Synthetic retinoids activate RARA- or PML/RARA-dependent transcription, but fail to degrade RARA or PML/RARA protein, which is insufficient for eradication of acute promyelocytic leukemia.
Abstract
In PML/RARA-driven acute promyelocytic leukemia (APL), retinoic acid (RA) induces leukemia cell differentiation and transiently clears the disease. Molecularly, RA activates PML/RARA-dependent transcription and also initiates its proteasome-mediated degradation. In contrast, arsenic, the other potent anti-APL therapy, only induces PML/RARA degradation by specifically targeting its PML moiety. The respective contributions of RA-triggered transcriptional activation and proteolysis to clinical response remain disputed. Here, we identify synthetic retinoids that potently activate RARA- or PML/RARA-dependent transcription, but fail to down-regulate RARA or PML/RARA protein levels. Similar to RA, these uncoupled retinoids elicit terminal differentiation, but unexpectedly fail to impair leukemia-initiating activity of PML/RARA-transformed cells ex vivo or in vivo. Accordingly, the survival benefit conferred by uncoupled retinoids in APL mice is dramatically lower than the one provided by RA. Differentiated APL blasts sorted from uncoupled retinoid–treated mice retain PML/RARA expression and reinitiate APL in secondary transplants. Thus, differentiation is insufficient for APL eradication, whereas PML/RARA loss is essential. These observations unify the modes of action of RA and arsenic and shed light on the potency of their combination in mice or patients.
Acute promyelocytic leukemia (APL) is driven by the PML/RARA fusion protein, which interferes with both transcriptional regulation by RARA and the assembly—and presumably function—of PML nuclear bodies (Lallemand-Breitenbach and de Thé, 2010). RARA signaling controls myeloid differentiation (Kastner et al., 2001), whereas PML is implicated in self-renewal (Ito et al., 2008), which likely explains how PML/RARA enforces both a promyelocyte differentiation block and acquisition of self-renewal. APL is a unique model in cancer biology as a result of the empirical discovery of two active drugs, retinoic acid (RA) and arsenic trioxide, which have been shown a posteriori to target PML/RARA (Quignon et al., 1997; de Thé and Chen, 2010). RA, which elicits APL cell differentiation ex vivo and in vivo, yields transient remissions in patients or mice. Arsenic initiates delayed differentiation in vivo only, but nonetheless cures up to 70% of de novo patients. Combined treatment with RA and arsenic definitively cures all mice and over 90% of patients (Lallemand-Breitenbach et al., 1999; Rego et al., 2000; Hu et al., 2009; de Thé and Chen, 2010).
Mechanistically, RA converts PML/RARA from a constitutive repressor into a transcriptional activator, which could explain the differentiation block reversal (Melnick and Licht, 1999). In addition, both RA and arsenic trigger PML/RARA degradation by, respectively, targeting each of its RARA and PML constitutive moieties (de Thé and Chen, 2010). Although some correlative studies have suggested that therapy-induced PML/RARA loss may be responsible for the clearance of leukemia-initiating cells (Nasr et al., 2008), blast differentiation through transcriptional activation of PML/RARA is still widely considered to account for therapeutic efficacy of RA, so that the molecular bases for this extraordinary clinical success remain disputed. Elucidation of the role of PML/RARA degradation was until now precluded by the lack of nuclear receptor mutants for which transcriptional activation and degradation would be fully uncoupled or of ligands that would activate transcription but fail to degrade the oncogenic fusion. Here, we identify two such molecules and demonstrate that although they trigger efficient APL cell differentiation, they fail to abolish leukemia-initiating activity ex vivo or in vivo. Thus PML/RARA degradation underlies RA anti-leukemic activity, unifying the modes of action of RA and arsenic.
