Plasmodium berghei (NK 65 strain) by Anopheles annulipes Walker. Nature 225: 97. [DOI] [PubMed] [Google Scholar]
- 18.Sinden RE, Butcher GA, Beetsma AL (2002) Maintenance of the Plasmodium berghei Life Cycle. In: Doolan DL, editor. Malaria Methods and Protocols. Totowa, NJ: Humana Press. pp. 25–40. [DOI] [PubMed]
- 19. Vaughan JA, Narum D, Azad AF (1991) Plasmodium berghei ookinete densities in three anopheline species. J Parasitol 77: 758–761. [PubMed] [Google Scholar]
- 20. Vincke IH (1954) Experimental transmission of Plasmodium berghei . Indian J Malariol 8: 257–262. [PubMed] [Google Scholar]
- 21. Yoeli M, Most H, Bone G (1964) Plasmodium berghei: cyclical transmissions by experimentally infected Anopheles quadrimaculatus . Science 144: 1580–1581. [DOI] [PubMed] [Google Scholar]
- 22. Frischknecht F, Martin B, Thiery I, Bourgouin C, Menard R (2006) Using green fluorescent malaria parasites to screen for permissive vector mosquitoes. Malar J 5: 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Habtewold T, Povelones M, Blagborough AM, Christophides GK (2008) Transmission blocking immunity in the malaria non-vector mosquito Anopheles quadriannulatus species A. PLoS pathogens 4: e1000070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Margolis L, Esch GW, Holmes JC, Kuris AM, Schad GA (1982) The use of ecological terms in parasitology (report of an ad hoc committee of the American Society of Parasitologists). J Parasitol 68: 131–133. [Google Scholar]
- 25. Pimenta PF, Touray M, Miller L (1994) The journey of malaria sporozoites in the mosquito salivary gland. J Eukaryot Microbiol 41: 608–624. [DOI] [PubMed] [Google Scholar]
- 26. Sterling CR, Aikawa M, Vanderberg JP (1973) The passage of Plasmodium berghei sporozoites through the salivary glands of Anopheles stephensi: an electron microscope study. J Parasitol 59: 593–605. [PubMed] [Google Scholar]
- 27.Sinden RE (1997) Infection of mosquitoes with rodent malaria. In: Crampton JM, Beard CB, Louis C, editors. The molecular biology of insect disease vectors: a methods manual. Cambridge: The University Press. pp. 67–91.
- 28. Billingsley PF, Medley GF, Charlwood D, Sinden RE (1994) Relationship between prevalence and intensity of Plasmodium falciparum infection in natural populations of Anopheles mosquitoes. Am J Trop Med Hyg 51: 260–270. [DOI] [PubMed] [Google Scholar]
- 29. Medley GF, Sinden RE, Fleck S, Billingsley PF, Tirawanchai N, et al. (1993) Heterogeneity in patterns of malarial oocyst infections in the mosquito vector. Parasitology 106 Pt 5 441–449. [DOI] [PubMed] [Google Scholar]