Abstract
Background
Childhood trauma has been linked to a number of negative outcomes later in life, including alcohol dependence. Previous studies have suggested a mediating role for neuroticism in the relationship between childhood trauma and psychopathology. In this study we investigate the prevalence of multiple types of childhood trauma in treatment-seeking alcohol dependent patients, and the associations between childhood trauma and alcohol dependence severity using multiple mediation analysis.
Method
The prevalence of five types of childhood trauma – emotional abuse, sexual abuse, physical abuse, emotional neglect, and physical neglect – was assessed in treatment seeking alcohol dependent patients (n = 280) and healthy controls (n = 137) using the Childhood Trauma Questionnaire. Multiple mediation analyses were used to model associations between childhood trauma measures and alcohol-related outcomes, primarily the severity of alcohol dependence in the alcohol dependent sample.
Results
Childhood trauma was significantly more prevalent and more severe in the alcohol dependent subjects. In addition, childhood trauma was found to influence alcohol dependence severity, an effect that was mediated by neuroticism. When individual trauma types were examined, emotional abuse was found to be the primary predictor of alcohol dependence severity, both directly and through the mediating effects of the impulsivity subfacet of neuroticism. Physical abuse also had a moderate direct effect on alcohol dependence severity. Mediation analysis did not reveal any association between childhood trauma and AUDIT score in the non-dependent control sample.
Conclusions
Childhood trauma is highly prevalent in treatment-seeking alcoholics and may play a significant role in the development and severity of alcohol dependence through an internalizing pathway involving negative affect. Our findings suggest that alcoholics with a history of childhood emotional abuse may be particularly vulnerable to severe dependence.
Introduction
Alcohol dependence is a common and debilitating disorder that is subject to both genetic and environmental influences. The heritability of alcohol dependence has been estimated at 50% (Goldman et al., 2005), implying that shared and non-shared environmental factors also contribute to individual differences in risk. Childhood trauma exposure has been linked to alcohol dependence (Copeland et al., 2011; Enoch, 2011; Magnusson et al., 2011; Widom et al., 2007; Young-Wolff et al., 2011), suggesting that adverse childhood experiences contribute to this environmental risk.
Childhood trauma has been linked to a multitude of negative consequences in both early life and adulthood, including alterations in brain structure and function (Bremner, 2003), variation in personality traits (McFarlane et al., 2005), increased risk for depression and anxiety (Heim and Nemeroff, 2001), and an earlier age of onset of alcohol use and abuse (Rothman et al., 2008). Many if not all of these outcomes are potentially interrelated, either through direct pathways or through common underlying mechanisms. For example, alcohol problems and dependence have been linked to higher levels of neuroticism (Ruiz et al., 2003), as have depression and anxiety disorders (Weinstock and Whisman, 2006), both of which are often comorbid with alcohol dependence. The common underlying mechanism for these outcomes is thought to be neurodevelopmental alterations that occur in response to the stress of traumatic experiences during childhood (Anda et al., 2006). Taken together, these findings suggest that childhood trauma and alcohol dependence may be linked via a negative affect pathway.
The severity of childhood trauma, e.g. assessed using a continuous severity score, may be a better predictor of negative outcomes than dichotomous measures that simply report presence or absence. Severity of emotional abuse has been associated with greater risk for relapse in cocaine dependent adults (Hyman et al., 2008), while severity of sexual abuse has been associated with a number of outcomes, including increased severity of symptoms in depression and posttraumatic stress disorder (PTSD) (Gamble et al., 2006; Glover et al., 2010). In some cases, relationships between childhood abuse severity and the outcomes of interest are “mediated” by a third factor, i.e., the relationship between predictor and outcome is partially accounted for by the relationships between the mediator and both predictor and outcome (Preacher and Hayes, 2008). For example, neuroticism has been found to mediate the relationship between sexual abuse severity and depression (Gamble et al., 2006). Given the reported association between alcohol-related problems and neuroticism, we hypothesize that neuroticism may play a similar mediating role between childhood trauma exposure and alcohol dependence severity.
In a recent publication, we reported that childhood trauma exposure was associated with increased risk for co-morbid psychiatric disorders and suicide attempts in treatment-seeking alcoholic inpatients (Huang et al., 2012). The current study expands on this and other research by investigating the associations between childhood trauma exposure and quantifiable outcomes specifically related to alcohol dependence. These include potential risk factors for alcohol dependence, such as an early onset of alcohol use and personality traits, concomitant features of alcohol dependence such as high levels of withdrawal anxiety, and finally, the severity of alcohol dependence. We first compare the prevalence and severity of childhood trauma exposure between alcohol dependent and non-acohol-dependent individuals. We then investigate potential mediating pathways between childhood trauma exposure and alcohol-related outcomes in both dependent and non-dependent individuals using mediation analysis.
Materials and Methods
Subjects
The primary sample for this study included 280 treatment-seeking individuals (90 females, 190 males) who met the Diagnostic and Statistical Manual for Mental Disorders, 4th Edition, Text-revised (DSM-IV-TR) criteria for alcohol dependence (hereafter referred to as AD subjects). A comparison sample of 137 subjects without any past or current alcohol dependence (52 females, 85 males; hereafter referred to as CON subjects) was also investigated. Diagnoses of alcohol dependence were determined using the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID). Treatment-seeking AD subjects were admitted to a 28-day inpatient treatment program run by the National Institute of Alcohol Abuse and Alcoholism (NIAAA) at the NIH Clinical Center in Bethesda, MD. A subset of the AD subjects (n = 196) were included in a previous investigation of childhood trauma exposure and risk for co-morbid psychiatric disorders (Huang et al., 2012). CON subjects were voluntarily enrolled in non-treatment NIAAA research protocols during the same period of time that the AD subjects were admitted as inpatients. While the CON subjects had no current or past alcohol dependence diagnoses, the sample did include some heavy drinkers (5 or more drinks in a day for males, and 4 or more drinks in a day for females) and several individuals (n = 10) who met criteria for current alcohol abuse. Table 1 provides subject sample characteristics for both AD and CON subjects.
Table 1.