RESULTS AND DISCUSSION
Uncoupled retinoids activate RARA signaling but fail to initiate RARA degradation
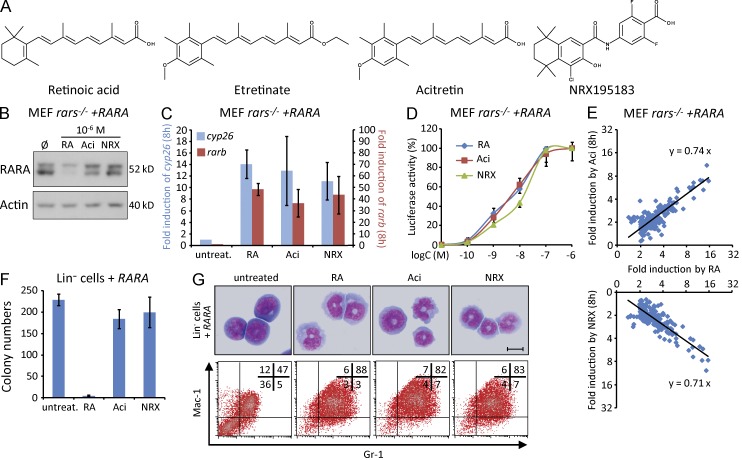
Previous studies had demonstrated that RA-induced RARA catabolism was tightly linked to its ability to activate transcription (Zhu et al., 1999). In an attempt to identify molecules that could modulate RA-triggered RARA degradation, we stably expressed an EGFP–RARA fusion in H1299 cells and examined the ability of 800 FDA-approved drugs to enhance or antagonize RA-induced degradation. Cells were treated with the drugs (10 µM) for 30 min before an overnight RA treatment (1 µM), and nuclear EGFP was quantified on live cells. As expected, some RAR or RXR agonists further reduced EGFP-RARA levels, whereas proteasome inhibitors blocked its RA-induced degradation. Interestingly, multiple drugs with glucocorticoid/progestative activities antagonized RA-induced RARA degradation. In contrast, antidepressive agents of different families promoted RARA degradation. Unexpectedly, RA-triggered EGFP-RARA degradation was antagonized by etretinate, a well-known retinoid used for treating psoriasis. This suggested that some retinoids may activate transcription without necessarily degrading RARA. Accordingly, contrary to RA, etretinate, acitretin, its active metabolite or NRX195183 (NRX), a well-characterized RARA-specific agonist (Fig. 1 A), were all incapable of degrading RARA in immortalized rara,b,g−/− mouse embryonic fibroblasts (rars−/− MEFs) stably reexpressing RARA (Fig. 1 B) or in cells expressing endogenous RARA (not depicted). Yet, acitretin and NRX, at a concentration of 1 µM, activate the transcription of primary RARA target genes (rarb or cyp26a1) or synthetic reporters (RARE3-Tk-Luc) as RA (Fig. 1, C and D). Moreover, in keeping with previous studies (Beard et al., 2002; Louisse et al., 2011), RA, NRX, and acitretin had similar dose–responses (and kinetics) for the activation of RARE3-Tk-Luc or for transcriptional activation of endogenous cyp26a1 (Fig. 1 D and not depicted). We finally performed array analysis of RARA-transduced rars−/− MEFs treated with RA, acitretin, or NRX. At 4 or 8 h, 1 µM retinoid displayed similar activation patterns, although the mean magnitude of induction was reduced by 25% with acitretin or NRX when compared with RA (Fig. 1 E), possibly reflecting the role of nuclear receptor degradation in sustained activation (Geng et al., 2012).
Figure 1.
Ligand-induced RARA transactivation and degradation can be uncoupled and control distinct biological effects. (A) Structures of RA, etretinate (Etre), acitretin (Aci) and NRX195183 (NRX). (B) Western blot analysis of RARA-transduced rars−/− MEFs after 6 h of treatment with RA, acitretin, or NRX at 1 µM. Actin demonstrates equal loading. (C) RA, acitretin, or NRX (1 µM), activate cyp26 and rarb gene expression in rars−/− MEFs stably reexpressing RARA, mean ± SD of three independent experiments. (D) Dose–response analysis of RA, acitretin, or NRX for the activation of RARE3-TK-Luc, a luciferase RA responsive reporter gene, in RARA-transduced rars−/− MEFs. Results are expressed as percentage of maximal activation, demonstrating similar affinities of the three retinoids. Means ± SD of 3 independent experiments. (E) Correlation between RA-, acitretin-, and NRX-triggered gene activation in rars−/− MEFs stably reexpressing RARA and treated for 8 h. Logarithmic scale. Analysis was restricted to genes induced more than twofold by RA or uncoupled retinoids in the transcriptomic arrays. Linear regression of the data is shown. Mean values of two independent experimental replicates. (F) Effect of RA, acitretin, or NRX on colony formation of RARA-transformed lineage-negative (Lin−) primary mouse hematopoietic progenitors after the first plating in methylcellulose (means ± SD of 3 independent experiments). (G) Effect of RA, acitretin, or NRX treatment on the cells described in F after 1 wk of methylcellulose culture (May–Grunwald Giemsa [MGG] staining, top; bar, 10 µm) or 24 h in liquid culture (FACS analysis, log10 fluorescence, bottom). Representative experiment of three independent ones.
