Abstract
Objective
To relate serum leptin levels to prevalent and incident radiographic knee osteoarthritis (OAK) and to determine if patterns of change in longitudinal serum leptin measures differ by knee OA status over a 10-year period.
Methods
Participants in the Michigan Study of Women’s Health Across the Nation underwent bilateral knee radiographs at baseline and follow-up visits 2, 4 and 11 for ascertainment of OAK status (Kellgren-Lawrence score ≥ 2). Serum leptin measures were available from baseline, follow-up visits 1 and 3–7.
Results
The baseline prevalence of OAK (average age 46 years) was 18%; the two-year incidence of OAK at follow-up visits 2 and 4 was 18% and 14%, respectively. Serum leptin levels were associated with prevalent and incident OAK. A 5 ng/mL increase in serum leptin was associated with 38% higher odds of prevalent OAK (OR=1.38, 95% CI 1.26, 1.52) and with 31% greater odds of incident OAK (OR=1.31, 95% CI 1.21, 1.41) after adjustment for covariates including BMI residuals. Leptin levels increased with time; on average, serum leptin levels increased by 0.38 ng/mL per year (p=0.0004). Women with incident OAK during the 10-year follow-up had consistently higher serum leptin levels as compared to women with no OAK during follow-up.
Conclusions
Our findings support a metabolic role of obesity on knee OA. Better understanding of the mechanisms by which increased fat mass is associated with joint damage is needed. Management of cardiometabolic dysfunction, including elevated serum leptin levels may be beneficial in forestalling the onset or progression of knee OA.
INTRODUCTION
As the leading cause of pain, functional limitations and disability in the United States (1), osteoarthritis is associated with decreased productivity and increased health expenditures (2). In 2003, the cost of medical care expenditures and earnings losses associated with arthritis and rheumatism was an estimated $128 billion (3). Osteoarthritis (OA), a joint condition characterized by loss of articular cartilage, subchondral bone remodeling, soft tissue damage and inflammation affects more than 26 million U.S. adults over the age of 25 (4).
OA disproportionately afflicts women and prevalence rises dramatically after the menopausal transition (5,6). However, disagreements persist as to whether the menopause, the accompanying change in hormone levels or some other physiologic processes occurring during the mid-life contribute to OA pathogenesis. Support for the importance of menopause-associated “estrogen deficiency” as a risk factor for knee OA has been mixed (7–11). Better characterization of the menopause transition has provided evidence that it is a time of hormonal change but also dramatic metabolic changes including decreased energy expenditure (12), changes in body composition and topology (13,14) and increased risk of metabolic syndrome (15).
Obesity is a well-documented risk factor for knee OA (16–23) and the impact of obesity on osteoarthritis onset and progression is likely due to several mechanisms. Some investigators have focused on the impact of obesity as a sheer mechanical force causing increased joint loading and subsequent damage to the articular cartilage (24–26). However, associations between obesity and OA in non-weight bearing joints such as those in the hands and/or wrists (23,27–29) suggest that alternative mechanisms impact the OA-obesity relationship and emphasize the role of adipose tissue.
There is emerging evidence about the active metabolic environment of chondrocytes, including glucose transport, cholesterol efflux, and lipid metabolism (30). These findings have prompted the consideration of novel obesity-related biomarkers in studies of osteoarthritis and have suggested that there may be shared pathophysiology between osteoarthritis, cardiovascular and metabolic diseases. Adipose tissue is now recognized as an endocrine organ as adipocytes have the ability to secrete active agents including adipokines (31). Efforts to examine the adipokines with respect to OA have focused on leptin because of its strong correlation with body size. Leptin levels in synovial fluid are correlated with the severity of knee OA (32) and leptin and its receptor have been identified in many joint tissues including human chondrocytes, osteophytes (33,34), synovium and infrapatellar fat pad (35).
Leptin might be an important link between obesity and osteoarthritis (30,36–39), but epidemiologic evidence of such a relationship is limited, possibly because few studies of OA have leptin measures available. No studies have evaluated whether changes in leptin are associated with osteoarthritis despite evidence that changes in body size are associated with joint damage (40,41). Thus, the goal of this investigation was to describe the relationship between serum leptin measures and knee OA prevalence and incidence and to determine whether changes in serum leptin levels over time differed by OA status in a mid-aged population of women.
MATERIALS AND METHODS
The Michigan Study of Women’s Health Across the Nation (SWAN) is one of seven sites for SWAN, a multiethnic cohort study characterizing the menopausal transition. The Michigan SWAN population, established in 1996, is a population-based sample of women from two Detroit-area communities identified through a community census based on electrical utility listings. A total of 543 eligible women were recruited from the Michigan site, including 325 African American and 218 Caucasian women. Eligibility criterion at baseline included 42–52 years of age, having an intact uterus, having had at least one menstrual period in the previous 3 months, no use of reproductive hormones in the previous 3 months, and self-identification with the site’s designated race/ethnic group (either African American or Caucasian at Michigan).
At the 1996 baseline, Michigan SWAN women completed the assessment protocol common to all SWAN sites; then a supplemental protocol including radiographs was implemented. Women were seen for annual follow-up visits, although the supplemental osteoarthritis protocol was included only at visits baseline, 2, 4, and 11. Participation at the annual assessments has been excellent, with 80% seen at follow-up visit 11.
Although the number of women participating in the radiograph protocol varied by year, there were few differences among those who participated and those who did not. Race and smoking status varied with annual participation; at follow-up visit 2, non-participants were more likely to be African-American and current smokers whereas at follow-up visit 4, non-participants were more likely to be Caucasian and at follow-up visit 11, current smokers were more likely to participate.
The University of Michigan Institutional Review Board approved the study protocol, and written informed consent was obtained from each participant.
Osteoarthritis Measures
Anterior-posterior radiographs of the knees have been taken weight-bearing in the semi-flexed position (42). Radiographs taken at baseline and follow-up visits 2 and 4 were obtained using General Electric radiograph equipment (model X-GE MPX-80; General Electric Medical Systems, Milwaukee, Wisconsin). Radiographs from follow-up visit 11 were obtained with the AXIOM Aristos radiographic system with integrated digital flat detector technology (Siemens, Erlangen, Germany). Knees were scored using the Kellgren and Lawrence (K-L) grading system of the Atlas of Standard Radiographs of Arthritis (43) such that 0=normal; 1=doubtful OA; 2=minimal OA; 3=moderate OA; 4=severe OA. Participants with artificial knee replacements were assigned a K-L score of 4. Prevalent knee osteoarthritis was defined as at least one knee with a K-L score ≥ 2 at a given visit. Incident knee osteoarthritis was defined new knee osteoarthritis (K-L score ≥ 2) in either knee given that the participant had a K-L score of 0 or 1 in both knees during the prior data collection cycle.