Subject Sample Characteristics
| Alcohol Dependent (AD) Subjects | Control (CON) Subjects | |||||
|---|---|---|---|---|---|---|
| Measure | Total Sample | Males | Females | Total Sample | Males | Females |
| Number of subjects | 280 | 190 | 90 | 137 | 85 | 52 |
| Age (years)† | 41.4 (±10.0) | 41.9 (±9.7) | 40.5 (±10.7) | 28.7 (±8.4) | 29.9 (±9.7) | 26.6 (±5.1) |
| Race | ||||||
| White | 158 (56.4%) | 101 (53.2%) | 57 (63.3%) | 88 (64.3%) | 53 (62.4%) | 35 (67.3%) |
| Black/African-American | 98 (35.0%) | 71 (37.4%) | 27 (30.0%) | 30 (21.9%) | 21 (24.7%) | 9 (17.3%) |
| Asian | 4 (1.4%) | 4 (2.1%) | 0 (0%) | 11 (8.0%) | 5 (5.9%) | 6 (11.5%) |
| American Indian/Alaskan | 2 (0.7%) | 0 (0%) | 2 (2.2%) | 0 (0%) | 0 (0%) | 0 (0%) |
| More than One Race | 5 (1.8%) | 2 (1.1%) | 3 (3.3%) | 6 (4.4%) | 4 (4.7%) | 2 (3.9%) |
| Unknown | 13 (4.6%) | 12 (6.3%) | 1 (1.1%) | 2 (1.5%) | 2 (2.4%) | 0 (0%) |
| Ethnicity | ||||||
| Hispanic | 16 (5.7%) | 14 (7.4%) | 2 (2.2%) | 8 (5.8%) | 3 (3.5%) | 5 (9.6%) |
| Non-Hispanic | 260 (92.9%) | 174 (91.6%) | 86 (95.6%) | 129 (94.2%) | 82 (96.5%) | 47 (90.4%) |
| Unknown | 4 (1.4%) | 2 (1.1%) | 2 (2.2%) | 0 (0%) | 0 (0%) | 0 (0% ) |
| Education (years)† | 13.7 (±2.7) | 13.5 (±2.8) | 14.3 (±2.5) | 15.8 (±2.8) | 15.3 (±3.1) | 16.6 (±2.2) |
| Alcohol Dependence Severity1 | 21.0 (±7.9) | 20.5 (±8.3) | 22.1 (±6.9) | N/A | N/A | N/A |
| AUDIT Score | N/A | N/A | N/A | 7.1 (±4.0) | 8.0 (±4.0) | 5.6 (±3.6) |
| Family History Density † | 0.17 (±0.17) | 0.15 (±0.16) | 0.21 (±0.19) | 0.03 (±0.07) | 0.03 (±0.07) | 0.03 (±0.09) |
| Personality Factors | ||||||
| Neuroticism † | 57.5 (±11.0 ) | 56.7 (±10.9 ) | 58.6 (±11.2 ) | 45.1 (±9.1) | 45.1 (±8.8) | 45.0 (±9.8) |
| Extraversion | 52.9 (±10.7) | 53.3 (±10.0) | 52.0 (±11.2) | 54.3 (±10.2) | 54.7 (±10.0) | 53.3 (±10.8) |
| Openness† | 50.6 (±10.4) | 49.5 (±10.1) | 53.9 (±10.4) | 55.3 (±10.6) | 54.1 (±10.2) | 58.2 (±11.2) |
| Agreeableness† | 46.3 (±12.1) | 46.9 (±12.4) | 46.4 (±13.1) | 49.0 (±11.7) | 48.4 (±11.5) | 50.0 (±12.3) |
| Conscientiousness† | 43.4 (±12.8) | 44.0 (±12.6) | 42.1 (±13.5) | 49.8 (±11.7) | 49.0 (±10.6) | 51.7 (±14.0) |
| Recent Drinking History (last 90 Days) | ||||||
| Total Drinks† | 1106.8 (±7210.3) | 1195.7 (±759.3) | 894.6 (±615.5) | 205.6 (±222.0) | 235.7 (±232.6) | 137.6 (±180.7) |
| # Drinking Days† | 71.5 (±22.0) | 72.4 (±22.2) | 69.9 (±21.6) | 42.3 (±26.1) | 45.7 (±26.4) | 34.6 (±24.0) |
| # Heavy Drinking Days† | 66.7 (±25.4) | 67.7 (±25.3) | 64.7 (±25.7) | 18.7 (±23.1) | 20.8 (±24.2) | 13.9 (±20.0) |
| Average # Drinks/Drinking Day† | 14.7 (±7.9) | 16.0 (±8.2) | 12.2 (±6.6) | 4.3 (±2.8) | 4.7 (±2.9) | 3.4 (±2.6) |
| Lifetime Alcohol Use | ||||||
| Age at first alcohol use† | 19.9 (±7.0) | 19.5 (±6.8) | 20.7 (±7.4) | 16.7 (±2.8) | 16.5 (±3.0) | 17.2 (±2.4) |
| # Y ears of heavy alcohol use† | 14.0 (±9.5) | 15.2 (±9.6) | 11.7 (±9.0) | 3.2 (±7.0) | 3.8 (±7.4) | 2.0 (±5.8) |
| Depression/Anxiety Ratings During Withdrawal1 | ||||||
| Anxiety(BSA subscale) | 12.1 (±7.0) | 10.8 (±6.9) | 14.7 (±6.4) | N/A | N/A | N/A |
| Depression (MADRS subscale) | 15.8 (±9.1) | 14.4 (±9.0) | 18.5 (±8.8) | N/A | N/A | N/A |
| Lifetime Psychiatric Comorbidy | ||||||
| Mood Disorder | 71 (25.4%) | 36 (19.0%) | 35 (38.9%) | 4 (2.9%) | 2 (2.4%) | 2 (3.9%) |
| Anxiety Disorder | 130 (46.4%) | 68 (35.8%) | 62 (68.9%) | 1 (0.8%) | 0 (0%) | 1 (1.9%) |
| Substance Use Disorder2 | 201 (71.8%) | 139 (73.1%) | 62 (68.9%) | 5 (3.7%) | 4 (4.7%) | 1 (1.9%) |
Notes: unless noted otherwise, numbers in parentheses are standard deviation. Alcohol dependence severity is measured by the Alcohol Dependence Severity Scale; family history density is measured using the Family Tree Questionnaire and represents the proportion of first and second degree relatives identified as having a definite alcohol problem; personality factors are measured by the Revised NEO Personality Inventory; recent drinking history is assessed by the Timeline Follow Back; lifetime alcohol use is assessed by the Addiction Severity Index for AD subjects and by the Lifetime Drinking History Assessment for CON subjects; depression and anixety ratings are measured by the Comprehensive Psychopathology Rating Scale, which produces two subscales, the Montgomery-Asberg Depression Scale (MADRS) and the Brief Scale for Anxiety (BSA).
Only collected for AD subjects
Other than alcohol abuse or dependence
Significant difference between AD and CON subjects (One-way ANOVA, p < 0.05)
Assessments
Childhood trauma was assessed in both groups using the Childhood Trauma Questionnaire (CTQ) (Bernstein and Fink, 1998; Bernstein et al., 2003). The CTQ is a 28-item self-report questionnaire that yields numerical scores for five categories of childhood trauma exposure: emotional abuse, physical abuse, sexual abuse, emotional neglect, and physical neglect. These quantitative scores are based on multiple Likert scale ratings for each type of trauma and range from 5 to 25. In addition, cut-off scores are indicated for none, low, moderate, and severe levels of trauma (Bernstein and Fink, 1998). Thus the CTQ provides both a measure of presence or absence of trauma and a measure of severity of exposure.
In addition to the CTQ, we assessed both groups of subjects for personality traits using the revised NEO personality inventory (NEO-PIR) (Costa and McCrae, 2002), family history of alcoholism using the Family Tree Questionnaire (FTQ) (Mann et al., 1985), and recent drinking patterns over the last 90 days using the Timeline Followback (TLFB) (Sobell and Sobell, 1992). Alcohol dependent subjects were further assessed using the Addiction Severity Index (ASI) (Developed by Thomas McLellan and collaborators from the University of Pennsylvania’s Center for the Studies of Addiction, distributed by the Treatment Research Institute, Philadelphis, PA, http://www.tresearch.org) for lifetime alcohol use, the Alcohol Dependence Scale (ADS) (Skinner and Allen, 1982) for alcohol dependence severity, and the Comprehensive Psychopathological Rating Scale (CPRS) (Asberg and Schalling, 1979) for depression and anxiety symptom ratings. With the exception of the CPRS, which was administered on Day 2 to assess depression and anxiety symptoms during acute withdrawal, all other assessments, including the SCID, were administered at least one week after admission in order to minimize any potential effects of withdrawal symptoms on responses to the questionnaires. The Lifetime Drinking History (Skinner and Sheu, 1982) assessment and the Alcohol Use Disorders Identification Test (AUDIT) (Babor, 1989) were used to assess alcohol use and misuse in the CON subjects.