We then compared the biological effects of these three retinoids in RARA-transformed murine primary hematopoietic progenitors, which exhibit a promyelocytic differentiation block and can be serially replated in methylcellulose cultures (Du et al., 1999; Zhu et al., 2005). As previously reported, RA induced terminal differentiation of these cells, as shown by MGG staining and FACS analysis, and completely abolished their clonogenic activity in methylcellulose (Fig. 1, F and G). In contrast, acitretin or NRX only elicited terminal differentiation (Fig. 1 F) and treated methylcellulose cultures exhibited normal clonogenic growth (Fig. 1 F). Thus, in RARA-transformed cells, transcriptional activation suffices to initiate differentiation, whereas RARA degradation underlies the loss of clonogenic activity, dramatically illustrating the pharmacological dissociation of these two previously intricately linked biological responses.
Uncoupled retinoids differentiate PML/RARA-transformed cells without affecting their clonogenic activity ex vivo
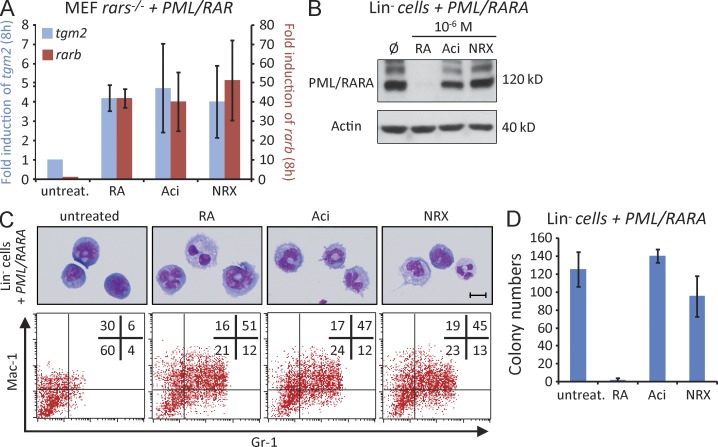
We similarly examined the effects of these retinoids on PML/RARA-expressing cells. In rars−/− MEFs stably expressing PML-RARA, two primary target genes, rarb and tgm2, were similarly up-regulated by the three drugs (Fig. 2 A). Yet, in these cells or in PML/RARA-transformed lin− murine hematopoietic progenitors, PML/RARA was completely degraded by RA treatment, but unaffected by treatment with acitretin or NRX, even at high concentrations (Fig. 2 B and not depicted). In methylcellulose cultures, acitretin or NRX again induced terminal differentiation of transformed primary progenitors (Fig. 2 C, top), but did not affect clonogenic growth, contrary to RA, which completely abolished colony formation (Fig. 2 D and not depicted). In the presence of uncoupled retinoids, differentiated PML/RARA-transformed cells could even be serially replated more than three times (unpublished data). Complete differentiation was similarly triggered by all three agents in liquid cultures (Fig. 2 C, bottom).
Figure 2.
Ligand-induced PML/RARA transactivation and degradation result in distinct biological effects. (A) RA, acitretin, or NRX (1 µM) activate rarb and tgm2 gene expressions in rars−/− MEFs stably expressing PML/RARA. Mean ± SD of three independent experiments. (B–D) Western blot analysis (B), differentiation on MGG staining (C, top; bar, 10 µm), and colony formation (D) of PML-RARA-transformed Lin− murine hematopoietic progenitors after 7-d treatment in methylcellulose culture with RA, acitretin, or NRX at 1 µM. Differentiation by FACS analysis (log10 fluorescence) after 24 h of treatment in liquid culture (C, bottom). Representative experiment of three independent ones.
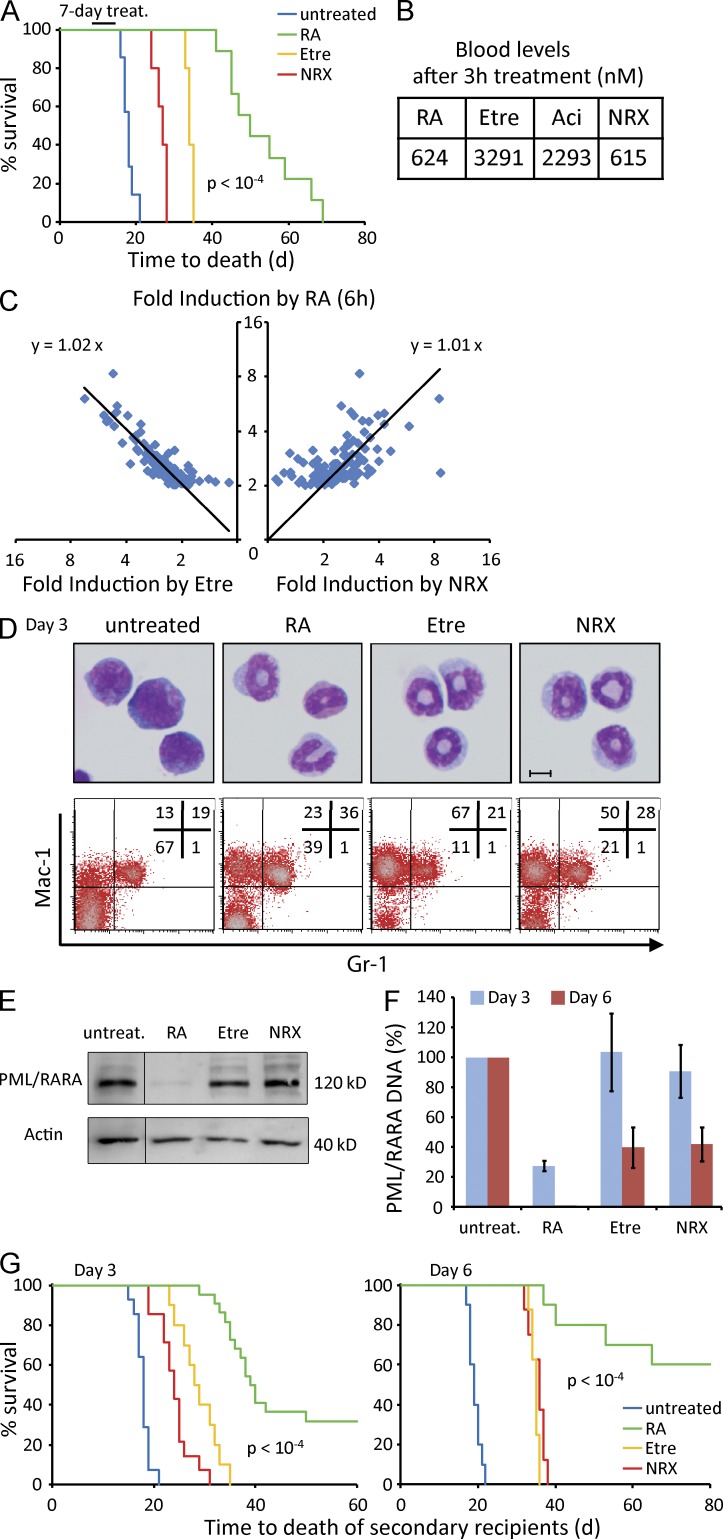
In vivo comparison of retinoids highlights the key role of PML/RARA degradation in APL clearance