Leptin Assay
The SWAN specimen collection protocol includes a fasted blood draw to provide samples for a specimen repository that is maintained at −80°C until processing. Serum leptin levels were determined spectrophotometrically using commercially-available colorimetric enzyme immunoassay kits (Millipore, St. Charles, MO) and run according to the manufacturer’s instructions. The coefficient of variation percent for duplicate samples was 3.7% and the lower limit of detection is 0.5 ng/mL. Banked serum specimens from visits baseline, 1 and 3–7 were assayed for leptin.
Other Measures
At each annual examination, height (cm) and weight (kg) was measured using a stadiometer and calibrated balance-beam scale, and used to calculate body mass index (BMI). Waist (cm) and hip (cm) circumferences have been measured annually, using a non-stretchable tape 3 cm above the umbilicus, after a relaxed expiration, and the maximum girth around the buttocks, respectively.
Menopause status was ascertained at each annual exam based on questions about bleeding patterns, current hormone use, hysterectomy and oophorectomy. Participants were categorized as being premenopausal (regular menses with bleeding in the past three months), early perimenopausal (bleeding in the past three months but increasing irregularity in menses), late perimenopausal (bleeding in the past year but not in past three months), postmenopausal (no bleeding for 12 months), hysterectomy, or unable to determine due to exogenous hormone use.
Race/ethnicity classification (African American or Caucasian) and annual current smoking status (yes/no) and was determined by self-report. Age at each visit was calculated as visit date minus birth date.
Statistical Analysis
Means and standard deviations (SD) or frequencies and percents of leptin, body size variables and relevant covariates were examined overall and by knee OA status. The statistical significance of differences by OA status were evaluated using t-tests, analysis of variance, or chi-square tests.
To fully utilize the richness of the available data, including multiple measures of knee OA status and annual assessment of serum leptin through follow-up visit 7, three analytical approaches were employed to relate serum leptin measures and knee OA status. In the first two approaches, the outcome of interest was knee osteoarthritis whereas in the third approach, leptin was the outcome. First, to determine the association of leptin levels and knee OA prevalence at baseline, we examined the cross-sectional association of serum leptin and knee OA using multivariable logistic regression analysis.
Second, to determine the association of leptin levels and incident knee OA, discrete-time survival analysis techniques were utilized to model the time to incident OA at follow-up visits 2, 4 and 11 as a function of serum leptin levels. To complete this analysis, a dataset was constructed with multiple observations per participant; each row in the dataset represented a study visit in which the participant was at risk of knee OA onset through follow-up visit 11. Once women developed knee OA, data from subsequent years of follow-up was not included in the dataset. The discrete-time logistic survival model was then estimated using logistic regression whereby the odds ratios are the effect estimates of interest. The incidence of knee OA at each follow-up visit was calculated as the number of new cases of knee OA at a given visit divided by the number of women who remained at risk for knee OA. As serum leptin levels were not available at follow-up visits 2 or 11, values from follow-up visits 1 and 7 were substituted, respectively.
Third, serum leptin levels from baseline to follow-up visit 7 were evaluated overall and by prevalent, incident, or no knee OA status through follow-up visit 11. Then, linear mixed models (PROC MIXED) with random intercepts and slopes for age were used to examine level and change in serum leptin measures over time. Osteoarthritis status by time interactions in the model evaluated whether the rates of change in serum leptin measures differed between women with prevalent, incident or no knee OA through follow-up visit 11. SAS PROC SGPLOT was used to graph predicted trajectories of serum leptin measures with corresponding 95% confidence intervals for each knee OA group.
Due to the collinearity between body size and serum leptin (r=0.73, P<0.0001), all multivariable modeling included residuals of BMI as the measure of body size confounding. The BMI residual variable represents the variation in BMI that remains following simple regression of BMI on leptin. Given that serum leptin represents the metabolic component of body size, the BMI residual represents the association of body size and OA through other pathways, including mechanical loading. Interactions of the BMI residual and serum leptin were tested to assess potential effect modification of the relationship between leptin and knee OA by body size. A sensitivity analysis was conducted to examine the consistency of the results after adjustment for waist-to-hip ratio instead of the BMI residuals. When adjusting for waist-to-hip ratio, the findings remained consistent although the estimates for leptin were attenuated by 14% (data not shown).
Model fit and final model selection was based on the Akaike’s information criterion and chi-square tests comparing the log likelihood ratios between candidate models. Models were adjusted for age, race/ethnicity, menopause status (or hysterectomy yes/no), smoking status, and BMI residuals, as appropriate. Statistical significance was defined at α<0.05 and all analyses were completed using SAS v9.3 (SAS Institute, Cary, NC).
RESULTS
The prevalence of radiographically-defined knee OA increased over the ten-year follow-up period. At baseline (mean age=46 years), 18% of participants had knee OA; at follow-up visit 11, 65% of women had knee OA (Table 1). Similarly, the prevalence of moderate to severe OA (K-L score of 3 or 4) changed from 4% at baseline to 28% ten years later.
Table 1.
Descriptive characteristics of the Michigan Study of Women’s Health Across the Nation (SWAN) sample at baseline, follow-up visit 04 and follow-up visit 11.