Statistical Analysis
The statistical analyses addressed two goals: 1) to assess the prevalence and severity of the different types of childhood trauma exposure in AD subjects compared to the non-alcohol-dependent CON subjects, and 2) to evaluate associations between childhood trauma exposure types and alcohol-related outcomes in both the AD and CON subjects. To assess prevalence, a dichotomous variable representing presence or absence of each trauma type was established for both AD and CON subjects using a cut-off score indicating at least a low level of severity. The cut-offs for each trauma type were as follows: emotional abuse ≥ 9, physical abuse ≥ 8, sexual abuse ≥ 6, emotional neglect ≥10, physical neglect ≥ 8 (Bernstein and Fink, 1998). Severity was assessed using the total scores obtained for each trauma type from the CTQ. Comparisons between AD and CON subjects were performed using chi-square analyses and one way analyses of variance (ANOVA).
For the second goal, we analyzed the data in two steps. First, we examined simple bivariate correlations between the trauma measures from the CTQ (total score as well as individual subtype scores), potential mediator variables, and the alcohol-related outcomes of alcohol dependence severity (ADS) score (for the AD subjects) and AUDIT score (for the CON subjects). Variables that exhibited significant bivariate associations with the ADS score or the AUDIT score were then carried forward into a multiple mediation analysis to more fully examine relationships between predictors and outcomes. Based on previous theoretical and empirical research, we used the following variables as potential mediators between childhood trauma exposure and alcohol-related outcomes: lifetime drinking history variables such as age of first alcohol use and history of heavy alcohol use, anxiety and depression symptoms during withdrawal (AD subjects only), and personality factors.
Multiple mediation analyses were conducted first using the total score from the CTQ, and then the scores for each trauma type individually as independent variables. Following methods recommended by Preacher and Hayes, we conducted separate analyses with each abuse/neglect type (e.g., emotional abuse) as the independent variable, and the other four types included as covariates in the model. This method allowed us to estimate the effects of each trauma type independently, in effect controlling for any correlation between scores for each trauma type (Preacher and Hayes, 2008). For the analyses, we used the INDIRECT macro developed for SAS (available at http://www.afhayes.com). This macro uses bootstrapping to estimate indirect or mediated effects, a method that is highly recommended when sample size is not large (e.g., < 400) in order to maintain statistical power without the assumption of multivariate normality (Preacher and Hayes, 2008). In addition, the macro allows for the inclusion of covariates as well as potential mediators in the analysis model. We included the demographic variables of age, gender (0 = male, 1 = female), and race (0 = white/caucasian, 1 = black or other) in all models tested, as well as a measure of family history of alcoholism (family history density from the FTQ). The latter is both a strong predictor of alcohol dependence and a risk factor for childhood maltreatment, as children of alcohol dependent parents are more likely to experience parent-child conflict (Hill et al., 1994). Psychiatric comorbidity (i.e., lifetime diagnosis of a mood, anxiety, or other substance use disorder, 0 = no, 1 = yes) was also included in the covariates for AD subjects (there was little to no psychiatric comorbidity in the CON subjects). Indirect effects were estimated via bootstrap analysis using 5000 randomly generated samples. Mediation is established if the 95% bias-corrected confidence interval for the indirect parameter estimate does not contain zero. All statistical analyses were conducted using SAS version 9.2 (SAS Institute, Cary, NC). The level of statistical significance was set at p < 0.05 for all tests.
Results
Prevalence and Severity of Childhood Trauma Exposure
The prevalence (presence/absence) and severity scores for childhood trauma in both AD and CON subjects are presented in Table 2. Childhood trauma exposure was significantly more prevalent in the AD subjects, with odds ratios ranging from 3.5 (95% CI 2.1–5.9) for physical abuse to 11.5 (95% CI 5.8–22.8) for emotional abuse. Severity scores were also significantly higher in the AD subjects, with effect sizes ranging from medium to large (Cohen’s d of 0.6 to 1.0). Of the five individual types of trauma, emotional abuse and neglect were the most frequent among the AD subjects. In addition, a much higher number of AD subjects experienced more than one type of childhood trauma, compared to CON subjects.
Table 2.
Comparison of childhood trauma exposure in AD and CON subjects
| AD Subjects |
CON Subjects |
Comparison of prevalence |
Comparison of severity |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Variable | Yes (%) |
No (%) |
Severity Score (SD) |
Yes (%) |
No (%) |
Severity Score (SD) |
χ2 | Odds Ratio1 (95% CI) |
F | Cohen’s d2 |
| Emotional Abuse | 133 (47.5%) |
147 (52.5%) |
9.8 (5.1) |
10 (7.3%) |
127 (92.3%) |
6.0 (1.7) |
67.0*** | 11.5 (5.8–22.8) |
73.6*** | 1.0 |
| Sexual Abuse | 79 (21.1%) |
221 (78.9%) |
7.6 (5.6) |
8 (5.8%) |
129 (94.2%) |
5.2 (1.0) |
15.8*** | 4.3 (2.0–9.3) |
26.2*** | 0.6 |
| Physical Abuse | 109 (38.9%) |
171 (61.1%) |
8.8 (4.3) |
21 (15.3%) |
116 (84.7%) |
5.9 (1.5) |
23.9*** | 3.5 (2.1–5.9) |
56.7*** | 0.9 |
| Emotional Neglect | 160 (57.1%) |
120 (42.9%) |
10.4 (5.0) |
29 (21.2%) |
108 (78.8%) |
7.5 (3.1) |
48.0*** | 5.0 (3.1–7.8) |
40.8*** | 0.7 |
| Physical Neglect | 77 (27.5%) |
203 (72.5%) |
7.4 (3.6) |
13 (9.5%) |
124 (90.5%) |
5.7 (2.1) |
17.6*** | 3.6 (1.9–6.8) |
25.5*** | 0.6 |
| Total Childhood Trauma Score |
44.1 (17.1) |
30.3 (6.7) |
82.6*** | 1.0 | ||||||
| Total Number of Trauma Types |
N (%) |
N (%) |
||||||||
| 0 | 73 (26.1%) | 81 (59.1%) | ||||||||
| 1 | 57 (20.4%) | 41 (29.9%) | ||||||||
| 2 | 44 (15.7%) | 8 (5.8%) | ||||||||
| 3 | 48 (17.1%) | 5 (3.7%) | ||||||||
| 4 | 41 (14.6%) | 1 (0.8%) | ||||||||
| 5 | 17 (6.1%) | 1 (0.8%) | ||||||||
Notes: SD = standard deviation, CI = confidence interval
Based on the comparison of frequency in AD subjects vs. CON subjects
Effect size for comparison of severity scores: Cohen’s d of 0.2 to 0.4 is a small effect size, 0.5 to 0.7 is a medium effect size, and greater than 0.8 is a large effect size
p < 0.001
Relationship between Childhood Trauma Exposure and Alcohol Dependence Severity in Treatment-Seeking Alcoholics
Supplemental Table 1 presents simple bivariate associations between the study variables for the AD subjects. CTQ total score, as well as all individual trauma types except for physical neglect, showed positive correlations with alcohol dependence severity, as did withdrawal anxiety and depression symptoms, and the personality domain of neuroticism. Negative correlations with alcohol dependence severity were found for age at first intoxication, and for the personality domains of agreeableness and conscientiousness. Based on these preliminary results, we included age at first intoxication, anxiety and depression symptoms, and neuroticism, agreeableness, and conscientiousness as potential mediators in the multiple mediation analyses.