This unexpected dissociation between differentiation and clonogenic activity ex vivo prompted us to examine the effects of these drugs in vivo. For this, we used a well-characterized APL mouse model (Brown et al., 1997; Lallemand-Breitenbach et al., 1999), in which APL cells derived from PML/RARA transgenics are serially transplanted in syngeneic hosts. Mice were treated with retinoids when the disease was established, allowing analysis of tumor response (bone marrow cell differentiation, growth, clonogenic activity as tested by transplantation in secondary recipients) and of mouse survival. A 7-d RA treatment yielded a very significant prolongation of survival (median of 50 vs. 18 d). The survival benefit was considerably smaller with NRX, acitretin, or etretinate, the metabolic precursor of acitretin identified in the original screen, when compared with RA (P < 10−4; Fig. 3 A and not depicted). Yet, retinoid plasma concentrations were measured in the same range (Fig. 3 B), target gene activations at 6 h were highly comparable (Fig. 3 C) and differentiation, as assessed by morphology after 3 d of in vivo treatment, was similar (Fig. 3 D, top). We could detect some differences in the expression of cell surface differentiation markers (Fig. 3 D, bottom), likely reflecting reappearance of some nonleukemic cells in the bone marrow of RA-treated mice. As expected, in APL blasts invading the bone marrow, PML/RARA was completely degraded after 3 d of RA treatment, whereas its level was unaffected in animals treated with uncoupled retinoids (Fig. 3 E).
Figure 3.
Uncoupled retinoids fail to clear APL. (A) Survival analysis of APL mice treated for 7 d with RA, etretinate (acitretin precursor), or NRX. 5 mice per group for NRX or etretinate, 10 for RA and controls. Pooled data from two independent experiments. Log rank test was used to evaluate significance of the survival difference between APL mice treated with RA or uncoupled retinoids. (B) Circulating levels of RA, acitretin, or NRX 3 h after initiation of therapy. Mean values of two mice per condition. (C) Correlation between RA-, etretinate-, and NRX-triggered gene activation in APL cells treated for 6 h in vivo. Logarithmic scale. Analysis was restricted to genes induced more than twofold by RA in the transcriptomic arrays. Linear regression of the data are shown. Mean value of two mice per condition. (D) MGG staining (bar, 10 µm) and FACS analysis (log10 fluorescence) of bone marrow cells from APL mice treated with RA, acitretin, or NRX for 3 d. Representative experiment of three independent ones. (E) Western blot analysis of PML/RARA levels in APL cells after 3-d in vivo treatment. (F) Quantification by Q-PCR of PML/RARA DNA in bone marrow cells of APL mice after 3- or 6-d treatment with RA, etretinate, or NRX. Means ± SD of three mice per condition. (G) Survival of secondary recipients inoculated with 106 bone marrow cells from 3- or 6-d treated APL mice. 10 mice per group for NRX or etretinate, 20 for RA and controls at 3 d. 8 per group at 6 d. Pooled data from 3 independent experiments. Log rank test was used to evaluate significance of the survival difference between secondary recipients injected with bone marrow cells from RA- or uncoupled retinoid–treated APL mice.
