Abstract
African Americans are less likely than Whites to enroll in hospice. In addition, patients are often referred to hospice very close to death, when they may not have time to take advantage of the full range of hospice services. Understanding how race and location before hospice enrollment are related to hospice length of stay (LOS) may inform the development of interventions to increase timely access to hospice care. Using data from a national hospice provider, African Americans and Whites admitted to routine home hospice care in a private residence between January 1, 2000, and December 31, 2003, were identified. Logistic regression was used to examine the association between race and hospice preadmission location (hospital vs other locations) and preadmission location and hospice LOS (≤7 days vs >7 days) after adjusting for demographic and hospice use variables. Of 43,869 enrollees, 15.3% were African American. One to 2 days before hospice enrollment, African Americans were more likely than Whites to be in the hospital than in all other locations (48.6% vs 32.3%, P < .001; adjusted odds ratio = 1.83, 95% confidence interval = 1.73– 1.95). Regardless of race, those whose preadmission location was the hospital were more likely than those from other locations to die 7 days or less after hospice enrollment. Initiatives to improve end-of-life care should focus on increasing timely access to hospice referrals in settings outside of the hospital. Future research should examine whether racial differences in hospice preadmission location reflect differences in preferences for care or disparities in timely access to hospice referrals in non-acute care settings.
Keywords: hospice, length of stay, race, end-of-life care
Hospice is one of the most comprehensive and effective models for care at the end of life. Not only is hospice use associated with better care of dying patients than conventional care, but hospice has also been shown to reduce healthcare costs in the last months of life.1–4 Although the number of hospice enrollees has increased significantly over the last decade, lengths of stay have remained low, with nearly one-third of people served by hospice in 2008 receiving services for 1 week or less.5 Shorter lengths of stay may not allow patients time to take advantage of the full range of services that hospice provides, including pain and symptom management and psychosocial and spiritual support.
Previous studies have identified a number of factors associated with shorter lengths of stay in hospice, including referral from a hospital.6–9 Although referral to hospice from a hospital may reflect a patient’s decision to transition from the use of life-sustaining therapies to care focused on comfort, such referrals may also reflect poorer access to care or to information about hospice in settings outside of the hospital. For example, because of fewer primary care visits and greater frequency of hospitalization in the last months of life, African Americans, a group historically underrepresented in hospice, may be more likely to be referred to hospice from hospitals.5,10–14 Additionally, African Americans referred to hospice from the hospital may experience shorter lengths of stay than enrollees referred from non-acute care settings. If this is true, initiatives targeting timely discussions about end-of-life care and hospice referrals in settings outside of the hospital may improve access to hospice and increase lengths of stay for African Americans with advanced illness whose goals of care are consistent with the hospice philosophy of care.
The purpose of this study was to examine racial differences in location of African-American and White home hospice patients in the 1 to 2 days before hospice enrollment (preadmission location) and determine whether racial differences existed in the relationship between hospice preadmission location and hospice length of stay (LOS). Understanding the relationships between race and hospice referral patterns across healthcare settings (acute vs non-acute) and patient location before hospice enrollment and LOS may inform the development of interventions to increase timely access to hospice care.
METHODS
Data Source
Data for these analyses were obtained from VITAS Healthcare, a national for-profit hospice provider. For the time period described in these analyses, VITAS had 26 hospice programs in eight states—California, Florida, Illinois, New Jersey, Ohio, Pennsylvania, Texas, and Wisconsin. After obtaining approval from the hospice provider and the Duke University Medical Center institutional review board, data were abstracted from the central administrative and clinical database of the provider. Processes for ensuring the quality of the information in the database included preprogrammed parameters, control processes for changing data entry, and monitoring of data entry for accuracy and timeliness by staff at each program.
Study Population
African-American and White hospice enrollees who were admitted to routine home hospice care, resided in a private residence at the time of hospice admission, and died between January 1, 2000, and December 31, 2003, were included.