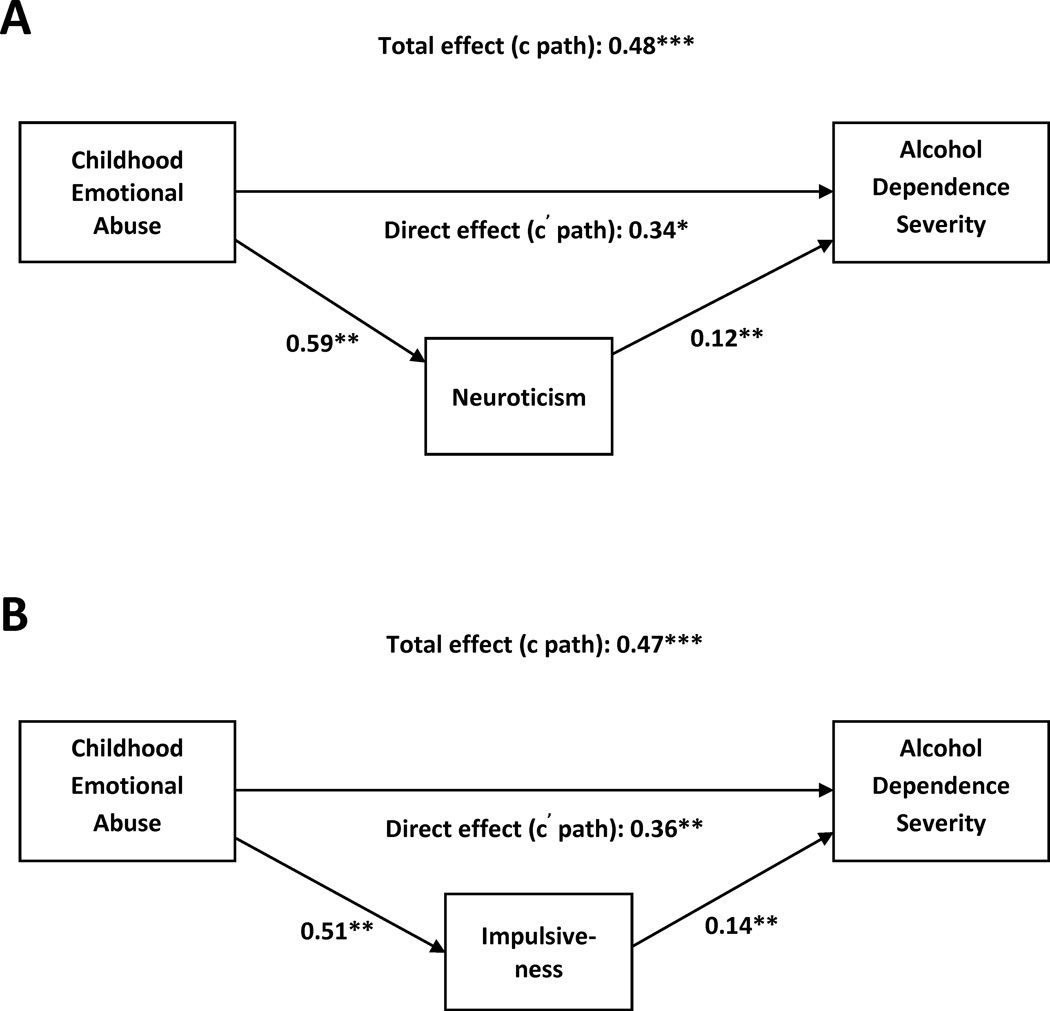
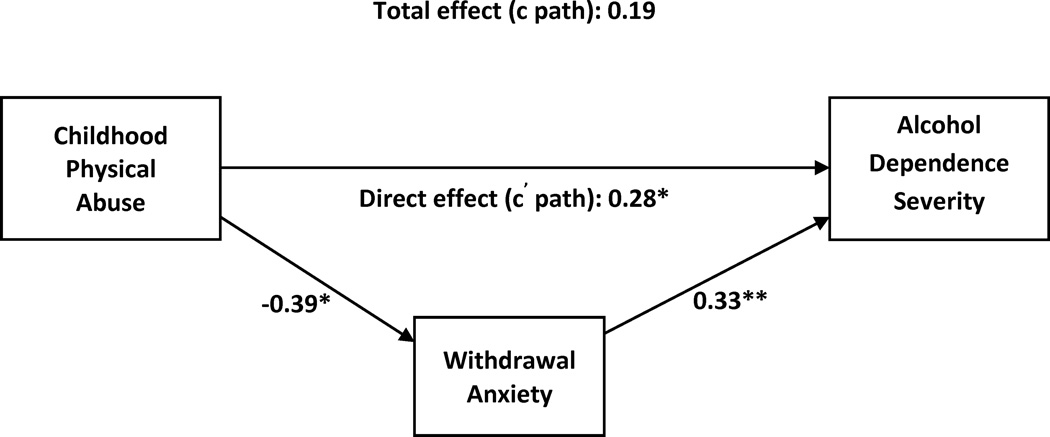
Table 3 presents the results of the multiple mediation analyses for CTQ total score and for each trauma type. All effect estimates are unstandardized regression coefficients, as recommended by Preacher and Hayes (Preacher and Hayes, 2008), and as such represent the average change in ADS score as a result of a one unit change in the independent variable. Since all trauma types are measured on the exact same scale (ranging from 5 to 25), comparison of the magnitude of the effect estimates is straightforward. The model using CTQ total score as the independent variable (R2 = 0.31, p < 0.0001) showed a significant total effect on ADS score (b = 0.09, p = 0.005) as well as an indirect effect mediated through neuroticism (bootstrapped estimate = 0.03, 95% CI = 0.01, 0.06). When the individual trauma types were evaluated, emotional abuse was found to exhibit significant total (b = 0.48, p < 0.0001) and direct effects (b = 0.34, p = 0.01) on ADS score, as well as an indirect effect through neuroticism (bootstrapped estimate = 0.08, 95% CI = 0.02, 0.16) (Figure 1a). Physical abuse was found to have a significant direct effect (b = 0.28, p = 0.04) on ADS score, as well as an indirect effect through withdrawal anxiety (bootstrapped estimate = −0.10, 95% CI = −0.25, −0.01). Because these effects occur in opposite directions, i.e., physical abuse showing a direct positive association with ADS score but an indirect negative association through withdrawal anxiety symptoms, the total effect estimate ended up being less than the direct effect estimate. Physical neglect was also found to have a significant direct effect on ADS score (b = −0.36, p = 0.03); curiously this effect (negative association) was in the opposite direction as that seen for physical abuse. Neither sexual abuse nor emotional neglect were found to have significant effects on ADS score using mediation analysis. The proportion of variance explained was the same for all models testing the individual trauma types (R2 = 0.35, p < 0.0001) due to the use of the same set of variables for each model, the only difference being which trauma type was used as the independent variable, and which trauma types as the covariates.
Table 3.