In line with our ex vivo observations, abundance of APL blasts (as assessed by the quantification of PML/RARA DNA in the bone marrow of APL mice) was significantly reduced after 3 (or 6) d of RA-treatment, but, again, was largely unaffected by the two uncoupled retinoids (Fig. 3 F). To directly assess leukemia-propagating activity in the marrows of treated animals, we transplanted 106 bone marrow cells in syngeneic secondary recipients and monitored their survival. In that setting, 3-d treatments with NRX or acitretin yielded modest effects (likely reflecting differentiation), whereas the survival of secondary mice was very significantly enhanced by RA-treatment, with 30% of injected animals never developing the disease (Fig. 3 G, left). An even more dramatic difference was noted using marrows of APL mice treated for 6 d (Fig. 3 G, right).
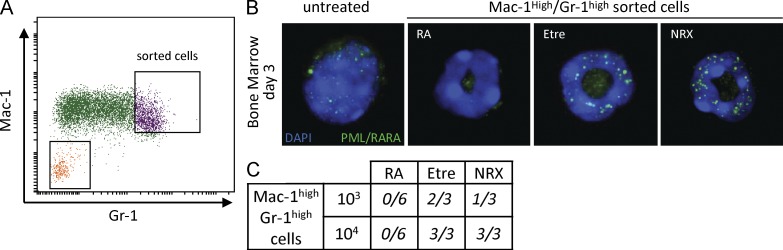
Differentiated blasts still expressing PML/RARA efficiently reinitiate APL
To rule out that leukemia-initiating activity of acitretin- or NRX-treated APL cells (Fig. 3 G) may reflect the presence of remaining undifferentiated blasts in the inoculates, we stringently sorted Mac-1high/Gr-1high cells from APL mice treated for 3 d with RA, NRX, or etretinate (Fig. 4 A). The quality of the sorting was verified by examination of cell morphology on MGG stains and by resorting (unpublished data). As expected, differentiated blasts from NRX- or etretinate-treated animals displayed abundant PML/RARA microspeckles, whereas those from RA-treated animals did not (Fig. 4 B). Strikingly, these cells reinitiated APLs when reinjected in irradiated syngeneic hosts, whereas those from RA-treated mice never did, even when 105 cells were reinjected (Fig. 4 C and not depicted). We cannot formally exclude the presence of very rare undifferentiated cells in the inoculum, despite their absence in 100-fold excess cells of RA-treated APL mice, which exhibit similar patterns and kinetics of differentiation. Interestingly, the resulting leukemia exhibited classical promyelocytic features, illustrating in vivo dedifferentiation of the terminally differentiated APL cells used for inoculation. Collectively, these data pharmacologically establish the uncoupling of differentiation and APL regression in vivo and underscore the key role of PML/RARA degradation in APL eradication.
Figure 4.
APL transplantation by inoculation of PML/RARA-expressing, terminally differentiated APL cells. (A) FACS sorting of the Mac-1high/Gr-1high cells from the bone marrow of APL mice treated for 3 d with RA, NRX, or acitretin (log10 fluorescence). (B) Immunofluorescence analysis of PML reveals nuclear PML/RARA microspeckles in bone marrow cells from 3-d NRX- or etretinate-treated mice (bar, 10 µm). Representative cell obtained in two different experiments. (C) Death by APL of sublethally irradiated syngeneic recipients inoculated with cells (103 or 104) sorted in A.