Outcome Variables
This study used three different multivariate models. In Model 1, the outcome was hospice preadmission location, which refers to the location of the enrollee in the 1 to 2 days before hospice admission. A healthcare provider in the hospital generally referred enrollees whose preadmission location was the hospital or emergency department (ED) to hospice. This variable was categorized as acute care setting (hospital or ED) or non-acute care setting (all other locations—home, nursing home, other). In Models 2 and 3, the sample was stratified according to race to examine the association between preadmission location and hospice LOS for African Americans (Model 2) and Whites (Model 3). Because the association between preadmission location and very short hospice stays was of interest, the outcome variable for Models 2 and 3 was categorized into a hospice LOS of 7 days or less versus longer than 7 days. This categorization has been used in other analyses.5,6
Covariates
Covariates for these analyses were selected a priori based on their relevance as potential confounders of the relationship between race and hospice preadmission location (Model 1) and preadmission location and LOS (Models 2 and 3). In addition to race and hospice preadmission location, the following variables were included in the models: age (< 65 vs ≥65), sex, marital status (married vs other), diagnosis (cancer vs noncancer), relationship of caregiver to patient (spouse, child, other relative, nonrelative, no caregiver listed), income, payment source (Medicare, Medicaid, charity, other), enrollment in health maintenance organization (HMO), and location of hospice according to region (South, Midwest, Northeast, West). Subjects’ ZIP codes were matched to 2000 U.S. census tract data to generate median household incomes. This income measure was divided into three categories, each containing one-third of the census tract median household income distribution of the sample (low, ≤$37,280; middle, $37,281–48,541; and high, ≥$48,542).
Analyses
Bivariate Analyses
To compare African Americans and Whites across demographic and hospice use variables, chi-square tests were used for categorical variables and nonparametric Wilcoxon tests for continuous variables. A two-sample median test was used to examine differences in LOS according to race and preadmission location. Differences were considered statistically significant at P < .05. To examine time to death after hospice enrollment according to race and preadmission location, Kaplan-Meier curves were generated. Two separate curves were generated for each racial group based on preadmission location (hospital and ED vs other).
Multivariate Analyses
In the first analysis (Model 1), logistic regression was used to determine whether race was an independent predictor of hospice preadmission location. In the second set of analyses (Models 2 and 3), logistic regression was used to determine whether preadmission location was an independent predictor of LOS categorized as 7 days or longer versus longer than 7 days. Separate models were fit for African Americans (Model 2) and Whites (Model 3) to determine whether the relationship between preadmission location and hospice LOS was the same for each racial group. All analyses were conducted using SAS version 9.1 (SAS Institute, Inc., Cary, NC).
RESULTS
During the 3-year study period, 43,869 African Americans and Whites died after electing routine home hospice care (in a private residence) from one of the hospice provider’s programs. Of these, 6,720 (15.3%) were African American. Sample characteristics according to race are listed in Table 1. African Americans were younger (mean age 71 vs 77, P < .001) and more likely to be unmarried, have a median household income $37,280 or less, have an admission diagnosis of cancer, and use Medicaid as a payment source than Whites. A slightly greater proportion of Whites than African Americans had a LOS of 1 week or less (23.8% vs 20.7%).
Table 1.