| Baseline N=542 |
Visit 04 N=252 |
Visit 11 N=387 |
|
|---|---|---|---|
|
| |||
| Mean (SD) | Mean (SD) | Mean (SD) | |
|
|
|||
| Age (years) | 46.1 (2.7) | 50.2 (2.7) | 56.9 (2.8) |
| Weight (kg) | 85.8 (21.8) | 87.9 (22.1) | 90.1 (22.2) |
| Height (cm) | 163.5 (6.2) | 162.8 (5.8) | 162.6 (6.2) |
| BMI (kg/m2) | 32.1 (8.0) | 33.2 (8.3) | 34.1 (8.4) |
| Waist circumference (cm) | 94.1 (17.1) | 98.5 (17.6) | 102.3 (17.6) |
| Hip circumference (cm) | 113.9 (16.2) | 115.4 (17.0) | 118.1 (16.9) |
| Waist:hip ratio | 0.82 (0.07) | 0.85 (0.08) | 0.87 (0.08) |
| Leptin (ng/mL) | 30.6 (18.3) | 34.4 (20.1) | ----- |
| n (%) | n (%) | n (%) | |
|
|
|||
| Knee Osteoarthritis | 98 (18.1%) | 109 (43.3%) | 251 (64.9%) |
| K-L Score | |||
| 0 | 322 (59.4%) | 61 (24.2%) | 44 (11.4%) |
| 1 | 122 (22.5%) | 79 (31.4%) | 89 (23.0%) |
| 2 | 78 (14.4%) | 84 (33.3%) | 147 (38.0%) |
| 3 | 19 (3.5%) | 27 (10.7%) | 62 (16.0%) |
| 4 | 1 (0.2%) | 1 (0.4%) | 45 (11.6%) |
| Obese (BMI ≥ 30 kg/m2) | 301 (56.1%) | 153 (61.5%) | 250 (64.6%) |
| Race/Ethnicity | |||
| African-American | 324 (59.8%) | 181 (71.8%) | 238 (61.5%) |
| Caucasian | 218 (40.2%) | 71 (28.2%) | 149 (38.5%) |
| Menopause Status | |||
| Premenopausal | 271 (50.3%) | 11 (4.4%) | 0 (0.0%) |
| Early Perimenopausal | 268 (49.7%) | 104 (41.4%) | 12 (3.1%) |
| Late Perimenopausal | 0 (0.0%) | 37 (14.7%) | 15 (3.9%) |
| Postmenopausal | 0 (0.0%) | 51 (20.3%) | 303 (78.3%) |
| Hysterectomy | 0 (0.0%) | 22 (8.8%) | 52 (13.4%) |
| Unknown, hormone use | 0 (0.0%) | 26 (10.4%) | 5 (1.3%) |
| Hormone therapy use | 0 (0.0%) | 45 (17.9%) | 32 (8.3%) |
| Current Smoker | 146 (27.3%) | 63 (25.1%) | 87 (22.5%) |
The mean baseline serum leptin level was 30.6 ng/mL. At follow-up visit 7, the average serum leptin level was 38.0 ng/mL (Appendix 1); we observed a statistically significant increasing trend in serum leptin levels over time (P<0.0001). Serum leptin levels were 43% higher at baseline among women with knee OA as compared to those without knee OA (P <0.0001). Serum leptin levels were not different according to race/ethnicity, age, menopause status, or smoking status (Table 2).
Table 2.
Descriptive Characteristics of the Michigan Study of Women’s Health Across the Nation (SWAN) Sample at Baseline and Follow-Up Visit 11, by Knee Osteoarthritis (OA) Status.
| Baseline | Follow-up Visit 11 | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| No OA Mean (SD) | OA Mean (SD) | P-value | No OA Mean (SD) | OA Mean (SD) | P-value | |
|
| ||||||
| Age (years) | 46.1 (2.8) | 46.0 (2.6) | 0.73 | 56.6 (2.8) | 57.1 (2.8) | 0.07 |
| Weight (kg) | 82.2 (20.0) | 101.8 (22.5) | <0.0001 | 74.9 (15.7) | 98.0 (21.0) | <0.0001 |
| Height (cm) | 163.5 (6.2) | 163.3 (6.4) | 0.85 | 162.3 (6.5) | 162.8 (6.0) | 0.48 |
| BMI (kg/m2) | 30.8 (7.3) | 38.1 (8.5) | <0.0001 | 28.4 (5.9) | 37.1 (7.9) | <0.0001 |
| Waist circumference (cm) | 91.5 (16.0) | 105.4 (17.5) | <0.0001 | 91.1 (15.0) | 108.1 (16.0) | <0.0001 |
| Hip circumference (cm) | 111.3 (14.9) | 125.5 (17.1) | <0.0001 | 107.1 (13.0) | 123.9 (15.8) | <0.0001 |
| Waist:hip ratio | 0.82 (0.07) | 0.84 (0.07) | 0.02 | 0.85 (0.08) | 0.87 (0.08) | 0.003 |
| Leptin (ng/mL) | 28.4 (17.2) | 40.6 (20.1) | <0.0001 | ----- | ----- | |
| n (%) | n (%) | n (%) | n (%) | |||
|
|
|
|||||
| Obese (BMI ≥ 30 kg/m2) | 221 (50.0%) | 80 (84.2%) | <0.0001 | 48 (36.1%) | 202 (79.5%) | <0.0001 |
| Ethnicity | ||||||
| African-American | 249 (56.1%) | 75 (76.5%) | 0.0002 | 75 (56.4%) | 163 (64.2%) | 0.14 |
| Caucasian | 195 (43.9%) | 23 (23.5%) | 58 (43.6%) | 91 (35.8%) | ||
| Menopause Status | ||||||
| Premenopausal | 230 (52.2%) | 41 (41.8%) | 0.06 | 0 (0.0%) | 0 (0.0%) | 0.01 |
| Early Perimenopausal | 211 (47.9%) | 57 (58.2%) | 9 (6.8%) | 3 (1.2%) | ||
| Late Perimenopausal | 0 (0.0%) | 0 (0.0%) | 6 (4.5%) | 9 (3.5%) | ||
| Postmenopausal | 0 (0.0%) | 0 (0.0%) | 105 (79.0%) | 198 (78.0%) | ||
| Hysterectomy | 0 (0.0%) | 0 (0.0%) | 12 (9.0%) | 40 (15.8%) | ||
| Unknown, hormone use | 0 (0.0%) | 0 (0.0%) | 1 (0.8%) | 4 (1.6%) | ||
| Hormone therapy use | 0 (0.0%) | 0 (0.0%) | N/A | 13 (9.8%) | 19 (7.5%) | 0.44 |
| Current Smoker | 121 (27.8%) | 25 (25.5%) | 0.65 | 40 (30.1%) | 47 (18.5%) | 0.01 |
Fifty-six percent of all participants were obese at baseline in 1996/7; by follow-up visit 11, the prevalence of obesity increased to 64.6%. Body size measures, with the exception of height, increased significantly over the study period and were 15–30% greater among women with knee OA as compared to those without knee OA.
By design, 60% of participants were African-American and 40% were Caucasian. In accordance with the inclusion criterion, all participants were pre- or early peri-menopausal at baseline and were not using exogenous hormones. By follow-up visit 11, most women (78%) were postmenopausal and only 8% were using exogenous hormones. Menopause status differed by OA status at follow-up visit 11 (P=0.02); women with OA were more likely to have had a hysterectomy as compared to women without knee OA.