Results of multiple mediation analyses for total CTQ score and for each trauma type for the AD subjects1
| Independent Variable (IV) |
Mediator | Effect of IV on Mediator |
Effect of Mediator on AD Severity2 |
Indirect Effect Estimate3 |
95% Bias-Corrected Confidence Interval |
Total Effect of IV |
Direct Effect of IV |
|---|---|---|---|---|---|---|---|
| CTQ Total Score | Age of First Intoxication | −0.001 | −0.10 | 0.0001 | −0.01, 0.01 | 0.09** | 0.05 |
| Withdrawal Depression | 0.03 | −0.09 | −0.003 | −0.02, 0.002 | |||
| Withdrawal Anxiety | 0.02 | 0.33** | 0.007 | 0.01, 0.03 | |||
| Nuroticism | 0.23*** | 0.13** | 0.03 | 0.01, 0.06† | |||
| Conscientiousness | −0.01 | −0.05 | 0.0008 | −0.003, 0.01 | |||
| Emotional Abuse | Age of First Intoxication | −0.03 | −0.08 | 0.003 | −0.02, 0.04 | 0.48*** | 0.34* |
| Withdrawal Depression | 0.14 | −0.07 | −0.01 | −0.09, 0.02 | |||
| Withdrawal Anxiety | 0.21 | 0.33** | 0.07 | −0.02, 0.21 | |||
| Neuroticism | 0.59** | 0.12** | 0.08 | 0.02, 0.16† | |||
| Conscientiousness | −0.06 | −0.07 | 0.004 | −0.02, 0.05 | |||
| Physical Abuse | Age of First Intoxication | −0.16 | 0.01 | −0.01, 0.06 | 0.19 | 0.28* | |
| Withdrawal Depression | −0.39* | 0.03 | −0.02, 0.14 | ||||
| Withdrawal Anxiety | −0.30* | −0.10 | −0.25, −0.01† | ||||
| Neuroticism | −0.04 | −0.01 | −0.07, 0.05 | ||||
| Conscientiousness | 0.47 | −0.03 | −0.09, 0.0004 | ||||
| Sexual Abuse | Age of First Intoxication | −0.02 | 0.001 | −0.01, 0.03 | −0.05 | −0.05 | |
| Withdrawal Depression | −0.09 | 0.01 | −0.01, 0.05 | ||||
| Withdrawal Anxiety | −0.01 | −0.002 | −0.07, 0.06 | ||||
| Neuroticism | 0.08 | 0.01 | −0.02, 0.05 | ||||
| Conscientiousness | 0.13 | −0.01 | −0.04, 0.01 | ||||
| Emotional Neglect | Age of First Intoxication | −0.23 | 0.02 | −0.003, 0.07 | −0.08 | −0.10 | |
| Withdrawal Depression | 0.24 | −0.02 | −0.10, 0.01 | ||||
| Withdrawal Anxiety | −0.02 | −0.002 | −0.11, 0.08 | ||||
| Neuroticism | 0.12 | 0.02 | −0.02, 0.08 | ||||
| Conscientiousness | −0.31 | 0.02 | 0.004, 0.08 | ||||
| Physical Neglect | Age of First Intoxication | 0.60* | −0.05 | −0.12, 0.01 | −0.30 | −0.34* | |
| Withdrawal Depression | 0.10 | −0.01 | −0.11, 0.02 | ||||
| Withdrawal Anxiety | 0.16 | 0.05 | −0.03, 0.19 | ||||
| Neuroticism | 0.23 | 0.03 | −0.02, 0.11 | ||||
| Conscientiousness | −0.10 | 0.006 | −0.02, 0.06 |
Effect estimates are unstandardized regression coefficients
For the analyses of each trauma type, coefficients for the effects of mediators on alcohol dependence severity are the same for each model, so are only presented in the table once
Based on 5000 bootstrapped samples
p < 0.05
p < 0.01
p < 0.001
Significant
Fig. 1.
Multiple mediation models of the relationship between emotional abuse and alcohol dependence severity. (A) Model including the personality domain neuroticism. Covariates and their effect estimates (in parentheses) are as follows: age (−0.01), race (−2.53**), gender (−0.54), family history density (11.09***), physical abuse (0.28*), sexual abuse (−0.05), emotional neglect (−0.11), physical neglect (−0.34*), lifetime history of a mood disorder (−2.10), lifetime history of an anxiety disorder (0.45), lifetime history of other substance use disorder (0.63) (B) Model including the subfacets of neuroticism. Covariates and their effect estimates (in parentheses) are as follows: age (−0.07), race (−1.78**), gender (−0.03), family history density (10.68***), physical abuse (0.25), sexual abuse (−0.08), emotional neglect (−0.08), physical neglect (−0.36*), lifetime history of a mood disorder (−1.67), lifetime history of an anxiety disorder (0.76), lifetime history of other substance use disorder (0.99) All path estimates and covariate coefficients are unstandardized regression coefficients. * p<0.05, ** p<0.01, *** p<0.001.
We conducted follow-up mediation analyses for CTQ total score (R2 = 0.30, p < 0.0001) and emotional abuse (R2 = 0.34, p < 0.0001) using the six subfacets of neuroticism as defined by the NEO-PIR (Supplemental Table 2) and found that, in the case of emotional abuse, the mediating effects of neuroticism are driven primarily by the subfacet labeled as impulsiveness (bootstrapped estimate = 0.07, 95% CI = 0.01, 0.17) (Figure 1b).
Figure 1 presents visual representations of the association between emotional abuse and alcohol dependence severity. Path estimates indicate that greater severity of childhood emotional abuse is associated with increased levels of neuroticism, primarily impulsiveness, which in turn is associated with increased alcohol dependence severity. The model for physical abuse (Figure 2) indicates that severity of physical abuse is negatively correlated with withdrawal anxiety symptoms, while directly positively correlated with ADS score. The contributions of the covariates, the effects of which were reasonably consistent across models, are also depicted. In terms of significant effects on ADS score, race (0 = white/caucasian, 1 = black/other) was negatively associated with ADS score, indicating that ADS score was higher among caucasian subjects. Family history of alcoholism, as measured by family history density, was highly positively correlated with ADS score. Gender and age, however, did not contribute significantly to ADS score.
Fig. 2.
Multiple mediation model of the relationship between physical abuse and alcohol dependence severity. Covariates and their effect estimates (in parentheses) are as follows: age (−0.01), race (−2.53**), gender (−0.54), family history density (11.09***), physical abuse (0.28*), sexual abuse (−0.05), emotional neglect (−0.11), physical neglect (−0.34*), lifetime history of a mood disorder (−2.10), lifetime history of an anxiety disorder (0.45), lifetime history of other substance use disorder (0.63) All path estimates and covariate coefficients are unstandardized regression coefficients. * p<0.05, ** p<0.01, *** p<0.001.
Relationship between Childhood Trauma Exposure and AUDIT Score in Control Subjects
Simple bivariate associations between the study variables for the CON subjects are presented in Supplemental Table 3. Physical abuse, physical neglect, CTQ total score, and heavy drinking years were positively correlated with AUDIT score, while age at first drink and the personality factors of openness and agreeableness were negatively correlated with AUDIT score. Based on these findings, we included age at first drink, heavy drinking years, openness, and agreeableness as potential mediators in the next step.
Due to such low prevalence and severity of several trauma types, particularly sexual abuse and physical abuse, in CON subjects, models using the individual trauma types as predictors/covariates were unreliable, producing unusually large effect estimates and confidence intervals. Consequently, only results for CTQ total score are presented (Supplemental Table 4). CTQ total score did not have any significant direct or indirect effects on AUDIT score.