Sample Characteristics According to Race
| Characteristic | n (%) | |
|---|---|---|
| African Americans n = 6,720 (15.3%) |
Whites n = 37,149 (84.7%) |
|
| Age* | ||
| <65 | 2,064 (30.7) | 6,677 (18.0) |
| ≥65 | 4,656 (69.3) | 30,472 (82.0) |
| Sex | ||
| Female | 3,601 (53.6) | 19,975 (53.5) |
| Male | 3,119 (46.4) | 17,274 (46.5) |
| Marital status* | ||
| Married | 2,300 (34.2) | 17,107 (46.1) |
| Other | 4,420 (65.8) | 20,042 (54.0) |
| Caregiver* | ||
| Spouse | 2,040 (30.4) | 14,914 (40.2) |
| Child | 2,837 (42.2) | 16,190 (43.6) |
| Other relative | 1,505 (22.4) | 4,272 (11.5) |
| Nonrelative | 242 (3.6) | 1,396 (3.8) |
| None identified | 96 (1.4) | 377 (1.0) |
| Diagnosis* | ||
| Cancer | 4,878 (72.6) | 21,657 (58.3) |
| Other | 1,842 (27.4) | 15,492 (41.7) |
| Median household income, $* | ||
| ≤37,280 | 4,650 (69.3) | 8,845 (23.9) |
| 37,281–48,541 | 1,280 (19.1) | 12,240 (33.1) |
| ≥48,542 | 777 (11.6) | 15,916 (43.0) |
| Payment source* | ||
| Medicare | 4,799 (71.4) | 30,783 (82.9) |
| Medicaid | 851 (12.7) | 915 (2.5) |
| Charity | 197 (2.9) | 525 (1.4) |
| Other | 873 (13.0) | 4,926 (13.3) |
| Health maintenance organization enrollment | ||
| Yes | 3,708 (55.2) | 20,337 (54.7) |
| No | 3,012 (44.8) | 16,812 (45.3) |
| Length of stay, days* | ||
| ≤7 | 1,393 (20.7) | 8,832 (23.8) |
| >7 | 5,327 (79.3) | 28,317 (76.2) |
| Hospice location* | ||
| South | 3,129 (45.6) | 19,773 (53.2) |
| Midwest | 2,248 (33.5) | 6,627 (17.8) |
| West | 690 (10.3) | 9,129 (24.6) |
| Northeast | 653 (9.7) | 1,620 (4.4) |
| Hospice preadmission location* | ||
| Acute care setting (hospital or emergency department) | 3,266 (48.6) | 11,981 (32.3) |
| Nonacute care setting | 3,454 (51.4) | 25,168 (67.8) |
| Home | 3,225 (93.4) | 20,994 (83.4) |
| Nursing home or assisted living | 226 (6.5) | 4,132 (16.4) |
| Other | 3 (0.1) | 42 (0.20) |
P < .001: chi-square test for difference between racial groups.
Preadmission Location
A significantly greater proportion of African Americans than Whites were in an acute care setting (hospital or ED) in the days before hospice enrollment (48.6% vs 32.3%, P < .001). Of those whose preadmission location was a non-acute care setting, home was the most common location for both racial groups (Table 1). In multivariate analysis, race was the single greatest predictor of hospice preadmission location (Table 2, Model 1). African Americans had an 83% higher odds of being in an acute care setting (vs non-acute care setting) than Whites before hospice enrollment (odds ratio (OR) = 1.83, 95% confidence interval (CI) = 1.73–1.95). Using Medicaid as payment source (vs Medicare) and living in the Northeast (vs South) were also associated with a greater likelihood of being in an acute care setting before hospice enrollment. Conversely, being aged 65 and older, participation in a HMO, and having a diagnosis of cancer were associated with a lower likelihood of being in an acute care setting than a non-acute care setting before hospice enrollment.