The proportion of women that were current smokers declined slightly over time; at baseline, 27% of women were current smokers whereas 23% were current smokers at follow-up visit 11. The proportion of current smokers was similar among women with and without knee OA at baseline; however, at follow-up visit 11, women with knee OA were less likely to be current smokers as compared to women without knee OA (19% vs. 29%, respectively) (P=0.02).
Cross-sectional analysis relating leptin levels to prevalent knee OA
Baseline serum leptin levels were positively and significantly associated with prevalent knee OA (Table 3). A 5 ng/mL increase in serum leptin was associated with 38% greater odds of having knee OA after adjustment for age, race/ethnicity, menopause status, current smoking status, and BMI residuals [95% confidence interval (CI) 1.26, 1.52]. African American women had 2.6 times greater odds of having knee OA at baseline as compared to Caucasian women (95% CI 1.46, 4.46).
Table 3.
Cross-sectional analysis of the relationship between serum leptin values and knee osteoarthritis status at baseline visit among Michigan Study of Women’s Health Across the Nation (SWAN) participants, adjusted for age, body mass index residuals, race/ethnicity, menopause status and baseline smoking status.
| Odds Ratio | 95% Confidence Interval | |
|---|---|---|
|
|
||
| Leptin* | 1.38 | 1.26, 1.52 |
| Age | 1.00 | 0.92, 1.10 |
| African American vs. Caucasian race/ethnicity | 2.55 | 1.46, 4.46 |
| Early peri-menopausal vs. premenopausal | 1.57 | 0.95, 2.60 |
| Current vs. not current smoker | 1.05 | 0.58, 1.90 |
Estimate represents 5 ng/mL change in leptin value.
Serum leptin levels and time to incident knee OA
The two-year incidence of knee OA at follow-up visits 2 and 4 was 18% and 14%, respectively. At follow-up visit 11, the 7-year incidence of knee OA was 47%. After adjustment for baseline age, race/ethnicity, baseline smoking status, and BMI residuals, higher serum leptin levels were associated with incident knee OA (Table 4). A 5 ng/mL higher serum leptin level was associated with 31% greater odds of incident knee OA (95% CI 1.21, 1.41). African American women had 52% greater odds of incident knee OA (95% CI 1.00, 2.30) as compared to Caucasian women. Baseline age and current smoking status were associated with lower odds of incident knee OA. A 1 year increase in baseline age was associated with 14% decreased odds of incident knee OA (95% CI 0.83, 0.88). Those who were current smokers had 52% decreased odds of having incident knee OA as compared to those who were not current smokers (95% CI 0.29, 0.80).
Table 4.
Discrete survival time analysis of relationship between serum leptin values and incident knee osteoarthritis among Michigan Study of Women’s Health Across the Nation (SWAN) participants, baseline to follow-up visit 11, adjusted for age, body mass index residuals, race/ethnicity, and baseline smoking status.
| Odds Ratio | 95% Confidence Interval | |
|---|---|---|
|
|
||
| Leptin* | 1.31 | 1.21, 1.41 |
| Baseline age | 0.86 | 0.83, 0.88 |
| African American race/ethnicity | 1.52 | 1.00, 2.30 |
| Baseline current vs. not current smoker | 0.48 | 0.29, 0.80 |
Estimate represents 5 ng/mL change in leptin value.
As a sensitivity analysis, incident knee OA cases were restricted to only those individuals with a KL=0 at baseline and findings were similar. A 5 ng/mL higher serum leptin level was associated with 30% greater odds of incident knee OA (95% CI 1.18, 1.44) following adjustment for covariates.
Trajectories of leptin in relation to knee OA status at follow-up visit 11
Serum leptin levels increased as women aged; on average, serum leptin levels increased by 0.38 ng/mL per year (p=0.0004). Serum leptin levels were highest among women with prevalent knee OA at baseline (Figure 1). After adjustment for age, BMI residuals, race/ethnicity, hysterectomy status and baseline smoking status, women with prevalent knee OA at baseline had serum leptin levels that were 21 ng/mL higher as compared to women that remained knee OA free throughout the 10 years of follow-up. Women who developed incident knee OA during follow-up had serum leptin levels that were 14 ng/mL higher as compared to those without knee OA. Most notably, the highest serum leptin levels among those women who never developed knee OA are still lower than those among women with knee OA. Also, the serum leptin levels among those with incident disease during the follow-up do not overlap with levels among those with prevalent disease at baseline. While serum leptin levels differed by knee OA status, there was no statistically significant difference in the slope of the leptin trajectories over time among the groups.
Figure 1.
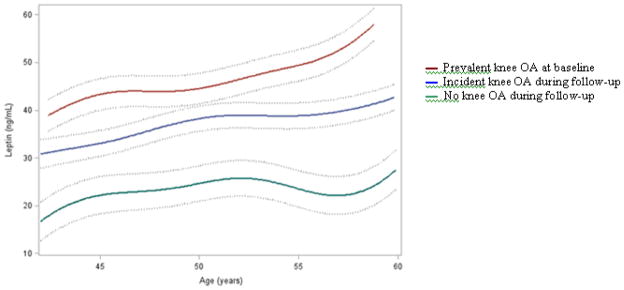
Predicted Trajectories of Serum Leptin (ng/mL) by Knee Osteoarthritis Status Among Michigan Study of Women’s Health Across the Nation (SWAN) Participants, adjusted for Age, Body Mass Index Residuals, Race/Ethnicity, Hysterectomy Status and Baseline Smoking Status.
To examine whether serum leptin levels were associated with knee OA progression, the trajectories of leptin among women with prevalent knee OA at baseline who progressed to moderate/severe knee OA at follow-up visit 11 were compared to those among women who did not progress. Women with prevalent knee OA who progressed had serum leptin levels that were 3.3 ng/mL higher as compared to women with prevalent knee OA who did not progress but this difference was not statistically significant (P=0.35).
DISCUSSION
While leptin may represent an important link between obesity and knee OA (30,36–39), few epidemiological studies have examined this hypothesis. This study is the first to examine serum leptin levels with respect to prevalent and incident knee OA and to relate longitudinal measures of serum leptin to subsequent OA status in a large population-based study. In this cohort of mid-life women, higher serum leptin levels were associated with increased odds of both prevalent and incident knee OA but the rate of change in serum leptin levels over time did not differ by knee OA status. The finding that serum leptin levels at baseline were highest among women with prevalent knee OA as compared to women with 10-year incident knee OA or no knee OA suggest that these women are the most metabolically compromised in terms of high leptin levels. Individuals with prevalent knee OA at baseline were relatively young at disease onset. We hypothesize that metabolic dysfunction may be an important risk factor for knee OA, particularly among younger individuals.