Discussion
We investigated the frequency and severity of childhood trauma exposure in alcohol dependents individuals compared to a non-dependent sample, and the potential associations between severity of childhood trauma exposure and alcohol-related outcomes. Consistent with previous research, we found that all types of childhood trauma were highly prevalent in treatment seeking alcoholics. Especially noteworthy was the high prevalence of emotional abuse: alcohol dependent subjects were more than 10 times as likely to have experienced emotional abuse than non-dependent subjects (note however that the confidence interval for this estimate was rather large). The observed differences in prevalence are probably more extreme than what would be observed if the comparison sample were non-treatment seeking heavy drinkers rather than a community sample. However, the mean severity scores for our CON subjects were very consistent with those found for other community samples (Scher et al., 2001). When we examined each trauma type for associations with alcohol dependence severity, emotional abuse emerged as the key predictor, even when controlling for other forms of abuse and neglect. Furthermore. the effect of emotional abuse on alcohol dependence severity was mediated by the impulsiveness subfacet of neuroticism. Childhood trauma was not associated with harmful alcohol use, as measured by the AUDIT score, in non-dependent individuals.
Studies of childhood trauma exposure have focused primarily on physical or sexual abuse, presumably because these types of maltreatment are thought to be more prevalent, more dangerous to the health of a child, and more salient to the victim. The effects of emotional maltreatment, either in the form of emotional abuse or emotional neglect, have been less well studied. One reason for this may be that the definition of emotional abuse is not as clear-cut as that for physical or sexual abuse (Rees, 2010). Despite the lack of consensus on the definition of emotional abuse, most agree that it involves persistent, repeated experience of non-physical harmful interactions with a parent or caregiver (Glaser, 2011; Thompson and Kaplan, 1996). Like physical and sexual abuse, emotional abuse has negative effects on a child’s psychological and physical development. Unlike physical and sexual abuse, however, emotional abuse is not considered a crime (Thompson and Kaplan, 1996), and this may be another reason why the consequences of emotional abuse are not given as much attention. The consequences of childhood emotional abuse persist into adulthood and have been linked specifically to mood disorders, in particular major depressive disorder and bipolar disorder (Etain et al., 2010; Huang et al., 2012). That the consequences of emotional abuse persist into adulthood is not surprising, given the long postulated relationship between emotional maltreatment by a caregiver and the development of insecure attachment styles (Bowlby, 1969). Insecure attachment in infancy has been linked to poor emotional regulation and social functioning in humans as well as in animal models (Bowlby, 1969; Riggs, 2010; Suomi, 1991), effects that carry forward into adulthood and increase risk for psychopathology throughout the life cycle.
Our findings suggest that emotional abuse may play a prominent role in the development of alcohol dependence, independent from the effects of other types of abuse. Previous studies of childhood trauma exposure and alcohol dependence have mostly focused on sexual and physical abuse and, for the most part, significant associations with alcohol dependence have been observed primarily in women (Copeland et al., 2011; Widom et al., 2007). Epidemiologically, treatment-seeking alcoholics are more likely to be male (LoCastro et al., 2008), a finding that is reflected in our study sample. This is one possible explanation for why we did not find the previously established associations between sexual abuse and alcohol dependence severity. It is also possible that previous studies, by not measuring or adjusting for emotional abuse, were unable to account for the contribution of this type of trauma, which is likely to have co-occurred with the sexual abuse (in our sample of alcohol dependent individuals, 70% of those who experienced sexual abuse also experienced emotional abuse). While we controlled for gender effects in our analyses, the results indicate that gender did not contribute to alcohol dependence severity, suggesting that emotional abuse may be an important risk factor for both men and women. It is possible, however, that gender effects would emerge in a larger sample, with different types of trauma having more gender-specific influences. As the number of women in our inpatient research programs increases, we hope to be able to address this question in the future.
Our finding that the relationship between emotional abuse and alcohol dependence severity can be partially accounted for by neurotic personality traits is consistent with other studies that have suggested a mediating role for neuroticism in the association between stressful life experiences and adult behavioral health (Gamble et al., 2006). Neuroticism is broadly defined as the propensity for negative emotionality, with underlying subfacets including anxiety, anger hostility, self-consciousness, vulnerability, depression, and impulsiveness. These traits develop in late childhood, after which it has been argued that they either remain relatively stable in adulthood (Costa, Jr. and McCrae, 1988), or comprise both a stable component (i.e., a person-specific set point) and a fluctuating component that is sensitive to life experiences (Ormel et al., 2012). The stable set-point is proposed to be the risk factor for alcohol dependence and other psychopathology, consistent with the notion that early childhood trauma would play a role in establishing this set-point. Our data indicate that emotional abuse is positively associated with high levels of neurotic personality traits in general; however, only the impulsiveness subfacet was found to subsequently influence alcohol dependence severity. The impulsiveness subfacet represents the tendency to act on urges rather than reigning them in to delay gratification (Costa and McCrae, 2002). In line with the emphasis on negative affect, the impulsiveness subfacet most likely reflects negative urgency, or the tendency to act rashly when experiencing negative mood (Dick et al., 2010). The consistent experience of negative mood coupled with increased negative urgency may be a driving force behind heavy alcohol consumption and thus more severe dependence.
Our findings for physical abuse are more difficult to interpret. In this case, the direct positive association between physical abuse and alcohol dependence severity is dampened by a negative indirect effect resulting from an inverse association between physical abuse and withdrawal anxiety symptoms. The commonly held belief is that childhood physical abuse increases risk for anxiety and depression. However, many of the studies linking physical abuse and anxiety fail to account for important confounders such demographics, parental history of anxiety, more current stressors, and other comorbid psychiatric disorders (Cougle et al., 2010; Fuller-Thomson et al., 2012). Even though we control for some of these factors in our analyses, the finding of a negative association between physical abuse and withdrawal anxiety was unexpected. Anxiety during acute withdrawal is a heavily state dependent measure that is influenced by a number of factors, including perhaps overall withdrawal severity. However, including the maximum CIWA score for each individual obtained within the first couple of days of acute withdrawal as a potential mediator did not change the results (data not shown). Furthermore, analyzing anxiety and depression ratings measured subsequent to acute withdrawal (on day 9, resulting in a decreased sample size of 234 subjects due to missing data), did not alter the results not contribute significantly to the outcome (data not shown).
The genetic risk for alcohol dependence has in large part been linked to shared genetic risk for externalizing psychopathology, which is characterized by aggressive and impulsive personality traits and antisocial behavior (Kendler et al., 2003; Krueger et al., 2005). Alcohol dependence is, however, also highly co-morbid with internalizing disorders such as anxiety and depression, and an internalizing pathway to alcohol dependence involving negative affect has also been described (Hussong et al., 2011). These two pathways are not necessarily mutually exclusive. Neuroticism as a personality trait in general has a strong shared genetic component with internalizing disorders (Hettema et al., 2006), but also accounts for some of the comorbidity between internalizing and externalizing disorders, as well as comorbidity within externalizing disorders (Khan et al., 2005). In this context, our findings are consistent with the concept of an internalizing pathway to alcohol dependence. We found exposure to emotional abuse correlated with neuroticism, which in turn correlated with greater severity of alcohol dependence. This “negative affect” pathway is likely to involve mood-related drinking motives, i.e., drinking to cope with negative mood, which have been shown to mediate relationships between negative affect, major depression, and alcohol-related problems (Young-Wolff et al., 2009).
Our study does have limitations. The findings are based on retrospective, cross-sectional analysis of childhood trauma exposure, which introduces the potential for recall bias and possible differences in recall bias between alcoholics and controls, limiting inferences regarding direct causality. Furthermore, our model is not to be taken as an exhaustive analysis of the link between childhood trauma and alcohol dependence severity. The “direct” effect of emotional abuse on alcohol dependence severity could be accounted for by other mediators not included in our analysis, such as variation in brain structure and function, and in the neuroendocrine stress response. In addition, we did not have data on recent or current life stressors or trauma that may have potentiated any relationships with early life experiences. Future studies will assess the potential moderating effects of these factors, as well as gender and genetic variation.