Table 2.
Multivariate Analyses of Predictors of Hospice Preadmission Location and Hospice Length of Stay (LOS)
| Predictor Variable | Adjusted Odds Ratio (95% Confidence Interval) | ||
|---|---|---|---|
| Model 1 | Model 2 | Model 3 | |
| Preadmission Location | Hospice LOS | Hospice LOS | |
| Total | African Americans | Whites | |
| Preadmission location hospital or emergency department | — | 1.51 (1.34–1.71) | 1.52 (1.44–1.59) |
| African Americans | 1.83 (1.73–1.95) | — | — |
| Age ≥65 | 0.77 (0.71–0.84) | 0.98 (0.80–1.21) | 0.96 (0.86–1.08) |
| Female | 1.01 (0.96–1.05) | 0.95 (0.83–1.08) | 0.82 (0.78–0.87) |
| Married | 0.99 (0.94–1.05) | 1.18 (1.01–1.37) | 1.11 (1.04–1.18) |
| Caregiver (reference: spouse) | |||
| Child | 1.00 (0.95–1.06) | 1.09 (0.94–1.26) | 1.10 (1.03–1.17) |
| Other relative | 0.94 (0.78–1.15) | 1.0 (0.60–1.68) | 1.0 (0.77. 1.28) |
| Nonrelative | 0.91 (0.81–1.02) | 0.68 (0.46–0.99) | 0.84 (0.72–0.96) |
| Cancer diagnosis | 0.91 (0.87–0.95) | 0.75 (0.65–0.85) | 0.70 (0.67–0.74) |
| Median household income, $ | |||
| ≤37,280 (reference) | |||
| 37,281–48,541 | 0.96 (0.91–1.02) | 1.13 (0.97–1.32) | 0.97 (0.91–1.04) |
| ≥48,542 | 0.99 (0.94–1.05) | 0.92 (0.76–1.11) | 1.01 (0.95–1.08) |
| Health maintenance organization enrollment | 0.84 (0.80–0.88) | 0.82 (0.71–0.94) | 0.79 (0.74–0.84) |
| Payment source (reference: Medicare) | |||
| Medicaid | 1.45 (1.28–1.65) | 0.94 (0.73–1.21) | 0.77 (0.64–0.93) |
| Charity | 1.15 (0.97–1.36) | 1.29 (0.89–1.87) | 1.54 (1.24–1.90) |
| Other | 1.18 (1.07–1.30) | 1.59 (1.23–2.04) | 1.73 (1.53–1.95) |
| Hospice location (reference: South) | |||
| Midwest | 0.99 (0.94–1.05) | 1.23 (1.07–1.42) | 1.13 (1.06–1.21) |
| West | 1.02 (0.97–1.08) | 1.84 (1.52–2.24) | 1.36 (1.28–1.44) |
| Northeast | 1.46 (1.34–1.60) | 1.27 (1.02–1.57) | 1.08 (0.96–1.22) |
Models 1, 2, 3: Logistic regression models that include all variables presented in table.
Outcome variables were preadmission location (acute care setting (hospital or emergency department) vs other) and hospice LOS (≤7 days vs >7 days).
Preadmission Location and LOS
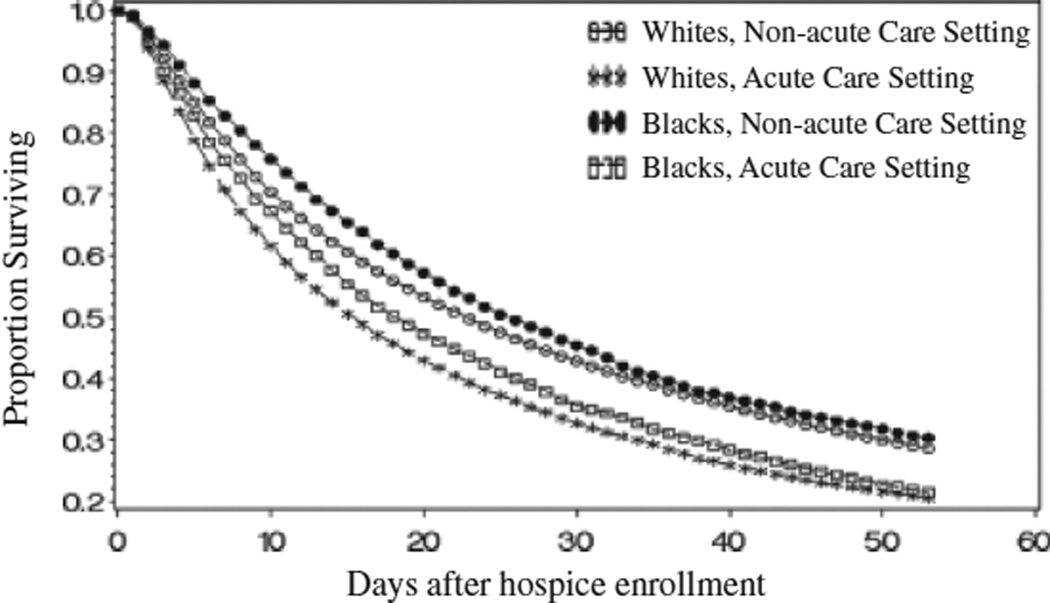
African Americans whose preadmission location was the hospital or ED were more likely to die 1 week or less after enrollment than those in non-acute care settings (24.5% vs. 17.2%, P < .001). This was also true for Whites (29.2% vs 21.2%, P < .001). Figure 1 displays survival according to race and preadmission location. The median time to death was 19 days for African Americans whose preadmission location was an acute care setting, versus 26 days for those whose preadmission location was a non-acute care setting (P < .001) and 16 days versus 23 days (P < .001), respectively, for Whites. The median time from hospice enrollment to death for African Americans was slightly greater than that of Whites for both pre-admission categories (19 days vs 16 days, P < .001 for acute care setting; 26 days vs 23 days, P = .002 for non-acute care settings).