Ku et al. reported that cross-sectional leptin levels (measured in synovial fluid) were related to knee OA severity among a population of knee surgery patients (32). Unlike our study, however, BMI did not differ by knee OA status, suggesting that our population and the Ku et al. population differ with respect to body size. Further, the leptin levels among women in the Michigan SWAN cohort are much higher than those reported by Ku et al.; 74% of the women in our study had baseline leptin levels that were higher than the upper range of values reported among patients in Ku et al. (15.8 ng/mL) (32). Data from the National Health and Nutrition Examination Study (NHANES) III estimates that the average serum leptin value among women in the United States aged ≥ 20 years is 12.7 ng/mL (44), suggesting that the Ku et al. population (32) may have leptin levels lower than the general United States population.
Exploration of the impact of leptin-OA relationship among a cohort of women is of particular interest given the findings that serum leptin levels were the most important cardiometabolic biomarker for knee OA using data from NHANES III (45). Further, differences in synovial leptin levels among OA patients versus controls were greater among women as compared to men (32). Leptin levels are higher among women (46–49) and correlate more strongly with subcutaneous adipose tissue (46–49), the fat depot which is proportionally larger among women as compared to men (50). Our data suggest that leptin may be an important OA biomarker among women.
Mechanistically, leptin has been associated with OA through catabolic or anabolic mechanisms. Leptin has an anabolic effect on chondrocytes and osteoblasts (33), which may be associated with repair of damaged cartilage but also increased osteophyte development. As the K-L scoring system reflects both joint space width (a proxy of cartilage loss) and the presence of osteophytes, the anabolic impact of leptin with respect to radiographically-defined knee OA can not be differentiated. Leptin may also have a catabolic effect on cartilage due to its pro-inflammatory capabilities. Synergistic relationships of leptin and proinflammatory cytokines including interleukin-1 beta (IL-1β), interleukin-6 (IL-6), interleukin-8 (IL-8), matrix metallopeptidase 9 (MMP-9), MMP-13 and nitric oxide have been reported (33,51,52). Increased local inflammation within the joint has a catabolic role in cartilage metabolism (51). It is possible that the proinflammatory impact of leptin may be detrimental to other collagenous tissues within the joint including the meniscus and ligaments.
Our analysis was complicated by the fact that leptin, being a product of adipose tissue, is highly correlated with all measures of body size and greater body size is a hypothesized risk factor for knee OA through non-metabolic mechanisms such as increased joint loading or poor muscle strength. Thus, our analyses were adjusted for the residuals of BMI on leptin in an effort to describe the metabolic impact of obesity (i.e., leptin) on knee OA, over-and-above the non-metabolic effect of greater body size.
Utilization of hand joints may be preferable over knees as the OA phenotype for studies evaluating the metabolic impact of obesity on joint status (53). A recent study using data from NHANES found no association of leptin and hand OA (54). However, in this analysis from Massengale et al. (54), the case definition of hand OA was based upon clinical exam in the absence of hand radiographs. Several studies have documented radiography is superior to physical exam for the characterization of hand OA in epidemiologic studies (55–57) and that use of clinical exam may under-estimate the prevalence of disease. Misclassification of OA status in this way may bias findings towards the null, which could explain the study’s report of no association between leptin and hand OA.
With respect to progression of hand OA, Yusuf et al. (58) reported slightly greater leptin levels (3 ng/mL) among those with progressive hand OA as compared to non-progressive disease (P=0.08). The study may have been under-powered to detect statistically significant differences in leptin given the relatively narrow range of leptin values in this population which included both men and women of normal body size. In addition, all participants in Yusuf et al. cohort had OA in multiple joints suggesting a more advanced level of disease overall. The mechanism by which leptin is associated with incident OA may be different than the mechanism by which leptin is associated with progressive OA. Taken together, the findings with respect to leptin and hand OA are not definitive and call for more work to be done exploring leptin levels among a population including both those with and without radiographic hand OA.
This study examined leptin levels with respect to knee OA prevalence and incidence in a non-clinical population. Strengths unique to this study include longitudinal leptin measures, repeated assessment of knee OA status, and information about potential confounders including body size, menopause status and smoking. The prevalence of knee OA continues to increase in the population, likely because of the aging of the population and the increasing proliferation of obesity. While obesity is a known risk factor for osteoarthritis, better characterization of the mechanisms through which greater fat mass is associated with joint damage will provide important information to aid in prevention and intervention strategies. We have reported here that serum leptin, an adipokine secreted by adipose tissue, is associated with knee OA prevalence and incidence over-and-above the non-metabolic impact of BMI. These findings provide further evidence that body mass influences OA through a metabolic pathway and provides support for the potential utility of serum leptin as a biomarker for OA risk.
Supplementary Material
SIGNIFICANCE AND INNOVATION.
This study is the first to examine serum leptin levels with respect to both prevalent and incident knee OA and to relate baseline and longitudinal measures of serum leptin to subsequent OA status.
Serum leptin levels are associated with prevalent and incident radiographic knee OA in a mid-aged population of women.
Serum leptin levels increase with age; on average, serum leptin levels increased by 0.38 ng/mL per year (p=0.0004) after adjustment for BMI.
We observed complete separation of estimated mean serum leptin levels over time among women with prevalent knee OA at baseline, women with incident knee OA during the 10-year follow-up period and among women who remained OA-free during follow-up. Even the lowest estimated mean serum leptin levels among women with prevalent knee OA at baseline were higher than the highest estimated levels among women with incident or no knee OA during follow-up.
Acknowledgments
Grant Support:
The Study of Women’s Health Across the Nation (SWAN) has grant support from the National Institutes of Health (NIH), DHHS, through the National Institute on Aging (NIA), the National Institute of Nursing Research (NINR) and the NIH Office of Research on Women’s Health (ORWH) (Grants NR004061; AG012505, AG012535, AG012531, AG012539, AG012546, AG012553, AG012554, AG012495, AG017719). This work was additionally supported by AG017104, AG027708 and a Doctoral Dissertation award from the Arthritis Foundation (#5375).