In conclusion, our results indicate that exposure to childhood trauma, in particular emotional and physical abuse, may be a particularly significant risk factor for the development of severe alcohol dependence. Our findings are based on a sample of treatment-seeking alcoholics, a population characterized by greater alcohol use, greater severity of dependence, greater psychiatric co-morbidity, and lower quality of life in general, compared to subjects identified as alcohol dependent in epidemiological samples (Fein and Landman, 2005; LoCastro et al., 2008). As such, our findings are particularly relevant for clinical populations of alcohol dependent patients, and point to the possibility that alcohol dependent patients with a history of childhood emotional abuse may represent a clinically distinct sub-group of alcoholics. Given that less than 1 in 4 alcoholics ever seek treatment (Hasin et al., 2007), and that relapse rates in alcoholics are very high, there is a clear need for individualized treatment approaches. Our data suggest that alcoholics with histories of childhood abuse may benefit from tailored treatment approaches that incorporate a focus on the long-term effects of childhood abuse and resulting psychiatric and psychosocial needs.
Supplementary Material
Acknowledgments
This study was supported by intramural research funding from the National Institute on Alcohol Abuse and Alcoholism. All study procedures were reviewed and approved by the National Institutes of Health Combined Neuroscience (CNS) Institutional Review Board. Voluntary, written informed consent was obtained from all participants.
Financial Support: This study was supported by intramural research funding from the National Institute on Alcohol Abuse and Alcoholism.
Footnotes
Declaration of Interest
None.
References
- Anda RF, Felitti VJ, Bremner JD, Walker JD, Whitfield C, Perry BD, Dube SR, Giles WH. The enduring effects of abuse and related adverse experiences in childhood. A convergence of evidence from neurobiology and epidemiology. European Archives of Psychiatry and Clinical Neuroscience. 2006;256:174–186. doi: 10.1007/s00406-005-0624-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asberg M, Schalling D. Construction of a new psychiatric rating instrument, the Comprehensive Psychopathological Rating Scale (CPRS) Progress in Neuro-Psychopharmacology. 1979;3(4):405–412. doi: 10.1016/0364-7722(79)90055-9. [DOI] [PubMed] [Google Scholar]
- Babor T. The Alcohol Use Disorders Identification Test: Guidelines for use in primary health care. WHO/MNH/DAT/89.4; 1989. [Google Scholar]
- Bernstein D, Fink L. Childhood Trauma Questionnaire: A Retrospective Self-Report Questionnaire and Manual. San Antonio, TX: Psychological Corp; 1998. [Google Scholar]
- Bernstein DP, Stein JA, Newcomb MD, Walker E, Pogge D, Ahluvalia T, Stokes J, Handelsman L, Medrano M, Desmond D, Zule W. Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse and Neglect. 2003;27:169–190. doi: 10.1016/s0145-2134(02)00541-0. [DOI] [PubMed] [Google Scholar]
- Bowlby J. Attachment and Loss. New York: Basic Books; 1969. [Google Scholar]
- Bremner JD. Long-term effects of childhood abuse on brain and neurobiology. Child and Adolescent Psychiatric Clinics of North America. 2003;12:271–292. doi: 10.1016/s1056-4993(02)00098-6. [DOI] [PubMed] [Google Scholar]
- Copeland WE, Magnusson A, Goransson M, Heilig MA. Genetic moderators and psychiatric mediators of the link between sexual abuse and alcohol dependence. Drug and Alcohol Dependence. 2011;115:183–189. doi: 10.1016/j.drugalcdep.2010.10.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costa PT, Jr, McCrae RR. Personality in adulthood: a six-year longitudinal study of self-reports and spouse ratings on the NEO Personality Inventory. Journal of Personality and Social Psychology. 1988;54:853–863. doi: 10.1037//0022-3514.54.5.853. [DOI] [PubMed] [Google Scholar]
- Costa PT, McCrae RR. NEO Personality Inventory-Revised (NEO PI-R)APA. Washington, DC: 2002. [Google Scholar]
- Cougle JR, Timpano KR, Sachs-Ericsson N, Keough ME, Riccardi CJ. Examining the unique relationships between anxiety disorders and childhood physical and sexual abuse in the National Comorbidity Survey-Replication. Psychiatry Research. 2010;177:150–155. doi: 10.1016/j.psychres.2009.03.008. [DOI] [PubMed] [Google Scholar]
- Dick DM, Smith G, Olausson P, Mitchell SH, Leeman RF, O'Malley SS, Sher K. Understanding the construct of impulsivity and its relationship to alcohol use disorders. Addict.Biol. 2010;15:217–226. doi: 10.1111/j.1369-1600.2009.00190.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Enoch MA. The role of early life stress as a predictor for alcohol and drug dependence. Psychopharmacology (Berl) 2011;214:17–31. doi: 10.1007/s00213-010-1916-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Etain B, Mathieu F, Henry C, Raust A, Roy I, Germain A, Leboyer M, Bellivier F. Preferential association between childhood emotional abuse and bipolar disorder. J.Trauma Stress. 2010;23:376–383. doi: 10.1002/jts.20532. [DOI] [PubMed] [Google Scholar]
- Fein G, Landman B. Treated and treatment-naive alcoholics come from different populations. Alcohol. 2005;36:19–26. [PMC free article] [PubMed] [Google Scholar]
- Fuller-Thomson E, Sohn HR, Brennenstuhl S, Baker TM. Is childhood physical abuse associated with anxiety disorders among adults? Psychol.Health Med. 2012 doi: 10.1080/13548506.2012.686618. [DOI] [PubMed] [Google Scholar]
- Gamble SA, Talbot NL, Duberstein PR, Conner KR, Franus N, Beckman AM, Conwell Y. Childhood sexual abuse and depressive symptom severity: the role of neuroticism. Journal of Nervous and Mental Disease. 2006;194:382–385. doi: 10.1097/01.nmd.0000218058.96252.ac. [DOI] [PubMed] [Google Scholar]
- Glaser D. How to deal with emotional abuse and neglect: further development of a conceptual framework (FRAMEA) Child Abuse and Neglect. 2011;35:866–875. doi: 10.1016/j.chiabu.2011.08.002. [DOI] [PubMed] [Google Scholar]
- Glover DA, Loeb TB, Carmona JV, Sciolla A, Zhang M, Myers HF, Wyatt GE. Childhood sexual abuse severity and disclosure predict posttraumatic stress symptoms and biomarkers in ethnic minority women. J.Trauma Dissociation. 2010;11:152–173. doi: 10.1080/15299730903502920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldman D, Oroszi G, Ducci F. The genetics of addictions: uncovering the genes. Nature Reviews Genetics. 2005;6:521–532. doi: 10.1038/nrg1635. [DOI] [PubMed] [Google Scholar]
- Hasin DS, Stinson FS, Ogburn E, Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV alcohol abuse and dependence in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Archives of General Psychiatry. 2007;64:830–842. doi: 10.1001/archpsyc.64.7.830. [DOI] [PubMed] [Google Scholar]
- Heim C, Nemeroff CB. The role of childhood trauma in the neurobiology of mood and anxiety disorders: preclinical and clinical studies. Biological Psychiatry. 2001;49:1023–1039. doi: 10.1016/s0006-3223(01)01157-x. [DOI] [PubMed] [Google Scholar]