Figure 1.
Survival according to race and preadmission location. Non-acute care setting = home, nursing home, assisted living, other. Acute care setting = hospital or emergency department. P < .001 for all pairwise comparisons.
Table 2 includes multivariate analyses stratified according to race of predictors of hospice LOS. African Americans (Model 2) whose preadmission location was the hospital or ED had 51% higher odds of dying 1 week or less after hospice enrollment than those in a non-acute care setting (OR = 1.51, 95% CI = 1.34–1.71). Similarly, Whites (Model 3) whose preadmission location was an acute care setting had a 52% higher odds of dying 1 week or less after hospice enrollment (OR = 1.52, 95% CI = 1.44–1.59).
DISCUSSION
In this study of hospice enrollees admitted to routine home hospice care in a private residence, African Americans were more likely than Whites to be in the hospital or ED than a non-acute care setting in the 1 to 2 days before hospice enrollment. African Americans and Whites who were in the hospital or ED had a similarly higher likelihood of dying 1 week or less after hospice enrollment than their counterparts who were in non-acute care settings. These findings have implications for the design of interventions to increase access to hospice care for African Americans and to promote earlier access to hospice for patients in all racial groups.
The finding that African-American race is an independent predictor of referral to hospice from a hospital can be understood in the context of what is known about racial differences in treatment preferences, resource use, and access to care. In some instances, admission to hospice after hospitalization may reflect care consistent with the preferences of a patient who is well informed about options for end-of-life care, including hospice. African Americans are more likely than Whites to want life-sustaining therapies at the end of life regardless of prognosis and have higher rates of hospitalization, cardiopulmonary resuscitation, and in-hospital deaths.11–15 Given longer time spent in acute care settings at the end of life, it is not surprising that African Americans were more likely than Whites to be in the hospital in the days before hospice enrollment. For some, the hospital stay may represent one last effort for cure. When this is unsuccessful, patients may be “ready” to transition to a course of care focused on comfort and enroll in hospice.
Although admission to hospice after an acute care stay may be consistent with the treatment preferences of some African Americans, for others it may reflect poorer access to referrals and information about hospice in non-acute care settings. African Americans report less exposure to information about hospice care than Whites.16,17 African Americans are also less likely to have a usual source of health care and have fewer primary care visits in the last year of life.13,18 A greater number of primary care visits in the year before death has been associated with fewer hospital days and less in-hospital death.13 This suggests that people with greater access to primary care may be referred to service providers earlier in the course of their illness, such as hospice or home health, who are able to meet their needs in non-acute care settings.
In addition to less access to primary care, African Americans are diagnosed at later stages in the course of many chronic illnesses.19 As a result, they may not have the opportunity to form relationships with specialists who provide care for the terminal illness. Lack of regular and ongoing follow-up with any healthcare provider—specialist or generalist—may lead to fewer opportunities in non-acute care settings to discuss prognosis or advance care planning or to receive information about hospice. Hospitalization may become the default way to seek health care. Because hospitals are largely oriented to the provision of acute care, even patients who are hospitalized repeatedly may not learn about hospice until late in the course of disease.
Although African Americans were more likely than Whites to be in the hospital before hospice enrollment, being in an acute care setting was associated with similarly higher odds of dying 1 week or less after hospice enrollment than being in a non-acute care setting for both racial groups. A number of studies have documented suboptimal outcomes in caregivers who believe that their loved ones were referred to hospice too late, including greater unmet needs for emotional support, communication, and lower satisfaction with care.20–22 Also, patients with shorter lengths of stay receive fewer hospice services, and their caregivers face a higher risk of major depression in the 6 to 8 months after the patient’s death.20,23,24 Although there is debate about the optimal LOS for hospice enrollees, very short stays are unlikely to allow hospice time to effectively provide the services that promote quality care for dying patients and their families, including pain and symptom management and psychosocial and spiritual support.