SWAN Clinical Centers: University of Michigan, Ann Arbor – Siobán Harlow, PI 2011 – present, MaryFran Sowers, PI 1994–2011; Massachusetts General Hospital, Boston, MA – Joel Finkelstein, PI 1999 – present; Robert Neer, PI 1994 – 1999; Rush University, Rush University Medical Center, Chicago, IL – Howard Kravitz, PI 2009 – present; Lynda Powell, PI 1994 – 2009; University of California, Davis/Kaiser – Ellen Gold, PI; University of California, Los Angeles – Gail Greendale, PI; Albert Einstein College of Medicine, Bronx, NY – Carol Derby, PI 2011 – present, Rachel Wildman, PI 2010 – 2011; Nanette Santoro, PI 2004 – 2010; University of Medicine and Dentistry – New Jersey Medical School, Newark – Gerson Weiss, PI 1994 – 2004; and the University of Pittsburgh, Pittsburgh, PA – Karen Matthews, PI.
NIH Program Office: National Institute on Aging, Bethesda, MD – Sherry Sherman 1994 – present; Marcia Ory 1994 – 2001; National Institute of Nursing Research, Bethesda, MD – Program Officers.
Central Laboratory: University of Michigan, Ann Arbor – Daniel McConnell (Central Ligand Assay Satellite Services).
SWAN Repository: University of Michigan, Ann Arbor – Dan McConnell 2011; MaryFran Sowers 2000 – 2011.
Coordinating Center: University of Pittsburgh, Pittsburgh, PA – Kim Sutton-Tyrrell, PI 2001 – present; New England Research Institutes, Watertown, MA - Sonja McKinlay, PI 1995 – 2001.
Steering Committee: Susan Johnson, Current Chair
Chris Gallagher, Former Chair
We thank the study staff at each site and all the women who participated in SWAN.
Footnotes
Financial Disclosure:
None of the authors have any financial conflicts of interests to declare.
DISCLAIMER
The content of this manuscript is solely the responsibility of the authors and does not necessarily represent the official views of the NIA, NINR, ORWH or the NIH.
References
- 1.Centers for Disease Control and Prevention (CDC) Prevalence of disabilities and associated health conditions among adults --- United States, 1999. MMWR Morb Mortal Wkly Rep. 2001;50:120–5. [PubMed] [Google Scholar]
- 2.United States Bone and Joint Decade. The Burden of Musculoskeletal Diseases in the United States. Rosemont, IL: American Academy of Orthopedic Surgeons; 2008. pp. 71–96. [Google Scholar]
- 3.Yelin E, Murphy L, Cisternas MG, Foreman AJ, Pasta DJ, Helmick CG. Medical care expenditures and earnings losses among persons with arthritis and other rheumatic conditions in 2003, and comparisons with 1997. Arthritis Rheum. 2007;56:1397–407. doi: 10.1002/art.22565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lawrence RC, Felson DT, Helmick CG, Arnold LM, Choi H, Deyo RA, et al. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part II Arthritis Rheum. 2008;58:26–35. doi: 10.1002/art.23176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Srikanth VK, Fryer JL, Zhai G, Winzenberg TM, Hosmer D, Jones G. A meta-analysis of sex differences prevalence, incidence and severity of osteoarthritis. Osteoarthritis Cartilage. 2005;13:769–81. doi: 10.1016/j.joca.2005.04.014. [DOI] [PubMed] [Google Scholar]
- 6.Lawrence RC, Helmick CG, Arnett FC, Deyo RA, Felson DT, Giannini EH, et al. Estimates of the prevalence of arthritis and selected musculoskeletal disorders in the United States. Arthritis Rheum. 1998;41:778–99. doi: 10.1002/1529-0131(199805)41:5<778::AID-ART4>3.0.CO;2-V. [DOI] [PubMed] [Google Scholar]
- 7.Gao W, Zeng C, Cai D, Liu B, Li Y, Wen X, et al. Serum concentrations of selected endogenous estrogen and estrogen metabolites in pre- and post-menopausal Chinese women with osteoarthritis. J Endocrinol Invest. 2010;33:644–9. doi: 10.1007/BF03346664. [DOI] [PubMed] [Google Scholar]
- 8.Sowers MR, McConnell D, Jannausch M, Buyuktur AG, Hochberg M, Jamadar DA. Estradiol and its metabolites and their association with knee osteoarthritis. Arthritis Rheum. 2006;54:2481–7. doi: 10.1002/art.22005. [DOI] [PubMed] [Google Scholar]
- 9.Samanta A, Jones A, Regan M, Wilson S, Doherty M. Is osteoarthritis in women affected by hormonal changes or smoking? Br J Rheumatol. 1993;32:366–70. doi: 10.1093/rheumatology/32.5.366. [DOI] [PubMed] [Google Scholar]
- 10.Cauley JA, Kwoh CK, Egeland G, Nevitt MC, Cooperstein L, Rohay J, et al. Serum sex hormones and severity of osteoarthritis of the hand. J Rheumatol. 1993;20:1170–5. [PubMed] [Google Scholar]
- 11.Spector TD, Perry LA, Jubb RW. Endogenous sex steroid levels in women with generalised osteoarthritis. Clin Rheumatol. 1991;10:316–9. doi: 10.1007/BF02208698. [DOI] [PubMed] [Google Scholar]
- 12.Lovejoy JC, Champagne CM, de Jonge L, Xie H, Smith SR. Increased visceral fat and decreased energy expenditure during the menopausal transition. Int J Obes (Lond) 2008;32:949–58. doi: 10.1038/ijo.2008.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shimokata H, Andres R, Coon PJ, Elahi D, Muller DC, Tobin JD. Studies in the distribution of body fat. II. Longitudinal effects of change in weight. Int J Obes. 1989;13:455–64. [PubMed] [Google Scholar]
- 14.Ley CJ, Lees B, Stevenson JC. Sex- and menopause associated changes in body-fat distribution. Am J Clin Nutr. 1992;55:950–4. doi: 10.1093/ajcn/55.5.950. [DOI] [PubMed] [Google Scholar]
- 15.Carr MC. The emergence of the metabolic syndrome with menopause. J Clin Endocrinol Metab. 2003;88:2404–11. doi: 10.1210/jc.2003-030242. [DOI] [PubMed] [Google Scholar]