Our findings have important implications for basic retinoid pharmacology because they demonstrate the existence of drugs that only activate (such as NRX or etretinate) or that activate and degrade (such as RA), revealing new perspectives for retinoid pharmacology and underscoring the importance of determining the structural bases for these differences. In APL, our data formally demonstrate that RA-elicited transcriptional activation promotes cell differentiation, whereas only PML/RARA loss fully abolishes leukemia-initiating activity. Sustained levels of RARA or PML/RARA protein may be required for self-renewal, independent from the transcriptional status of direct target genes, although it remains possible that a small subset of targets is differentially regulated by the three retinoids. Our findings explain why many retinoids, like etretinate, that are not efficient RARA degraders promoted some ex vivo and even in vivo tumor differentiation in patients, but failed to clear the disease (Breitman et al., 1981; Flynn et al., 1983; Sampi et al., 1985), an endpoint only later achieved by all-trans-RA (Huang et al., 1988). They also explain why genetically RA-resistant APLs undergo terminal differentiation through rexinoid-mediated transcriptional activation by the PML/RARA-RXRA complex (Guillemin et al., 2002; Altucci et al., 2005), but fail to regress upon treatment because PML/RARA is not efficiently degraded. Many leukemia-associated fusions repress differentiation genes. These fusions have been targeted by several transcription-modulating agents, such as cytokines or histone deacetylase inhibitors (Johnstone, 2002; Altucci et al., 2005; Leiva et al., 2012). Our results suggest that even if those drugs achieve transcriptional reactivation and restore differentiation, they are unlikely to clear the disease. Finally, these observations unify the modes of action of RA and arsenic and shed light on the dramatic synergy between RA and arsenic in mice or patients (Lallemand-Breitenbach et al., 1999; Rego et al., 2000; Hu et al., 2009; de Thé and Chen, 2010). Oncoprotein degradation may thus represent a feasible and efficient therapeutic option in other malignancies (Ablain et al., 2011).
MATERIALS AND METHODS
Chemicals, cell culture, and viruses.
PML/RARA and RARA transduction of lineage negative (Lin−) primary hematopoietic progenitors was performed exactly as previously described (Du et al., 1999). ATRA, Acitretin (Sigma-Aldrich), or NRX195183 (gift from R. Chandraratna, Allergan, Irvine, CA) were used at the indicated concentrations. After a 1-wk treatment, colonies were counted and cells were harvested, analyzed, or replated in methylcellulose medium for an additional week.
Immortalized MEFs from which the three RARs were excised (provided by P. Chambon, Institut de génétique et de biologie moléculaire et cellulaire, Strasbourg, France) were transduced with MSCV retroviruses expressing RARA or PML/RARA as described in Zhou et al., 2006. Cells were cultured in DMEM containing 10% FBS and treated for 4 or 8 h before gene and protein expression analysis. Reporter plasmid RARE-3-Tk-Luc (de Thé et al., 1990) was transfected into rars−/− MEFs transduced or not with RARA or PML/RARA, and luciferase activity was monitored.
Animal experiments and cell analyses.
Mouse work was performed as previously described (Nasr et al., 2008) in accordance with established institutional guidance and approved protocols from the Comité Régional d’Ethique Expérimentation Animale n°4, which enforces the EU 86/609 directive. 25 mg/kg/d of acitretin and etretinate (the precursor of acitretin; Santa Cruz Biotechnology, Inc.) or 50 mg/kg/day NRX were administered intraperitoneally. ATRA (Innovative Research of America) was administered as subcutaneous 10-mg pellets that consistently released a daily quantity of drug (0.5 mg). Determination of blood levels was performed as previously reported (Nasr et al., 2008). Log-rank test on Kaplan-Meier analysis was used to evaluate statistical significance of survival differences.
Real-time PCR for the quantification of gene expression or PML-RARA DNA, protein analyses by Western Blot, or immunofluorescence, flow cytometry analysis, and cell-sorting procedures were previously described (Nasr et al., 2008). All microscopy observations of immunofluorescence or MGG stains were made using an Axiovert 200M (60× lens, NA 1.4, oil; Carl Zeiss) or an Olympus BX63 (40× lens), respectively.
Array analyses.
Samples were hybridized on Affymetrix Mouse Gene 1.1 ST Arrays and log2 measures were obtained using RMA normalization. For each condition, the fold induction between treatment and control was calculated based on averaged expression measures.
Acknowledgments
We warmly thank P. Chambon for rara,b,g−/− MEFs. We thank F. Jollivet, C. Berthier, and H. Soilihi for technical help; M. Pla for animal facility; B. Gourmel for HPLC/mass spectrometry analyses; N. Setterblad for cell sorting; and all members of the Biophenics laboratory. We thank all laboratory members for helpful discussions; M. Dawson for advice; and F. Sigaux, J.C. Gluckman, and laboratory members for critical reading of the manuscript.
The laboratory is supported by Institut National de la Santé et de la Recherche Médicale, Centre National de la Recherche Scientifique, University Paris Diderot, Institut Universitaire de France, Ligue Nationale contre le Cancer, Institut National du Cancer, Canceropole & Region Ile de France, Prix Griffuel and the European Research Council (Senior grant 268729-STEMAPL to H. de Thé). J. Ablain was supported by a fellowship from Ecole Polytechnique and Fondation ARC. M. Leiva was supported by a Marie Curie intra-European fellowship (PIEF-GA-2009-254256).