Although LOS was short for enrollees of both racial groups, as in other studies, African Americans had slightly longer LOS than Whites.6,8,9 The median time from hospice enrollment to death for African Americans whose preadmission location was the hospital or ED was 19 days, versus 26 days for those in non-acute care settings and 16 days versus 23 days respectively for Whites. These analyses cannot determine the reasons for or significance of these differences. It seems unlikely that small differences in median LOS according to race (3 days for those with same preadmission) would result in appreciable differences in the mobilization of services that improve patient or caregiver outcomes. Rather, these findings highlight the need for efforts to increase LOS for patients in both racial groups, especially those referred from acute care settings who are at greatest risk for very short hospice stays.
The Medicare Hospice Benefit is one target for changes that may decrease the number of short stays in hospice and promote quality care for patients throughout the course of life-limiting illness. For patients who want to continue to receive potentially curative therapies, the either–or approach that characterizes the Medicare Hospice Benefit, whereby patients have to choose cure-directed or palliative therapies may increase the probability that these patients enroll in hospice late in the course of illness. Based on their greater preferences for life-prolonging therapies, the provisions of Medicare Hospice Benefit may disproportionately affect African Americans who report a greater need for hospice services.25 However, regardless of race, based on their preferences for care, some patients may be unwilling to enroll in hospice until very late in the course of illness. For many, one last hospitalization may precede enrollment, as these results suggest.
To accommodate a range of preferences in patients with serious illness, some private insurers are piloting programs that include a longer period of eligibility for hospice (prognosis of 12 months vs 6 months with the Medicare Hospice Benefit) and continued receipt of curative treatment while also receiving hospice services. There is evidence that these programs result in not only greater hospice enrollment and longer LOS, but also decreases in hospitalizations; therefore, despite liberalizing the type of care that patients can receive while on hospice, there is no adverse affect on cost.26
Another potential target for efforts to increase hospice LOS is the hospital. Older adults with advanced illness are often hospitalized multiple times in the last year of life.10–13 Thus, there may be missed opportunities in the acute care setting for earlier referrals to hospice. Involvement of hospital-based palliative care teams for patients with serious illness may increase the likelihood of hospice referral earlier in the course of disease.27 These teams address the physical and psychosocial needs of patients, helping patients to transition to hospice or other support services in the non-acute care setting, and provide appropriate care for those who may spend their last days in the hospital.
This study has a number of limitations. These data are drawn from a for-profit hospice provider and included enrollees in only eight states, so the findings may not be generalizable to hospice enrollees throughout the United States. For the period of these analyses, the sample had a lower rate of patients who were enrolled in hospice for 1 week or less than national data.28 This difference may reflect marketing efforts by the hospice provider or other factors not included in the analysis. Also, the sample was drawn from those who enrolled in hospice between 2000 and 2003. The results of the analysis may differ from an analysis of more-recent data, although if present, it is likely that these differences are small, given even higher rates of short hospice stays and continued racial differences in health services utilization at the end of life. Finally, this study is a retrospective analysis of hospice enrollees. Although some potential reasons for racial differences in hospice referral source are offered, no information was available on patient preferences, access to care, reasons for hospitalization, or other factors that may explain the results. Additionally, there was no information on the characteristics of healthcare providers or the practices of individual hospice programs that may influence referral of patients to hospice in different settings.
The findings of these analyses suggest that one potential target for initiatives to improve end-of-life care and increase hospice LOS for African Americans and Whites is increasing access to hospice referrals in settings outside of the hospital. For African Americans, who are more likely than Whites to be referred to hospice from acute care settings, such initiatives may be more successful if they focus on improving access to care in non-acute care settings throughout the continuum of illness. Future research should examine whether racial differences in hospice preadmission location reflect differences in preferences for care or disparities in access to hospice information and referrals in non-acute care settings.
ACKNOWLEDGMENTS
The analysis was funded by 1K08AG028975-01A1—Beeson Career Development Award in Aging.
Sponsor’s Role: Although the analysis uses data from the VITAS Healthcare Corporation, the study was not funded by VITAS and does not reflect the views of the VITAS Healthcare Corporation. Vitas had no role in the study design, analysis, interpretation of data, preparation, or approval of the manuscript.