- 16.Lewis-Faning E, Fletcher E. A statistical study of 1,000 cases of chronic rheumatism-Part III. Postgrad Med J. 1945;21:137–46. doi: 10.1136/pgmj.21.234.137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Anderson JJ, Felson DT. Factors associated with osteoarthritis of the knee in the first national Health and Nutrition Examination Survey (HANES I). Evidence for an association with overweight, race, and physical demands of work. Am J Epidemiol. 1988;128:179–89. doi: 10.1093/oxfordjournals.aje.a114939. [DOI] [PubMed] [Google Scholar]
- 18.Davis MA, Ettinger WH, Neuhaus JM. Obesity and osteoarthritis of the knee: evidence from the National Health and Nutrition Examination Survey (NHANES I) Semin Arthritis Rheum. 1990;20:34–41. doi: 10.1016/0049-0172(90)90045-h. [DOI] [PubMed] [Google Scholar]
- 19.Hochberg MC, Lethbridge-Cejku M, Scott WW, Jr, Reichle R, Plato CC, Tobin JD. The association of body weight, body fatness and body fat distribution with osteoarthritis of the knee: data from the Baltimore Longitudinal Study of Aging. J Rheumatol. 1995;22:488–93. [PubMed] [Google Scholar]
- 20.Manninen P, Hiihimaki H, Heliövaara M, Mäkelä P. Overweight, gender and knee osteoarthritis. Int J Obes Relat Metab Disord. 1996;20:595–7. [PubMed] [Google Scholar]
- 21.Coggon D, Reading I, Croft P, McLaren M, Barrett D, Cooper C. Knee osteoarthritis and obesity. Int J Obes Relat Metab Disord. 2001;25:622–7. doi: 10.1038/sj.ijo.0801585. [DOI] [PubMed] [Google Scholar]
- 22.Lachance L, Sowers M, Jamadar D, Jannausch M, Hochberg M, Crutchfield M. The experience of pain and emergent osteoarthritis of the knee. Osteoarthritis Cartilage. 2001;9:527–32. doi: 10.1053/joca.2000.0429. [DOI] [PubMed] [Google Scholar]
- 23.Hart DJ, Spector TD. The relationship of obesity, fat distribution and osteoarthritis in women in the general population: the Chingford Study. J Rheumatol. 1993;20:331–5. [PubMed] [Google Scholar]
- 24.Mundermann A, Dyrby CO, Andriacchi TP. Secondary gait changes in patients with medial compartment knee osteoarthritis: increased load at the ankle, knee, and hip during walking. Arthritis Rheum. 2005;52:2835–44. doi: 10.1002/art.21262. [DOI] [PubMed] [Google Scholar]
- 25.Maly MR, Costigan PA, Olney SJ. Contribution of psychosocial and mechanical variables to physical performance measures in knee osteoarthritis. Phy Ther. 2005;85:1318–28. [PubMed] [Google Scholar]
- 26.Rejeski WJ, Craven T, Ettinger WH, Jr, McFarlane M, Shumaker S. Self-efficacy and pain in disability with osteoarthritis of the knee. J Gerontol B Psychol Sci Soc Sci. 1996;51:P24–9. doi: 10.1093/geronb/51b.1.p24. [DOI] [PubMed] [Google Scholar]
- 27.Carman WJ, Sowers M, Hawthorne VM, Weissfeld LA. Obesity as a risk factor for osteoarthritis of the hand and wrist: a prospective study. Am J Epidemiol. 1994;139:119–29. doi: 10.1093/oxfordjournals.aje.a116974. [DOI] [PubMed] [Google Scholar]
- 28.Grotle M, Hagen KB, Natvig B, Dahl FA, Kvien TK. Obesity and osteoarthritis in knee, hip and/or hand: an epidemiological study in the general population with 10 years follow-up. BMC Musculoskelet Disord. 2008;9:132. doi: 10.1186/1471-2474-9-132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Oliveria SA, Felson DT, Cirillo PA, Reed JI, Walker AM. Body weight, body mass index, and symptomatic osteoarthritis of the hand, hip and knee. Epidemiology. 1999;10:161–6. [PubMed] [Google Scholar]
- 30.Katz JD, Agrawal S, Velasquez M. Getting to the heart of the matter: osteoarthritis takes its place as part of the metabolic syndrome. Curr Opin Rheumatol. 2010;22:512–9. doi: 10.1097/BOR.0b013e32833bfb4b. [DOI] [PubMed] [Google Scholar]
- 31.Kershaw EE, Flier JS. Adipose tissue as an endocrine organ. J Clin Endocrinol Metab. 2004;89:2548–56. doi: 10.1210/jc.2004-0395. [DOI] [PubMed] [Google Scholar]
- 32.Ku JH, Lee CK, Joo BS, An BM, Choi SH, Wang TH, Cho HL. Correlation of synovial fluid leptin concentrations with the severity of osteoarthritis. Clin Rheumatol. 2009;28:1431–5. doi: 10.1007/s10067-009-1242-8. [DOI] [PubMed] [Google Scholar]
- 33.Dumond H, Presle N, Terlain B, Mainard D, Loeuille D, Netter P, Pottie P. Evidence for a key role of leptin in osteoarthritis. Arthritis Rheum. 2003;48:3118–29. doi: 10.1002/art.11303. [DOI] [PubMed] [Google Scholar]
- 34.Gegout PP, Francin PJ, Mainard D, Presele N. Adipokines in osteoarthritis: friends or foes of cartilage homeostasis? Joint Bone Spine. 2008;75:669–71. doi: 10.1016/j.jbspin.2008.07.008. [DOI] [PubMed] [Google Scholar]
- 35.Presle N, Pottie P, Dumond H, Guillaume C, Lapicque F, Pallu S, et al. Differential distribution of adipokines between serum and synovial fluid in patients with osteoarthritis. Contribution of joint tissues to their articular production. Osteoarthritis Cartilage. 2006;14:690–5. doi: 10.1016/j.joca.2006.01.009. [DOI] [PubMed] [Google Scholar]
- 36.Rai MF, Sandell LJ. Inflammatory mediators: tracing links between obesity and osteoarthritis. Crit Rev Eukaryot Gene Expr. 2011;21:131–42. doi: 10.1615/critreveukargeneexpr.v21.i2.30. [DOI] [PubMed] [Google Scholar]
- 37.Gómez R, Conde J, Scotece M, Gómez-Reino JJ, Lago F, Gualillo O. What’s new in our understanding of the role of adipokines in rheumatic diseases? Nat Rev Rheumatol. 2011;7:528–36. doi: 10.1038/nrrheum.2011.107. [DOI] [PubMed] [Google Scholar]
- 38.Sowers MR, Karvonen-Gutierrez CA. The evolving role of obesity in knee osteoarthritis. Curr Opin Rheumatol. 2010;22:533–7. doi: 10.1097/BOR.0b013e32833b4682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lajeunesse D, Pelletier JP, Martel-Pelletier J. Osteoarthritis: a metabolic disease induced by local abnormal leptin activity? Curr Rheumatol Rep. 2005;7:79–81. doi: 10.1007/s11926-005-0057-0. [DOI] [PubMed] [Google Scholar]