The authors have no conflict of interest to disclose.
Footnotes
Abbreviations used:
- APL
- acute promyelocytic leukemia
- RA
- retinoic acid
References
- Ablain J., Nasr R., Bazarbachi A., de Thé H. 2011. The drug-induced degradation of oncoproteins: an unexpected Achilles’ heel of cancer cells? Cancer Discovery. 1:117–127 10.1158/2159-8290.CD-11-0087 [DOI] [PubMed] [Google Scholar]
- Altucci L., Rossin A., Hirsch O., Nebbioso A., Vitoux D., Wilhelm E., Guidez F., Schiavone E.M., Grimwade D., Zelent A., et al. 2005. Rexinoid-triggered differentiation and tumor-selective apoptosis of acute myeloid leukemia by protein kinase A-mediated desubordination of retinoid X receptor. Cancer Res. 65:8754–8765 10.1158/0008-5472.CAN-04-3569 [DOI] [PubMed] [Google Scholar]
- Beard R.L., Duong T.T., Teng M., Klein E.S., Standevan A.M., Chandraratna R.A. 2002. Synthesis and biological activity of retinoic acid receptor-alpha specific amides. Bioorg. Med. Chem. Lett. 12:3145–3148 10.1016/S0960-894X(02)00647-9 [DOI] [PubMed] [Google Scholar]
- Breitman T.R., Collins S.J., Keene B.R. 1981. Terminal differentiation of human promyelocytic leukemic cells in primary culture in response to retinoic acid. Blood. 57:1000–1004 [PubMed] [Google Scholar]
- Brown D., Kogan S., Lagasse E., Weissman I., Alcalay M., Pelicci P.G., Atwater S., Bishop J.M. 1997. A PMLRARalpha transgene initiates murine acute promyelocytic leukemia. Proc. Natl. Acad. Sci. USA. 94:2551–2556 10.1073/pnas.94.6.2551 [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Thé H., Chen Z. 2010. Acute promyelocytic leukaemia: novel insights into the mechanisms of cure. Nat. Rev. Cancer. 10:775–783 10.1038/nrc2943 [DOI] [PubMed] [Google Scholar]
- de Thé H., Vivanco-Ruiz M.M., Tiollais P., Stunnenberg H., Dejean A. 1990. Identification of a retinoic acid responsive element in the retinoic acid receptor beta gene. Nature. 343:177–180 10.1038/343177a0 [DOI] [PubMed] [Google Scholar]
- Du C., Redner R.L., Cooke M.P., Lavau C. 1999. Overexpression of wild-type retinoic acid receptor alpha (RARalpha) recapitulates retinoic acid-sensitive transformation of primary myeloid progenitors by acute promyelocytic leukemia RARalpha-fusion genes. Blood. 94:793–802 [PubMed] [Google Scholar]
- Flynn P.J., Miller W.J., Weisdorf D.J., Arthur D.C., Brunning R., Branda R.F. 1983. Retinoic acid treatment of acute promyelocytic leukemia: in vitro and in vivo observations. Blood. 62:1211–1217 [PubMed] [Google Scholar]
- Geng F., Wenzel S., Tansey W.P. 2012. Ubiquitin and proteasomes in transcription. Annu. Rev. Biochem. 81:177–201 10.1146/annurev-biochem-052110-120012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guillemin M.C., Raffoux E., Vitoux D., Kogan S., Soilihi H., Lallemand-Breitenbach V., Zhu J., Janin A., Daniel M.T., Gourmel B., et al. 2002. In vivo activation of cAMP signaling induces growth arrest and differentiation in acute promyelocytic leukemia. J. Exp. Med. 196:1373–1380 10.1084/jem.20021129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu J., Liu Y.F., Wu C.F., Xu F., Shen Z.X., Zhu Y.M., Li J.M., Tang W., Zhao W.L., Wu W., et al. 2009. Long-term efficacy and safety of all-trans retinoic acid/arsenic trioxide-based therapy in newly diagnosed acute promyelocytic leukemia. Proc. Natl. Acad. Sci. USA. 106:3342–3347 10.1073/pnas.0813280106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang M.E., Ye Y.C., Chen S.R., Chai J.R., Lu J.X., Zhoa L., Gu L.J., Wang Z.Y. 1988. Use of all-trans retinoic acid in the treatment of acute promyelocytic leukemia. Blood. 72:567–572 [PubMed] [Google Scholar]
- Ito K., Bernardi R., Morotti A., Matsuoka S., Saglio G., Ikeda Y., Rosenblatt J., Avigan D.E., Teruya-Feldstein J., Pandolfi P.P. 2008. PML targeting eradicates quiescent leukaemia-initiating cells. Nature. 453:1072–1078 10.1038/nature07016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnstone R.W. 2002. Histone-deacetylase inhibitors: novel drugs for the treatment of cancer. Nat. Rev. Drug Discov. 1:287–299 10.1038/nrd772 [DOI] [PubMed] [Google Scholar]