Footnotes
Related Presentations and Published Abstracts Johnson KS. Racial differences in location prior to hospice enrollment and association with hospice length of stay. Poster presentation, Society of General Internal Medicine Annual Meeting, April 2008. Pittsburgh, Pennsylvania.
Conflict of Interest: The editor in chief has reviewed the conflict of interest checklist provided by the authors and has determined that the authors have no financial or any other kind of personal conflicts with this paper.
Author Contributions: Kimberly S. Johnson: study concept, design, analysis, interpretation, manuscript preparation. Maragatha Kuchibhatla: analysis, interpretation, and manuscript preparation. James A. Tulsky: study design, analysis, interpretation, manuscript preparation.
REFERENCES
- 1.Taylor DH, Ostermann J, Van Houtven CH, et al. What length of hospice use maximizes reduction in medical expenditures near death in the US Medicare program? Soc Sci Med. 2007;65:1466–1478. doi: 10.1016/j.socscimed.2007.05.028. [DOI] [PubMed] [Google Scholar]
- 2.Pyenson B, Connor S, Fitch K, et al. Medicare cost in matched hospice and non-hospice cohorts. J Pain Symptom Manage. 2004;28:200–210. doi: 10.1016/j.jpainsymman.2004.05.003. [DOI] [PubMed] [Google Scholar]
- 3.Teno JM, Clarridge BR, Casey V. Family perspective on end-of-life care at the last place of care. JAMA. 2004;291:88–93. doi: 10.1001/jama.291.1.88. [DOI] [PubMed] [Google Scholar]
- 4.Stevenson DG, Bramson JS. Hospice care in the nursing home settings: A review of the literature. J Pain Symptom Manage. 2009;38:440–451. doi: 10.1016/j.jpainsymman.2009.05.006. [DOI] [PubMed] [Google Scholar]
- 5.National Hospice and Palliative Care Organization. 2009 NHPCO Facts and Figures: Hospice Care in America. [Accessed May 14, 2010]; [on-line]. Available at http://www.nhpco.org/files/public/Statistics_Research/NHPCO_facts_and_figures.pdf. [Google Scholar]
- 6.Miller SC, Weitzen S, Kinzbrunner B. Factors associated with the high prevalence of short hospice stays. J Palliat Med. 2003;6:725–736. doi: 10.1089/109662103322515239. [DOI] [PubMed] [Google Scholar]
- 7.Somova MJ, Somov PG, Lawrence JC, et al. Factors associated with length of stay in a mid-sized, urban hospice. Am J Hosp Palliat Care. 2000;17:99–105. doi: 10.1177/104990910001700209. [DOI] [PubMed] [Google Scholar]
- 8.Han B, Remsburg RE, McAuley WJ, et al. Length of hospice care among U.S. adults, 1992–2000. Inquiry. 2007;44:104–113. doi: 10.5034/inquiryjrnl_44.1.104. [DOI] [PubMed] [Google Scholar]
- 9.Christakis NA, Iwashyna TJ. Impact of the individual and market factors on the timing of initiation of hospice care. Med Care. 2000;38:528–541. doi: 10.1097/00005650-200005000-00009. [DOI] [PubMed] [Google Scholar]
- 10.Shugarman LR, Decker SL, Bercovitz A. Demographic and social characteristics and spending at the end of life. J Pain Symptom Manage. 2009;38:15–26. doi: 10.1016/j.jpainsymman.2009.04.004. [DOI] [PubMed] [Google Scholar]
- 11.Hanchate A, Kronman AC, Young-Xu Y, et al. Racial and ethnic differences in end-of-life costs: Why do minorities cost more than whites? Arch Intern Med. 2009;169:493–501. doi: 10.1001/archinternmed.2008.616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Smith AK, Earle CC, McCarthy EP. Racial and ethnic differences in end-of-life care in fee-for-service Medicare beneficiaries with advanced cancer. J Am Geriatr Soc. 2009;57:153–158. doi: 10.1111/j.1532-5415.2008.02081.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kronman AC, Ash AS, Freund KM, et al. Can primary care visits reduce hospital utilization among Medicare beneficiaries at the end of life? J Gen Intern Med. 2008;23:1330–1335. doi: 10.1007/s11606-008-0638-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cohen LL. Racial/ethnic disparities in hospice care: A systematic review. J Palliat Med. 2008;11:763–767. doi: 10.1089/jpm.2007.0216. [DOI] [PubMed] [Google Scholar]