- 40.Apold H, Meyeer HE, Espenhaug B, Nordsletten L, Havelin LI, Flugsrud GB. Weight gain and the risk of total hip replacement in a population-based prospective cohort study of 265,725 individuals. Osteoarthritis Cartilage. 2011;19:809–15. doi: 10.1016/j.joca.2011.03.013. [DOI] [PubMed] [Google Scholar]
- 41.Brennan SL, Cicuttini FM, Pasco JA, Henry MJ, Wang Y, Kotowicz MA, et al. Does an increase in body mass index over 10 years affect knee structure in a population-based cohort study of adult women? Arthritis Res Ther. 2010;12:R139. doi: 10.1186/ar3078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Buckland-Wright C. Protocols for precise radio-anatomical positioning of the tibiofemoral and patellofemoral compartments of the knee. Osteoarthritis Cartilage. 1995;3(Suppl A):71–80. [PubMed] [Google Scholar]
- 43.Kellgren JH, Lawrence JS. Atlas of standard radiographs of arthritis. II. Philadelphia: FA Davis; 1963. The epidemiology of chronic rheumatism. [Google Scholar]
- 44.Ruhl CE, Everhart JE. Leptin concentrations in the United States: relations with demographic and anthropometric measures. Am J Clin Nutr. 2001;74:295–301. doi: 10.1093/ajcn/74.3.295. [DOI] [PubMed] [Google Scholar]
- 45.Karvonen-Gutierrez CA, Sowers MR, Heeringa SG. Sex dimorphism in the association of cardiometabolic characteristics and osteophytes-defined radiographic knee osteoarthritis among obese and non-obese adults: NHANES III. Osteoarthritis Cartilage. 2012;20:614–21. doi: 10.1016/j.joca.2012.02.644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Rosenbaum M, Nicolson M, Hirsch J, Heymsfield SB, Gallagher D, Chu F, et al. Effects of gender, body composition, and menopause on plasma concentrations of leptin. J Clin Endocrinol Metab. 1996;81:3424–27. doi: 10.1210/jcem.81.9.8784109. [DOI] [PubMed] [Google Scholar]
- 47.Ostlund RE, Yang JW, Klein S, Gingerich R. Relation between plasma leptin concentration and body fat, gender, diet, age, and metabolic covariates. J Clin Endocrinol Metab. 1996;81:3909–13. doi: 10.1210/jcem.81.11.8923837. [DOI] [PubMed] [Google Scholar]
- 48.Kennedy A, Gettys TW, Watson P, Wallace P, Ganaway E, Pan Q, et al. The metabolic significance of leptin in humans: gender-based differences in relationship to adiposity, insulin sensitivity, and energy expenditure. J Clin Endocrinol Metab. 1997;82:1293–1300. doi: 10.1210/jcem.82.4.3859. [DOI] [PubMed] [Google Scholar]
- 49.Saad MF, Damani S, Gingerich RL, Riad-Gabriel MG, Khan A, Boyadiian R, et al. Sexual dimorphism in plasma leptin concentration. J Clin Endocrinol Metab. 1997;82:579–84. doi: 10.1210/jcem.82.2.3739. [DOI] [PubMed] [Google Scholar]
- 50.Garaulet M, Perex-Llamas F, Fuente T, Zamora S, Tebar FJ. Anthropometric, computed tomography and fat cell data in an obese population: Relationship with insulin, leptin, tumor necrosis factor-alpha, sex hormone binding globulin, and sex hormones. Eur J Endocrinol. 2000;143:657–66. doi: 10.1530/eje.0.1430657. [DOI] [PubMed] [Google Scholar]
- 51.Simopoulou T, Malizos KN, Iliopoulos D, Stefanou N, Papatheodorou L, Ioannou M, Tsezou A. Differential expression of leptin and leptin’s receptor isoform (Ob-Rb) mRNA between advanced and minimally affected osteoarthritic cartilage; effect on cartilage metabolism. Osteoarthritis Cartilage. 2007;15:872–83. doi: 10.1016/j.joca.2007.01.018. [DOI] [PubMed] [Google Scholar]
- 52.Vuolteenaho K, Koskinen A, Kukkonen M, Nieminen R, Pajvarinta U, Moilanen T, Moilanen E. Leptin enhances synthesis of proinflammatory mediators in human osteoarthritic cartilage--mediator role of NO in leptin-induced PGE2, IL-6 and IL-8 production. Mediators Inflamm. 2009:1–10. doi: 10.1155/2009/345838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Yusuf E. Metabolic factors in osteoarthritis: obese people do not walk on their hands. Arthritis Res Ther. 2012;14:123. doi: 10.1186/ar3894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Massengale M, Reichmann WM, Losina E, Solomon DH, Katz JN. The relationship between hand osteoarthritis and serum leptin concentration in participants of the Third National Health and Nutrition Examination Survey. Arthritis Res Ther. 2012;14:R132. doi: 10.1186/ar3864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Dieppe P, Cushnaghan J. The natural course and prognosis of osteoarthritis. In: Moskowitz R, Howell DJ, Goldberg VM, Mankin JH, editors. Osteoarthritis: Diagnosis and Medical Surgical Management. 2. London: Saunders; 1992. pp. 399–412. [Google Scholar]
- 56.Hart DJ, Spector TD, Egger P, Coggon D, Cooper C. Defining osteoarthritis of the hand for epidemiologic studies. The Chingford Study. Ann Rheum Dis. 1994;53:220–3. doi: 10.1136/ard.53.4.220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Valkenburg HA. Clinical versus radiological osteoarthritis in the general population. In: Peyron JG, editor. Epidemiology of Osteoarthritis. Paris: Geigy; 1991. pp. 53–8. [Google Scholar]
- 58.Yusuf E, Ioan-Facsinay A, Bijsterbosch J, Klein-Wieringa I, Kwekkeboom J, Slagboom PE, Huizinga TW, Kloppenburg M. Association between leptin, adiponectin and resistin and long-term progression of hand osteoarthritis. Ann Rheum Dis. 2011;70:1282–4. doi: 10.1136/ard.2010.146282. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