- Kastner P., Lawrence H.J., Waltzinger C., Ghyselinck N.B., Chambon P., Chan S. 2001. Positive and negative regulation of granulopoiesis by endogenous RARalpha. Blood. 97:1314–1320 10.1182/blood.V97.5.1314 [DOI] [PubMed] [Google Scholar]
- Lallemand-Breitenbach V., de Thé H. 2010. PML nuclear bodies. Cold Spring Harb. Perspect. Biol. 2:a000661 10.1101/cshperspect.a000661 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lallemand-Breitenbach V., Guillemin M.-C., Janin A., Daniel M.-T., Degos L., Kogan S.C., Bishop J.M., de Thé H. 1999. Retinoic acid and arsenic synergize to eradicate leukemic cells in a mouse model of acute promyelocytic leukemia. J. Exp. Med. 189:1043–1052 10.1084/jem.189.7.1043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leiva M., Moretti S., Soilihi H., Pallavicini I., Peres L., Mercurio C., Dal Zuffo R., Minucci S., de Thé H. 2012. Valproic acid induces differentiation and transient tumor regression, but spares leukemia-initiating activity in mouse models of APL. Leukemia: official journal of the Leukemia Society of America, Leukemia Research Fund, U.K [DOI] [PubMed]
- Louisse J., Gönen S., Rietjens I.M., Verwei M. 2011. Relative developmental toxicity potencies of retinoids in the embryonic stem cell test compared with their relative potencies in in vivo and two other in vitro assays for developmental toxicity. Toxicol. Lett. 203:1–8 10.1016/j.toxlet.2011.02.012 [DOI] [PubMed] [Google Scholar]
- Melnick A., Licht J.D. 1999. Deconstructing a disease: RARalpha, its fusion partners, and their roles in the pathogenesis of acute promyelocytic leukemia. Blood. 93:3167–3215 [PubMed] [Google Scholar]
- Nasr R., Guillemin M.C., Ferhi O., Soilihi H., Peres L., Berthier C., Rousselot P., Robledo-Sarmiento M., Lallemand-Breitenbach V., Gourmel B., et al. 2008. Eradication of acute promyelocytic leukemia-initiating cells through PML-RARA degradation. Nat. Med. 14:1333–1342 10.1038/nm.1891 [DOI] [PubMed] [Google Scholar]
- Quignon F., Chen Z., de Thé H. 1997. Retinoic acid and arsenic: towards oncogene-targeted treatments of acute promyelocytic leukaemia. Biochim. Biophys. Acta. 1333:M53–M61 [DOI] [PubMed] [Google Scholar]
- Rego E.M., He L.Z., Warrell R.P., Jr, Wang Z.G., Pandolfi P.P. 2000. Retinoic acid (RA) and As2O3 treatment in transgenic models of acute promyelocytic leukemia (APL) unravel the distinct nature of the leukemogenic process induced by the PML-RARalpha and PLZF-RARalpha oncoproteins. Proc. Natl. Acad. Sci. USA. 97:10173–10178 10.1073/pnas.180290497 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sampi K., Honma Y., Hozumi M., Sakurai M. 1985. Discrepancy between in-vitro and in-vivo inductions of differentiation by retinoids of human acute promyelocytic leukemia cells in relapse. Leuk. Res. 9:1475–1478 10.1016/0145-2126(85)90039-6 [DOI] [PubMed] [Google Scholar]
- Zhou J., Pérès L., Honoré N., Nasr R., Zhu J., de Thé H. 2006. Dimerization-induced corepressor binding and relaxed DNA-binding specificity are critical for PML/RARA-induced immortalization. Proc. Natl. Acad. Sci. USA. 103:9238–9243 10.1073/pnas.0603324103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu J., Gianni M., Kopf E., Honoré N., Chelbi-Alix M., Koken M., Quignon F., Rochette-Egly C., de Thé H. 1999. Retinoic acid induces proteasome-dependent degradation of retinoic acid receptor alpha (RARalpha) and oncogenic RARalpha fusion proteins. Proc. Natl. Acad. Sci. USA. 96:14807–14812 10.1073/pnas.96.26.14807 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu J., Zhou J., Peres L., Riaucoux F., Honoré N., Kogan S., de Thé H. 2005. A sumoylation site in PML/RARA is essential for leukemic transformation. Cancer Cell. 7:143–153 10.1016/j.ccr.2005.01.005 [DOI] [PubMed] [Google Scholar]