- 15.Barnato AE, Anthony DL, Skinner J, et al. Racial and ethnic differences in preferences for end-of-life-treatment. J Gen Intern Med. 2009;24:695–701. doi: 10.1007/s11606-009-0952-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ludke RL, Smucker DR. Racial differences in willingness to use hospice services. J Palliat Med. 2007;10:1329–1337. doi: 10.1089/jpm.2007.0077. [DOI] [PubMed] [Google Scholar]
- 17.Johnson KS, Kuchibhatla M, Tulsky JA. Racial differences in self-reported exposure to information about hospice care. J Palliat Med. 2009;12:921–927. doi: 10.1089/jpm.2009.0066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cherry DK, Woodwell DA, Rechtsteinger EA. Advance Data from Vital and Health Statistics; no 387. Hyattsville, MD: National Center for Health Statistics; 2007. National Ambulatory Medical Care Survey: 2005 Summary. [PubMed] [Google Scholar]
- 19.U.S. Department of Health and Human Services. Rockville, MD: National Healthcare Disparities Report; 2009. [Accessed May 14, 2010]. Agency for Healthcare Research and Quality. [on-line]. Available at http://www.ahrq.gov/qual/nhdr09/nhdr09.pdf. [Google Scholar]
- 20.Rickerson E, Harrold J, Kapo J, et al. Timing of hospice referral and families’ perceptions of services: Are earlier hospice referrals better? J Am Geriatr Soc. 2005;53:819–823. doi: 10.1111/j.1532-5415.2005.53259.x. [DOI] [PubMed] [Google Scholar]
- 21.Schockett ER, Teno JM, Miller SC, et al. Late referral to hospice and bereaved family member perception of quality of end-of-life care. J Pain Symptom Manage. 2005;30:400–407. doi: 10.1016/j.jpainsymman.2005.04.013. [DOI] [PubMed] [Google Scholar]
- 22.Teno JM, Shu JE, Casarett D, et al. Timing of referral to hospice and quality of care: Length of stay and bereaved family members’ perceptions of the timing of hospice referral. J Pain Symptom Manage. 2007;34:120–125. doi: 10.1016/j.jpainsymman.2007.04.014. [DOI] [PubMed] [Google Scholar]
- 23.Bradley EH, Prigerson H, Carlson MDA, et al. Depression among surviving caregivers: Does length of hospice enrollment matter? Am J Psychiatry. 2004;161:2257–2262. doi: 10.1176/appi.ajp.161.12.2257. [DOI] [PubMed] [Google Scholar]
- 24.Kris AE, Cherlin EJ, Prigerson H, et al. Length of hospice enrollment and subsequent depression in family caregivers: 13-month follow-up study. Am J Geriatr Psychiatry. 2006;14:264–269. doi: 10.1097/01.JGP.0000194642.86116.ce. [DOI] [PubMed] [Google Scholar]
- 25.Fishman J, O’Dwyer P, Lu HL, et al. Race, treatment preferences, and hospice enrollment: Eligibility criteria may exclude patients with the greatest needs for care. Cancer. 2009;115:689–697. doi: 10.1002/cncr.24046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Spettell CM, Rawlins WS, Krankauer R, et al. A comprehensive case management program to improve palliative care. J Palliat Med. 2009;12:827–832. doi: 10.1089/jpm.2009.0089. [DOI] [PubMed] [Google Scholar]
- 27.Fromme EK, Bascom PB, Smith MD, et al. Survival, mortality, and location of death for patients seen by a hospital-based palliative care team. J Palliat Med. 2006;6:903–911. doi: 10.1089/jpm.2006.9.903. [DOI] [PubMed] [Google Scholar]
- 28.Medicare Payment Advisory Commission. Report to the Congress: New approaches in Medicare. Washington, DC: 2004. Jun, [Accessed May 14, 2010]. Hospice care in Medicare: Recent trends and review of issues (Chapter 6) [on-line]. Available at http://www.medpac.gov/publications%5Ccongressional_reports%5CJune04_ch6.pdf. [Google Scholar]