- Hettema JM, Neale MC, Myers JM, Prescott CA, Kendler KS. A population-based twin study of the relationship between neuroticism and internalizing disorders. American Journal of Psychiatry. 2006;163:857–864. doi: 10.1176/ajp.2006.163.5.857. [DOI] [PubMed] [Google Scholar]
- Hill EM, Blow FC, Young JP, Singer KM. Family history of alcoholism and childhood adversity: joint effects on alcohol consumption and dependence. Alcohol Clin.Exp.Res. 1994;18:1083–1090. doi: 10.1111/j.1530-0277.1994.tb00085.x. [DOI] [PubMed] [Google Scholar]
- Huang M-C, Schwandt ML, Ramchandani VA, George DT, Heilig M. Impact of multiple types of childhood trauma exposure on risk of psychiatric comorbidity among alcoholic inpatients. Alcoholism, Clinical and Experimental Research. 2012 doi: 10.1111/j.1530-0277.2011.01695.x. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hussong AM, Jones DJ, Stein GL, Baucom DH, Boeding S. An internalizing pathway to alcohol use and disorder. Psychol.Addict.Behav. 2011;25:390–404. doi: 10.1037/a0024519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hyman SM, Paliwal P, Chaplin TM, Mazure CM, Rounsaville BJ, Sinha R. Severity of childhood trauma is predictive of cocaine relapse outcomes in women but not men. Drug and Alcohol Dependence. 2008;92:208–216. doi: 10.1016/j.drugalcdep.2007.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler KS, Prescott CA, Myers J, Neale MC. The structure of genetic and environmental risk factors for common psychiatric and substance use disorders in men and women. Archives of General Psychiatry. 2003;60:929–937. doi: 10.1001/archpsyc.60.9.929. [DOI] [PubMed] [Google Scholar]
- Khan AA, Jacobson KC, Gardner CO, Prescott CA, Kendler KS. Personality and comorbidity of common psychiatric disorders. British Journal of Psychiatry. 2005;186:190–196. doi: 10.1192/bjp.186.3.190. [DOI] [PubMed] [Google Scholar]
- Krueger RF, Markon KE, Patrick CJ, Iacono WG. Externalizing psychopathology in adulthood: a dimensional-spectrum conceptualization and its implications for DSM-V. Journal of Abnormal Psychology. 2005;114:537–550. doi: 10.1037/0021-843X.114.4.537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LoCastro JS, Potter JS, Donovan DM, Couper D, Pope KW. Characteristics of first-time alcohol treatment seekers: the COMBINE Study. J.Stud.Alcohol Drugs. 2008;69:885–895. doi: 10.15288/jsad.2008.69.885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magnusson A, Lundholm C, Goransson M, Copeland W, Heilig M, Pedersen NL. Familial influence and childhood trauma in female alcoholism. Psychological Medicine. 2011:1–9. doi: 10.1017/S0033291711001310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mann RE, Sobell LC, Sobell MB, Pavan D. Reliability of a family tree questionnaire for assessing family history of alcohol problems. Drug and Alcohol Dependence. 1985;15:61–67. doi: 10.1016/0376-8716(85)90030-4. [DOI] [PubMed] [Google Scholar]
- McFarlane A, Clark CR, Bryant RA, Williams LM, Niaura R, Paul RH, Hitsman BL, Stroud L, Alexander DM, Gordon E. The impact of early life stress on psychophysiological, personality and behavioral measures in 740 non-clinical subjects. J.Integr.Neurosci. 2005;4:27–40. doi: 10.1142/s0219635205000689. [DOI] [PubMed] [Google Scholar]
- Ormel J, Riese H, Rosmalen JG. Interpreting neuroticism scores across the adult life course: immutable or experience-dependent set points of negative affect? Clinical Psychology Review. 2012;32:71–79. doi: 10.1016/j.cpr.2011.10.004. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav.Res.Methods. 2008;40:879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- Rees CA. Understanding emotional abuse. Arch.Dis.Child. 2010;95:59–67. doi: 10.1136/adc.2008.143156. [DOI] [PubMed] [Google Scholar]
- Riggs SA. Childhood emotional abuse and the attachment system across the life cycle: what theory and research tell us. Journal of Aggression, Maltreatment and Trauma. 2010;19:5–51. [Google Scholar]
- Rothman EF, Edwards EM, Heeren T, Hingson RW. Adverse childhood experiences predict earlier age of drinking onset: results from a representative US sample of current or former drinkers. Pediatrics. 2008;122:e298–e304. doi: 10.1542/peds.2007-3412. [DOI] [PubMed] [Google Scholar]
- Ruiz MA, Pincus AL, Dickinson KA. NEO PI-R predictors of alcohol use and alcohol-related problems. Journal of Personality Assessment. 2003;81:226–236. doi: 10.1207/S15327752JPA8103_05. [DOI] [PubMed] [Google Scholar]
- Scher CD, Stein MB, Asmundson GJ, McCreary DR, Forde DR. The childhood trauma questionnaire in a community sample: psychometric properties and normative data. J.Trauma Stress. 2001;14:843–857. doi: 10.1023/A:1013058625719. [DOI] [PubMed] [Google Scholar]
- Skinner HA, Allen BA. Alcohol dependence syndrome: measurement and validation. Journal of Abnormal Psychology. 1982;91(3):199–209. doi: 10.1037//0021-843x.91.3.199. [DOI] [PubMed] [Google Scholar]
- Skinner HA, Sheu WJ. Reliability of alcohol use indices. The Lifetime Drinking History and the MAST. Journal of Studies on Alcohol. 1982;43:1157. doi: 10.15288/jsa.1982.43.1157. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB. Timeline Follow-back: A technique for assessing self-reported ethanol consumption. In: Allen J, Litten R, editors. Measuring Alcohol Consumption: Psychosocial and Biochemical Methods. Totowa, NJ: Humana Press; 1992. pp. 41–72. [Google Scholar]
- Suomi SJ. Early stress and adult emotional reactivity in rhesus monkeys. Ciba Foundation Symposium. 1991;156:171–183. doi: 10.1002/9780470514047.ch11. [DOI] [PubMed] [Google Scholar]
- Thompson AE, Kaplan CA. Childhood emotional abuse. British Journal of Psychiatry. 1996;168:143–148. doi: 10.1192/bjp.168.2.143. [DOI] [PubMed] [Google Scholar]
- Weinstock LM, Whisman MA. Neuroticism as a common feature of the depressive and anxiety disorders: a test of the revised integrative hierarchical model in a national sample. Journal of Abnormal Psychology. 2006;115:68–74. doi: 10.1037/0021-843X.115.1.68. [DOI] [PubMed] [Google Scholar]
- Widom CS, White HR, Czaja SJ, Marmorstein NR. Long-term effects of child abuse and neglect on alcohol use and excessive drinking in middle adulthood. J.Stud.Alcohol Drugs. 2007;68:317–326. doi: 10.15288/jsad.2007.68.317. [DOI] [PubMed] [Google Scholar]
- Young-Wolff KC, Kendler KS, Ericson ML, Prescott CA. Accounting for the association between childhood maltreatment and alcohol-use disorders in males: a twin study. Psychological Medicine. 2011;41:59–70. doi: 10.1017/S0033291710000425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young-Wolff KC, Kendler KS, Sintov ND, Prescott CA. Mood-related drinking motives mediate the familial association between major depression and alcohol dependence. Alcohol Clin.Exp.Res. 2009;33:1476–1486. doi: 10.1111/j.1530-0277.2009.00978.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.